Recent national data have shown that the annual prevalence of depression among adolescents has increased from 8.7% in 2005 to 11.3% in 2014.1 An increasing prevalence in adolescent depression is concerning since depression can have significant consequences for youth including academic difficulty, comorbid mental health problems, and suicidal thoughts.2–4 Given that depression can have significant consequences, is treatable, and can reoccur across the lifespan,5 professional organizations have included routine screening for depression in their preventive health recommendations. For instance, a recent recommendation by the United States Preventive Services Task Force is that yearly adolescent depression screening6 should occur, starting at age 12, in situations where appropriate follow-up is possible.7 Despite these recommendations, however, physician implementation of preventive services (including depression screening) is only 34.5%.8 Thus, it is important and possible to improve physician treatement of adolescent depression.9
A combination of shortened visit times, low physician self-efficacy in relation to screening, and concerns over how to interpret and intervene with positive depression screens contribute to low screening compliance.10–12 It has been shown, however, that the use of standardized depression screening tools validated with adolescents, such as the Patient Health Questionnaire (PHQ-2 and PHQ-9), can improve rates of depression symptom identification in primary care clinics.13–15 Once depression has been identified, physician compliance with adolescent depression treatment recommendations – including recommendations to refer youth to specialized mental health treatment – is largely unknown.10 One recent survey, however, found that whereas 60% of physicians report screening children and youth for depression, only 64% report referring depressed youth to community treatment, and only 24% report treating, managing or co-managing the treatment of depressed youth in primary care.16
One demonstrated method for increasing preventive care screening and encouraging appropriate physician responses to positive screening results in other contexts, is the implementation of computer decision support systems (CDSS). Studies with adults have found that using a CDSS can improve the primary care management of depression.17,18 The present study evaluates how the integration of automated depression screening and response-driven physician management prompts into a primary care CDSS impacts physician identification and reported treatment of adolescent depression symptoms.
METHODS
CHICA System Overview
The Child Health Improvement through Computer Automation (CHICA) System is a CDSS that integrates electronic medical record (EMR) system data, pre-visit screening data, and correlative physician responses from previous visits to generate appropriate follow-up screening recommendations, tools, and physician prompts.
When a patient checks into a clinic, the CHICA system automatically generates a Pre-Screener Form (PSF) based on information in the patient’s EMR, including age, current medical conditions, and known risk factors for morbidity based on the child’s developmental stage and medical conditions. The PSF is administered on an electronic tablet and is completed prior to the physician encounter. It consists of two parts: 1) a form for the nurse to record patient vitals, height, and weight; and 2) a 20-item patient questionnaire on a variety of health-related topics such as diet, depression, sexual behaviors, and substance use. For patients aged 12 and older, instructions at the top of the patient questionnaire advise that adolescents should answer the questions on their own behalf. Follow-up items to the 20-item screener are immediately, and electronically, administered when necessary.
A provider worksheet (PWS) is generated based on patient responses to the PSF items. The PWS is printed and given to the physician for follow-up. Partially completed PSFs still generate a PWS. The PWS consists of 6 physician prompts with corresponding check boxes. When a physician responds to worksheet prompts, the form is scanned and uploaded by clinic staff after the patient encounter. The CHICA system analyzes physician responses using optimal mark and character recognition to detect which action items were reported by the physician and then records the appropriate actions in a database. Together, PSF and PWS provide screening and correlative options for physician follow-up. More detailed information about CHICA--including rule processing, development of Arden rules, data storage, and implementation--can be found in previous publications.19,20 When the system was first implemented, CHICA users, including physicians and clinic staff, completed a brief training led by the creators of CHICA. An electronic newsletter alerts all users of new CHICA modules being tested. In addition to quarterly meetings regarding CHICA operation, CHICA users may contact the CHICA developers or other research staff directly regarding questions or concerns with the system. Additionally, CHICA support staff make regular visits to participating clinics to maintain rapport with clinic staff, troubleshoot any technical issues, and answer any questions that staff members may have about the CHICA system.
Study Design and Depression Screening Process
Adolescents aged 12–20 who presented to their pediatric primary care clinic for an annual (non-sick) or sick visit between October, 2014, and October, 2015, were selected to participate in the prospective cohort study. It should be noted that the current study is part of an ongoing controlled clinical trial, using a subset of data from the intervention sites only. The depression CDSS module was implemented in 2 clinic sites (clinic A and clinic B). Although most adolescents were seen by pediatricians during usual primary care clinic hours, some adolescents were seen during onsite adolescent clinic hours by fellowship-trained adolescent medicine physicians with adolescent health specific nursing support. Both clinic sites are part of a Midwest county hospital system (Eskenazi Health). IRB approval was received by the local university and honored by the hospital system in which the study took place.
For this study, the PSF included an adaptation of a brief two-item depression screener, the Patient Health Questionnaire-2 (PHQ-2).21 If the patient answered “yes” to either question in the PHQ-2, a longer nine-item depression screener, the Patient Health Questionnaire-9 (PHQ-9)13 was automatically administered at the end of the 20-item screener. The PHQ-2 and PHQ-9 are the recommended screening sequence among adolescent populations.7 An example item from the PHQ-2 is “During the past few weeks, have you felt very sad or down as though you have nothing to look forward to?” The sensitivity of the PHQ-2 and PHQ-9 are 74% and 96% respectively, with a specificity of 75% and 82%.13,21
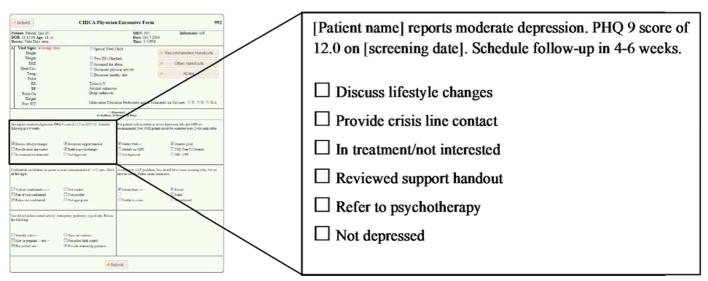
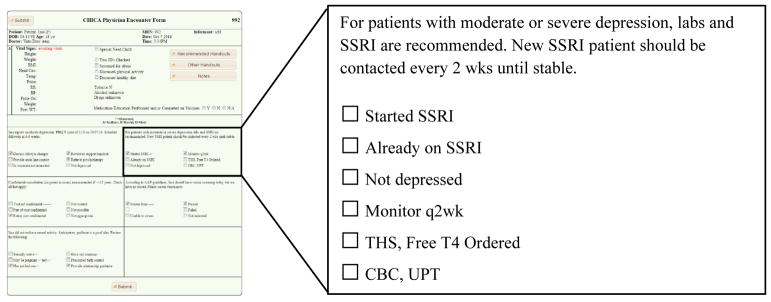
The PHQ-9 was automatically scored by CHICA. A score of 0–4 points indicates minimal/no depression symptoms, 5–9 mild depression symptoms, 10–14 moderate depression symptoms, 15–19 moderately severe and 20+ severe depression symptoms.22 A score ≥5 was considered a positive depression screen for this study. Moderately severe and severe categories were collapsed into one “severe” category for the purposes of this study. In the case of a positive depression screen, the PHQ-9 score and associated action items were printed on the PWS. For example, a moderate PHQ-9 score generated the physician prompt shown in Figures 1 and 2. Physician prompts were based on the Guidelines for Adolescent Depression-Primary Care (GLAD-PC) from the American Academy of Pediatrics.23 Physicians indicated which actions they performed or intended to perform by checking boxes next to the corresponding action items.
Figure 1.
Example Physician Prompt – Moderate Depression
Figure 2.
Example Physician Prompt – SSRI
Physician feedback regarding potential selective serotonin reuptake inhibitor (SSRI) use were included for youth with PHQ-9 scores in the moderate and severe range. For example, a positive depression screen for a patient not already taking an SSRI would generate a prompt seen in Figure 2.
Chart Abstraction
Data on physician responses were captured through the CHICA system. However, in some cases, the physicians did not indicate a response to a depression alert in CHICA. In cases where patients screened positive for depression symptoms and no physician responses were recorded on the PWS, a chart review was conducted by trained research assistants to see if physicians took action but failed to mark the corresponding check box on the PWS. Data from the chart review were added to the database and included in the final analysis.
Analyses
Descriptive statistics [means, standard deviations (SD), and frequencies] were calculated for patient demographics, clinic site, clinic type, PHQ-9 scores, and reported physician follow-up at the first visit during the study time frame for both the overall sample and the subset that screened positive for depression symptoms. We then calculated the prevalence of positive depression screening and described reported physician treatment practices for depression. Fisher’s exact test was performed to compare prevalence among depression groups (mild, moderate and severe). Lastly, we conducted logistic regression analyses to model reported physician mental health referral and SSRI initiation using the following predictors: gender, race, age (early, middle, and late adolescence), clinic site (clinic A, clinic B), clinic type (general pediatric, adolescent medicine) and PHQ-9 score (mild, moderate, and severe).
RESULTS
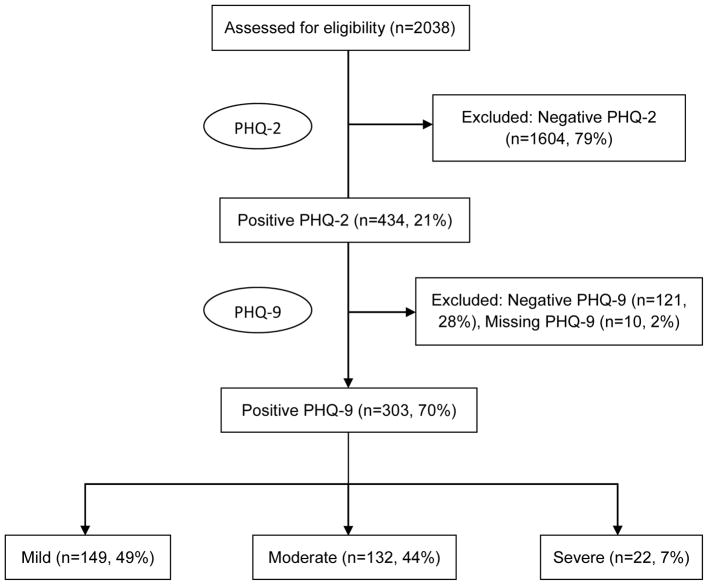
Our sample population included 2,038 youth [51% female; 60% Black; mean age=14.6 years (SD=2.1)]. See demographic information for overall sample and youth that scored above 5 on the PHQ-9 in Table 1. Just over 20% of youth (21.2%) screened positive for depression symptoms on the PHQ-2 (see flow-chart in Figure 3 which outlines depression screening of youth in primary care). Of the 434 youth with a positive PHQ-2 screen, 121 scored 0–4 on the PHQ-9 (27.8%) and 303 (69.8%) scored 5 or above [63% female; 60% Black; mean age=15.2 years (SD=2.1)], indicating possible depression. Of those 303 youth, 149 scored in the mild range (5–10, 49.1%), 132 scored in the moderate range (11–15, 43.5%) and 22 scored in the severe range (above 15; 7.2%).
Table 1.
Youth demographics, primary physician clinic type, and insurance among participants.
| All youth n=2,038 |
Elevated PHQ-9 n=303 |
|||
|---|---|---|---|---|
| N | % | N | % | |
| Race | ||||
| Black | 1286 | 60.3 | 182 | 60.1 |
| Hispanic | 305 | 14.3 | 47 | 15.5 |
| Other | 374 | 17.5 | 51 | 16.8 |
| White | 169 | 7.9 | 23 | 7.6 |
| Gender | ||||
| Female | 1088 | 51.1 | 193 | 63.7 |
| Male | 1042 | 48.9 | 110 | 36.3 |
| Mean Age (SD) | 14.6 (2.1) | 15.2 (2.1) | ||
| Insurance | ||||
| Public | 1134 | 53.2 | 179 | 59.1 |
| Private | 103 | 4.8 | 6 | 2.0 |
| Self-pay | 148 | 7.0 | 25 | 8.3 |
| Other | 746 | 35.0 | 93 | 30.7 |
| Clinic type | ||||
| General | 1803 | 84.6 | 240 | 79.2 |
| Adolescent | 328 | 15.4 | 63 | 20.8 |
| PHQ-9 Interpretation | ||||
| Mild | 149 | 49.2 | ||
| Moderate | 132 | 43.6 | ||
| Severe | 22 | 7.3 | ||
| Mean PHQ-9 Score (SD) | All adolescents | 10.8 (5.0) | ||
| Early adolescents (n=121) | 10.7 (4.8) | |||
| Middle adolescents (n=135) | 10.5 (5.0) | |||
| Late adolescents (n=47) | 11.9 (4.6) | |||
Figure 3.
Flow Diagram
Looking first at data contained in the CHICA system, 60% (n=181) of records with a positive depression screen showed no reported physician action on the PWS. With the addition of data gathered via chart review and visual inspection of the PWS, this number decreased by 135 indicating that only 15% (46 records) of youth that screened 5 or above on the PHQ-9 had no documented physician follow-up. Thirty percent of records included in the chart review were audited by a second research assistant with 94% inter-rater agreement and a pooled kappa of κ=0.27. A low kappa value despite high agreement is likely due to the low prevalence of certain follow-up items as kappa is known to be affected by imbalanced marginal totals.24 In all, physicians documented follow-up actions (either on the PWS or in the patient chart) 91% of the time for youth in the mild depression range, 93% of the time for youth in the moderate range, and 100% of the time for youth in the severe range.
Physician responses are detailed in Table 2. The follow-up categories are not mutually exclusive and physicians can check all that apply to that encounter with a youth. A significant minority of youth in the mild (22.8%) and moderate (19.7%) range were not depressed, based on physician follow-up during the encounter. All youth that scored in the severe range were determined to be depressed by physicians. Additionally, 12.8% of youth in the mild range, 6.1% of youth in the moderate range, and 18.2% of youth in the severe range were already receiving treatment at the time of visit. Of the remaining 183 (60.3%) adolescents that screened positive, the most commonly reported follow-up action by physicians was referral to mental health services (34.2% mild, 46.8% moderate, and 72.2% severe range).
Table 2.
Description of physician follow-up for youth in mild, moderate and severe PHQ-9 range.
| Follow up items | Mild N=149 |
Moderate N=132 |
Severe N=22 |
p value |
|---|---|---|---|---|
| Discussed lifestyle changes | 45 (30.2%) | 36 (27.3%) | 1 (4.5%) | 0.03 |
| Provided crisis line contact | 14 (9.4%) | 9 (6.8%) | 4 (18.2%) | 0.20 |
| In treatment/not interested | 19 (12.8%) | 8 (6.1%) | 4 (18.2%) | 0.06 |
| Reviewed support handout | 16 (10.7%) | 24 (18.2%) | 4 (18.2%) | 0.16 |
| Referred to psychotherapy | 51 (34.2%) | 61 (46.2%) | 16 (72.2%) | <0.01 |
| Not depressed | 34 (22.8%) | 26 (19.7%) | 0 (0.0%) | 0.02 |
| SSRI prescribing/considerationsa | ||||
| Started on SSRI | 11 (8.3%) | 7 (31.8%) | <0.01 | |
| Already on SSRI | 7 (4.7%) | 14 (10.6%) | 5 (22.7%) | 0.01 |
| Not depressed | 7 (4.7%) | 35 (26.5%) | 2 (9.1%) | <0.01 |
| Monitor SSRI every 2 wks | 16 (12.1%) | 4 (18.2%) | <0.01 | |
| Ordered TSH | 3 (2.0%) | 17 (12.9%) | 3 (13.6%) | <0.01 |
| Ordered free T4 | 17 (12.9%) | 3 (13.6%) | <0.01 | |
| Ordered CBC/UPT | 5 (3.4%) | 19 (14.4%) | 4 (18.2%) | <0.01 |
SSRI recommendations only provided for youth in moderate and severe ranges.
Steps for the possible initiation of SSRIs were also assessed. Almost 11% of youth in the moderate range and 22.7% of youth in the severe range were already prescribed an SSRI. A minority of youth (26.7% of youth in the moderate range and 9.1% of youth in the severe range) were either not interested in an SSRI, or the physician determined they were not good candidates for an SSRI. Of youth who scored in the moderate and severe range, 8.4% and 31.8% respectively began an SSRI at the primary care visit according to physician-reported data. A number of tests commonly related to the initiation of an SSRI were also conducted (see Table 2).
Two logistic regression models were developed to model predictors of physician follow-up actions. The first focused on youth in the mild, moderate or severe range who were not already in treatment and who physicians determined were depressed (N=215). The outcome was physician-reported referral to mental health services. Predictors included youth gender, race, age group, clinic site (clinic A, clinic B), clinic type (general pediatric, adolescent medicine) and PHQ-9 score (mild, moderate, and severe). Age groups were defined as follows: early adolescence 12–15 years, middle adolescence 15–17 years, and late adolescence 18–20 years. Significant predictors in the multivariate analysis included clinic site [40.2% clinic A vs. 73.9% clinic B; AOR 4.46 (2.43, 8.18); p≤0.0001] and PHQ-9 score [severe 77.8% vs. mild 47.5%; AOR 4.66 (1.36, 15.97); p≤0.01]. Youth demographic characteristics and clinic type (general pediatric vs. adolescent medicine) did not predict physician-reported referral to mental health services.
A second model focused on youth in the moderate or severe range who were not already prescribed an SSRI and who were interested in exploring an SSRI (N=100). The outcome was physician-reported initiation of SSRI. Predictors were identical to those in the first model. Similar to the first model, only clinic site [28.6% vs. 6.9%; AOR 6.48 (1.69, 24.80); p≤0.01] and depression score [severe range 46.7% vs. moderate range 10.6%; AOR 9.01 (2.28, 36.30); p≤0.001] were significant. Youth demographics and clinic type did not predict physician reported initiation of an SSRI.
DISCUSSION
Depression is a common condition among adolescents and even with preventive screening guidelines, the rates of screening, diagnosing, and treatment of adolescent depression remain low.25 It is vitally important to identify youth at-risk for depression, given the poor outcomes experienced by depressed youth. Primary care is an ideal setting to identify, diagnosis and treat depression.8 This study demonstrates that it is possible to successfully implement a depression algorithm within an existing CDSS that both screens and identifies youth at risk for depression symptoms. This study also shows the extent to which physicians using the algorithm report adherence to adolescent depression treatment guidelines recommended by the system when youth are identified as at-risk for depression. Below we discuss the findings of the current study in relation to previous research.
In the current study, 20% of adolescents screened positive for depression symptoms using the PHQ-2. This rate falls within the range of 12–26% reported by previous studies of depression screeners among adolescents.13,25–28 Similarly, 14% of youth scored in the mild, moderate, or severe range on the PHQ-9. As in previous studies,26,27 our findings demonstrate the feasibility of using the PHQ-2 and PHQ-9 as computer-based depression screening for adolescents in a primary care setting.
Physician Feedback and Anticipatory Guidance
To further evaluate physician follow-up, our study implemented physician prompts for each depression screen in the mild, moderate, and severe range (See Table 2). Studies of CDSS have shown that 49–96% of CDSS alerts are ignored by physicians.29,30 In the current study, we found that physicians definitively checked a box on the PWS indicating that they had received the alert and responded in some manner only 40% of the time. Upon chart review, however, we found that physicians actually responded to positive depression screens 85% of the time, suggesting that providers may have been guided by the decision support, even if they did not check the appropriate box. This discrepancy warrants further research, as ignoring a CDSS alert can result in physician practices that are not aligned with evidence-based standards.31 This also highlights the need to conduct chart reviews when initially implementing CDSS to monitor the possibility of noncompliance.
Although 85% of physicians ultimately took action based on positive depression screens, 15% did not. Potential contributing factors noted in the CDSS literature include “alert fatigue,”32,33 experience with the CDSS, perceived importance of the topic, ease of physician guidance, physicians’ level of comfort with the topic,34 and positioning of a prompt on the page.35 Regardless, this finding highlights a need to continue working toward reduced physician burden in CDSS implementation. Additionally, it is recommended that automated CDSS data collection methods, such as accessing and integrating information in the chart note, be improved to more accurately assess physician behavior.
In general, physicians responded with more extensive follow-up for youth with more severe depression symptoms. This was not true, however, in the case of the lifestyle changes handout. Physicians reported using this handout more often with mildly and moderately depressed youth than with severely depressed youth. Based on this finding, it is possible that physicians reported utilizing the handout for patients when they did not feel a mental health referral was necessary but felt the teen could benefit from anticipatory guidance regarding lifestyle changes to improve their mood. Although studies on anticipatory guidance specifically related to adolescent depression are limited, the general utility of anticipatory guidance is well documented in the literature and applicable to the prevention of adolescent depression.34,35
Our regression models revealed that only clinic site and PHQ-9 score predicted both physician-reported mental health referral and SSRI initiation. Youth demographic information such as age, race/ethnicity and gender did not predict these practices. This is an important and promising finding given the well-documented existence of racial and ethnic disparities in depression treatment.36 Of note, most patients sampled were Medicaid insured, limiting the opportunity to detect outcome variation related to patients’ socioeconomic status.
Physician Follow-up Regarding SSRI
In assessing reported physician behavior regarding prescription of SSRIs, over 30% of youth with a PHQ-9 score in the severe range were reportedly started on an SSRI, compared to under 10% of youth who scored in the moderate range. Physicians were much more likely to document that youth in the moderate range did not need medication in the physician assessment. We were unable to determine whether an SSRI was not initiated because the adolescent was not a good candidate or because the adolescent was not interested. Previous research has found roughly 50% of youth with depression were reluctant or refused to initiate psychiatric medication.37 Thus, further research is needed to determine if it would be helpful to build a psychiatric decision aide into CHICA to help the adolescent (and caregiver) determine whether an SSRI might be beneficial. This finding also highlights the fact that further research is needed to improve rates of SSRI initiation in primary care settings with adolescents.
Limitations
There are some limitations to the current study. The CHICA system has been implemented in general pediatric clinics for over 10 years. Over 85% of the youth seen in these clinic are under the age of 12. For this reason, the clinics have traditionally asked parents to complete the patient questionnaire on their child’s behalf. With the advent of the adolescent depression module in CHICA, instructions advising caregivers to have children 12 and older answer on their own behalf were implemented. Unfortunately, we have no way of knowing whether adolescents completed the PHQ-2 and PHQ-9 on their own behalf for this study. The rate of endorsement in our clinic sample was similar to that of other primary care clinics, however, increasing the face validity of our findings.13,25–28 Moving forward, future studies of CDSS screening mechanisms should focus on methods for ensuring adolescent self-report. Additionally, we are unable to determine whether or not physicians and patients followed through with physician-reported follow-up actions. For example, it is possible that a physician reported referring a patient for psychiatric evaluation and the patient did not complete the referral. Therefore, we cannot say definitively that our findings showed physician adherence to guidelines—only that physicians documented adherence.
This study was implemented into one health care system, and the generalizability of its findings to other settings may therefore be limited. Additionally, we did find significant clinic variability in mental health referral and initiation of SSRI by physicians. We did not study organizational factors in the current study and were unable to determine the cause of the clinic variability. Future research may be warranted to identify organizational barriers that impact physician-reported adherence to adolescent depression treatment guidelines. Because the CDSS generated a hardcopy physician worksheet, rather than additional electronic guidance for physicians, future research should explore the effects of a CDSS that is fully and automatically integrated within an EMR. Lastly, although chart reviews revealed that more physicians followed adolescent treatment guidelines for depression than the CDSS responses suggested, we cannot say with certainty that this improved adherence was caused by the adolescent depression treatment CDSS algorithm.
CONCLUSION
In summary, screening for adolescent depression is a practice that can be implemented into the annual physical exam using well-established screening tools that are integrated into a CDSS. As the current study demonstrates, there continue to be barriers to successfully implementing CDSS into everyday practice. However, the study also demonstrates that physician behavior can be supported to more accurately reflect treatment guidelines for the treatment of adolescent depression.
Acknowledgments
This study was funded by a grant from AHRQ R01HS022681. The authors wish to thank the CHIRDL programing team for their work in completing this project. We would also like to thank Margaret J. Blythe, MD and Laura M. Kester, MD for their support of this project and help in adapting the depression treatment algorithm.
Abbreviations
- CDSS
computer decision support system
- CHICA
Child Health Improvement through Computer Automation
- PWS
provider worksheet
- PHQ
Patient Health Questionnaire
Footnotes
Clinical Trials Registry: NCT02244138
Implications and Contribution: Professional organizations recommend adolescent depression screening when appropriate interventions are available. Little is known about how computer-based decision support systems (CDSS) can aid physicians in treating adolescent depression. This study demonstrates that a CDSS focused on adolescent depression can inform the primary care practice of physicians.
References
- 1.Mojtabai R, Olfson M, Han B. National trends in the prevalence and treatment of depression in adolescents and young adults. Pediatrics. 2016;138(6) doi: 10.1542/peds.2016-1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pomerantz EM, Altermatt ER, Saxon JL. Making the grade but feeling distressed: Gender differences in academic performance and internal distress. J Educ Psychol. 2002;94(2):396. [Google Scholar]
- 3.Kessler RC, Avenevoli S, McLaughlin K, Green JG, Lakoma M, Petukhova M, Pine D, Sampson N, Zaslavsky A, Merikangas KR. Lifetime co-morbidity of DSM-IV disorders in the US National Comorbidity Survey Replication Adolescent Supplement (NCS-A) Psychol Med. 2012;42(09):1997–2010. doi: 10.1017/S0033291712000025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weissman MM, Wolk S, Goldstein RB, Moreau D, Adams P, Greenwald S, Klier CM, Ryan ND, Dahl RE, Wickramaratne P. Depressed adolescents grown up. JAMA. 1999;281(18):1707–1713. doi: 10.1001/jama.281.18.1707. [DOI] [PubMed] [Google Scholar]
- 5.Rohde P, Lewinsohn PM, Klein DN, Seeley JR, Gau JM. Key characteristics of major depressive disorder occurring in childhood, adolescence, emerging adulthood, and adulthood. Clin Psychol Sci. 2013;1(1):41–53. doi: 10.1177/2167702612457599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American Academy of Pediatrics. 2016 recommendations for preventive pediatric health care. Pediatrics. 2016;137(1):25–27. [Google Scholar]
- 7.Siu AL. Screening for depression in children and adolescents: US Preventive Services Task Force recommendation statement. Ann Intern Med. 2016;164:I–28. doi: 10.7326/M15-2957. [DOI] [PubMed] [Google Scholar]
- 8.Mangione-Smith R, DeCristofaro AH, Setodji CM, Keesey J, Klein DJ, Adams JL, Schuster MA, McGlynn EA. The quality of ambulatory care delivered to children in the United States. N Engl J Med. 2007;357(15):1515–1523. doi: 10.1056/NEJMsa064637. [DOI] [PubMed] [Google Scholar]
- 9.Gadomski AM, Fothergill KE, Larson S, Wissow LS, Winegrad H, Nagykaldi ZJ, Olson AL, Roter DL. Integrating mental health into adolescent annual visits: Impact of previsit comprehensive screening on within-visit processes. J Adolesc Health. 2015;56(3):267–273. doi: 10.1016/j.jadohealth.2014.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wissow LS, Brown J, Fothergill KE, Gadomski A, Hacker K, Salmon P, Zelkowitz R. Universal mental health screening in pediatric primary care: A systematic review. J Am Acad Child Adolesc Psychiatry. 2013;52(11):1134–1147 e1123. doi: 10.1016/j.jaac.2013.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Buckelew SM, Adams SH, Irwin CE, Gee S, Ozer EM. Increasing clinician self-efficacy for screening and counseling adolescents for risky health behaviors: Results of an intervention. J Adolesc Health. 2008;43(2):198–200. doi: 10.1016/j.jadohealth.2008.01.018. [DOI] [PubMed] [Google Scholar]
- 12.Fallucco EM, Conlon MK, Gale G, Constantino JN, Glowinski AL. Use of a standardized patient paradigm to enhance proficiency in risk assessment for adolescent depression and suicide. J Adolesc Health. 2012;51(1):66–72. doi: 10.1016/j.jadohealth.2011.12.026. [DOI] [PubMed] [Google Scholar]
- 13.Richardson LP, McCauley E, Grossman DC, McCarty CA, Richards J, Russo JE, Rockhill C, Katon W. Evaluation of the Patient Health Questionnaire-9 item for detecting major depression among adolescents. Pediatrics. 2010;126(6):1117–1123. doi: 10.1542/peds.2010-0852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sudhanthar S, Thakur K, Sigal Y, Turner J. Improving validated depression screen among adolescent population in primary care practice using electronic health records (EHR) BMJ Qual Improvement Rep. 2015;4(1) doi: 10.1136/bmjquality.u209517.w3913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Trivedi MH, Kern JK, Grannemann BD, Altshuler KZ, Sunderajan P. A computerized clinical decision support system as a means of implementing depression guidelines. Psychiatr Serv. 2004;55(8):879–885. doi: 10.1176/appi.ps.55.8.879. [DOI] [PubMed] [Google Scholar]
- 16.Stein REK, Storfer-Isser A, Kerker BD, Garner A, Szilagyi M, Hoagwood KE, O’Connor KG, Horwitz SM. Beyond ADHD: How well are we doing? Acad Pediatr. 2015 doi: 10.1016/j.acap.2015.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Korsen N, Scott P, Dietrich AJ, Oxman T. Implementing an office system to improve primary care management of depression. Psychiatr Q. 2003;74(1):45–60. doi: 10.1023/a:1021193606120. [DOI] [PubMed] [Google Scholar]
- 18.Kroenke K, Taylor-Vaisey A, Dietrich AJ, Oxman TE. Interventions to improve provider diagnosis and treatment of mental disorders in primary care. A critical review of the literature. Psychosomatics. 2000;41(1):39–52. doi: 10.1016/S0033-3182(00)71172-8. [DOI] [PubMed] [Google Scholar]
- 19.Anand V, Biondich PG, Liu G, Rosenman M, Downs SM. Child health improvement through computer automation: The CHICA system. Stud Health Technol Inform. 2004;107(Pt 1):187–191. [PubMed] [Google Scholar]
- 20.Carroll AE, Bauer NS, Dugan TM, Anand V, Saha C, Downs SM. Use of a computerized decision aid for ADHD diagnosis: A randomized controlled trial. Pediatrics. 2013;132(3):e623–e629. doi: 10.1542/peds.2013-0933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Richardson LP, Rockhill C, Russo JE, Grossman DC, Richards J, McCarty C, McCauley E, Katon W. Evaluation of the PHQ-2 as a brief screen for detecting major depression among adolescents. Pediatrics. 2010;125(5):e1097–e1103. doi: 10.1542/peds.2009-2712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kroenke K, Spitzer RL, Williams JB. The PHQ-9. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zuckerbrot RA, Cheung AH, Jensen PS, Stein RE, Laraque D. Guidelines for adolescent depression in primary care (GLAD-PC): Identification, assessment, and initial management. Pediatrics. 2007;120(5):e1299–e1312. doi: 10.1542/peds.2007-1144. [DOI] [PubMed] [Google Scholar]
- 24.Feinstein AR, Cicchetti DV. High agreement but low Kappa: The problems of two paradoxes. J Clin Epidemiol. 1990;43(6):543–549. doi: 10.1016/0895-4356(90)90158-l. [DOI] [PubMed] [Google Scholar]
- 25.Ozer EM, Zahnd EG, Adams SH, Husting SR, Wibbelsman CJ, Norman KP, Smiga SM. Are adolescents being screened for emotional distress in primary care? J Adolesc Health. 2009;44(6):520–527. doi: 10.1016/j.jadohealth.2008.12.016. [DOI] [PubMed] [Google Scholar]
- 26.Paperny DM, Aono JY, Lehman RM, Hammar SL, Risser J. Computer-assisted detection and intervention in adolescent high-risk health behaviors. Pediatrics. 1990;116(3):456–462. doi: 10.1016/s0022-3476(05)82844-6. [DOI] [PubMed] [Google Scholar]
- 27.Chisolm DJ, Gardner W, Julian T, Kelleher KJ. Adolescent satisfaction with computer-assisted behavioural risk screening in primary care. Child Adolesc Ment Health. 2008;13(4):163–168. doi: 10.1111/j.1475-3588.2007.00474.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fein JA, Pailler ME, Barg FK, Wintersteen MB, Hayes K, Tien AY, Diamond GS. Feasibility and effects of a web-based adolescent psychiatric assessment administered by clinical staff in the pediatric emergency department. Arch Pediatr Adolesc Med. 2010;164(12):1112–1117. doi: 10.1001/archpediatrics.2010.213. [DOI] [PubMed] [Google Scholar]
- 29.van der Sijs H, Mulder A, van Gelder T, Aarts J, Berg M, Vulto A. Drug safety alert generation and overriding in a large Dutch university medical centre. Pharmacoepidemiol Drug Saf. 2009;18(10):941–947. doi: 10.1002/pds.1800. [DOI] [PubMed] [Google Scholar]
- 30.Bauer NS, Carroll AE, Saha C, Downs SM. Experience with decision support system and comfort with topic predict clinicians’ responses to alerts and reminders. J Am Med Inform Assoc. 2016;23(e1):e125–130. doi: 10.1093/jamia/ocv148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Coiera E, Aarts J, Kulikowski C. The dangerous decade. J Am Med Inform Assoc. 2012;19(1):2–5. doi: 10.1136/amiajnl-2011-000674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Collins S, Currie L, Patel V, Bakken S, Cimino JJ. Multitasking by clinicians in the context of CPOE and CIS use. Stud Health Technol Inform. 2007;129(Pt 2):958–962. [PubMed] [Google Scholar]
- 33.Carroll AE, Anand V, Downs SM. Understanding why clinicians answer or ignore clinical decision support prompts. Appl Clin Inform. 2012;3(3):309–317. doi: 10.4338/ACI-2012-04-RA-0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.González HM, Vega WA, Williams DR, Tarraf W, West BT, Neighbors HW. Depression care in the United States: Too little for too few. ArchGen Psychiatr. 2010;67(1):37–46. doi: 10.1001/archgenpsychiatry.2009.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stein REK, Zitner LE, Jensen PS. Interventions for adolescent depression in primary care. Pediatrics. 2006;118(2):669–682. doi: 10.1542/peds.2005-2086. [DOI] [PubMed] [Google Scholar]
- 36.Alegría M, Chatterji P, Wells K, Cao Z, Chen CN, Takeuchi D, Jackson J, Meng XL. Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatr Serv. 2008;59(11):1264–1272. doi: 10.1176/appi.ps.59.11.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.DeBar LL, Clarke GN, O’Connor E, Nichols GA. Treated prevalence, incidence, and pharmacotherapy of child and adolescent mood disorders in an HMO. Ment Health Serv Res. 2001;3(2):73–89. doi: 10.1023/a:1011512901714. [DOI] [PubMed] [Google Scholar]