Abstract
Background and Aims:
Many patients experience moderate-to-severe pain after laparoscopic cholecystectomy. We aimed to compare the efficacy of ultrasound-guided bilateral subcostal transversus abdominis plane (TAP) block with port-site infiltration for post-operative analgesia after laparoscopic cholecystectomy.
Methods:
Patients undergoing elective laparoscopic cholecystectomy under general anaesthesia were divided into two groups of 40 each to receive ultrasound-guided bilateral subcostal TAP block (T) with 0.25% bupivacaine 20 ml each side or port-site infiltration with 0.5% bupivacaine 5 ml each at 4 ports (I) at the end of the surgery before extubation. All patients received paracetamol 1 g intravenous 8th hourly. Tramadol 1 mg/kg intravenous bolus and diclofenac 1 mg/kg intravenous infusion were used as the first- and second-line rescue analgesics when Numerical Rating Scale (NRS) ≥4, or when the patient complained of pain. NRS at 1, 2, 3, 6, 12 and 24 h after surgery, time to first analgesic request and total dose of analgesics in 24 h were recorded. Chi-square test and independent t-test were used to compare qualitative and quantitative data, respectively.
Results:
Time to first analgesic (mean±SD) in Group I and Group T was 292.7 ± 67.03 and 510.3 ± 154.55 min and mean tramadol required was141.8 ± 60.01 mg and 48.69 ± 36.14 mg, respectively (P = 0.001 for both). Mean NRS at 2, 3, 6, 12 and 24 h was significantly lower in Group T.
Conclusion:
Ultrasound-guided bilateral subcostal TAP block provides superior post-operative analgesia after laparoscopic cholecystectomy compared to port-site infiltration.
Keywords: Bupivacaine, laparoscopic cholecystectomy, post-operative analgesia, transversus abdominis plane block
INTRODUCTION
Laparoscopic cholecystectomy is a safe and effective procedure done for various gall bladder disease conditions and has become the treatment of choice for symptomatic gall stones. Compared to open cholecystectomy, laparoscopic method is associated with less post-operative pain, early recovery reduced hospital expenses and improved cosmesis and patient satisfaction, and thus, it is even done as a day-care surgery.[1,2,3] Although minimally invasive, many of the patients experience moderate-to-severe pain in the early post-operative period.[4]
Subcostal transversus abdominis plane (TAP) block can provide sensory block of the T7 to T12 nerves as against the classical posterior approach which provides sensory block from T10 to L1 spinal segment levels.[5] The accuracy and quality of nerve blockade can be enhanced with the guidance of ultrasound. Port-site infiltration with local anaesthetics is another effective method of providing analgesia after laparoscopic cholecystectomy.[6] However, there is a paucity of literature comparing the efficacy of these two methods, so we planned this study.
The aim of the study was to compare the efficacy of USG-guided bilateral subcostal TAP block with port-site infiltration using bupivacaine for post-operative analgesia after laparoscopic cholecystectomy with a hypothesis that both TAP block and port-site infiltration are effective in providing post-operative analgesia.
METHODS
It was a double-blinded randomised comparative clinical trial done on patients undergoing elective laparoscopic cholecystectomy in a state-owned tertiary care teaching hospital during 2015–2016 after getting Institutional Research and Ethical Committee approval. Eighty patients with the American Society of Anesthesiologists (ASA) physical status I/II, aged between 20 and 65 years with a body mass index (BMI) of 18–35 kg/m2 scheduled for elective laparoscopic cholecystectomy, were recruited and randomised into two groups of 40 each using computer-generated random number chart. An informed written consent was obtained from each patient with respect to the nature of anaesthesia and options of analgesia. Patients with allergy to local anaesthetics, infection at the site of injection, chronic pain syndromes, prolonged opioid medication, coagulopathy and those patients who received any analgesic 24 h before surgery were excluded from the study.
Preoperatively all patients were instructed regarding how to read the NRS that was used for assessing the pain in the post-operative period. Education status of the patients were assessed to eliminate bias due to difference in education level of the participants which may influence the interpretation of NRS. All patients received oral premedication with ranitidine 150 mg and metoclopramide 10 mg 2 h before the proposed surgery, and injection midazolam 0.5 mg was given intravenously (IV) immediately before induction. Induction was with injection propofol 2 mg/kg IV and injection fentanyl 2 μg/kg IV. Endotracheal intubation with appropriate size cuffed endotracheal tube was facilitated with injection succinylcholine 1.5 mg/kg intravenously. Anaesthesia was maintained with oxygen (33%), nitrous oxide (66%) and isoflurane (0.4%to 0.8%) and injection atracurium 0.5 mg/kg IV bolus for muscle relaxation. Additional atracurium was given as deemed necessary by the attending anaesthesiologist. Intraoperative monitors included electrocardiogram, non-invasive blood pressure, pulse oximeter and end-tidal carbon dioxide. Vitals signs were maintained stable throughout intraoperative period.
All patients received injection paracetamol 1 g intravenous infusion intraoperatively at the beginning of surgery. At the end of surgery before extubation, patients received either port-site local anaesthetic infiltration or ultrasound-guided bilateral subcostal TAP block. Port-site infiltration was with 20 mL of 0.5% bupivacaine (5 mL at each of the four port sites – umbilical, epigastric, midclavicular and anterior axillary ports on the right side) by the operating surgeon. Bilateral ultrasound-guided subcostal TAP block was performed by the attending experienced anaesthesiologist with 20 mL of 0.25% bupivacaine on each side using SonoSite MicroMaxx transportable ultrasound and high-frequency (6–13 MHz) linear transducer. A total of 100 mg of bupivacaine was used in both groups. The anaesthesiologist and surgeon performing the block were not involved in post operative follow up of patient.
Postoperatively, all patients received paracetamol 1 g intravenous infusion 8th hourly. For breakthrough pain, injection tramadol 1 mg/kg intravenous bolus and diclofenac 1 mg/kg intravenous infusion were given as the first- and second-line rescue analgesics, respectively. NRS for pain was assessed serially at 1, 2, 3, 6, 12 and 24 h after surgery. The assessor and the patients were unaware of the type of intervention received. Rescue analgesics were administered when NRS ≥4 or when the patient complained of pain. Time for first analgesic request and NRS at first analgesic request were recorded. The duration of analgesia was taken as the time from block administration to the time at which patient complained of pain or NRS was ≥4 on assessment at serial intervals. Total doses of rescue analgesics required in the first 24 h were recorded. Occurrence of any complications such as haematoma, bleeding, nausea, vomiting and allergic reactions was also observed.
Our primary objective was to find the mean total analgesic requirement in 24 h and the duration of analgesia and secondary objective to assess the quality of analgesia using Numerical Rating Scale (NRS).
In a previous study,[7] the mean post-operative fentanyl consumption was 86.9 ± 73.79 μg in port-site infiltration compared to 33.16 ± 54.17 μg in TAP block group. Keeping a power at 80% and alpha error at 0.05, a sample size of 23 would be required in each group. Hence, we recruited 40 patients in each group to compensate for the dropouts if any. Statistical analysis of the data was done using the Statistical Package for the Social Sciences for Windows (SPSS Inc., Chicago) software version 18. Qualitative data such as sex, ASA physical status, education and adverse effects were compared using Chi-square test. Quantitative data such as age, height, weight, BMI, numeric rating scales, time to first analgesic request and total analgesic requirement in 24 h were compared using independent t-test. P < 0.05 was taken as statistically significant.
RESULTS
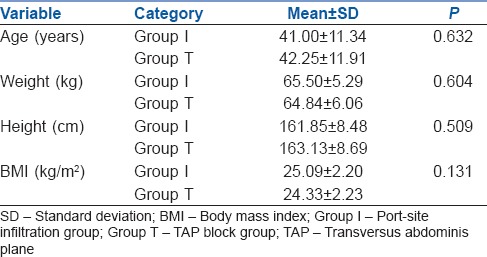
A total of 80 patients were recruited for the study and all patients completed the study [Figure 1]. Both groups were comparable with respect to sex, ASA physical status and educational status. There was no significant difference between the groups with respect to demographic variables such as age, weight, height and BMI [Table 1].
Figure 1.
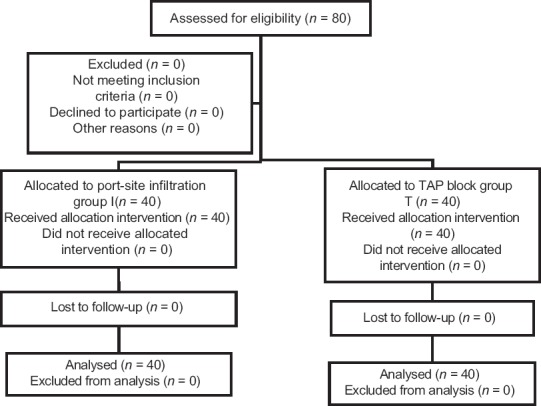
Consort flow chart
Table 1.
Comparison of demographic variables of study population with P values
The mean first rescue analgesic (tramadol) requirement was 141.8 ± 60.01 mg in Group I and 48.69 ± 36.14 mg in Group T (P = 0.001). Four participants in Group I required second rescue analgesic diclofenac but none in Group T. The duration of analgesia was 290.7 ± 67.03 min in Group I and 510.35 ± 154.55 min in Group T (P = 0.001). The mean NRS at first analgesic request was 6.08 ± 0.92 in Group I and 4.38 ± 0.490 in Group T (P = 0.001).
The mean NRS for pain was zero at 1 h in both the groups. The mean NRS at 2, 3, 6, 12 and 24 h in Group I and Group T is summarised in Table 2. The mean pain scores at all time frames except at 1 h were lower in Group T compared to Group I [Figure 2] and were statistically significant (P < 0.05).
Table 2.
Numerical Rating Scale of study groups with P value
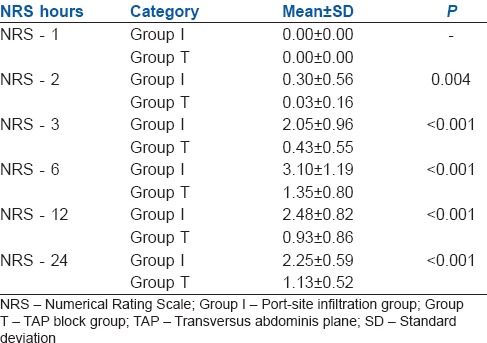
Figure 2.
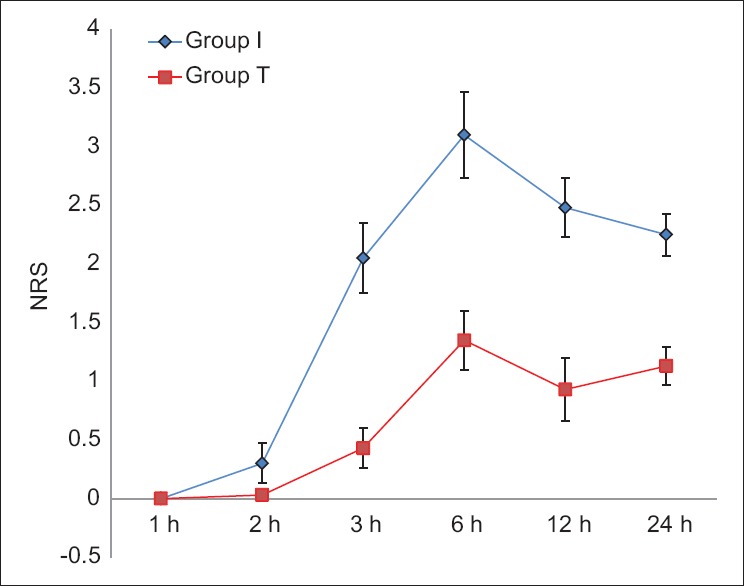
Line graph comparing Numerical Rating Scale at 1, 2, 3, 6, 12 and 24 h after transversus abdominis plane block (Group T) and port-site infiltration (Group I)
Two patients had vomiting in the post-operative period in Group I, but there was no adverse effect in Group T. The difference in incidence of this adverse effect was not statistically significant (P = 0.152). No other adverse effects were noted in either group.
DISCUSSION
Cholecystectomy is a common surgical procedure done for various gall bladder disease conditions including cholelithiasis. It is proven that lack of effective post-operative pain control will not only result in adverse physiological effects but also can end in chronic pain.[8] Because of the excellent quality of analgesia provided by local anaesthetics without much side effects such as sedation, they are widely used for post-operative analgesia in various surgeries including laparoscopic cholecystectomy. Amongst the different analgesic techniques, port-site infiltration and TAP block are found to be very effective in providing post-operative analgesia.[9,10,11] In the present study, a comparison was done between these two methods for post-operative analgesia in laparoscopic cholecystectomy.
Even though the classic approach initially described[12] was through the lumbar triangle of petit, to cover the upper abdominal dermatomes, anterior subcostal approach was described.[13] TAP block was not free of complications[14] until the introduction of ultrasound in regional anaesthesia. Ultrasound-guided TAP block helps in clearly demarcating the anatomy, increases the margin of safety and help in deposition of local anaesthetic under vision which increases the success rate and reduces the volume of drug needed for effective block.[15] Hence, in our study, USG-guided subcostal TAP block was used for post-operative analgesia.
In this study, port-site infiltration was done with 0.5% bupivacaine at four port sites, using total volume of 20 ml of bupivacaine. In a previous study[16] comparing 0.25% and 0.5% of levobupivacaine and placebo for TAP block, comparable pain scores and post-operative analgesic requirement were obtained between the two different doses of levobupivacaine. So here, TAP block was performed using smaller concentration (0.25%) of bupivacaine to reduce local anaesthetic toxicity if any. In both port-site infiltration and TAP block, a total of 100 mg of bupivacaine was used to avoid confounding due to dose differences.
In our study, of the 80 participants, 40 received port-site infiltration (Group I) and 40 received USG-guided bilateral subcostal TAP block (Group T). The groups were comparable with respect to sex, ASA physical status, age, height, BMI and education status.
NRS for pain was zero at 1 h in both the groups. That means port-site infiltration and TAP block are effective in providing analgesia in the 1st h. NRS was significantly lower in Group T compared to Group I at all other time frames. The mean NRS at first analgesic request was 6.08 ± 0.92 in Group I and 4.38 ± 0.49 in Group T which shows that the intensity of pain was less in TAP group compared to infiltration. In a study[9] conducted on 43 patients, the mean pain scores at 1 h and 4 h were less in TAP block compared to port-site infiltration. Our study results were also consistent with a previous study[17] done for post-operative analgesia after laparoscopic cholecystectomy with lower pain scores after TAP block compared to port-site infiltration.
The duration of analgesia was 290.7 ± 67.03 min in Group I and 510.35 ± 154.55 min in Group T. Long duration of analgesia may be due to slow absorption of the drug from the less vascular tissue plane between the muscles in TAP block compared to tissue infiltration. Mean tramadol requirement was 141.8 ± 60.01 mg in Group I and 48.69 ± 36.14 mg in Group T. Four patients required second rescue analgesic diclofenac for pain control in Group I but none in Group T. From this, it is evident that TAP block reduces the overall post-operative analgesic requirement and has got both opioid and non-steroidal anti-inflammatory drug-sparing effect in the post-operative period which are consistent with above studies.[9,17] There were two episodes of vomiting in Group I which was not statistically significant when compared to Group T. Higher incidence of vomiting in Group I may be due to greater tramadol requirement in Group I for pain control.
In a retrospective study[7] where 51 patients underwent day-care laparoscopic cholecystectomy were analysed for post-operative pain scores, patient satisfaction scores and post-operative fentanyl requirement in recovery and cost for the post-operative analgesic technique were used. In contrast to our study, there was no significant difference in pain scores and post-operative opioid consumption between these groups. Here, ropivacaine was used to administer TAP block without ultrasound guidance that may be the reason for the difference in outcome compared to our study. In another study,[18] there was no clinically significant difference in pain scores and post-operative analgesic requirement between TAP block and port-site infiltration even though the duration of analgesia and severity of pain were not assessed. Here, only 15 ml of 0.5% ropivacaine in each side with the classic approach was used for TAP block.
In another study post-operative morphine consumption and pain scores were assessed after giving TAP block or port-site infiltration after single-incision laparoscopic cholecystectomy.[19] In contrast to our study, they found that TAP block was not effective in reducing the 24 h morphine consumption even though it provided analgesia in the early post-operative period.
In this study, analgesic techniques were administered postoperatively, but if it was administered preoperatively, it might have decreased the intraoperative pain and opioid requirement also thereby benefitting the patient. Large volume of drug was used in the study, and even though there were no adverse events related to local anaesthetic toxicity, monitoring the plasma level of bupivacaine will help to reduce local anaesthetic toxicity if it occurs and will also help to calculate the minimum effective volume of drugs for TAP block which is yet to be discovered. Dynamic pain assessment is more important than static pain to facilitate early mobilisation which was not assessed here. Overall patient satisfaction scale assessment was not done which is the ultimate aim of all post-operative analgesic techniques. Further studies are required to show the analgesic efficacy of USG-guided TAP block in various other abdominal surgeries using different local anaesthetics at different doses and continuous catheter techniques.
CONCLUSION
USG-guided bilateral subcostal TAP block is effective and found to be superior in providing post-operative analgesia after laparoscopic cholecystectomy with reduced pain scores, longer duration and less post-operative analgesic requirement compared to port-site infiltration.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Zacks SL, Sandler RS, Rutledge R, Brown RS., Jr A population-based cohort study comparing laparoscopic cholecystectomy and open cholecystectomy. Am J Gastroenterol. 2002;97:334–40. doi: 10.1111/j.1572-0241.2002.05466.x. [DOI] [PubMed] [Google Scholar]
- 2.Ahmad NZ, Byrnes G, Naqvi SA. A meta-analysis of ambulatory versus inpatient laparoscopic cholecystectomy. Surg Endosc. 2008;22:1928–34. doi: 10.1007/s00464-008-9867-2. [DOI] [PubMed] [Google Scholar]
- 3.Vaughan J, Gurusamy KS, Davidson BR. Day-surgery versus overnight stay surgery for laparoscopic cholecystectomy. Cochrane Database Syst Rev. 2013;7:CD006798. doi: 10.1002/14651858.CD006798.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kum CK, Wong CW, Goh PM, Ti TK. Comparative study of pain level and analgesic requirement after laparoscopic and open cholecystectomy. Surg Laparosc Endosc. 1994;4:139–41. [PubMed] [Google Scholar]
- 5.Tran TM, Ivanusic JJ, Hebbard P, Barrington MJ. Determination of spread of injectate after ultrasound-guided transversus abdominis plane block: A cadaveric study. Br J Anaesth. 2009;102:123–7. doi: 10.1093/bja/aen344. [DOI] [PubMed] [Google Scholar]
- 6.Altuntaş G, Akkaya ÖT, Özkan D, Sayın MM, Balas Ş, Özlü E, et al. Comparison of intraabdominal and trocar site local anaesthetic infiltration on postoperative analgesia after laparoscopic cholecystectomy. Turk J Anaesthesiol Reanim. 2016;44:306–11. doi: 10.5152/TJAR.2016.75983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kadam VR, Howell S, Kadam V. Evaluation of postoperative pain scores following ultrasound guided transversus abdominis plane block versus local infiltration following day surgery laparoscopic cholecystectomy-retrospective study. J Anaesthesiol Clin Pharmacol. 2016;32:80–3. doi: 10.4103/0970-9185.168195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stiff G, Rhodes M, Kelly A, Telford K, Armstrong CP, Rees BI, et al. Long-term pain: Less common after laparoscopic than open cholecystectomy. Br J Surg. 1994;81:1368–70. doi: 10.1002/bjs.1800810939. [DOI] [PubMed] [Google Scholar]
- 9.Tolchard S, Davies R, Martindale S. Efficacy of the subcostal transversus abdominis plane block in laparoscopic cholecystectomy: Comparison with conventional port-site infiltration. J Anaesthesiol Clin Pharmacol. 2012;28:339–43. doi: 10.4103/0970-9185.98331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sinha S, Palta S, Saroa R, Prasad A. Comparison of ultrasound-guided transversus abdominis plane block with bupivacaine and ropivacaine as adjuncts for postoperative analgesia in laparoscopic cholecystectomies. Indian J Anaesth. 2016;60:264–9. doi: 10.4103/0019-5049.179464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hasaniya NW, Zayed FF, Faiz H, Severino R. Preinsertion local anesthesia at the trocar site improves perioperative pain and decreases costs of laparoscopic cholecystectomy. Surg Endosc. 2001;15:962–4. doi: 10.1007/s004640000294. [DOI] [PubMed] [Google Scholar]
- 12.Rafi AN. Abdominal field block: A new approach via the lumbar triangle. Anaesthesia. 2001;56:1024–6. doi: 10.1046/j.1365-2044.2001.02279-40.x. [DOI] [PubMed] [Google Scholar]
- 13.Carney J, Finnerty O, Rauf J, Bergin D, Laffey JG, Mc Donnell JG, et al. Studies on the spread of local anaesthetic solution in transversus abdominis plane blocks. Anaesthesia. 2011;66:1023–30. doi: 10.1111/j.1365-2044.2011.06855.x. [DOI] [PubMed] [Google Scholar]
- 14.Lancaster P, Chadwick M. Liver trauma secondary to ultrasound-guided transversus abdominis plane block. Br J Anaesth. 2010;104:509–10. doi: 10.1093/bja/aeq046. [DOI] [PubMed] [Google Scholar]
- 15.Hebbard P. Subcostal transversus abdominis plane block under ultrasound guidance. Anesth Analg. 2008;106:674–5. doi: 10.1213/ane.0b013e318161a88f. [DOI] [PubMed] [Google Scholar]
- 16.Ra YS, Kim CH, Lee GY, Han JI. The analgesic effect of the ultrasound-guided transverse abdominis plane block after laparoscopic cholecystectomy. Korean J Anesthesiol. 2010;58:362–8. doi: 10.4097/kjae.2010.58.4.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saxena R, Joshi S, Srivastava K, Tiwari S, Sharma N, Valecha UK, et al. Comparative study of ultrasound-guided abdominal field blocks versus port infiltration in laparoscopic cholecystectomies for post-operative pain relief. Indian J Anaesth. 2016;60:578–83. doi: 10.4103/0019-5049.187790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ortiz J, Suliburk JW, Wu K, Bailard NS, Mason C, Minard CG, et al. Bilateral transversus abdominis plane block does not decrease postoperative pain after laparoscopic cholecystectomy when compared with local anesthetic infiltration of trocar insertion sites. Reg Anesth Pain Med. 2012;37:188–92. doi: 10.1097/AAP.0b013e318244851b. [DOI] [PubMed] [Google Scholar]
- 19.Bava EP, Ramachandran R, Rewari V, Chandralekha, Bansal VK, Trikha A, et al. Analgesic efficacy of ultrasound guided transversus abdominis plane block versus local anesthetic infiltration in adult patients undergoing single incision laparoscopic cholecystectomy: A randomized controlled trial. Anesth Essays Res. 2016;10:561–7. doi: 10.4103/0259-1162.186620. [DOI] [PMC free article] [PubMed] [Google Scholar]


