Abstract
Background:
Several procedures have been proposed to address irreparable rotator cuff (RC) tears with pseudoparalysis. One recently proposed procedure is superior capsular reconstruction (SCR) using a tensor fasciae latae (TFL) autograft.
Hypothesis:
SCR with a locally available long head of the biceps tendon (LHB) autograft is biomechanically equivalent to SCR using TFL autograft for preventing superior humeral migration and the development of RC arthropathy in patients with irreparable RC tears.
Study Design:
Controlled laboratory study.
Methods:
Ten cadaveric shoulders (5 matched pairs) were tested. One shoulder from each pair was randomly assigned to the LHB reconstruction group using our novel technique, while the contralateral side was assigned to the TFL reconstruction group. SCR with a TFL autograft was performed based on previously described techniques. Massive RC tears were created by detachment of the supraspinatus and infraspinatus footprints from the greater tuberosity. The force required to superiorly translate the humerus 1.5 cm was then tested and recorded using a servohydraulic testing machine under 2 conditions: (1) after a massive RC tear and (2) after SCR with either a TFL autograft or an LHB autograft.
Results:
SCR with an LHB autograft required 393.2% ± 87.9% (P = .029) of the force needed for superior humeral migration in the massive RC tear condition, while SCR with a TFL autograft required 194.0% ± 21.8% (P = .0125). The LHB reconstruction group trended toward a stronger reconstruction when normalized to the torn condition (P = .059).
Conclusion:
SCR with an LHB autograft is a feasible procedure that is shown to be biomechanically equivalent and potentially even stronger than SCR with a TFL autograft in the prevention of superior humeral migration.
Clinical Relevance:
This new technique may help to prevent superior humeral migration and the development of RC arthropathy in patients with irreparable RC tears.
Keywords: superior capsular reconstruction, rotator cuff arthropathy, irreparable rotator cuff, biceps tendon autograft, biomechanical, superior humeral migration
The rotator cuff (RC) is a primary dynamic stabilizer of the glenohumeral joint. Throughout the physiological shoulder range of motion, the RC maintains concentric reduction of the humeral head on the glenoid.2,14 When disrupted, the joint kinematics is altered, resulting in superior humeral translation, articular wear, and ultimately arthritis (RC arthropathy).13,16,17
Repairing massive RC tears can be challenging and technically difficult. Chronic tears, in particular, may be deemed irreparable because of significant muscle atrophy and tendon retraction.5,11,15 Several procedures have been proposed to address irreparable RC tears, including partial repair, pectoralis major or latissimus dorsi tendon transfer, fascia or dermal-based patches, and reverse total shoulder arthroplasty.1,9,10 The multitude of procedures available is an indication that there is no single consensus to the treatment of irreparable RC tears in the young active population. Reverse total shoulder arthroplasty has emerged as a potential treatment for irreparable RC tears in older patients; however, in patients younger than 65 years, evidence suggests a survival rate of 76% at 10 years and complication rates as high as 50%.4,6,18 Although a feasible option for some patients, relatively young patients may outlive the implant and are not ideal candidates for this procedure.
For these patients with irreparable RC tears, there are few procedures available that will prevent superior humeral head migration and subsequent RC arthropathy. One recently proposed option is arthroscopic superior capsular reconstruction (SCR) with a tensor fasciae latae (TFL) autograft.12 The graft restores superior glenohumeral stability and function of shoulder joints with irreparable RC tears but also involves a separate incision and procedure to harvest the graft, potentially increasing pain, the risk for infections, and donor site morbidity.
Our goal was to prevent superior humeral migration and the development of RC arthropathy in patients with irreparable RC tears. We aimed to test the resistant force for superior humeral migration in a cadaveric biomechanical model after SCR with the long head of the biceps tendon (LHB) and compare this with the previously described technique of SCR with a TFL autograft. We hypothesized that SCR with a locally available LHB autograft would be a biomechanically equivalent option.
Methods
Ten cadaveric shoulders (5 matched pairs) were received by donation to the university anatomy program and were tested in this study. One shoulder from each pair was randomly assigned to the LHB reconstruction group, with the contralateral side assigned to the TFL reconstruction group. All shoulders were dissected of skin and soft tissue, and only the RC muscles and LHB insertion on the glenoid remained. The entire footprints of the supraspinatus and infraspinatus tendons on the greater tuberosity were then excised to re-create an irreparable massive RC tear. To create a similar, reproducible, massive RC tear in each cadaveric specimen, we identified the anterior and posterior edges of both the infraspinatus and supraspinatus tendons and sharply detached the entire footprints of these 2 tendons. We confirmed the same massive RC tear dimensions between matched cadaveric pairs to remove any variables in our data with regard to RC tear size.
The glenoid was then separated from the scapula 5 cm medial to the articular surface and fixed horizontally into a quadrangular block of polymethyl methacrylate (PMMA) bone cement set into a mounting bracket, as seen in Figure 1. Both axes of the glenoid were aligned to the mounting bracket using a mounting level. The humerus was transected 7 cm distal to the inferior margin of the articular surface and mounted perpendicularly into a second quadrangular block of PMMA bone cement. The glenoid was mounted horizontally onto a load cell with the humerus fixed to the loading arm in the hanging arm position on a DynaMight 8841 testing system (Instron) (Figure 1). A compressive load of 22 N was applied across the glenohumeral joint to simulate intracapsular pressure on a custom mount with a precalibrated compressive spring. Under computer control, the humeral head was centered on the glenoid and then translated 1.5 cm superiorly. This was repeated for 50 cycles, and the force resisting superior translation was characterized for each cycle.
Figure 1.
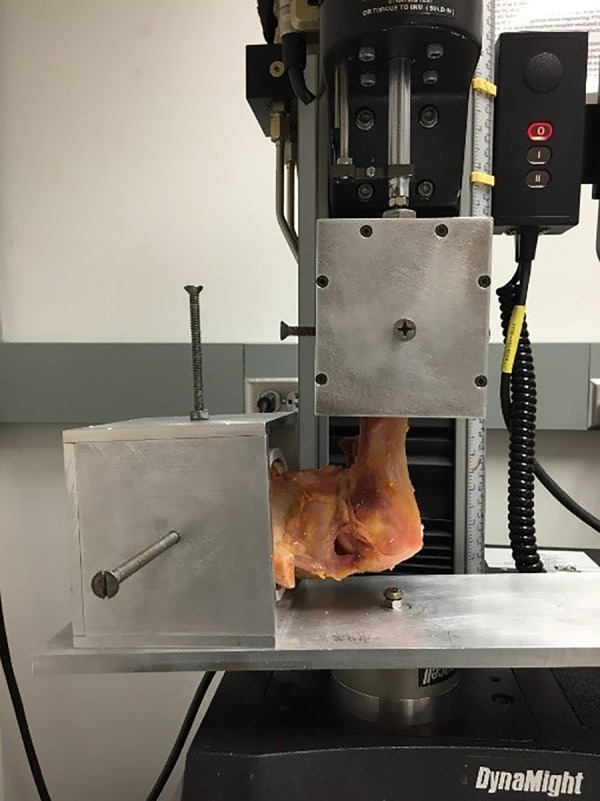
Cadaveric shoulder mounting and servohydraulic testing performed after rotator cuff tear and superior capsular reconstruction.
After baseline measurements of superior humeral migration for shoulders with a massive RC tear were taken, 5 cadaveric specimens underwent SCR utilizing a TFL autograft. A single orthopaedic surgeon (R.E.) performed both reconstruction types. We utilized a cadaveric TFL autograft, which was obtained from a matched cadaveric thigh, and performed patch reconstruction as described by Mihata et al.12 We emulated this model to create a standardized control with which our new reconstruction model could be compared.
This technique involved attaching one end of the once-folded TFL autograft to the superior glenoid using two 5 mm–diameter Corkscrew II anchors and No. 2 FiberWire sutures (Arthrex). These anchors were inserted into the superior glenoid at approximately the 10- and 12-o’clock positions on the glenoid of a right shoulder and the 1- and 2-o’clock positions of a left shoulder.12 The lateral edge of the TFL autograft was then attached to the RC footprint on the greater tuberosity using a double-row technique. Two Corkscrew II anchors were placed medially at the edge of the articular cartilage, and another 2 were placed laterally 5 to 10 mm inferior to the highest tip of the greater tuberosity. We then performed side-to-side closure of the patch to the infraspinatus and subscapularis. This completed the TFL patch reconstruction procedure.
The remaining 5 cadaveric shoulders underwent SCR utilizing the LHB and our new technique. The LHB remained intact at its origin on the superior anterior glenoid and transected sharply at the musculotendinous junction distally. The length of the LHB varied among specimens; however, we determined that 12 cm was necessary for this reconstruction procedure. A cinching stitch was then placed through the distal transected end of the LHB using FiberLink sutures (Arthrex). Next, using this stitch, the LHB was attached to the superior posterior glenoid by using a single 2.9-mm PushLock anchor (Arthrex). The placement of this anchor was approximately 2 cm posterior to the LHB insertion site and was similar to the placement of the medial anchor in TFL reconstruction as described by Mihata et al.12
After securing the distal end of the LHB to the superior glenoid, a loop of the LHB with the apex distal and lateral remained, as the glenoid origin was still intact as well. We then removed any remaining soft tissue at the lateral and superior edges of the articular surface of the humeral head to prepare for anchor placement. We then created a tunnel for the anchor and biceps tendon using an 8.5-mm piloted head reamer aimed at 45° from horizontal, starting at the center of the supraspinatus footprint insertion at the lateral and superior edges of the humeral head articular cartilage. This was drilled to a depth of 20 mm. We then placed the fork of an 8-mm SwiveLock tenodesis anchor (Arthrex) over the biceps tendon loop, equidistant from the native insertion and the new second glenoid fixation point, to create a “V” configuration with equal tension on both limbs. The fork was then advanced into the previously reamed tunnel with the arm abducted 45°. The LHB now created a tensioned “V” configuration over the humeral head. A comparison of both reconstruction techniques can be seen in Figure 2.
Figure 2.
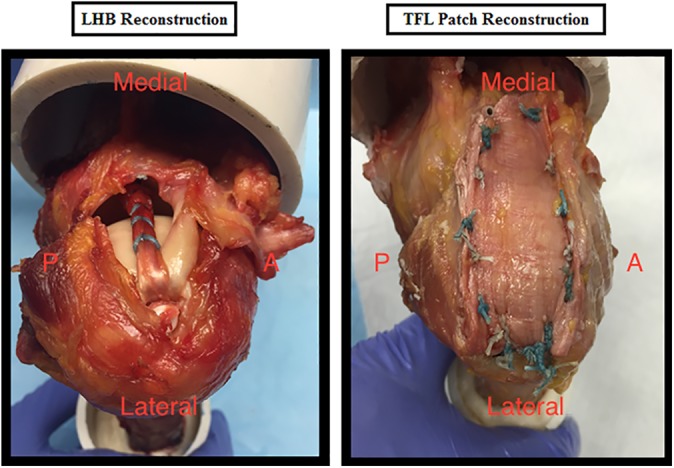
Superior capsular reconstruction with long head of the biceps tendon (LHB) and tensor fasciae latae (TFL).P, posterior; A, anterior.
The force required to superiorly migrate the humerus in each specimen was again tested after SCR. This resulted in 2 groups: (1) SCR with a TFL autograft and (2) SCR with an LHB autograft. These groups were tested under 2 conditions: (1) a massive RC tear without SCR and (2) a massive RC tear after SCR. The force required to superiorly translate the humerus 1.5 cm in our cadaveric massive RC models (“torn condition”) was compared before and after SCR with either technique. The change or increase in force required to superiorly translate the humerus was also compared between the torn condition and each reconstruction group. Cadaveric demographics, mean force required to superiorly translate the humerus, and change in mean force when normalized to the torn condition were recorded and analyzed using standard t tests.
Results
The mean age of the specimens was 63 years (range, 59-67 years). Two of the 10 specimens were male. Compared with the massive RC tear condition, SCR with an LHB autograft required 393.2% ± 87.9% (P = .029) of the force needed for superior humeral migration, while SCR with a TFL autograft required 194.0% ± 21.8% (P = .0125) of the force. The mean force required for superior humeral migration after SCR with an LHB autograft was 66.9 ± 5.6 N versus 22.5 ± 7.2 N in the RC tear condition (P = .0006). The mean force required for superior humeral migration after SCR with a TFL autograft was 160.9 ± 50.6 N versus 76.1 ± 17.2 N in the RC tear condition (P = .0656). The LHB reconstruction group trended toward a stronger reconstruction than SCR with a TFL autograft when normalized to the torn condition (P = .059). There were no noted failures in either group after testing.
Discussion
Superior migration of the humeral head secondary to RC deficiency leads to RC arthropathy and labral degeneration. Patients with irreparable RC tears who are relatively young and active are not ideal candidates for reverse total shoulder replacement. For these patients in particular, the possibility of regaining shoulder stability and joint congruency by preventing superior humeral migration could change the natural history of their condition.
The recent literature supports the concept of SCR and has shown clinical improvement in patients with irreparable massive RC tears after SCR with a TFL autograft and dermal allograft reconstruction.7,8 In a prospective observation study of 24 patients who underwent SCR with a dermal allograft, Mihata et al12 found that all patients demonstrated a significant improvement in pain, range of motion, and strength with improved American Shoulder and Elbow Surgeons and 12-Item Short Form Health Survey scores at 3-year follow-up.
Our study proposes the use of a locally available LHB autograft for SCR. The results show that SCR with our proposed LHB autograft technique significantly increases the mean force required for superior humeral migration compared with the RC tear condition and trends toward a stronger reconstruction compared with previously utilized TFL patch reconstruction when normalized to the torn condition. In addition, our technique utilizes fewer anchors and sutures than previously described TFL and dermal allograft techniques. Consequently, this will certainly decrease the overall cost of the LHB autograft procedure compared with the cost of dermal allograft reconstruction.
Although this is a novel technique, the concept of using the LHB in the treatment of patients with massive RC tears has been previously supported. Cho et al3 compared RC repair with and without augmentation with the LHB in 68 patients. In their study, the LHB was transected at its glenoid origin, shuttled into the subacromial space, incorporated into the lateral edge of the RC, and attached to the anatomic RC insertion site on the humeral head. After an average follow-up of 21 months, patients in the RC repair group with biceps augmentation showed improved forward flexion, external rotation, and internal rotation strength than those without biceps augmentation.
There are several limitations to our study. First, the study was based on cadaveric models, and clinical function and strength results may differ because of other dynamic stabilizers of the shoulder. Second, performing SCR with an LHB autograft arthroscopically may be technically more demanding than performing the SCR technique in our cadaveric model. Third, our study did not take into account shoulders that may not have a viable LHB for SCR. In these cases, we propose the use of a TFL autograft or dermal allograft as a viable option for SCR. The difference between the 2 techniques did not achieve statistical significance, and therefore, the question of whether the LHB technique is biomechanically superior to the TFL technique could not be definitively answered.
SCR with an LHB autograft is a feasible procedure that is shown to be biomechanically equivalent and potentially even stronger than SCR with a TFL autograft in the prevention of superior humeral migration. SCR with an LHB autograft may prevent superior humeral migration and its associated conditions in patients with irreparable RC tears. Further clinical prospective studies are needed to compare clinical outcomes, specifically shoulder range of motion and strength, after SCR with an LHB autograft.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: G.N. is a paid speaker/presenter for Arthrex. M.M. is a paid speaker/presenter for Arthrex and Prodigy Surgical Distribution. I.V. is a paid consultant for Acumed, Smith & Nephew, Tenex Health, and Zimmer Biomet and is a paid speaker/presenter for Arthrex and Pacira Pharmaceuticals.
Ethical approval for this study was waived by the University of Rochester Research Subjects Review Board.
References
- 1. Bedi A, Dines J, Warren RF, Dines DM. Massive tears of the rotator cuff. J Bone Joint Surg Am. 2010;92(9):1894–1908. [DOI] [PubMed] [Google Scholar]
- 2. Burkhart SS. Fluoroscopic comparison of kinematic patterns in massive rotator cuff tears: a suspension bridge model. Clin Orthop Relat Res. 1992;(284):144–152. [PubMed] [Google Scholar]
- 3. Cho NS, Yi JW, Rhee YG. Arthroscopic biceps augmentation for avoiding undue tension in repair of massive rotator cuff tears. Arthroscopy. 2009;25(2):183–191. [DOI] [PubMed] [Google Scholar]
- 4. Ek ET, Neukom L, Catanzaro S, Gerber C. Reverse total shoulder arthroplasty for massive irreparable rotator cuff tears in patients younger than 65 years old: results after five to fifteen years. J Shoulder Elbow Surg. 2013;22:1199–1208. [DOI] [PubMed] [Google Scholar]
- 5. Gartsman GM. Massive, irreparable tears of the rotator cuff: results of operative debridement and subacromial decompression. J Bone Joint Surg Am. 1997;79(5):715–721. [DOI] [PubMed] [Google Scholar]
- 6. Guery J, Favard L, Sirveaux F, Oudet D, Mole D, Walch G. Reverse total shoulder arthroplasty: survivorship analysis of eighty replacements followed for five to ten years. J Bone Joint Surg Am. 2006;88(8):1742–1747. [DOI] [PubMed] [Google Scholar]
- 7. Gupta AK, Hug K, Berkoff DJ, et al. Dermal tissue allograft for the repair of massive irreparable rotator cuff tears. Am J Sports Med. 2012;40(1):141–147. [DOI] [PubMed] [Google Scholar]
- 8. Gupta AK, Hug K, Boggess B, Gavigan M, Toth AP. Massive or 2-tendon rotator cuff tears in active patients with minimal glenohumeral arthritis: clinical and radiographic outcomes of reconstruction using dermal tissue matrix xenograft. Am J Sports Med. 2013;41(4):872–879. [DOI] [PubMed] [Google Scholar]
- 9. Kim SJ, Lee IS, Kim SH, Lee WY, Chun YM. Arthroscopic partial repair of irreparable large to massive rotator cuff tears. Arthroscopy. 2012;28(6):761–768. [DOI] [PubMed] [Google Scholar]
- 10. Kokkalis ZT, Mavrogenis AF, Scarlat M, et al. Human dermal allograft for massive rotator cuff tears. Orthopedics. 2014;37(12):e1108–e1116. [DOI] [PubMed] [Google Scholar]
- 11. Lo IK, Burkhart SS. Arthroscopic repair of massive, contracted, immobile rotator cuff tears using single and double interval slides: technique and preliminary results. Arthroscopy. 2004;20(1):22–33. [DOI] [PubMed] [Google Scholar]
- 12. Mihata T, Lee TQ, Watanabe C, et al. Clinical results of arthroscopic superior capsule reconstruction for irreparable rotator cuff tears. Arthroscopy. 2013;29(3):459–470. [DOI] [PubMed] [Google Scholar]
- 13. Neer CS, 2nd, Craig EV, Fukuda H. Cuff-tear arthropathy. J Bone Joint Surg Am. 1983;65(9):1232–1244. [PubMed] [Google Scholar]
- 14. Parsons IM, Apreleva M, Fu FH, Woo SL. The effect of rotator cuff tears on reaction forces at the glenohumeral joint. J Orthop Res. 2002;20(3):439–446. [DOI] [PubMed] [Google Scholar]
- 15. Rokito AS, Cuomo F, Gallagher MA, Zuckerman JD. Long-term functional outcome of repair of large and massive chronic tears of the rotator cuff. J Bone Joint Surg Am. 1999;81(7):991–997. [DOI] [PubMed] [Google Scholar]
- 16. Su WR, Budoff JE, Luo ZP. The effect of anterosuperior rotator cuff tears on glenohumeral translation. Arthroscopy. 2009;25(3):282–289. [DOI] [PubMed] [Google Scholar]
- 17. Visotsky JL, Basamania C, Seebauer L, Rockwood CA, Jensen KL. Cuff tear arthropathy: pathogenesis, classification, and algorithm for treatment. J Bone Joint Surg Am. 2004;86(suppl 2):35–40. [PubMed] [Google Scholar]
- 18. Wall B, Nové-Josserand L, O’Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007;89(7):1476–1485. [DOI] [PubMed] [Google Scholar]


