INTRODUCTION
Quadratus lumborum block (QLB) is a technique for postoperative analgesia after abdominal surgeries. Nomenclature on types of QLB keeps changing.[1] An ultrasound-guided transmuscular quadratus lumborum (TQL) block, which involves passage of the needle through the QL muscle and injection of the local anaesthetic (LA) into the anterior aspect of the fascial interspace between the QL and psoas muscle is also called the QLB3.[2] There have been case reports on the use QLB block in abdominal surgery as an analgesic technique in paediatric and adult patients.[3,4,5] There is a general paucity of literature on continuous use of TQL block in adults for major abdominal surgery.[6,7] We have previously reported TQL block performed at L4 resulting in transient paraesthesia of the leg in one case.[6] In view of this issue, we performed the same block at L2 level without adverse effect. So far, no studies examined the analgesic effect of TQL catheters placed at different levels utilizing the anterior approach for major abdominal surgery. The aim of this study was to evaluate the efficacy of these blocks at two levels in open midline incision surgery.
METHODS
Ten consecutive patients (7 males, 3 females) undergoing elective open abdominal surgery with any midline incision were recruited in 2016 at The Queen Elizabeth Hospital. Patients unable to provide consent and allergic to fentanyl, ropivacaine, and oral opioids were excluded. Human Research Ethics Committee approval was obtained. All patients received general anaesthesia with endotracheal intubation and were administered intermittent doses of Fentanyl for analgesia. The patients were placed in a lateral position following the surgical procedure and prior to extubation to insert the QLB catheters under ultrasound guidance using a 2–5-MHz frequency curved probe (SonoSite X-Porte, SonositeInc, Bothell, Washington, USA). A lower approach (L4) was used in five patients where the probe was placed transversely in the posterior axillary line and moved towards L4 transverse process (iliac crest level). In the remaining five patients the probe was placed close to the transverse process at the L2 level. After identifying the QL muscle above the transverse process, an 18-gauge Touhy's needle was introduced at the respective transverse process, in a posterior to anterior direction, in plane through the QL muscle by saline hydro-dissection to reach the anterior thoracolumbar fascia [Figures 1 and 2]. A bolus of 20 ml of ropivacaine 0.5% was administered followed by bilateral catheter insertion directing cephalad to the depth of 3–4 cm to infuse ropivacaine 0.2% at 5–8 ml/h each side for 48 h. Patients were also administered multimodal analgesia with 1 g Paracetamol every 6 h, Dexamethasone 8 mg, and Fentanyl PCA. Parameters measured by acute pain service were dermatomal levels, pain scores on cough, and total analgesic consumption in the 48 h after surgery. Pain score ranged from 0 (no pain) to 10 (worst possible pain).
Figure 1.
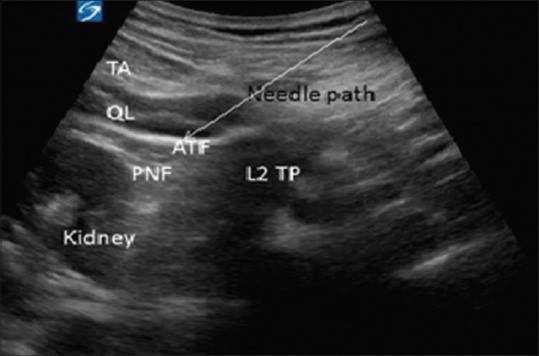
The sonoanatomy of TQL block at L2. TA = Transrversus abdominis, QL = Quadratus lumborum muscle, ATF = Anterior thoracolumbar fascia, PNF = Perinephric fascia, TP = Transverse process
Figure 2.
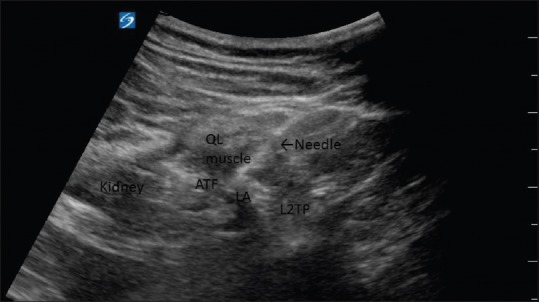
The ultrasound guided TQL with LA injected at L2 level. QL = Quadratus lumborum muscle, ATF = Anterior thoracolumbar fascia, TP= Transverse process
RESULTS
Table 1 provides details of patient characteristics and the nerve block. Mean pain score during recovery was slightly higher among patients who had the block at L2 when compared to those at L4 (L2 v L4: 4.20 v 1.20). However, group differences were negligible at both time points (24 h: L2 v L4: 5.4 v 5.0) (48 h: L2 v L4: 5.6 v 5.6).
Table 1.
The demographics, dermatomes, pain scores, and analgesia used
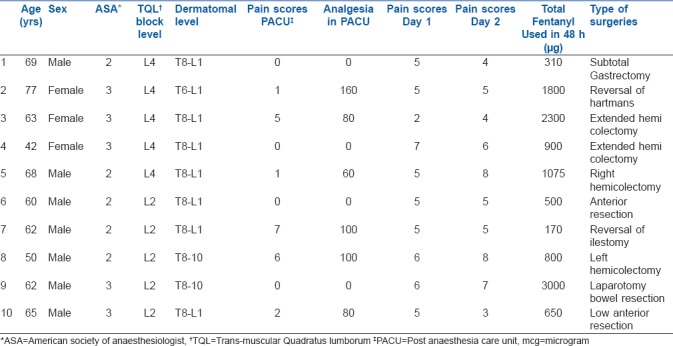
Mean fentanyl consumption over the 48 h was 1024 and 1277 mcg for block performed at L2 and L4, respectively. Femoral nerve palsy and hypotension occurred when blocks were performed at L4; however, there were no adverse events at L2. There were no complications relating to catheter, infections, or systemic side effects to ropivacaine during the study period.
DISCUSSION
Continuous TQL block in abdominal open surgery reduced pain scores; the lower-level (L4) approach resulted in adverse effects such as hypotension and nerve palsy. This nerve palsy is possibly from the LA tracking to the lower lumbar roots and its proximity to the lumbar plexus in psoas muscle. Unanticipated femoral nerve palsy was also reported after transversalis fascia block and QLB.[8,9] Unexplained hypotension following this block has also been reported.[10] We chose Borglum's QLB3, reporting anaesthesia from T7 to L1 based on traces of contrast in the thoracic paravertebral space.[11] There are no such studies performed at L2 level.
Ueshima reported that a single shot technique was effective for almost 24 h with dermatomes level up to T7.[12] We achieved dermatomal level up to T8, but there is a need for a technique that achieves cephalad block with catheters providing prolonged analgesia. However, because T6 is ideal for an incision close to xiphoid, there may be room for improvement on cephalad spread in terms of bolus dosing and infusions.
TQL catheters have the advantage of analgesic benefit for both upper and lower abdominal surgery. The lower iliac crest level at L4 and higher near L1 spine, near the 12th rib have been established as approaches to TQL block.[2,13] At the L2 level we would qualify for the in between (mid-level) TQL block. At this stage we are unsure whether high,[13] mid or low level[2] TQL technique is optimal; however, this series suggests that L2 Rao's technique has an advantage with no adverse effects. Larger studies and randomized control trials are warranted to establish the efficacy and safety of these techniques. This study is limited by the small case series.
CONCLUSION
A TQL catheter placed either at L4 and L2 levels reduced postoperative pain scores and analgesic use after major abdominal surgeries. Absence of neurological adverse events in the L2 group may suggest its possible safety.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We thank Dr Venkatesan Thiruvenkatarajan for his editing and Karen Taylor and P Williams for spell check.
REFERENCES
- 1.El Boghdadly K EH, Short A, Chin KJ. Quadratus lumborum block nomenclature and anatomical considerations. Reg Anesth Pain Med. 2016;41:548–9. doi: 10.1097/AAP.0000000000000411. [DOI] [PubMed] [Google Scholar]
- 2.Borglum J MB, Jensen K, Lonnqvist PA, ChristensenAF, Sauter A, et al. Ultrasound-guided transmuscular quadratus lumborum blockade. Br J Anaesth. 2013 [Google Scholar]
- 3.Baidya DK, Maitra S, Arora MK, Agarwal A. Quadratus lumborum block: An effective method of perioperative analgesia in children undergoing pyeloplasty. J Clin Anaesth. 2015;27:694–6. doi: 10.1016/j.jclinane.2015.05.006. [DOI] [PubMed] [Google Scholar]
- 4.Chakraborty A, Goswami J, Patro V. Ultrasound-guided continuous quadratus lumborum block for postoperative analgesia in a pediatric patient. A A Case Rep. 2015;4:34–6. doi: 10.1213/XAA.0000000000000090. [DOI] [PubMed] [Google Scholar]
- 5.Shaaban M, Esa WA, Maheshwari K, Elsharkawy H, Soliman LM. Bilateral Continuous Quadratus Lumborum Block for Acute Postoperative Abdominal Pain as a Rescue After Opioid-Induced Respiratory Depression. A A Case Rep. 2015;5:107–11. doi: 10.1213/XAA.0000000000000188. [DOI] [PubMed] [Google Scholar]
- 6.Kadam VR, Taylor L, Tong M. Continuous Transmuscular Quadratus Lumborum Block Catheter Technique for Post-Operative Pain Relief in Upper Abdominal Surgery-Case Report. J Anesth Pain Med. 2016;1:1–2. [Google Scholar]
- 7.Warusawitharana C, Basar SHMA, Jackson BL, Niraj G. Ultrasound guided continuous transmuscular quadratus lumborum analgesia for open renal surgery: A case series. J Clin Anesth. 2017;42:100–1. doi: 10.1016/j.jclinane.2017.08.025. [DOI] [PubMed] [Google Scholar]
- 8.Lee S, Goetz T, Gharapetian A. Unanticipated motor weakness with ultrasound-guided transversalis fascia plane block. A A Case Rep. 2015;5:124–5. doi: 10.1213/XAA.0000000000000237. [DOI] [PubMed] [Google Scholar]
- 9.Wikner M. Unexpected motor weakness following quadratus lumborum block for gynaecological laparoscopy. Anaesthesia. 2017;72:230–2. doi: 10.1111/anae.13754. [DOI] [PubMed] [Google Scholar]
- 10.Sá M, Cardoso JM, Reis H, Esteves M, Sampaio J, Gouveia I, et al. Quadratus lumborum block: Are we aware of its side effects? A report of 2 cases. Rev Bras Anestesiol. 2017;23:S0034–7094. [Google Scholar]
- 11.Carney J, Finnerty O, Rauf J, Bergin D, Laffey JG, Mc Donnell JG. Studies on the spread of local anaesthetic solution in transversus abdominis plane blocks. Anaesth Intensive Care. 2011;66:1023–30. doi: 10.1111/j.1365-2044.2011.06855.x. [DOI] [PubMed] [Google Scholar]
- 12.Ueshima H, Yoshiyama S, Otake H. The ultrasound-guided continuous transmuscular quadratus lumborum block is an effective analgesia for total hip arthroplasty. J Clin Anesth. 2016;35:235–7. doi: 10.1016/j.jclinane.2015.12.033. [DOI] [PubMed] [Google Scholar]
- 13.Elsharkawy H. Quadratus lumborum block with paramedian sagittal oblique (subcostal) approach. Anaesthesia. 2016;71:241–2. doi: 10.1111/anae.13371. [DOI] [PubMed] [Google Scholar]


