Abstract
The laryngeal mask airway (LMA) Protector™ has recently made its way into clinical practice. As little is reported on this novel supraglottic airway device, we describe our experiences through intubation and Bailey manoeuvre using the LMA Protector™, and the assessment of vocal cord mobility using a flexible bronchoscope through it in three patients undergoing hemithyroidectomies.
Keywords: Airway management, case report, laryngeal masks, thyroidectomy
INTRODUCTION
The role of supraglottic airway devices (SADs) has expanded. No longer just primary airway devices for oxygenation and ventilation, SADs can also be used for airway rescue as an intubation conduit as well as for emergence and extubation as part of the Bailey manoeuvre. Intubation through a SAD results in a lower stimulating haemodynamic response compared to intubation via laryngoscopy, and it is recognized as Plan B in the Difficult Airway Society's (DAS) unanticipated difficult airway guidelines,[1] and as Step 2 of the algorithm for unanticipated difficult tracheal intubation in adults proposed by the All India Difficult Airway Association (AIDAA).[2] The Bailey manoeuvre involves the replacement of an endotracheal tube (ETT) with a SAD to maintain a patent airway at the end of surgery. This method has a smoother emergence profile than tracheal extubation and is one of the advanced techniques for difficult extubation in the DAS and AIDAA extubation guidelines.[3,4] Hence, it is useful for thyroid surgeries, whereby an ETT may induce coughing in patients during extubation that can result in surgical wound reopening and subsequent development of haematoma.[5] Not only does this approach provide a more superior emergence from anesthesia with reduced cardiovascular stimulation and cough reflex, but the SAD also allows a flexible bronchoscope to be inserted in situ to assess for vocal cord mobility and any presence of laryngeal oedema.[6,7] In addition, should there be a need for reintubation (e.g., if a vocal cord palsy is seen on bronchoscopy), the SAD can be used as an intubation conduit.
The laryngeal mask airway (LMA; Teleflex® Medical Asia, Singapore) Protector™ was recently introduced with little published studies on its utility to date. In this case report, we describe the successful use and expanding role of the LMA Protector™ in three patients scheduled for elective hemithyroidectomies. In all patients, the LMA Protector™ was used in conjunction with the Bailey manoeuvre for assessment of vocal cord mobility and to achieve smoother emergence from anaesthesia. Even though none of the patients required reintubation, the use of LMA Protector™ at the start of the surgery as an intubation conduit showed that it can be used for this purpose as well. Written informed consent for the use of bronchoscopic images and details of the case for publication of this report was obtained for all patients.
CASE REPORT
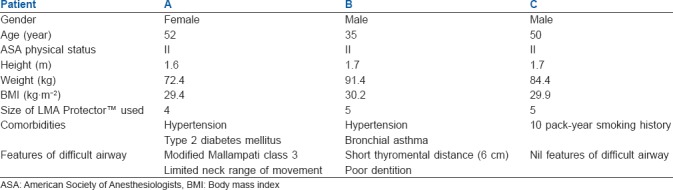
We recruited three patients who were scheduled for elective hemithyroidectomies. All of them were American Society of Anesthesiologists’ (ASA) physical status II with body mass indices ranging 29.4–30.2 kg·m−2 [Table 1]. Standard anaesthetic monitoring devices such as pulse oximeter, non-invasive blood pressure cuff, electrocardiogram leads, capnogram, body temperature probe and train-of-four (TOF) neuromuscular monitor were placed for all patients. General anaesthesia was induced following standard protocols.
Table 1.
A summary of demographic profiles, comorbidities, and airway assessments of patients undergoing elective hemithyroidectomies
In all three patients, an appropriate size LMA Protector™ was placed atraumatically after induction of anaesthesia on the first attempt. Once a TOF of 0 was elicited, oral intubation with a size 7.0 Fastrach™-reinforced ETT (Teleflex® Medical Asia, Singapore) was performed through the LMA Protector™ guided by a Karl Storz Flexible Intubating Video Endoscope (FIVE™; Karl Storz, Tuttlingen, Germany). In all three cases, either a Brimacombe grade 2 (vocal cords and anterior epiglottis seen) or grade 3 (vocal cords and posterior epiglottis seen) equivalent fiber-optic laryngeal views were obtained [Figure 1].[8] The ETT was easily railroaded over the bronchoscope into the trachea using the LMA Protector™ as a conduit for all cases. The LMA Protector™ was then removed over the ETT with the use of either the Fastrach™ stabilizing rod or a pediatric-sized Magills forceps.[9] The reinforced ETT was subsequently secured in a northward facing direction for the rest of the surgery. Surgery proceeded uneventfully in all three cases.
Figure 1.
Preintubation laryngeal views shows Brimacombe grade 2 view for patients A (a) and C (c), and Brimacombe grade 3 view for patient B (b)
At the end of the surgery, Bailey manoeuvre was performed following preoxygenation and thorough oral suctioning while keeping the patient in a deep plane of anesthesia. In each case, the original LMA Protector™ was reinserted posterior to the in situ ETT. Subsequently, the LMA Protector™ cuff was inflated to a pressure of 60 cm H2O before the ETT cuff was deflated and the ETT removed. After verification of the LMA placement with capnography, reversal of paralysis guided by TOF readings was performed using standard doses of intravenous neostigmine and glycopyrrolate.
Once spontaneous respiration returned with the patient still under general anaesthesia, the fibrescope was reinserted into the LMA Protector™ to assess vocal cord mobility. In all three patients, bilateral vocal cords were visualized to be moving, providing a reassuring sign that injury to the recurrent laryngeal nerve did not occur intraoperatively [Figure 2]. The patients were then transferred to the postanaesthesia care unit for them to awaken and the LMA Protector™ to be taken out. There were no patient symptoms or signs suggestive of recurrent laryngeal nerve palsy, hence correlating well to the vocal cord mobility observed through the LMA Protector™ at the end of surgery.
Figure 2.
Postextubation laryngeal views. In patients A (a), B (b) and C (c), there was good mobility of vocal cords bilaterally
DISCUSSION
The LMA Protector™ was recently introduced into clinical practice in 2016. The novel aspect of this new SAD is its fixed-curved structure that allows easy insertion, while its wide internal airway lumen diameter (up to 13 mm) allows flexibility and thereby enhancing its use as an intubation conduit. Currently, there is a paucity of published data available evaluating its safety, efficacy, and utility in human subjects, with only a number of studies evaluating its use in specific scenarios.[10,11,12]
From our report, we can appreciate the clinical advantages that the LMA Protector™ has to offer. All three patients had successful LMA Protector™ insertion on the first attempt and were found to have adequate placement as assessed via flexible bronchoscopy as shown in Figure 1. We found no difficulty inserting the ETT through the LMA Protector™ during intubation, and in replacing the LMA Protector™ for the ETT when performing the Bailey manoeuvre. These were possible because the LMA Protector™ has a large diameter airway channel with an unobstructed glottic opening, therefore permitting its manipulation with an ETT. The manufacturer's guide from Teleflex® has indicated that a size 3 LMA Protector™ is able to admit a size 6.5 ETT. The LMA Protector™ sizes 4 and 5 were able to admit a size 7.5 ETT. This feature is particularly important in both anticipated and unanticipated difficult airway situations, in which the LMA Protector™ can be used as an intubation conduit.[13]
Additionally, we describe the novel dual-purpose use of the LMA Protector™ for assessment of vocal cord mobility postoperatively with a flexible bronchoscope. Hence, this feature not only allows prompt identification of vocal cord dysfunction suggestive of recurrent laryngeal nerve injury but also permits an ETT to be railroaded over the flexible bronchoscope and through the LMA Protector™ for securement of airway in cases of severe vocal cord paralysis.
CONCLUSION
We describe our initial experiences of using the LMA Protector™ in thyroid surgeries, particularly in its versatility to be used as an intubation conduit, and as a replacement of the ETT during deep extubation through which a flexible bronchoscope can be inserted to visualize postoperative vocal cord mobility.
Financial support and sponsorship
Nil.
Conflicts of interest
Leng Zoo Tan was sponsored by Teleflex a training trip to Germany to learn about the LMA Protector™ from Professor Friedrich Pühringer: Professor and Chairman of the Department of Anesthesiology and Intensive Care Medicine at the Klinikum am Steinenberg in Reutlingen on 12th April 2016. Leng Zoo Tan has agreed to this arrangement to learn the correct usage of the LMA Protector™, which was a novel product at that point in time. The LMA Protector™ used for the case report was also provided free by Teleflex. This was necessary as the LMA Protector™ was not available for purchase at the point of the case report. Leng Zoo Tan did not, at any time, receive payment for any aspect of the submitted work.
REFERENCES
- 1.Frerk C, Mitchell VS, McNarry AF, Mendonca C, Bhagrath R, Patel A, et al. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth. 2015;115:827–48. doi: 10.1093/bja/aev371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Myatra SN, Shah A, Kundra P, Patwa A, Ramkumar V, Divatia JV, et al. All India Difficult Airway Association 2016 guidelines for the management of unanticipated difficult tracheal intubation in adults. Indian J Anaesth. 2016;60:885–98. doi: 10.4103/0019-5049.195481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mitchell V, David R, Patel A, Swampillai C, Higgs A. Difficult Airway Society Guidelines for the management of tracheal extubation. Anaesthesia. 2012;67:318–40. doi: 10.1111/j.1365-2044.2012.07075.x. [DOI] [PubMed] [Google Scholar]
- 4.Kundra P, Garg R, Patwa A, Ahmed SM, Ramkumar V, Shah A, et al. All India Difficult Airway Association 2016 guidelines for the management of anticipated difficult extubation. Indian J Anaesth. 2016;60:915–21. doi: 10.4103/0019-5049.195484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Terris DJ, Snyder S, Carneiro-Pla D, Inabnet III WB, Kandil E, Orloff L, et al. American Thyroid Association statement on outpatient thyroidectomy. Thyroid. 2013;23:1193–202. doi: 10.1089/thy.2013.0049. [DOI] [PubMed] [Google Scholar]
- 6.Nair I, Bailey PM. Use of the laryngeal mask for airway maintenance following tracheal extubation. Anaesthesia. 1995;50:174. doi: 10.1111/j.1365-2044.1995.tb15104.x. [DOI] [PubMed] [Google Scholar]
- 7.Ellard L, Brown DH, Wong DT. Extubation of a difficult airway after thyroidectomy: Use of a flexible bronchoscope via the LMA-Classic™. Can J Anaesth. 2012;59:53–7. doi: 10.1007/s12630-011-9619-y. [DOI] [PubMed] [Google Scholar]
- 8.Brimacombe J, Berry A. A proposed fiber-optic scoring system to standardize the assessment of laryngeal mask airway position. Anesth Analg. 1993;76:457. [PubMed] [Google Scholar]
- 9.Tan DJA, Tan LZ, Seet E. Low-skill flexible bronchoscopic intubation – Overcoming common pitfalls. J Clin Anesth. 2017;38:83–4. doi: 10.1016/j.jclinane.2017.01.028. [DOI] [PubMed] [Google Scholar]
- 10.Tan LZ, Tan DJA, Seet E. Laryngeal mask airway protector™: Advanced uses for laparoscopic cholecystectomies. Indian J Anaesth. 2017;61:673–5. doi: 10.4103/ija.IJA_240_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sng BL, Ithnin FB, Mathur D, Lew E, Han NL, Sia AT. A preliminary assessment of the LMA protector™ in non-paralysed patients. BMC Anesthesiol. 2017;17:26. doi: 10.1186/s12871-017-0323-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tan LZ, Tan DJA, Seet E. Use of the Laryngeal Mask Airway (LMA) Protector™ for shoulder surgeries in beach-chair position. J Clin Anesth. 2017;39:110–1. doi: 10.1016/j.jclinane.2017.03.036. [DOI] [PubMed] [Google Scholar]
- 13.Van Zundert AA, Skinner MW, Van Zundert TC, Luney SR, Pandit JJ. Value of knowing physical characteristics of the airway device before using it. Br J Anaesth. 2016;117:12–6. doi: 10.1093/bja/aew106. [DOI] [PMC free article] [PubMed] [Google Scholar]




