Abstract
The aim of this study is to report 11 cases of erector spinae plane (ESP) block used for unilateral or bilateral abdominal surgery, adding to the overall limited experience with abdominal ESP block. The procedures were carried out at a teaching hospital in 11 patients (eight males, three females, ages 36–80 years) requiring abdominal surgery, including laparoscopic surgery. Each patient required surgery under different physical circumstances and likely different conceptions of what constituted pain. Two of the eleven patients were administered the ESP block and did not require general anaesthesia. Most of the patients with the ESP block maintained a numerical rating scale (NRS) for pain of 0–2/10 postoperatively. An occasional patient required paracetamol analgesia. There were no cases of opiate rescue. Obesity in a 46-year-old woman was believed to cause unclear ultrasonographic visualisation, interfering with entry of the ESP catheter. She, however, had no post-operative pain. She was given the usual intravenous metamizole 2 g for 10 h and required only analgesics at 16 h. ESP block, which produces analgesia by blocking trunk nerves, is an appropriate approach to patients requiring abdominal surgery, whether laparoscopic or open.
Keywords: Nerve block, pain, pain management, post-operative, regional anaesthesia
INTRODUCTION
Multimodal anaesthesia that combines the use of an epidural catheter and general anaesthesia is a common technique used for surgical procedures associated with intense post-operative pain. The technique is considered a quality standard because it provides good control of the anticipated pain. Placement of the epidural catheter is not always possible, however, due to technical difficulties or patient-related conditions that contraindicate its insertion.
The erector spinae plane (ESP) block,[1] described recently, provides extensive, potent unilateral analgesia. The block is initiated by injecting anaesthetic in the plane between the erector spinae muscle and the transverse process, with its effect seemingly due in part to diffusion of the local anaesthetic into the paravertebral space through spaces between adjacent vertebrae. The anaesthetic then acts on both the dorsal and ventral branches of the thoracic spinal nerves.[1,2,3]
Its safety profile is different from that of the epidural catheter alone. The ESP block is performed under ultrasonographic guidance. The target is the transverse process, which is easily identifiable and is relatively distant from neural or major vascular structures and the pleura. An advantage is that it provides extensive analgesia with a single puncture. These characteristics allow its placement with the patient in different postural positions, such as a sitting position or in a lateral decubitus or prone position. Thus, it is possible to perform the block at metameric levels relatively distant from the surgical zone, thereby avoiding local problems that could contraindicate the puncture at a specific point.
Till date, most publications about the ESP block focused on its use for thoracic surgery,[4,5,6,7,8,9] with only a few references to surgery at the abdominal level.[10,11] The case series, which include 11 patients (the largest series published so far), help consolidate the overall experience with the ESP block during unilateral or bilateral abdominal surgery.
CASE REPORTS
Case 1
An 80-year-old male underwent radical prostatectomy under epidural and general anaesthesia. Before anaesthetic induction, an epidural catheter was placed at the T11–T12 level without incident. An initial bolus of 8 ml of 0.125% bupivacaine was administered. During the surgery, two more boluses of 8 ml of 0.125% were administered in a short time as the patient showed clinical signs of pain. Remifentanil 0.15–0.25 μg/kg/min was given. Thirty minutes before the end of surgery, intravenous metamizole (2 g) and a new epidural bolus of 8 ml of 0.125% bupivacaine were administered.
In the post-anaesthetic recovery room, the patient complained of pain (numerical rating scale [NRS] 7/10). Due to the now non-functioning epidural catheter, and considering that ESP block could produce analgesia at the abdominal level when performed at a low thoracic level,[10,11] we decided to perform bilateral ESP block at the T8 level after obtaining informed consent. With the patient in sitting position, we proceeded with the technique as described by Forero et al.,[1] using a linear high-frequency ultrasonographic probe (Esaote LA523, 4-13 MHz; Esaote Europe B.V., Maastrich, The Netherlands), and a neural block set StimuLong Nanoline 19G ×100 mm needle and catheter (Pajunk Medizintechnologie Gm, Geisingen, Germany).
Taking the C7 spinous process as a reference, the T8 spinous process was identified by palpation. Once located, the probe was placed over the spinous process and slipped laterally approximately 3 cm until the transverse process was identified [Figure 1]. At this point, the probe was rotated longitudinally, and the puncture was performed in the craniocaudal direction following the previous infiltration with a local anaesthetic. Visualising the needle in plane along its entire length, when it contacted the transverse process, 1 ml of anaesthetic solution was injected. Hydrodissection of the interfascial plane between the erector spinae muscle and the transverse process was confirmed by visualising the local anaesthetic spreading in a linear pattern between the muscle and the bony acoustic shadows of the transverse process [Figure 2a and b], ensuring correct localisation. Then, up to 20 ml of bupivacaine 0.5% in 5 ml aliquots were injected. After the injection, an epidural catheter for continuous infusion during the post-operative period was inserted and secured. The procedure was repeated following the same steps on the contralateral side. Subsequently, we connected two infusers to each catheter and administered 0.18% ropivacaine at a rate of 7 ml/h in each.
Figure 1.
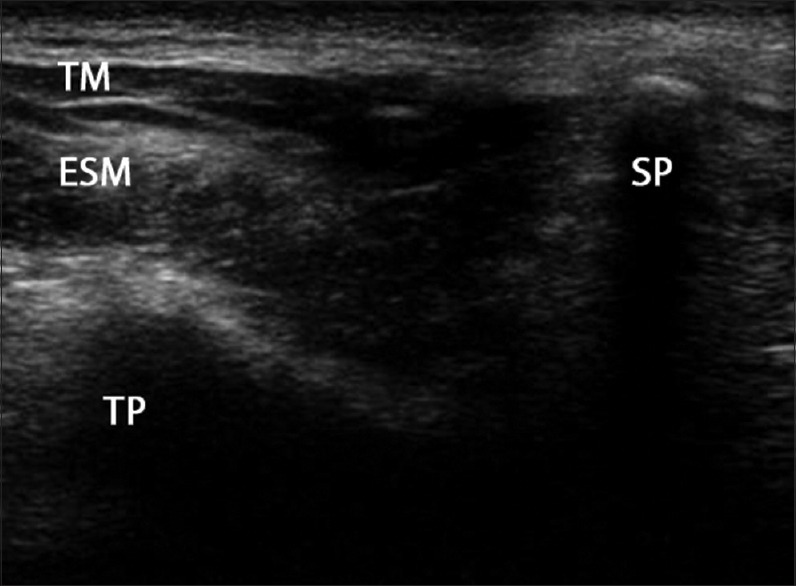
Ultrasonographic transverse section of the T8 vertebra. ESM = Erector spinae muscle; SP = Spinous process; TM = Trapezius muscle; TP = Transverse process
Figure 2.
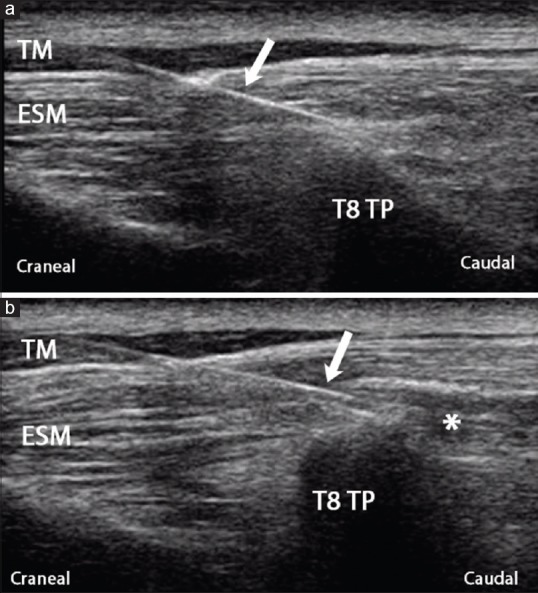
Ultrasonography, sagittal view. Needle in contact with T8 transverse process. (a) Before injecting anaesthetic. (b) After injecting anaesthetic. ESM = Erector spinae muscle; TM trapezius muscle; TP = Transverse process. Arrow = Needle. *Hydrodissection of the interfascial plane after injection
Twenty minutes after performing the block, the patient reported the disappearance of pain (NRS 0/10), and there was decreased sensation to pinprick over the anterior abdomen from the T6 to L1 dermatomes. The catheters were maintained in place for 48 h. The patient required only one dose of analgesic (paracetamol). There was no need for an opioid. No complications associated with the procedure were reported.
Cases 2-5
In cases 2–5, we used an ESP block in each of the four patients (two women, two men; ages 48–72 years) who were scheduled to undergo laparoscopic nephrectomy. As part of the multimodal analgesia, the ESP catheter was inserted only before the induction of anaesthesia. The ESP block was performed as described above in all patients after obtaining their informed consent.
We performed the ESP block at the T8 level before induction of anaesthesia, with the patient in a sitting position. The highest NRS score was 2/10 in one patient and 1/10 in the remaining three patients during the post-operative follow-up (36–48 h). These patients reported only low-intensity, diffuse abdominal discomfort, which we attributed to peritoneal irritation related to gas insufflation during the laparoscopy. In addition to ropivacaine 0.18% infusion at 7 ml/h, which we maintained for 48 h, intravenous paracetamol (1 g) was prescribed, which was sufficient to address the abdominal discomfort. In no patient was it necessary to use an analgesic rescue with opioids.
Case 6
In case 6, a 64-year-old male was scheduled to undergo laparoscopic nephrectomy and ipsilateral inguinal herniorrhaphy during the same surgical session. After obtaining informed consent, we performed a unilateral ESP block using 20 ml of bupivacaine 0.5% at the T9 level to reach a lower metameric level because of the additionally scheduled inguinal herniorrhaphy. With the patient in a sitting position, we placed the ESP catheter at the T9 level before induction of anaesthesia. During the laparoscopic procedure, new information was found that discouraged nephrectomy, and hence, only open inguinal herniorrhaphy was finally performed. In the recovery area, the patient reported mild, diffuse abdominal discomfort (NRS 1/10) that was treated with intravenous paracetamol. The patient had decreased sensation to pinprick over the anterior abdomen and the upper inner side of the thigh from the T8 to L2 dermatomes. The ESP catheter was maintained in place for 24 h, and the patient did not require further analgesia.
Case 7
In case 7, a 36-year-old man was scheduled for right nephrectomy. After obtaining informed consent, the ESP block was performed with the patient anaesthetised (patient's preference). The materials and techniques were the same as in the previous cases – the only difference being that the patient was in the lateral decubitus position. Although the ESP block was performed without difficulty, it was not possible to introduce a catheter for post-operative analgesia. This patient required intravenous rescue analgesia after approximately 16 h because of the effects of the ESP blockade.
Case 8
In case 8, a 46-year-old obese woman (body mass index was 39.6 kg/m2) was scheduled to undergo renal transplantation. After obtaining informed consent, we performed an ESP block before induction of anaesthesia, with the patient in a sitting position. Ultrasonographic visualisation of the transverse processes was not clear. After the needle contacted the T7 transverse process, 20 ml of 0.5% bupivacaine was administered, producing the fascial plane hydrodissection, but it was not possible to introduce the catheter. We attributed the failure in this case to the fact that the insertion angle was steeper than in previous cases because of the greater distance from the skin to the transverse process due to the patient's obesity. Thus, we were forced to use a more acute angle to contact the transverse process. It is likely that the needle contact with the transverse process was excessively frontal, on its upper face, thereby preventing entry of the catheter.
This patient required low doses of intravenous remifentanil during the intervention (0.02 μg/kg/min), and she woke up without pain. Except for intravenous metamizole 2g, 10 hours after the surgery, she did not require additional analgesics until 16 h postoperatively.
Case 9
In case 9, a 66-year-old hypertensive male, who had previously undergone cephalic pancreatectomy to remove a cholangiocarcinoma – was scheduled for gastroenterotomy. During previous surgery, placement of the epidural catheter was difficult. At this admission, after obtaining informed consent, we established bilateral blockade at the T7 level before induction of anaesthesia, placing two catheters with the patient in a sitting position.
Intraoperatively, the patient required only low doses of remifentanil, and opiates rescue was not needed at the end of the surgery. During the post-operative period, the patient maintained an NRS of 0–1/10 during the 48 h the catheters remained in place. No intravenous analgesic rescue was required.
Case 10
In case 10, a 77-year-old man who was obese (body mass index was 37.9 kg/m2), hypertensive, dyslipidaemic, and had type 2 diabetes was admitted to our department with a history of non-ST elevation acute coronary syndrome and atrial fibrillation. He was scheduled for open cholecystectomy due to suspicion of malignant neoplasia of the gallbladder. As the surgeon planned a large subcostal incision, after obtaining informed consent, we performed a bilateral block at the T7 level before induction of anaesthesia, with the patient in a sitting position. After placing the ESP catheter on the left side without incident, on the right side as we did not observe net hydrodissection of the planes. It was therefore considered that the technique had failed. The left catheter was withdrawn, and intravenous analgesia was administered. On awakening, the patient complained of moderate pain on the right side (NRS 4/10) but not on the left side (NRS 0/10).
Case 11
In case 11, a 78-year-old male was scheduled for open inguinal herniorrhaphy. He had a history of difficult intradural puncture and severe nausea on administration of opioids. After obtaining informed consent, ESP block was performed at the ipsilateral T9 level. Unlike the previous cases, we used a commercial setup for the plexus block that included an 18G, 100 cm needle with a hyperechoic 20G catheter (Vygon, Ecouen, France). This apparatus allowed us to check the entrance of the catheter in the hydrodissection cavity and its placement caudal to the point of contact with the transverse process. The surgery was performed 15 min after placement under light sedation (midazolam 3 mg and propofol 30 mg) –an opioid-free analgesia protocol with intravenous ketamine (20 mg), magnesium sulphate (15 mg/kg/h for 10 min and 8 mg/kg/h afterwards), and lidocaine 1.5 mg/kg/h. The patient reported minimal discomfort at some point during the procedure but did not require analgesia during the post-operative period up to hospital discharge 48 h later.
DISCUSSION
ESP block is a recently described technique that produces analgesia through a truncal nerve block.[1] The erector spinae muscle comprises a set of muscles and tendons that extend through the lumbar, thoracic, and cervical areas. It is located in the lateral sulcus of the spine and includes the iliocostalis, longissimus and spinalis muscles.
ESP block is performed by injecting anaesthetic under the erector spinae muscle and into the inter-fascial plane between this muscle and the transverse processes. Its effect seems to be due in part to diffusion of the local anaesthetic into the paravertebral space through the non-osseous spaces between adjacent vertebrae, which then acts on both the dorsal and ventral branches of the thoracic spinal nerves,[1,2,5] as well as the communicating branches that feed the sympathetic chain.[11] It thus has an effect profile similar to that of retrolaminar and paravertebral blocks.[3,12,13]
Initially, the technique was carried out at the level of the transverse process of T5, achieving an anaesthetic distribution ranging from C7-T1 to T8 and resulting in effective analgesia of the ipsilateral thoracic wall.[1] As the erector spinae muscle extends throughout the lumbar region, ESP block can also produce abdominal analgesia if it is performed at a lower level.[2]
The ESP block represents a simpler, possibly safer alternative to epidural or paravertebral thoracic block because the transverse process, which represents the ultrasonic target, is easily visualised and the point of injection is far from the neuroaxis, pleura, and large vascular structures.[6] This location is an advantage in anaesthetised patients or those with additional difficulties.[7] In addition, the extensive craniocaudal diffusion of the anaesthetic allows wide coverage with a single injection, allowing the approach to occur at points relatively distant from the surgical zone.[6]
The first publications addressing this novel block focussed on thoracic analgesia. They described its use as treatment for thoracic neuropathic pain,[1] costal fractures,[8] thoracic vertebral surgery,[5] breast surgery[14] and thoracic surgery in one child in whom the blockade was performed at the end of the surgical intervention, with the patient still anaesthetised,[6] as a rescue technique during thoracotomy for lobectomy in the case of a non-functioning epidural catheter,[9] and as a technique of choice for thoracoscopic lobectomy.[4] There were also some references to its use for abdominal surgery, such as repair of ventral hernias or bariatric surgery.[10,11]
Our experience focusses on the surgery performed at the abdominal level. In publications on ESP block for abdominal surgery, the block was performed at the level of T7 and its effect showed extensive extension from the T6 to T12 dermatomes,[10,11] whereas injection of 20 ml of contrast material at T7 in cadavers showed extensive craniocaudal spread between the levels of the C5-T2 and L2–L3 transverse processes.[10] Based on these data, and because the surgery in our patients is generally performed at a level slightly lower than that described in those publications, we decided to perform the blockade at the level of T8 (even T9 when the inguinal region was included in the surgical field).
Although our purpose in all patients was to place the catheter so it could be used to prolong the blockade when necessary, in two cases, it was not possible. In one of them (Case 8), the angle of incidence of the needle with the transverse process was too steep owing to the characteristics of the patient. We surmised that introduction of the catheter was prevented because the needle contact with the transverse process was excessively frontal, on its upper face, preventing entry of the catheter. The other case (Case 7) occurred when we performed the blockade under anaesthesia with the complete neuromuscular blockade. We observed the rapid disappearance of the hydrodissection cavity, which we thought could hinder the catheter's progression. In both patients, the duration of analgesia was greater than 16 hours, with no other analgesics required during this period. This duration makes it feasible for many patients to benefit from the ESP block without placement of a catheter.
The shapes of the transverse processes vary considerably among the thoracic vertebrae, which can lead to errors in their identification by ultrasonography. At the middle thoracic level, around T5, the transverse process is nearly cylindrical (about 2 cm in length) and its end projects approximately 3 cm from the spinous process of the vertebra [Figure 3]. Thus, its ultrasonographic image is semilunar with a posterior shadow, as described in several publications.[1,8]
Figure 3.
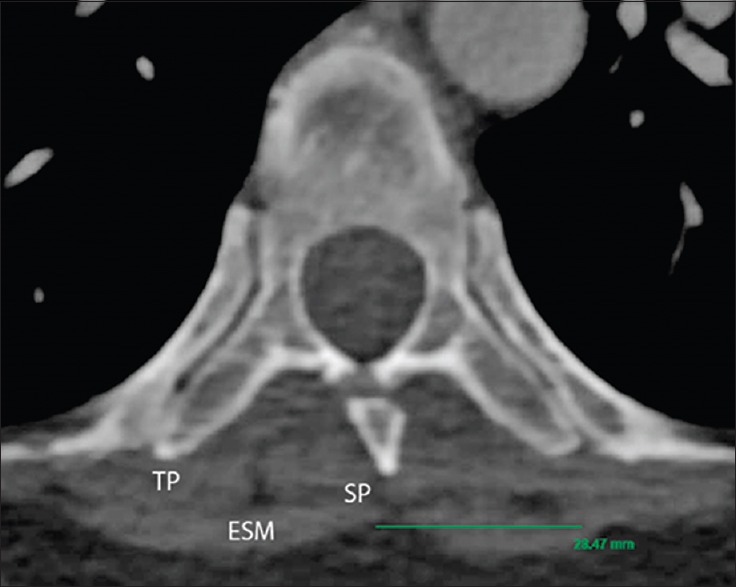
Computed tomography scan. Transverse section of the T5 vertebra. ESM = Erector spinae muscle; SP = Spinous process; TP = Transverse process
At a lower thoracic level, however, such as from T7 [Figure 4a] or T9 [Figure 4b], the transverse process becomes an angular projection that barely protrudes from the articular processes, with its distant end <2.5 cm from the axis of the spinous processes. Thus, the ultrasonographic image changes, becoming less rounded, almost triangular and the transducer should be placed closer to the spinous processes, overlapping the images of the articular processes [Figures 1 and 2].
Figure 4.
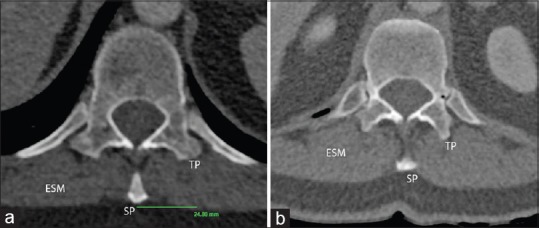
(a) Computed tomography scan. Transverse section of the T7 vertebra. ESM = Erector spinae muscle; SP = Spinous process; TP = Transverse process. (b) Computed tomography scan. Transverse section of the T9 vertebra. ESM = Erector spinae muscle; SP = Spinous process; TP = Transverse process
CONCLUSION
ESP block was initially described for post-operative pain control or analgesic rescue when other techniques failed. In our experience, however, intra-operative use reduces the need for intravenous analgesics during surgery. Our experience with unilateral ESP blockade during laparoscopic nephrectomy shows a high rate of success and no complications related to either catheter placement or continuous administration of local anaesthetic. This discovery encourages us to continue to use it as the first-line analgesia as part of multimodal analgesia, replacing the use of the epidural catheter.
The experience with bilateral blockades in abdominal surgery has also been positive. It is a useful alternative to the epidural catheter or intradural anaesthesia, especially when there are contraindications to these techniques or their performance is difficult or unsuccessful.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We would like to thank Nancy Schatken, BS, MT (ASCP), from Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.
REFERENCES
- 1.Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: A Novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41:621–7. doi: 10.1097/AAP.0000000000000451. [DOI] [PubMed] [Google Scholar]
- 2.Chin KJ, Forero M, Adhikary SD. Reply to Dr. Ueshima and Dr. Murouchi. Reg Anesth Pain Med. 2017;42:124–5. doi: 10.1097/AAP.0000000000000531. [DOI] [PubMed] [Google Scholar]
- 3.Ueshima H, Otake H. Similarities between the retrolaminar and erector spinae plane blocks. Reg Anesth Pain Med. 2017;42:123–4. doi: 10.1097/AAP.0000000000000526. [DOI] [PubMed] [Google Scholar]
- 4.Scimia P, Basso Ricci E, Droghetti A, Fusco P. The ultrasound-guided continuous erector spinae plane block for postoperative analgesia in video-assisted thoracoscopic lobectomy. Reg Anesth Pain Med. 2017;42:537. doi: 10.1097/AAP.0000000000000616. [DOI] [PubMed] [Google Scholar]
- 5.Ueshima H, Otake H. Clinical experiences of ultrasound-guided erector spinae plane block for thoracic vertebra surgery. J Clin Anesth. 2017;38:137. doi: 10.1016/j.jclinane.2016.12.028. [DOI] [PubMed] [Google Scholar]
- 6.Muñoz F, Cubillos J, Bonilla AJ, Chin KJ. Erector spinae plane block for postoperative analgesia in pediatric oncological thoracic surgery. Can J Anaesth. 2017;64:880–2. doi: 10.1007/s12630-017-0894-0. [DOI] [PubMed] [Google Scholar]
- 7.El-Boghdadly K, Pawa A. The erector spinae plane block: Plane and simple. Anaesthesia. 2017;72:434–8. doi: 10.1111/anae.13830. [DOI] [PubMed] [Google Scholar]
- 8.Hamilton DL, Manickam B. Erector spinae plane block for pain relief in rib fractures. Br J Anaesth. 2017;118:474–5. doi: 10.1093/bja/aex013. [DOI] [PubMed] [Google Scholar]
- 9.Forero M, Rajarathinam M, Adhikary S, Chin KJ. Continuous erector spinae plane block for rescue analgesia in thoracotomy after epidural failure: A Case report. A A Case Rep. 2017;8:254–6. doi: 10.1213/XAA.0000000000000478. [DOI] [PubMed] [Google Scholar]
- 10.Chin KJ, Adhikary S, Sarwani N, Forero M. The analgesic efficacy of pre-operative bilateral erector spinae plane (ESP) blocks in patients having ventral hernia repair. Anaesthesia. 2017;72:452–60. doi: 10.1111/anae.13814. [DOI] [PubMed] [Google Scholar]
- 11.Chin KJ, Malhas L, Perlas A. The erector spinae plane block provides visceral abdominal analgesia in bariatric surgery: A Report of 3 cases. Reg Anesth Pain Med. 2017;42:372–6. doi: 10.1097/AAP.0000000000000581. [DOI] [PubMed] [Google Scholar]
- 12.Murouchi T. Consideration of block nomenclature: Erector spinae plane block or retrolaminar block? Reg Anesth Pain Med. 2017;42:124. doi: 10.1097/AAP.0000000000000525. [DOI] [PubMed] [Google Scholar]
- 13.Hamilton DL, Manickam B. The erector spinae plane block. Reg Anesth Pain Med. 2017;42:276. doi: 10.1097/AAP.0000000000000565. [DOI] [PubMed] [Google Scholar]
- 14.Bonvicini D, Giacomazzi A, Pizzirani E. Use of the ultrasound-guided erector spinae plane block in breast surgery. Minerva Anestesiol. 2017;83:1111–2. doi: 10.23736/S0375-9393.17.12015-8. [DOI] [PubMed] [Google Scholar]


