Abstract
Low- and middle-income countries (LMICs) are experiencing a growing burden of non-communicable diseases (NCDs) and confront challenges of leadership, lack of local data and evidence, and gaps in implementation of successful interventions. To address these challenges, we designed an interdisciplinary training program, the Public Health Leadership and Implementation Academy (PH-LEADER) for NCDs. The year-long program has three components; a two-month preparation period; a three-week, in-person summer short course; and an in-country mentored project phase. The training was directed at mid-career, high-potential public health professionals from LMICs who are involved in NCDs prevention and control. We collected demographic data and information about achievements and products attained from participation in the program among trainees. Over four and a half years (2012–2016), 67 NCDs professionals (mean age 38.7 years; 58% male) from 11 countries have been trained. The training program has promoted the design and implementation of 49 projects focused on implementation of programs and policies addressing NCDs; 20 manuscripts submitted for publication; and four abstracts submitted for conference presentations. The PH-LEADER program promotes the design and implementation of evidence-based strategies to address NCDs in LMICs. Impact on trainee implementation research capacity and leadership skills and ultimately on NDCs prevention and control is yet to be assessed.
Keywords: capacity building, chronic disease, implementation science, leadership
Non-communicable diseases (NCDs), encompassing cardiovascular disease (CVD), diabetes, cancers, mental illness, and chronic respiratory diseases, threaten the health and economies of individuals and populations alike.1 NCDs account for 68% of all deaths worldwide and are a serious public health threat to low- and middle-income countries (LMICs), where 80% of NCDs occur.2-4 It is estimated that by 2020, NCDs will account for 80% of the global burden of disease and will cause seven out of every ten deaths in LMICs.5 NCDs are also a barrier to development6 because the economically active age group (25–64 years) in LMICs bears the greatest morbidity and mortality, resulting in loss of human capital and productivity.
To address the growing NCDs burden, LMICs confront major challenges such as limited health financing, scarcity of local data/evidence, and heterogeneity in access and care delivery. These challenges are compounded by two significant and often underrecognized challenges—limited human capacity and lack of leadership. Limited capacity is one of the reasons that implementation of proven strategies (e.g., lifestyle modification, tobacco control, CVD risk reduction through low-cost drugs, quality diabetes care) to prevent onset of risk factors7-9 or incidence of diseases (CVD events, cancers, diabetes complications)10-14 is sub-optimal, especially so in LMICs. Lack of leadership can be a barrier to evidence-based public health practice and can affect public health system performance.15,16
Though training can improve implementation research capacity and leadership skills in the public health workforce,17-19 no training opportunities that combine these skillsets exist for LMICs. To address this gap, we designed the Public Health Leadership and Implementation Academy (PH-LEADER) for NCDs. The primary goal of this program is to build implementation science capacity and leadership skills to promote the development of a cadre of 21st-century global NCDs leaders. In the present article, we describe the program and present preliminary findings of an ongoing impact evaluation.
METHODS
The field of implementation science focuses on making research findings more useful in everyday clinical and public health practice,20,21 assimilating issues of cost-effectiveness and efficiency, acceptability, availability, and sustainability into programmatic endeavors to improve population health.22 Implementation research requires the ability to identify, understand, and address the barriers to adoption and maintenance of evidence-based interventions and capacity to adapt findings from controlled settings to real-world contexts and to promote sustainability.23 Few, if any, LMICs have sufficient implementation research capacity to achieve systems enhancement and integration of preventative and curative services required to address NCDs.
Implementation research also requires strong leaders to address challenges and opportunities (e.g., political issues) associated with disseminating evidence16; it requires leaders who can challenge the status quo of an organization and introduce new ways of making decisions.16 Effective leaders can shape the organizational culture to make it supportive of innovative, evidence-based public health strategies. Indeed, organizational leadership that is focused on the science base, quality, and performance is a strong predictor of solid public health system performance.15 Public health leaders must have transformational, legislation and political, transorganizational, and team/group competencies to address the complex and changing demands of public health services.24 Further, effective leaders must have the ability to apply scientific knowledge to public health problems.25 Training that fosters leadership competencies while providing education and encouragement represents a promising strategy to promote effective leadership.18
Our training program directly addresses applied capacity in implementation sciences and leadership competencies. Our collaborative program is founded on longstanding, robust partnerships between Emory University (Atlanta, Georgia) and world-class institutions in Mexico (Instituto Nacional de Salud Pública [INSP]) and India (Public Health Foundation of India [PHFI]). The program aims to promote the development of mid-career health professionals from LMICs by fostering implementation science and leadership competencies and offering encouragement and career development opportunities. The PH-LEADER program is supported by National Institutes of Health's (NIH) Fogarty International Center.
The program is based on the evidence-based public health (EBPH) framework, which outlines essential components to improve evidence use in public health.16 These include making decisions on the basis of the best available, peer-reviewed evidence; using data and information systems systematically; applying program-planning frameworks; engaging the community in decision making; conducting sound evaluation; and disseminating findings. To complete these tasks, analytical skills (public health surveillance, systematic reviews, economic evaluation, and epidemiology), implementation science skills (designing evidence-based interventions, monitoring/promoting their implementation, and assessing their impacts), and leadership skills (promoting commitment, decision making) are needed (Figure 1).
FIGURE 1.
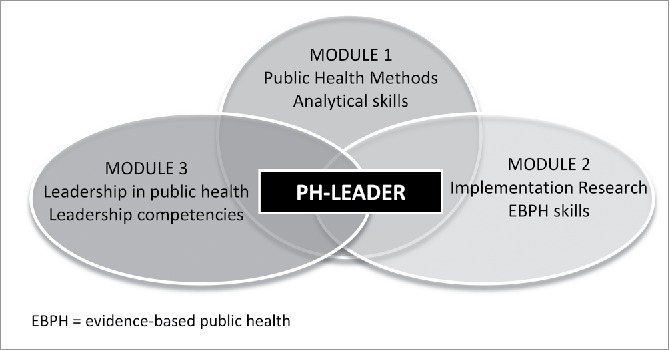
PH-LEADER Training Course Modules, Focus, and Targeted Skills
The PH-LEADER program focuses on fostering the aforementioned skills. The year-long program is a hybrid model incorporating three complementary components: a two-month preparation period, a three-week summer short course (the academy), and a nine-month in-country, mentored project phase (Table 1). The two-month preparation period involves readings and information documents aimed at laying the knowledge and work-dynamic foundation the course will require. This preparation period precedes the summer course.
TABLE 1.
PH-LEADER 12-Month Training Program Components and Competencies Targeted
| Program Content | Competencies |
|---|---|
|
|
|
|
|
|
The summer academy is a three-week, intensive, multidisciplinary, executive-style course hosted at Emory University. The course incorporates world-class faculty and a dynamic mix of theoretical concepts, applied learning, active discussion, and workshops. The course is composed of three modules: public health methods, implementation research, and leadership. The public health methods module includes courses in basic health economics, basic epidemiology, data integration and information systems, and health systems research to provide trainees with analytical skills to identify and quantify a problem. The implementation research module targets EBPH skills and includes two-part sessions that lead participants from program concept and design through implementation and evaluation, using case studies as examples to illustrate and learn from previous experiences. The leadership module includes interactive and participatory sessions on leadership, management, and communication to enhance self-awareness and self-efficacy23 and organizational management sessions to support participants' abilities to maneuver institutional, political, and cultural environments (Table 1).24
The summer academy is followed by a structured nine-month mentored phase that involves applying theoretical knowledge and distance learning. This phase includes two tandem components: monthly webinars and participant-led in-country mentored projects (Table 1). The monthly webinars include sessions to reinforce analytical, implementation research, and leadership skills and serve to provide a platform for completion of group assignments and to maintain the network of trainees engaged and interacting. For the mentored project component, participants design their own project, which can focus on the design, implementation, and/or evaluation of policies, interventions, or strategies for addressing NCDs in their home countries.
For the mentored project, participants identify experienced PH-LEADER faculty who serve as in-country mentors throughout project completion. These mentors are largely public health academics from the national public health institutes in Mexico and India and, in some cases, US academics and Centers for Disease Control and Prevention personnel who provide remote mentorship. Once trainees are back in their in-country positions, they consult with mentors for project guidance, career planning and advice, advice on addressing challenging work situations, and professional development guidance. The nature of the trainee–mentor interactions is ad hoc and dependent on initiative from the trainee, with some encouragement and assignments to prompt interactions with mentors and guidance seeking.
The principles participants learn during the summer academy are expected to be integrated and applied during the mentored phase at trainees' home institutions. This phase is expected to have a cascade effect where each trainee joins the alumni network, shares tools and training with in-country peers, and mentors future prospective leaders and innovators.
Participant Recruitment and Selection
PH-LEADER targeted mid-career, high-potential professionals from Mexico and India (funded by the NIH) as well as participants from other LMICs (through other funding support). Eligible applicants for NIH-supported enrollment were practitioners or researchers directly affiliated with the INSP or PHFI or with specified strategic partner institutions in their country. The training program was advertised internally at partner institutions (e.g., INSP and PHFI) and externally via email listservs, websites, and word of mouth, encouraging interested participants to apply. Applicants with high potential based on their years of experience, their likelihood of moving into a position of influence within their organization, and with potential to impact public health and NCDs in their home country were accepted. The first cohort of trainees began the program in 2013 and subsequent annual cohorts in 2014, 2015, and 2016, with this being the last year of the program.
Program Evaluation
We collected demographic information to assess the characteristics of trainees. To assess the program's impact on professional development, we collected self-reported annual information regarding achievements (e.g., job promotion and career advancements) and products (e.g., publications, project scale-up or expansion, additional funding obtained) associated with program participation.
Impact evaluation is ongoing and we are currently collecting data on trainee-perceived competence to carry out implementation research and leadership competencies to assess changes on these outcomes.
RESULTS
The program set an original goal of training 60 professionals from India and Mexico over five years. Despite a reduction in the funding period, the program has leveraged local support and trained a total of 67 NCDs professionals (mean age 38.7 years; 58% male) over the four and a half years of implementation (2012–2016). Trainees to date have come from 11 countries: Barbados, Brazil, Colombia, India, Guatemala, Georgia, Liberia, Malawi, Mexico, the Kingdom of Saudi Arabia, and the United States (Table 2).
TABLE 2.
PH-LEADER Trainee Characteristics by Cohort Year
| Characteristic | 2013 Cohort (n = 14), Mean (SD) or n (%) | 2014 Cohort (n = 21) Mean (SD) or n (%) | 2015 Cohort (n = 32) Mean (SD) or n (%) |
|---|---|---|---|
| Age | 39.6 (6.6) | 38.1 (6.6) | 38.4 (7.7) |
| Male | 6 (57) | 10 (56) | 20 (62) |
| Position | |||
| Researcher | 7 (50) | 7 (33) | 11 (35) |
| Professor | 3 (22) | 6 (29) | 7 (23) |
| Director | 2 (14) | 6 (29) | 7 (23) |
| Consultant | 2 (14) | 2 (9) | 6 (19) |
| Institution | |||
| Academic | 3 (21) | 4 (19) | 6 (19) |
| Government | 7 (50) | 6 (29) | 9 (28) |
| Foundation | 3 (22) | 11 (52) | 5 (16) |
| Civil society | 0 | 0 | 2 (6) |
| Health care | 1 (7) | 0 | 9 (28) |
| Country | |||
| India | 6 (43) | 10 (48) | 13 (42) |
| Mexico | 6 (43) | 8 (38) | 6 (19) |
| Brazil | 1 (7) | 1 (5) | — |
| Colombia | 1 (7) | 1 (5) | — |
| Kingdom of Saudi Arabia | — | — | 6 (19) |
| Barbados | — | — | 2 (6) |
| Georgia | — | — | 1 (3) |
| Guatemala | — | — | 1 (3) |
| Malawi | — | 1 (5) | — |
| Liberia | — | — | 1 (3) |
| United States | — | — | 1 (3) |
In terms of reported achievements across trainee cohorts, the training program has led to the design and implementation of promising strategies, to additional funding, and to several manuscripts. To date, 49 projects that focus on implementation of programs and policies addressing NCDs have been completed or are ongoing. Further, trainees have submitted a total of 20 manuscripts for publication (13 India/seven Mexico); submitted four abstracts for conference presentations (one India/three Mexico); and have developed new research proposals building upon existing projects (three India/three Mexico).
The one-year program cost on average 4,000 USD per participant. However, for the majority of participants, the program was free because they were covered by funding from NIH. Non-NIH-supported participants identified funding through other sources to attend. For the others, a tiered fee system was applied by country income group of the participant.
The impact evaluation of the program is still ongoing and results will be included in a subsequent, more comprehensive manuscript.
DISCUSSION
The PH-LEADER program is a unique, interdisciplinary, multifaceted training program that bridges NCDs, implementation science, and public health leadership in an integrative manner. This program provides a blended learning experience that includes face-to-face, e-learning, and practical experiences with world-leading experts in an interdisciplinary setting. To date, the program has trained 67 NCDs professionals from 11 countries over the four and a half years of implementation (2012–2016). The program promotes the design and implementation of strategies aimed at addressing the NCD burden in LMICs.
Existing training initiatives show that implementation research and leadership skills can be improved,17-19 though they have tackled these skillsets separately. For instance, the EBPH program focuses on training public health practitioners to use an evidence-based, scientific approach to develop and evaluate NCD programs.17,19 The US National Public Health Leadership Institute program focuses on training collaborative leaders and creating networks among them to address public health problems.18 Our program addresses both skillsets jointly and introduces business principles and innovations that may be leveraged by participants to evaluate the effectiveness of their programs and how they can impact the culture of their home institutions.
The program's overarching vision is that through energizing and kick-starting the careers of young professionals and contributing to LMICs' institutional capacity development and maturing of systems, we will make a significant contribution to addressing NCDs.26,27 We ultimately see the program as having an impact on LMICs in terms of the ability for trainees to successfully manage and guide their teams and projects and in the quality of research projects they carry out to address NCDs. As PH-LEADER alums take on leadership roles in their countries, we will encourage them to remain self-aware and harness their training, experience, and knowledge to be more effective leaders. Indeed, in leading teams, we hope that PH-LEADER alums will disseminate some of these leadership principles, guiding and mentoring others, having a ripple effect and influencing organizational cultures and program effectiveness. Overall, we believe that the PH-LEADER program can contribute to increase both the global health leadership workforce and its ability to address the burdens of NCDs in LMICs.
Over the years, implementation of PH-LEADER has taught us several lessons. First, we learned that bringing together middle-level decision makers from universities, public institutions, and the public sector for a grueling executive education–style course is an effective strategy to expand trainee networks, which can lead to fruitful collaborations to effect change. We have also learned that program implementation and refinement is a dynamic, iterative process and, as such, our program has evolved over time and will continue to do so in the following years. Because trainees come from different countries and institutions, it has been challenging to set a common ground to nurture discussion and collaborative work. Through empathy, respect, and acceptance, the program has become an open forum for the exchange of ideas in a supportive environment that fosters cross-cultural exchange and to grapple with issues from different perspectives.
The program is still ongoing, as are the efforts to assess its impact and promote its sustainability. Our ongoing evaluation is examining the effects of PH-LEADER on trainee implementation research skills and leadership competencies. Future evaluations will examine the long-term impact of PH-LEADER; we plan to follow trainees over five years after training to examine impact on competencies. Future evaluations will also assess the impact of trainee projects on NCDs, though this will be challenging. We plan to encourage project completion and support data collection to assess impacts on prevention or treatment outcomes. Finally, sustainability of the program cannot be ensured if solely based on US government funds; thus, we are currently exploring strategies to sustaining the program post-NIH funding (e.g., seeking funding from private philanthropies or foundations, shortening the program duration, and delivering it in-country).
CONCLUSION
The PH-LEADER program is a unique, interdisciplinary, multifaceted training program that bridges NCDs, implementation science, and public health leadership in an integrative manner. We ultimately see the program as having an impact on LMICs in terms of the ability for trainees to successfully manage and guide their teams and projects and in the quality of research projects they carry out to address NCDs. The gap between evidence and real-world implementation of effective strategies to address NCDs could be shortened by training effective public health leaders; this program can contribute to increase both the global health leadership workforce and its ability to address the burdens of NCDs in LMICs.
DISCLOSURE OF POTENTIAL CONFLICTS OF INTEREST
The authors were involved in the design and implementation of the program. The authors declare no other conflict of interest.
ACKNOWLEDGMENTS
We thank the faculty members who have participated over the years and provided mentoring and guidance to our trainees.
Funding
The PH-LEADER program and research reported in this publication were supported by the Fogarty International Center of the National Institutes of Health under Award Number D43TW009135. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
REFERENCES
- [1].Terzic A, Waldman S. Chronic diseases: the emerging pandemic. Clin Transl Sci 2011; 4(3): 225-226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].International Diabetes Federation Diabetes atlas. 7th ed. 2015. Available at http://www.diabetesatlas.org/resources/2015-atlas.html (accessed 10May2016)
- [3].World Health Organization Global status report on noncommunicable diseases. 2014. Available at http://www.who.int/nmh/publications/ncd-status-report-2014/en/ (accessed 12May2016) [DOI] [PubMed]
- [4].Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2013; 386(9995): 743-800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].World Health Organization Global action plan for the prevention and control of noncommunicable diseases 2013–2020. 2013. Available at http://www.who.int/nmh/events/ncd_action_plan/en/ (accessed 5June2016) [Google Scholar]
- [6].Beaglehole R, Bonita R, Horton R, Adams C, Alleyne G, Asaria P, Baugh V, Bekedam H, Billo N, Casswell S, et al.. Priority actions for the non-communicable disease crisis. Lancet 2011; 377(9775): 1438-1447. [DOI] [PubMed] [Google Scholar]
- [7].Diabetes Prevention Program Research Group 10-Year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet 2009; 374(9702): 1677-1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Li G, Zhang P, Wang J, Gregg EW, Yang W, Gong Q, Li H, Li H, Jiang Y, An Y, et al.. The long-term effect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention Study: a 20-year follow-up study. Lancet 2008; 371(9626): 1783-1789. [DOI] [PubMed] [Google Scholar]
- [9].Lindström J, Ilanne-Parikka P, Peltonen M, Aunola S, Eriksson JG, Hemiö K, Hämäläinen H, Härkönen P, Keinänen-Kiukaanniemi S, Laakso M, et al.. Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the Finnish Diabetes Prevention Study. Lancet 2006; 368(9548): 1673-1679. [DOI] [PubMed] [Google Scholar]
- [10].Saaddine JB, Engelgau MM, Beckles GL, Gregg EW, Thompson TJ, Narayan KM. A diabetes report card for the United States: quality of care in the 1990s. Ann Intern Med 2002; 136(8): 565-574. [DOI] [PubMed] [Google Scholar]
- [11].Beckles GL, Engelgau MM, Narayan KM, Herman WH, Aubert RE, Williamson DF. Population-based assessment of the level of care among adults with diabetes in the U.S. Diabetes Care 1998; 21(9): 1432-1438. [DOI] [PubMed] [Google Scholar]
- [12].Saydah SH, Fradkin J, Cowie CC. Poor control of risk factors for vascular disease among adults with previously diagnosed diabetes. JAMA 2004; 291(3): 335-342. [DOI] [PubMed] [Google Scholar]
- [13].Savage PJ. Treatment of diabetes mellitus to reduce its chronic cardiovascular complications. Curr Opin Cardiol 1998; 13(2): 131-138. [DOI] [PubMed] [Google Scholar]
- [14].EUROASPIRE II Study Group Lifestyle and risk factor management and use of drug therapies in coronary patients from 15 countries; principal results from EUROASPIRE II Euro Heart Survey Programme. Eur Heart J 2001; 22(7): 554-572. [DOI] [PubMed] [Google Scholar]
- [15].Scutchfield FD, Knight EA, Kelly AV, Bhandari MW, Vasilescu IP. Local public health agency capacity and its relationship to public health system performance. J Public Health Manag Pract 2004; 10(3): 204-215. [DOI] [PubMed] [Google Scholar]
- [16].Brownson RC, Fielding JE, Maylahn CM. Evidence-based public health: a fundamental concept for public health practice. Annu Rev Public Health 2009; 30: 175-201. [DOI] [PubMed] [Google Scholar]
- [17].Brownson RC, Diem G, Grabauskas V, Legetic B, Potemkina R, Shatchkute A, Baker EA, Campbell CR, Leet TL, Nissinen A, et al.. Training practitioners in evidence-based chronic disease prevention for global health. Promot Educ 2007; 14(3): 159-163. [PubMed] [Google Scholar]
- [18].Umble K, Steffen D, Porter J, Miller D, Hummer-McLaughlin K, Lowman A, Zelt S. The National Public Health Leadership Institute: evaluation of a team-based approach to developing collaborative public health leaders. Am J Public Health 2005; 95: 641-644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Gibbert WS, Keating SM, Jacobs JA, Dodson E, Baker E, Diem G, et al. Training the workforce in evidence-based public health: an evaluation of impact among US and international practitioners. Prev Chronic Dis 2013; 10: 130120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Narayan KM, Benjamin E, Gregg EW, Norris SL, Engelgau MM. Diabetes translation research: where are we and where do we want to be? Ann Intern Med 2004; 140(11): 958-963. [DOI] [PubMed] [Google Scholar]
- [21].Narayan KM, Gregg EW, Engelgau MM, Moore B, Thompson TJ, Williamson DF, Vinicor F. Translation research for chronic disease: the case of diabetes. Diabetes Care 2000; 23(12): 1794-1798. [DOI] [PubMed] [Google Scholar]
- [22].Damschroder L, Aron D, Keith R, Kirsh S, Alexander J, Lowery J. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci 2009; 4(50). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Garfield SA, Malozowski S, Chin MH, Narayan KM, Glasgow RE, Green LW, Hiss RG, Krumholz HM. Considerations for diabetes translational research in real-world settings. Diabetes Care 2003; 26(9): 2670-2674. [DOI] [PubMed] [Google Scholar]
- [24].Wright K, Rowitz L, Merkle A, Reid WM, Robinson G, Herzog B, Weber D, Carmichael D, Balderson TR, Baker E. Competency development in public health leadership. Am J Public Health 2000; 90(8): 1202–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Halverson PK, Mays G, Kalzuny AD, House RM. Developing leaders in public health: the role of executive training programs. J Health Admin Educ 1997; 15: 87-100. [PubMed] [Google Scholar]
- [26].Chalkidou K, Levine R, Dillon A. Helping poorer countries make locally informed health decisions. BMJ 2010; 341: c3651. [DOI] [PubMed] [Google Scholar]
- [27].Frenk J. The global health system: strengthening national health systems as the next step for global progress. PLoS Med 2010; 7(1): e1000089. [DOI] [PMC free article] [PubMed] [Google Scholar]


