Abstract
Objective
The stress of having a child with cancer can impact the quality of relationships within the family. The current study describes the longitudinal trajectory of marital, parent-child and sibling conflict beginning around the time of diagnosis through the first year of treatment. We examined the average level of marital, parent-child and sibling conflict at each monthly time point in the first year of treatment; the proportion of families that fall into the distressed range of marital, parent-child and sibling conflict at each time point; the typical trajectory of conflict during the first year of treatment and whether there are differences in trajectories across families.
Method
One hundred and sixty families of children newly diagnosed with cancer (M age=5.6 years; range=2–18 years) participated in a short-term prospective longitudinal study. Primary caregivers provided monthly reports of marital, parent-child and sibling conflict.
Results
Using Multilevel Modeling (MLM), most families showed stability in quality of family relationships, although considerable between-family variability was observed. For married couples, 25–36% of couples were in the distressed range at one time point over the first year of treatment. For married couples, more distress occurred at earlier months, particularly Month 3. For parent-child and sibling dyads, the most difficult time periods were during later months.
Conclusion
Implications for development of interventions that target at-risk family relationships are discussed. Identifying processes that predict between-family variability in trajectories of family relationships is an important next step, particularly for the marital relationship.
The stress of having a child with cancer affects the entire family unit and impacts relationships within the family (Long & Marsland, 2011). From a family systems perspective, the family is considered a system comprised of multiple interrelated parts, including individuals as well as relationships between individuals. In the context of childhood chronic illness, the child’s illness has consequences for all parts of the system (Kazak, 1989). Indeed, implications of a child’s cancer diagnosis such as the potential life-threatening nature of the illness, extensive and invasive treatment, repeated hospitalizations, and changes in roles and responsibilities can have far-ranging impact on the family as a whole (Hoekstra-Weebers, Jaspers, Kamps & Klip, 1998). To cope with this experience, family members may turn to each other for support. However, the stress of diagnosis and treatment can place considerable strain on the family and can lead to heightened levels of family conflict (Lavee, 2005).
For children, the quality of family relationships is a central factor that shapes their development (Gottman & Katz, 1989). Of all characteristics of family relationships, the nature and frequency of conflict is one of the best predictors of childhood adjustment (Cummings, Davies & Campbell, 2000). Indeed, Rutter (1985) identified family conflict as one of six risk factors most predictive of child psychopathology. Family conflict includes overt or covert negativity that may interfere with communication and emotional connection, and has been associated with a variety of adjustment difficulties in children, including conduct problems, depression and anxiety (Gottman & Katz, 1989; Cummings et al., 2000).
In families facing a diagnosis of pediatric cancer, conflict can be particularly problematic as it can compromise the family’s ability to work together to support the child through the difficult period of medical treatment and interfere with patient care. Empirical findings among non-cancer pediatric populations support the link between family conflict and detrimental medical outcomes. Children with diabetes who experience family conflict display poor adherence to medical regime and poor metabolic control (Lewin et al, 2006; Miller-Johnson et al, 1994). Family conflict can also affect a child’s response to medication (Townsend, Demeter, Youngstrom, Drotar & Findling, 2007) and is associated with a higher volume of health care use (Riley et al, 1993).
Few empirical studies have directly examined conflict in families of children with cancer. Research that has addressed this issue has largely focused on marital distress and conflict between the primary caregiver and the child with cancer. Moreover, studies on the effects of childhood cancer on the parent’s marriage have yielded conflicting results. Some studies have emphasized the adverse effects on the marital relationship. For example, Dahlquist et al. (1993) reported an elevated incidence of marital distress in parents of children with cancer at two months after diagnosis. Some studies report a steady decline in marital satisfaction from diagnosis to 10–12 months later (Fife, Norton & Groom, 1987). Similarly, Burns et al (2016) reported 25.5% of mothers and 21.3% of fathers reported significant marital distress and diagnosis and this increased to 36.2% of mothers and 42.6% of fathers two years later. Other studies show variability among couples in the pattern of marital satisfaction over time. For example, Hoekstra-Weebers et al. (1998) found that 43% of fathers and mothers reported more dissatisfaction at 12 months post-diagnosis, 29% of fathers and 43% of mothers reported no change in their level of satisfaction, and 26% of fathers and 14% of mothers indicated improvements in marital satisfaction over the 12 month period. Yet other studies find that the level of marital adjustment in this population does not differ from that of control groups (Larson, Wittrock & Sandgren, 1994; Leventhal-Belfer, Bakker & Russo, 1993). Studies of divorce suggest that the divorce rate is no higher in parents of children with cancer than in control groups (Syse et al, 2010).
While there is a body of work on parent-child communication and parenting stress in families of children with cancer (Long & Marsland, 2011; Mooney-Doyle & Deatrick, 2016; Bluebond-Langner, Wiener, Mack & Wolfe, 2016), only a handful of studies have examined conflict between primary caregivers and the child with cancer. Ishibashi (2001) found that children with cancer report higher levels of conflict with parents than healthy controls. Children’s report of conflict with mothers has also been associated with higher psychological distress in pediatric cancer patients (Marine & Miller, 1998). Although a larger body of research has examined sibling experiences and adjustment during pediatric cancer (Alderfer et al., 2010; Wilkins & Woodgate, 2005), only two studies to date have examined sibling conflict in families of children with cancer. Labay and Walco (2004) reported that sibling conflict was not associated with children’s psychosocial adjustment. Among adolescents with cancer, sibling conflict levels did not differ from a healthy comparison sample (Marine & Miller, 1998).
Methodological and conceptual limitations have contributed to contradictory findings and have left many questions unanswered. First, studies of family conflict typically examine family functioning at one point in time. To our knowledge, there are no longitudinal empirical studies of parent-child conflict, and six longitudinal studies of marital satisfaction have been reported. Three longitudinal studies evaluated families around the point of diagnosis and then at a second point in time many months or even years later. For example, Dahlquist et al (1996) evaluated families at two months post-diagnosis and then 20 months later, while Wijnberg-Williams, Van de Wiel, Kamps and Hoekstra-Weebers (2015) assessed families at diagnosis and then 5 years later. Burns et al (2016) evaluated families at diagnosis and then two years later. Three studies evaluated families at three or more time points across the first year of diagnosis. Hoekstra-Weebers et al (1998) assessed families at diagnosis, 6 months and 12 months later, and Kazak et al (2011) assessed families at diagnosis, 3 months and 6 months later. Fife, Norton and Groom (1987) evaluated families at five points in the first year of treatment, including diagnosis, 2 months, 4 months, 7 months and 10 months later. Additional research is needed on the longitudinal course of conflict in the parent-child, sibling and marital subsystems to better understand the impact of cancer on family relationships.
Second, one of the limitations of early studies is that they provide little descriptive information about family conflict over the first year of treatment. While declines in marital satisfaction (Fife et al, 1987) and between-family variability in the direction of changes in marital satisfaction have been reported (Hoekstra-Weebers et al, 1998), there is little information about the number of families that become maritally distressed over the course of treatment. The first year of treatment is a particularly vulnerable time for families, and there may be key points in the first year of diagnosis and treatment that are associated with increases in family conflict. Understanding the trajectory of family conflict over the first year of diagnosis and treatment can help us identify which family sub-systems are at greatest risk and build interventions that target at risk relationships and strengthen families as they face the challenges of a diagnosis of cancer.
A third methodological limitation is that studies to date focus on mean levels of marital quality which can obscure variability in the course and timing of any potential changes in marital adjustment (Long & Marsland, 2011). Fife et al (1987) reported that the sharpest decline in marital satisfaction occurred approximately four months following diagnosis but this was not based on any statistical analysis, and has not been replicated in other studies. Prior research largely provides information about the status of families at each observation, and how they might change from one time point to the next. However, family conflict is typically assumed to unfold as a result of dynamic interactions over time, and worsening (or improving) conflict is likely to change in a monotonic fashion. Trajectory models, such as growth curve modeling (e.g. Bollen & Curran, 2006), allow repeated observations over time to be summarized with a parsimonious line (i.e. a trajectory) that is assumed to produce the observations at each time point. For example, if marital satisfaction among parents of a child with cancer is steadily declining on average, growth curve models can provide a general summary of that decline. Moreover, they can provide information about the degree of individual differences in change, describing whether and how families might be differing from one another in how conflict changes over time. In contrast, the auto-regressive models (i.e. predicting one time point from the previous time point) that have typically been used to date provide no information about average change, but only provide information about how well rank order at one time point predicts rank order at the next. It is even possible to have high time-to-time correlations (which is often interpreted as “stability”) even while all participants in a sample are changing at similar rates (Bollen & Curran, 2006). Thus, growth curve models allow for a more in depth characterization of the trajectory of family conflict, including identifying critical points for conflict and better understanding variability across families in the course of conflict. Knowing when and which families show the most clinically significant changes in marital satisfaction can help guide the development of interventions that are administered at the time of greatest family need.
Fourth, the literature to date has been very limited and is based on a narrow view of what constitutes the family. Only a handful of studies have examined parent-child relationships in children with cancer, and these have largely been restricted to studies of social support or discipline (Decker, 2007; Wasserman, Thompson, Wilimas & Fairclough, 1987). To our knowledge, there are only two studies that have examined how a diagnosis of cancer impacts the relationship between cancer patients and their sibling. Sibling relationships are typically the longest family relationship a child will have and may become stressed during treatment because of changes in family structure and daily routines. Because children with cancer may spend less time with their healthy siblings due to time in treatment and side effects, positive communication between siblings may be reduced and conflict may increase (Breyer, Kunin, Kalish & Patenaude, 1993). Since attention and resources are typically directed towards helping the cancer patient, siblings may feel neglected and experience resentment towards the patient and their parents (Rollins, 1990). Previous research has consistently shown that receiving less favorable parental treatment than one’s sibling is positively associated with child behavior problems (McHale, Crouter, McGuire & Updegraff, 1995). Examining relationship quality between the cancer patient and their sibling can provide a fuller picture of how cancer diagnosis and treatment reverberates through the family and impacts other familial relationships.
In the current paper, we describe the longitudinal trajectory of marital, parent-child and sibling conflict beginning around the time of diagnosis through the first year of treatment. Monthly assessments of marital, parent-child and sibling conflict were obtained and multi-level modeling data analytic strategies were used to describe the trajectory of conflict within each family sub-system. Three main questions were addressed: (1) What is the average level of marital, parent-child and sibling conflict at each time point in the first year of treatment? (2) What proportion of families fall into the distressed range of marital, parent-child and sibling conflict at each time point and what proportion of families remain distressed over time? (3) What is the typical trajectory of conflict during the first year of treatment, and to what degree are there differences across families in that trajectory? Based on previous research, we hypothesized that couples would show a decline in marital satisfaction over the first year of treatment with considerable variability in the pattern between couples. No a priori hypotheses about percent or level of marital distress were proposed as there is little data to support specific predictions. Based on Ishibashi (2001), we also hypothesized that parent-child conflict would be relatively elevated at diagnosis and decrease over the first year of treatment, with considerable variability between dyads. Based on Marine & Miller (1998), we hypothesized that sibling conflict would be stable over time and would show average levels comparable to healthy sibling dyads, although variability in the pattern between sibling dyads was expected.
Method
Participants
One hundred and fifty-nine families participated in the present study. Children were ages 2–18 (M = 6.3 years, SD = 3.5 years, 49% male) and had been recently newly diagnosed with cancer or a CNS tumor. While the majority of the sample was children ages 2–10, 19 adolescents were also included. The majority of children with cancer were identified as White/Caucasian (84.1%), with the remaining identified as Black/African-American (5.6%), Asian (0.8%), American Indian (0.8%), or other (8.8%). 15.1% of participants identified as ethnically Hispanic. Most families identified the primary caregiver as the mother (85.5%) and the secondary caregiver as the father (77.0%). Most caregivers were married (78.3%). See Table 1 for child diagnosis, treatment intensity and additional demographic information.
Table 1.
Sample Demographic Information
| n | % of Sample | ||
|---|---|---|---|
| Primary Caregiver | |||
|
| |||
| Relationship to Child | Mother | 146 | 85.3 |
| Father | 19 | 11.1 | |
| Grandmother | 3 | 1.8 | |
| Other | 3 | 1.8 | |
| Race | White/Caucasian | 128 | 88.9 |
| African-American | 7 | 4.9 | |
| Asian | 4 | 2.8 | |
| Other | 5 | 3.4 | |
| Ethnicity | Hispanic | 13 | 9 |
| Not Hispanic | 131 | 91 | |
| Highest Education | No High School Diploma | 4 | 2.7 |
| High School Diploma | 35 | 23.8 | |
| College | 90 | 61.3 | |
| Graduate or Professional | 18 | 12.2 | |
|
| |||
| Family Information | |||
|
| |||
| Annual Income | Under $10,000 | 4 | 2.9 |
| $10,000–$49,000 | 50 | 36.8 | |
| $50,000–$99,000 | 46 | 33.8 | |
| $100,000–$150,000 | 24 | 17.6 | |
| $150,000 + | 12 | 8.9 | |
| Average Number of Children in Family (SD) | 2.4 (0.91) | ||
|
| |||
| Disease Information | |||
|
| |||
| Diagnosis | Leukemia | 58 | 36.5 |
| Lymphoma | 17 | 10.7 | |
| Sarcoma | 17 | 10.7 | |
| Wilm’s Tumor | 13 | 8.2 | |
| Neuroblastoma | 6 | 3.8 | |
| Other | 13 | 8.2 | |
| CNS Tumor | 35 | 22.0 | |
| Relapsed on Study | 2 | 1.3 | |
| Treatment Intensity | Level 1: Least Intensive | 9 | 5.7 |
| Level 2: Mod. Intensive | 57 | 35.8 | |
| Level 3: Very Intensive | 81 | 50.9 | |
| Level 4: Most Intensive | 12 | 7.5 | |
Note. Treatment intensity ratings based on Intensity of Treatment Rating (ITR-3; Kazak, 2011).
Procedure
Participants were recruited from two children’s hospitals in urban areas, and were approached within two weeks following the child’s diagnosis. Families were considered eligible if they had a child newly diagnosed with a tumor or cancer who was 2–18 years old at the time of diagnosis, English-speaking, and had no history of developmental delay. Current caregivers also needed to be the same caregiver as prior to the child’s diagnosis. Children with NF1, relapsed cancer, or secondary malignancies were not eligible. All study procedures were approved by the Institutional Review Boards at all participating institutions (University of Washington; Vanderbilt University).
Families were initially approached by their physician or nurse, and interested families were then approached by a member of the research team and consent and HIPAA authorization were obtained. Of the 502 families eligible for participation across both sites, 309 were approached, 176 enrolled, with 159 completing at least one study component. Of the families approached who did not enroll, refusal was due to either excessive time required or no reason was given. Informed consent was obtained from primary caregivers at the time of enrollment. Data were collected over a twelve-month period beginning with an initial questionnaire packet for each caregiver distributed at the time of consent, followed by monthly questionnaire packets distributed through the mail. If a completed questionnaire packet was not received by the study team within the two-week window for that time point, the packet was skipped and the next month’s packet was sent. Primary caregivers completed packets at each time point for a total of 12 packets. On average, primary caregivers completed 6.8 packets. Secondary caregivers completed packets at Month 1, Month 6 and Month 12, for a total of 3 packets. On average, secondary caregivers completed 2.1 packets. Overall, 89% of primary caregivers and 61.3% of secondary caregivers completed at least one packet. After the initial questionnaire, the highest percentage of primary caregivers were retained at Month 6 (67.5%) and the lowest at Month 2 (5%). Number of completed packets was not correlated with any demographic variables, including child age, gender, diagnosis, or ethnicity, or caregiver age, education or marital status.
Additionally, an in-person visit was conducted within the first 3 months following diagnosis during which physiological and observational data were collected from family members. Families exhibiting considerable distress during observations were approached by study PIs for follow-up and referral as needed. For the present study, data from the primary caregiver’s report of marital adjustment, parent-child conflict and sibling conflict across the first year of treatment were used for all analyses.
Measures
Treatment intensity
The Intensity of Treatment Rating (ITR-3; Kazak et al., 2012) was used to assess treatment intensity of children with cancer. Intensity ratings ranged from 1 (least intensive) – 4 (most intensive) based on diagnosis, stage or risk level, and number of treatment modalities. Data was abstracted from medical records by a research assistant.
Marital adjustment
The Dyadic Adjustment Scale (DAS; Spanier, 1976) was used to assess marital adjustment via primary caregiver report. The DAS is a well-validated 35-item self-report questionnaire used to assess inter-adult adjustment and conflict via assessing dyadic consensus, dyadic satisfaction, affectional expression, and dyadic cohesion. The DAS yields an Overall Dyadic Adjustment score, computed as a sum of all items, with higher scores indicating better adjustment. Wood, Crane, and Law (2005) established ranges for mildly distressed (96–107), moderately distressed (80–95.9), and severely distressed (<80) couples. Cronbach’s alpha in our sample ranged from .91–.97, with an average of .96 across the twelve time points.
Parent-child conflict
The conflict subscale of the Parenting Questionnaire (Fauchier & Margolin, 2004) was used to assess parent-child conflict between caregivers and the child with cancer via primary caregiver report. Six items such as “my child and I disagree and quarrel” were rated on a 5-point scale. A total conflict score was computed as a sum of the six items, with higher scores indicating greater conflict. Because there are no established norms for a distressed range on this questionnaire, we operationalized “distressed” as those who scored above one standard deviation above the mean at each time point. One standard deviation was used as it is the standard cutoff for relationship distress in other types of relationships (e.g., marital distress). Concurrent validity has been demonstrated by Fauchier and Margolin (2004). In our sample, Cronbach’s alpha ranged from .70–.82, with an average of .77 across the twelve time points.
Sibling conflict
Sibling conflict was measured via primary caregiver report using the conflict subscale of the Sibling Relationship Questionnaire (SRQ; Furman & Buhrmester, 1985). Nine items assessed total frequency of sibling conflict in the past month, with 3 items each assessing sibling antagonism, competition, and quarrelling. Higher scores indicated greater frequency of conflict. As with the measure of parent-child conflict, there are no established norms for a distressed range on the SRQ and we operationalized “distressed” as those who scored above one standard deviation above the mean at each time point. In families with two or more siblings, primary caregivers were instructed to complete the questionnaire thinking about the target child’s relationship with siblings in general. In terms of reliability and validity, longitudinal measurement invariance has been demonstrated for the SRQ (Derkman et al., 2015) and in our sample Cronbach’s alpha ranged from .91 – .99 with an average of .95 across the twelve times points.
Data Analytic Strategy
To address the hypotheses related to mean levels and proportion of the sample in the “distressed” range at each time point, we initially calculated descriptive information for 12 monthly time points over the first year of treatment. As mentioned above, for marital adjustment, cut-offs developed by Wood, Crane, and Law (2005) were used to categorize mild, moderate, and severe distress. For parent-child and sibling conflict, we operationalized “distressed” as one standard deviation above the mean at each time point. Due to concern regarding potential non-random missing data at each time point, we used Multiple Imputation in SPSS 19.0 to estimate missing data for all constructs at each time point. Final estimates were pooled estimates from 20 imputed data sets. However, because so few families (n = 7, or 4.5% of families) were able to complete the Time 2 follow up, we did not trust that the imputation results of Time 2 accurately reflected the missing data. Indeed, the bounds and distribution of the data that were imputed data at Time 2 were substantially different than the distributions of the data at all other time points. Thus, for re-analysis with the imputed data, Time 2 was removed from all analyses resulting in 11 time points (i.e., Month 1, Month 3-Month 12).
To address hypotheses related to change over time, we estimated growth curve models in a Multilevel Modeling (MLM) approach, using the Maximum Likelihood estimator (ML) in SPSS 18.0. Eleven time points were used to estimate growth models. Multilevel models are a useful tool for examining non-independent data such as repeated measures nested within individuals. Multilevel models are also able to assess both within and between cluster effects simultaneously (Raudenbush & Bryk, 2002), in this case modeling both within-family trajectories of conflict as well as between-family differences in trajectories of conflict over time.
Modeling proceeded as follows: We first estimated an unconditional growth model with time estimated as a linear function. This model estimated an intercept parameter, representing the starting point of the family conflict variable (i.e. the baseline assessment), as well as a linear time parameter, which represents the rate of linear change over time in family conflict and the direction of such change (i.e., increase or decrease in conflict over the first year of treatment). Thus, time was coded from 0, Baseline to 10, representing the 11 month follow up. In addition to intercept and time parameters, we then tested whether estimating random effects for these parameters improved model fit using −2LL differences to test whether including these random effects improved model fit (Raudenbush & Bryk, 2002). Random effects test whether there were between-family differences in the initial levels or rate of change in conflict. Significant random effects suggest that there was sufficient variance in the growth parameters between families to recommend that future studies test potential predictors that may account for these within family differences in conflict over time. Finally, we tested whether adding a quadratic effect improved model fit, which tested whether the rate of change increased or decreased over time.
Results
Table 2 presents descriptive information including means, standard deviations, and proportion of the sample in the distressed range for all constructs at each time point. Number of distressed families at each time point was calculated as the percentage of families that fell in the distressed range relative to the total number of respondents at that time point. Given the wide age range of the sample, all analyses were run with and without inclusion of the 19 families with adolescents. There were no substantial differences in the pattern of results across family subsystems, and so results on the full sample was reported.
Table 2.
Descriptive Information
| Time | T1 | T3 | T4 | T5 | T6 | T7 | T8 | T9 | T10 | T11 | T12 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Marital Adjustment (n = 153) | |||||||||||
|
| |||||||||||
| Mean | 119.7 | 116.2 | 118.8 | 121.7 | 115.3 | 121.2 | 122.0 | 123.1 | 120.7 | 121.8 | 122.0 |
| SD | 23.5 | 39.0 | 25.2 | 24.9 | 28.5 | 33.3 | 29.3 | 34.1 | 30.2 | 32.1 | 27.4 |
| % Mild Distress | 15.0% | 15.0% | 13.0% | 11.8% | 10.4% | 7.8% | 10.4% | 9.2% | 11.1% | 9.2% | 9.2% |
| % Mod. Distress | 4.5% | 10.5% | 7.2% | 7.8% | 7.6% | 9.2% | 9.2% | 6.5% | 11.1% | 9.8% | 10.5% |
| % Sev. Distress | 6.5% | 16.3% | 7.8% | 5.9% | 11.8% | 4.2% | 9.1% | 9.1% | 7.8% | 8.5% | 6.5% |
| % Total Distress | 26.1% | 36.6% | 28.1% | 25.5% | 35.3% | 28.8% | 28.8% | 24.8% | 30.1% | 27.5% | 26.1% |
|
| |||||||||||
| Parent-Child Conflict (n = 153) | |||||||||||
|
| |||||||||||
| Mean | 8.8 | 9.6 | 9.1 | 9.2 | 9.4 | 9.3 | 9.0 | 8.6 | 8.8 | 9.1 | 8.9 |
| SD | 3.0 | 4.1 | 2.7 | 3.0 | 3.1 | 4.0 | 3.0 | 2.7 | 2.8 | 3.4 | 3.3 |
| % ≥ 1 SD | 12.4% | 13.7% | 15.6% | 13.1% | 16.3% | 12.4% | 14.4% | 15.0% | 19.0% | 18.3% | 14.4% |
|
| |||||||||||
| Sibling Conflict (n = 129) | |||||||||||
|
| |||||||||||
| Mean | 2.3 | 2.3 | 2.3 | 2.3 | 2.3 | 2.3 | 3.3 | 2.4 | 2.5 | 1.9 | 2.4 |
| SD | .96 | 2.1 | 1.1 | .93 | .97 | 1.1 | 1.1 | 1.6 | 1.5 | .69 | 1.1 |
| % ≥ 1 SD | 13.6% | 11.8% | 17.4% | 15.7% | 18.7% | 14.7% | 3.9% | 13.7% | 15.9% | 18.8% | 14.9% |
Note. Means, standard deviations, and distressed percentages are based on pooled estimates from 20 imputed data sets to account for missing data.T2 excluded due to substantial missing data (see Method). For marital adjustment, higher scores indicate better adjustment. For parent-child and sibling conflict, higher scores indicate higher conflict.
Marital Adjustment
Average Levels of Marital Adjustment
Based on observed mean levels, marital adjustment ranged from 116.9 to 123.1, which is in the happily married range. The lowest mean level of marital adjustment was at Month 3 (M = 116.2, SD = 39.0) followed by Month 4 (M = 118.8, SD = 25.2). The maximum change in means between subsequent measurements was a 6.4-point decrease between Month 5 and Months 6.
Proportion of Families in Distressed Range on Marital Adjustment
In our sample, more couples fell in one of the distressed ranges (mild, moderate, or severe) at Month 3 (36.6%) and Month 6 (35.3%) than at other time points, with the fewest couples falling in any distressed range at Month 9 (24.8%). On average, more couples were mildly distressed at any time point than moderately or severely distressed. The proportion of the sample that was either in the mild, moderate or severely distressed ranges differed by a maximum of 11.8% between time points. Additionally, the greatest number of couples in any distressed category at any time point occurred for severely distressed couples during Month 3 (16.3%) and mildly distressed couples during Month 1 (15.0%) and Month 3 (15.0%).
Trajectory of Marital Adjustment
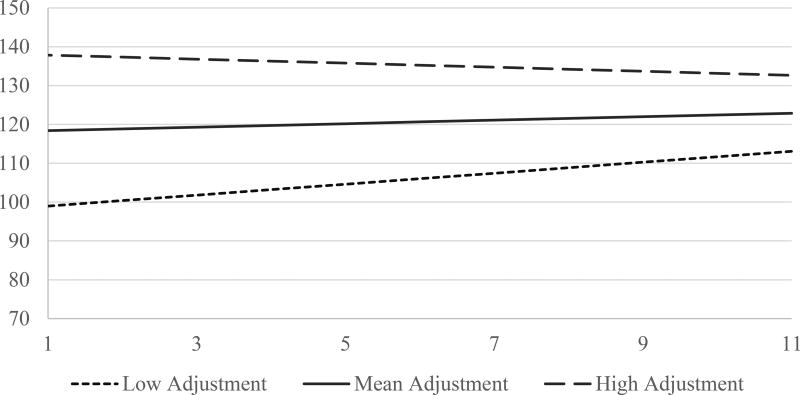
The final growth model suggested that marital adjustment was on average stable during the first year of treatment, though substantial variability existed between families. A fully random linear growth model best fit the data, and improved fit criteria compared to the fully fixed and random intercept models (see Table 3 for fit indices). On average, families’ initial level of marital adjustment was 117.98 (SE =2.75, p < .001) and no linear effect of time was found. Variance estimates in the final model suggested that variability existed between families in both intercept (σ2 = 426.5, SE = 143.1) and linear slope (σ2 = 1.40, SE = 0.18). In other words, 68.2% of families would be expected to range between 97.38 to 138.6 in their initial levels of marital adjustment, and range between −0.73 and 1.63 in their rate of change. To visualize this variability, we plotted the model implied trajectory for families who were high, at the mean, and low on initial adjustment levels based on the correlation between the intercept and linear slope (r = −0.50). As Figure 1 depicts, families who started low in marital adjustment were expected to increase over time while families who started high in marital adjustment were expected to decrease slightly, suggesting a pattern of convergence to the mean.
Table 3.
Model Fit Indices and Comparisons
| −2 RLL | # of parameters | Δ in χ2 | p | |
|---|---|---|---|---|
| Marital Adjustment | ||||
|
| ||||
| Fully Fixed | 16230.3 | 3 | ||
| Random Intercept | 15908.1 | 4 | 322.2 | < .001 |
| Random Intercept & Slope | 15870.8 | 6 | 37.3 | < .001 |
|
| ||||
| Parent-Child Conflict | ||||
|
| ||||
| Fully Fixed | 8753.4 | 3 | ||
| Random Intercept | 8256.3 | 4 | 497.1 | < .001 |
| Random Intercept & Slope | 8199.9 | 6 | 56.4 | < .001 |
|
| ||||
| Sibling Conflict | ||||
|
| ||||
| Fully Fixed | 5585.6 | 3 | ||
| Random Intercept | 5254.6 | 4 | 330.0 | < .001 |
| Random Intercept & Slope | 5228.5 | 6 | 26.1 | < .001 |
Note. RLL = Restricted Log Likelihood.
Figure 1.
Model implied trajectories of marital adjustment based on correlation between intercept and linear slope variability estimates. Low adjustment = −1 SD; high adjustment = +1 SD.
Parent-Child Conflict
Average Levels of Parent-Child Conflict
Parent-child conflict ranged from 8.6–9.6, which corresponds with a low to average level on a scale ranging from 0 to 30. The highest mean level of conflict was at Months 3 (M = 9.6, SD = 4.1), and the maximum change in means between subsequent measurements was a 0.8-point difference between Month 1 and Month 3.
Proportion of Families in Distressed Range on Parent-Child Conflict
More families tended to fall in the distressed range in parent-child conflict during Month 10 (19%) and Month 11 (18.3%) than at other time points, with the least number of families reporting distress during Month 1 (12.4%) and Month 7 (12.4%).
Typical Trajectory of Parent-Child Conflict
Akin to marital adjustment, the final growth model suggested that parent-child conflict was on average stable during the first year of treatment, though substantial variability existed between families. A fully random linear model best fit the data, and improved fit criteria compared to the fully fixed and random intercept models (see Table 3 for fit indices). This model suggested that on average initial level of parent-child conflict was 9.24 (SE = 0.29, p < .001) and there was no effect of time. However, variance estimates in the final model suggested that there was variability between families in both intercept (σ2 = 6.03, SE = 1.89) and linear slope (σ2 = 0.06, SE = 0.03). In other words, 68.2% of families would be expected to range between 6.79 and 11.69 in their initial levels of parent-child conflict, and range between −.28 and .20 in their rate of change, suggesting that some families showed increases Month 1 to Month 12, and other families showed declines (e.g., see Figure 1 for marital adjustment).
Sibling Conflict
Average Levels of Sibling Conflict
Sibling conflict ranged from 1.9–2.5, which corresponds with an average level on a scale ranging from 0 to 5. The maximum change in means between subsequent measurements was a 0.6 difference between Month 10 and Month 11.
Proportion of Families in Distressed Range on Sibling Conflict
More families tended to fall in the distressed range in sibling conflict during Month 11 (18.8%) and Month 6 (18.7%) than at any other time point. The fewest families fell in this range during Month 8 (3.9%).
Typical Trajectory of Sibling Conflict
The final growth model suggested that sibling conflict was stable on average during the first year of treatment, though substantial variability existed between families. A fully random linear model best fit the data. This model suggested that on average, initial level of sibling conflict was 2.27 (SE = .11, p < .001) and there was no effect of time. Variance estimates in the final model suggested that variability existed between families in the intercept (σ2 = .79, SE = 0.29) and linear slope (σ2 = .004, SE = 0.003). In other words, 68.2% of families would be expected to range from 1.38 to 3.16 in their initial levels of sibling conflict, and from −.06 to .06 in their rate of change.
Discussion
Using a prospective longitudinal design with monthly assessments, the present study described the average levels and trajectories of family relationships during the first year of treatment for pediatric cancer. Marital adjustment, parent-child conflict and sibling conflict remained relatively stable across all families, suggesting that most families are able to weather the storm and maintain reasonably good relationships among family members even in the face of the significant stresses associated with the diagnosis and treatment of pediatric cancer.
Couples in our sample were generally happily married, with scores comparable to samples of married couples (Crane et al., 1990; Spanier, 1976) and parents of chronically-ill children (Dahlquist et al., 1996; Walker, Manion, Cloutier & Johnson, 1992). At the same time, 25–36% of couples fell into the maritally distressed ranges at any given time point. Since the operational definition of marital distress is scoring 1 standard deviation above the norm on a measure of marital satisfaction, the probability in the general population that any one individual in a couple will report marital distress is 15.9% (Gottman, personal communication, 12/12/16). A greater proportion of our sample is showing marital distress compared to national averages at each time point, although the degree to which they show increased rates varies across time. Although previous studies have reported on changes in marital satisfaction over the course of treatment for pediatric cancer, to our knowledge this is the first study to report on the degree to which couples are experiencing clinical levels of marital distress in the first year of treatment. These data suggest that a sizable subset of couples (26–36%) experience mild, moderate or severe marital distress at some point in the first year of treatment, though overall more couples report mild and moderate than severe distress. Notably, however, the proportion of couples with mild, moderate, and severe distress were all elevated at Month 3 (36.6%), with 16% of couples scoring in the severe range. Assuming that marital adjustment is normally distributed, this is a much larger proportion that would be expected in the broader population. The first two months of diagnosis is a particularly stressful time when families are making treatment-related decisions, changing roles and responsibilities, and mobilizing resources to focus on the child’s well-being. It may take some time for this early stress to exert a negative impact on the marital relationship, and our data suggest that by Month 3 some strain to the marriage emerges. Taken together, these findings suggest that while on average couples do not report substantial marital distress during their child’s cancer treatment, a substantial subset experience marital distress. More families are reporting some level of marital distress than would be expected in the general population, thus therapeutic intervention may beneficial for some families, particularly in the early months post-diagnosis when stress may be the highest.
Another area of family relationships examined is the degree of conflict between the child with cancer and their primary caregiver. Overall, the amount of reported parent-child conflict was low, suggesting that for most families the unique stresses involved in the cancer experience do not spillover and result in higher conflict in the parent-child relationship. However, a greater percentage of families fell in the distressed range for parent-child conflict in the later months of first year of treatment than in earlier months. These results suggest that while parent-child conflict is generally low over the first 12 months of diagnosis and treatment, it may increase for a significant subset of families a few months after diagnosis. Parents may be reluctant to engage in conflict with the child with cancer soon after diagnosis because they are trying to protect their child (Thomasgard & Metz, 1993), but as the family adapts to the diagnosis and treatment over time they are more likely to revert back to their typical patterns of interaction.
The third family relationship examined was sibling conflict. Overall, the amount of reported sibling conflict was low and, consistent with Marine and Miller (1998), is comparable to studies of typically developing children. This suggest that for most families the cancer experience does not result in higher conflict in the sibling relationship. At the same time, the highest subset of families that fell into the distressed range on sibling conflict occurred at months 6 and 11 (19%), which is higher than would be expected in the broader population based on a normal distribution (i.e., 15.9%). Therefore, sibling conflict may be elevated for some families during treatment.
Taken together, these results suggest that for most families the first year of diagnosis and treatment does not result in significant detrimental effects on the quality of family relationships. Key periods for increases in conflict were also observed. For couples, the most difficult time periods were the first six months post-diagnosis. The largest number of couples fell into the mild, moderate or severely distressed range during Month 3. This is consistent with Fife et al (1987) who reported that the sharpest decline in marital satisfaction occurred approximately four months following diagnosis. For siblings, the most difficult time periods were at Months 6 and 11. For parent-child dyads, later months were higher risk periods. Inspection of means indicates that the greatest number of families fell into the distressed range in parent-child conflict during Months 9 and 10. It is interesting that marital distress occurs first while parent-child and sibling conflict increase later in the first year of treatment. It is possible that when a child is diagnosed with cancer, the stress placed on the family affects the marriage more rapidly than in other dyads, as couples must confront issues such as treatment decisions and reorganization of family roles in the initial months after diagnosis. Issues that come up early in the treatment process, such as treatment decisions, how to manage changing family needs, and involvement of grandparents or other caregivers can result in conflict and tax the couple’s relationship. In contrast, parent-child dyads may be less likely to show conflict soon after diagnosis, as parents may be reluctant to engage in conflict with the child with cancer. Likewise, siblings may be initially reluctant to engage in conflict with the ill-child as they feel concern for their sibling’s well-being, though over time may begin to sense differential treatment or frustration with changes in the family leading to eventual elevations in conflict. Over time parent-child and sibling conflict may also be more likely to rise as a result of continuous stress on the family.
Another possibility is that over time there may be spillover from marital distress to other family subsystems. Family researchers have suggested that there can be a transfer of mood, affect or behavior from one sub-system (e.g., the marital dyad) to another sub-system (e.g., the parent-child dyad; Erel & Burman, 1995). When children are diagnosed with cancer, it may be that marital difficulties in the early part of diagnosis and treatment process results in a cascading process of distress in other family sub-systems such as the parent-child. Further research on the temporal relationship between marital, parent-child and sibling relationship quality in families of children with cancer will be important to test this hypothesis. To the extent that a spillover effect is operating, prevention and intervention efforts focused on strengthening the marital dyad can have positive cascading effects on other family subsystems.
While on average there is relative stability in marital, parent-child and sibling conflict, there was also substantial variability in all three family subsystems indicating that there are individual differences in how family relationships change through the first year of treatment. For example, while on average initial marital adjustment is in the happily married range and couples show stability in marital adjustment over time, intercept variability estimates suggested a substantial range for initial starting points (e.g., 97.38–138.6 for couples within +/− 1 SD of the sample mean), many of which would fall within the distressed range (<107). Similarly, while there was no average effect of time for sibling conflict, an examination of variability estimates suggest that this is likely because some families are declining while others are increasing over the first year of treatment. Thus, examining average trajectories of family relationships without considering variability occludes our understanding of the pattern of conflict across families. Further research is needed to understand the factors that predict differential trajectories of marital, parent-child and sibling conflict over the first year of treatment to identify at risk families (Kazak, 1989).
The study had several strengths as well as limitations. One limitation is that it may be difficult for parents of children with cancer to acknowledge having conflict with a child undergoing treatment. As overall levels of parent-child conflict were low, it is possible that parents may be minimizing the conflict they are having with their child. Assessing the degree to which parent report of parent-child conflict maps on to observational assessments of parent-child interaction can help disentangle the degree to which desirability effects are operating. Another limitation is the varied response rates at each time point. While multiple imputation was used to account for missing data in all analyses, examining patterns of missing data may have implications for study design and feasibility. Notably, due to very low response rate at Month 2, there was not enough data available to use multiple imputation at this time point, and it was therefore dropped from the current study. Thus, future studies should consider feasibility of collecting monthly data during treatment, and particularly close to diagnosis when families are experiencing high levels of stress and making important treatment decisions. All measures were completed by the primary caregiver, in this case mostly mothers, so our results only reflect a single perspective of each family subsystem. Future studies may benefit from including the child’s perspectives on family functioning, as results may differ as a function of the respondent. In addition, measures of parent-child and sibling conflict do not have established clinical cutoffs for distress so it is unclear whether using a single standard deviation above the mean accurately captures family distress and may in fact lead to an overestimation of distress. Finally, given that our sample was primarily white, middle-class, and educated, generalizability of findings may be limited. For example, given that financial strain associated with childhood cancer is a substantial issue for many families (Bona et al., 2015) and is associated with higher family conflict (Wadsworth & Compas, 2002), lower SES families may be exhibit higher rates of conflict compared to families in the current study. Findings from the current study should be considered in light of these limitations, as experiences and perspectives of subgroups of families may differ from our sample.
Strengths of the study include the monthly assessments of family relationship quality, which allowed for a novel and nuanced description of changes in family relationships over the first year of treatment. To our knowledge, this is the first study in this area to use growth models to examine trajectories of family relationships rather than auto-regressive models. This method addresses methodological limitations in the current literature by allowing us to glean information about both average levels of change in conflict, as well as how families differ from one another over time. Use of a well-validated measure of marital quality with clear clinical-cutoffs also allowed us to determine the number of families showing clinically significant difficulties.
This study provides a rich description of family relationships during the first year of pediatric cancer treatment. Our findings suggest that most families are able to maintain reasonably good relationships among family members during the first year of treatment. At the same time, 25–36% of couples, and up to 19% of parent-child and sibling dyads are showing either distress or higher than average levels of conflict at any given point during the treatment process. Of those families showing distress, the earlier months post-diagnosis are a higher risk period for difficulties in marital adjustment, and later months pose a greater risk for sibling and parent-child conflict. Importantly, substantial individual differences in the trajectories of family conflict were observed, suggesting that some families are negatively impacted by the cancer experience over time. Research building on this work should focus on identifying temporal relations between changes in marital adjustment and subsequent parent-child or sibling conflict, as well as determining factors that predict variability in trajectories of conflict.
Acknowledgments
This research was supported by grant R01-CA134794 from the National Cancer Institute to the first author
References
- Alderfer MA, Long KA, Lown EA, Marsland AL, Ostrowski NL, Hock JM, Ewing LJ. Psychosocial adjustment of siblings of children with cancer: a systematic review. Psycho-Oncology. 2010;19(8):789–805. doi: 10.1002/pon.1638. [DOI] [PubMed] [Google Scholar]
- Bollen KA, Curran PJ. Latent curve models: A structural equation perspective. Vol. 467. John Wiley & Sons; 2006. [Google Scholar]
- Bona K, London WB, Guo D, Abel G, Lehmann L, Wolfe J. Prevalence and impact of financial hardship among New England pediatric stem cell transplantation families. Biology of Blood and Marrow Transplantation. 2015;21(2):312–318. doi: 10.1016/j.bbmt.2014.10.016. [DOI] [PubMed] [Google Scholar]
- Breyer J, Kunin H, Kalish LA, Patenaude AF. The adjustment of siblings of pediatric cancer patients—a sibling and parent perspective. Psycho-Oncology. 1993;2(3):201–208. doi: 10.1002/pon.2960020306. [DOI] [Google Scholar]
- Burns W, Péloquin K, Sultan S, Moghrabi A, Marcoux S, Krajinovic M, Robaey P. A 2-year dyadic longitudinal study of mothers' and fathers' marital adjustment when caring for a child with cancer. Psycho-Oncology. 2016 doi: 10.1002/pon.4189. [DOI] [PubMed] [Google Scholar]
- Crane DR, Allgood SM, Larson JH, Griffin W. Assessing marital quality with distressed and nondistressed couples: A comparison and equivalency table for three frequently used measures. Journal of Marriage and the Family. 1990:87–93. [Google Scholar]
- Cummings EM, Davies P, Campbell SB. Developmental psychopathology and family process: Research, theory, and clinical implications. New York: Guilford; 2000. [Google Scholar]
- Dahlquist LM, Czyzewski DI, Jones CL. Parents of children with cancer: A longitudinal study of emotional distress, coping style, and marital adjustment two and twenty months after diagnosis. Journal of pediatric psychology. 1996;21(4):541–554. doi: 10.1093/jpepsy/21.4.541. [DOI] [PubMed] [Google Scholar]
- Dahlquist L, Dahlquist L, Czyzewski D, Copeland K, Jones C, Taub E, Vaughan J. Parents of children newly diagnosed with cancer: Anxiety, coping, and marital distress. Journal of Pediatric Psychology. 1993;18(3):365–376. doi: 10.1093/jpepsy/18.3.365. [DOI] [PubMed] [Google Scholar]
- Decker CL. Social support and adolescent cancer survivors: A review of the literature. Psycho-Oncology. 2007;16(1):1–11. doi: 10.1002/pon.1073. [DOI] [PubMed] [Google Scholar]
- Derkman MMS, Scholte RHJ, Van Der Veld WM, Engels RCME. Factorial and construct validity of the Sibling Relationship Questionnaire. European Journal of Psychological Assessment. 2010;26(4):277–283. doi: 10.1027/1015-5759/a000037. [DOI] [Google Scholar]
- Erel O, Burman B. Interrelatedness of marital relations and parent-child relations: A meta-analytic review. Psychological Bulletin. 1995;118(1):108–132. doi: 10.1037/0033-2909.118.1.108. [DOI] [PubMed] [Google Scholar]
- Fauchier A, Margolin A. Affection and conflict in marital and parent-child relationships. Journal of Marital and Family Therapy. 2004;30(2):197–211. doi: 10.1111/j.1752-0606.2004.tb01234.x. [DOI] [PubMed] [Google Scholar]
- Fife BJ, Norton G, Groom The family's adaptation to childhood leukemia. Social Science & Medicine. 1987;24(2):159–168. doi: 10.1016/0277-9536(87)90248-6. [DOI] [PubMed] [Google Scholar]
- Grant S, Carlsen K, Bidstrup PE, Bastian GS, Lund LW, Dalton SO, Johansen C. Parental separation and pediatric cancer: A Danish cohort study. Pediatrics. 2012;129(5):e1187–e1191. doi: 10.1542/peds.2011-2657. [DOI] [PubMed] [Google Scholar]
- Gottman JM, Katz LF. Effects of marital discord on young children's peer interaction and health. Developmental psychology. 1989;25(3):373–381. doi: 10.1037/0012-1649.25.3.373. [DOI] [Google Scholar]
- Ishibashi A. The needs of children and adolescents with cancer for information and social support. Cancer nursing. 2001;24(1):61–67. doi: 10.1097/00002820-200102000-00010. [DOI] [PubMed] [Google Scholar]
- Kazak AE. Families of chronically ill children: a systems and social-ecological model of adaptation and challenge. Journal of consulting and clinical psychology. 1989;57(1):25. doi: 10.1037//0022-006x.57.1.25. [DOI] [PubMed] [Google Scholar]
- Kazak AE, Hocking MC, Ittenbach RF, Meadows AT, Hobbie W, DeRosa BW, Reilly A. A revision of the intensity of treatment rating scale: classifying the intensity of pediatric cancer treatment. Pediatric blood & cancer. 2012;59(1):96–99. doi: 10.1002/pbc.23320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labay LE, Walco GA. Brief report: empathy and psychological adjustment in siblings of children with cancer. Journal of Pediatric Psychology. 2004;29(4):309–314. doi: 10.1093/jpepsy/jsh032. [DOI] [PubMed] [Google Scholar]
- Larson LS, Wittrock DA, Sandgren AK. When a child is diagnosed with cancer: I. Sex differences in parental adjustment. Journal of Psychosocial Oncology. 1994;12(1–2):123–142. [Google Scholar]
- Lavee Y. Correlates of change in marital relationships under stress: The case of childhood cancer. Families in Society: The Journal of Contemporary Social Services. 2005;86(1):112–120. [Google Scholar]
- Leventhal-Belfer L, Bakker AM, Russo CL. Parents of childhood cancer survivors: A descriptive look at their concerns and needs. Journal of psychosocial oncology. 1993;11(2):19–41. doi: 10.1300/J077V11N02_02. [DOI] [Google Scholar]
- Lewin AB, Heidgerken AD, Geffken GR, Williams LB, Storch EA, Gelfand KM, Silverstein JH. The relation between family factors and metabolic control: the role of diabetes adherence. Journal of Pediatric Psychology. 2006;31(2):174–183. doi: 10.1093/jpepsy/jsj004. [DOI] [PubMed] [Google Scholar]
- Long KA, Marsland AL. Family adjustment to childhood cancer: a systematic review. Clinical child and family psychology review. 2011;14(1):57–88. doi: 10.1007/s10567-010-0082-z. [DOI] [PubMed] [Google Scholar]
- Marine S, Miller D. Social support, social conflict, and adjustment among adolescents with cancer. Journal of Pediatric Psychology. 1998;23(2):121–130. doi: 10.1093/jpepsy/23.2.121. [DOI] [PubMed] [Google Scholar]
- McHale SM, Crouter AC, McGuire SA, Updegraff KA. Congruence between Mothers' and Fathers' Differential Treatment of Siblings: Links with Family Relations and Children's Well-Being. Child Development. 1995;66(1):116–128. doi: 10.1111/j.1467-8624.1995.tb00859.x. [DOI] [PubMed] [Google Scholar]
- Miller-Johnson S, Emery RE, Marvin RS, Clarke W, Lovinger R, Martin M. Parent-child relationships and the management of insulin-dependent diabetes mellitus. Journal of consulting and clinical psychology. 1994;62(3):603. doi: 10.1037//0022-006x.62.3.603. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. Vol. 1. Sage; 2002. [Google Scholar]
- Riley AW, Finney JW, Mellits ED, Starfield B, Kidwell S, Quaskey S, Shematek JP. Determinants of children's health care use: an investigation of psychosocial factors. Medical care. 1993:767–783. doi: 10.1097/00005650-199309000-00002. [DOI] [PubMed] [Google Scholar]
- Rutter M. Family and school influences on behavioural development. Journal of Child Psychology and Psychiatry. 1985;26(3):349–368. doi: 10.1111/j.1469-7610.1985.tb01938.x. [DOI] [PubMed] [Google Scholar]
- Spanier GB. Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. Journal of Marriage and the Family. 1976:15–28. [Google Scholar]
- Straus MA, Hamby SL, Finkelhor D, Moore DW, Runyan D. Identification of child maltreatment with the Parent-Child Conflict Tactics Scales: Development and psychometric data for a national sample of American parents. Child abuse & neglect. 1998;22(4):249–270. doi: 10.1016/s0145-2134(97)00174-9. doi: 0.1016/S0145-2134(97)00174-9. [DOI] [PubMed] [Google Scholar]
- Syse A, Loge J, Lyngstad T. Does childhood cancer affect parental divorce rates? A population-based study. Journal of Clinical Oncology Official Journal of the American Society of Clinical Oncology. 2010;28(5):872–877. doi: 10.1200/JCO.2009.24.0556. [DOI] [PubMed] [Google Scholar]
- Thomasgard M, Metz WP. Parental overprotection revisited. Child Psychiatry and Human Development. 1993;24(2):67–80. doi: 10.1007/BF02367260. [DOI] [PubMed] [Google Scholar]
- Wadsworth ME, Compas BE. Coping with family conflict and economic strain: The adolescent perspective. Journal of Research on Adolescence. 2002;12(2):243–274. [Google Scholar]
- Wasserman AL, Thompson EI, Wilimas JA, Fairclough DL. The psychological status of survivors of childhood/adolescent Hodgkin's disease. American Journal of Diseases of Children. 1987;141(6):626–631. doi: 10.1001/archpedi.1987.04460060044029. [DOI] [PubMed] [Google Scholar]
- Wijnberg-Williams BJ, Van de Wiel H, Kamps W, Hoekstra-Weebers JE. Effects of communication styles on marital satisfaction and distress of parents of pediatric cancer patients: a prospective longitudinal study. Psycho-Oncology. 2015;24(1):106–112. doi: 10.1002/pon.3617. [DOI] [PubMed] [Google Scholar]
- Wilkins KL, Woodgate RL. A review of qualitative research on the childhood cancer experience from the perspective of siblings: a need to give them a voice. Journal of Pediatric Oncology Nursing. 2005;22(6):305–319. doi: 10.1177/1043454205278035. [DOI] [PubMed] [Google Scholar]
- Wood ND, Crane DR, Schaalje GB, Law DD. What works for whom: A meta-analytic review of marital and couples therapy in reference to marital distress. The American Journal of Family Therapy. 2005;33(4):273–287. [Google Scholar]