Abstract
BACKGROUND
The increased incidence of bile duct injuries (BDIs) after the adoption of laparoscopic cholecystectomy has been well documented. However, the longitudinal impact of bile leaks and BDIs on survival and healthcare use have not been studied adequately. The aims of this analysis were to determine the incidence, long-term outcomes, and costs of bile leaks and ductal injuries in a large population.
STUDY DESIGN
The California Office of Statewide Health Planning and Development database was queried from 2005 to 2014. Bile leaks, BDIs, and their management strategy were defined. Survival was calculated by Kaplan-Meier failure estimates with multivariable regression and propensity analyses. Cost analyses used inflation adjustments and institution-specific cost-to-charge ratios.
RESULTS
Of 711,454 cholecystecomies, bile leaks occurred in 3,551 patients (0.50%) and were managed almost exclusively by endoscopists. Bile duct injuries occurred in 1,584 patients (0.22%) with 84% managed surgically. Patients with a bile leak were more likely to die at 1 year (2.4% vs 1.4%; odds ratio 1.85; p < 0.001). Similarly, BDI patients had an increased 1-year mortality (7.2% vs 1.3%; odds ratio 2.04; p < 0.0001). Survival of BDI patients was better with an operative approach (odds ratio 0.19; p < 0.001) when compared with endoscopic management. Operatively managed BDIs were also associated with fewer emergency department visits and readmissions, as well as lower cumulative costs at 1 year ($60,539 vs $118,245; p < 0.001).
CONCLUSIONS
The 0.22% incidence of BDIs observed in California is lower than reported in the first decade after the introduction of laparoscopic cholecystectomy. Bile leaks are 2.3 times more common than BDIs. Patients with a bile leak or BDI have diminished survival. Surgical repair of a BDI leads to enhanced survival and reduced cumulative cost compared with endoscopic management.
Laparoscopic cholecystectomy is one of the most commonly performed operations in the US, accounting for approximately 1.2 million cases per year.1 When undertaken electively, this procedure is safe, with more than half of the cases performed on an outpatient basis with same-day discharge. However, major morbidity occurs in approximately 5% of patients,2 with the most morbid complication being a bile duct injury (BDI). After the adoption of laparoscopic cholecystectomy, the incidence of BDI has increased from 0.1% to 0.2%3 during the open cholecystectomy era to 0.4% to 0.6%.4,5 However, recent analyses from Europe6 and the US7,8 suggest that the incidence of BDIs has returned to prelaparoscopy rates.
Although the early clinical outcomes of BDIs have been well documented, the longitudinal impact of bile leaks and ductal injuries on survival, healthcare use, and cost have been less well defined. Most patients with BDIs are referred to tertiary centers for surgical, endoscopic, or percutaneous management. As such, longitudinal tracking of these patients with complete follow-up is difficult. Additionally, little is known about the incidence or long-term consequences of cystic duct leaks, which are most commonly managed successfully in the short-term by endoscopists. As part of a quality review effort, the California Office of Statewide Health Planning and Development (OSHPD) contracted the authors to assess these issues further. The aims of this analysis were to determine the incidence and long-term outcomes of bile leaks and ductal injuries managed surgically, endoscopically, or percutaneously in a large population.
METHODS
California Office of Statewide Health Planning and Development
All patients who underwent a cholecystectomy in California from 2005 to 2014 were identified from the California Office of Statewide Health Planning and Development (OSHPD) database. The California OSHPD is a unique database that captures all episodes of patient care across California-licensed facilities regardless of age or insurance status. Each patient is assigned a unique identifier to capture his or her progression through the healthcare system (inpatient, ambulatory surgery, and emergency department care episodes) over time. Additionally, this database is linked to the California Department of Public Health Death Statistical Master File for mortality records. The OSHPD is 1 of 12 departments within the California Health and Human Services Agency and maintains this database for all California-licensed facilities. A cholecystectomy expert panel, comprising the coauthors, was assembled by the California OSHPD. In conjunction with consultants from the Hospital Quality Institute, the expert panel determined appropriate inclusion criteria, identifiable outcomes and definitions using ICD-9 diagnoses and procedure codes and CPT codes, where appropriate.
Inclusion criteria
Inclusion criteria were patients undergoing a cholecystectomy with a benign pathology diagnosis, including acute cholecystitis, biliary colic, choledocholithiasis, or gallstone pancreatitis. Patients undergoing a laparoscopic or open cholecystectomy were identified by ICD-9 procedure codes of 51.21, 51.22, 51.23, or 51.24 as a primary procedure in the inpatient database. Patients with CPT codes 47562–64, 47600, 47605, 47610, 47612, 47620, 49310, 49311, and 56340–42 as a primary procedure in the ambulatory surgery database were also identified. The benign pathology diagnoses were identified with primary ICD-9 diagnosis codes 574.0 to 574.2, 575.0 to 575.8, 789.0, and 789.01 (eTable 1).
Exclusion criteria
Patients who underwent any other abdominal surgical procedures at the same time as the cholecystectomy; had an earlier cholecystostomy tube; or had a diagnosis of gall-bladder, liver, ampullary, bile duct, pancreatic, or duodenal cancer at the time of or after cholecystectomy were excluded. Additionally, patients who underwent cholecystectomy for initially presumed benign gallbladder neoplasms, but returned with malignancy on the final pathology and subsequently underwent cancer treatments within 1 year of cholecystectomy were also excluded.
Variables definition
Bile leaks were defined as patients undergoing an isolated ERCP or percutaneous transhepatic cholangiography within 4 weeks after cholecystectomy. Patients were censored from bile leak evaluation if they had an additional diagnosis of retained stones. Bile duct injury managed operatively was defined as patients undergoing choledochoenterostomy or suture of the common bile duct at the time of or after cholecystectomy, as well as patients undergoing a hepatectomy or liver transplantation after cholecystectomy, as defined previously in the literature.9–11 Bile duct injury managed endoscopically was defined as patients undergoing more than 1 ERCP within a year after cholecystectomy. Bile duct injury managed percutaneously was defined as patients undergoing 1 or more percutaneous transhepatic cholangiography, more than 4 weeks but within 1 year after cholecystectomy. Patients were censored from common bile duct injury evaluation if they had a diagnosis of gallbladder, liver, ampullary, distal bile duct, pancreatic, or duodenal neoplasms after cholecystectomy, but before the procedures mentioned previously. Hospital teaching status was hand-coded as institutions with a surgical residency, those affiliated with a surgical residency, or those not affiliated with a surgical residency.
Mortality analysis
The mortality analysis included patients undergoing cholecystectomy from 2005 to 2013, given that the mortality records for 2014 were not available to be linked to the OSHPD database. The survival analysis was adjusted for the following covariates: age, sex, race, payer status, Charlson’s Comorbidity Index score,12,13 elective vs nonelective surgery, outpatient vs inpatient setting, sepsis, cholangitis, and hospital teaching status. Cox proportional hazard rates were used to compare cumulative incidences of deaths, with follow-up time defined as the minimum time between date of operation to time of outcomes, censoring death, or end of study period.
Cost analysis
First, an inflation adjustment of historical dollars to 2015 dollars was performed. Hospital charges were then converted to cost estimates by comparing Net Patient Revenue, as reported by California Hospital Annual Financial Data, vs total hospital charges for all patients that year. Cumulative costs were calculated longitudinally by totaling the total cost incurred by any healthcare episode (ambulatory, inpatient, or emergency department visits).
Statistical analysis
Fisher’s exact test was used to compare categorical variables. Shapiro-Wilk test was used to assess for normality of the distribution for continuous variables. All results for continuous variables were expressed as mean ± SD, and skewed variables were expressed as medians and inter-quartile ranges. Student’s t-test was used to compare continuous variables with normal distribution, and Kruskal-Wallis was used for continuous variables with non-normal distributions. Covariates with p values <0.1 and clinically meaningful variables were included in the logistic regression model. Regression analyses were performed clustering on individual hospitals to account for intraclass correlation. Propensity score matching of patients based on the covariates mentioned was performed for the survival analysis with a caliper of ±0.05 to obtain adjusted longitudinal mortality graphs. All tests were performed 2-sided, and a significance level of p < 0.05 was considered to indicate statistical significance. All statistical analyses were performed using Inter-cooled STATA software, version 12.0 (Stata Corp).
RESULTS
Patient demographics
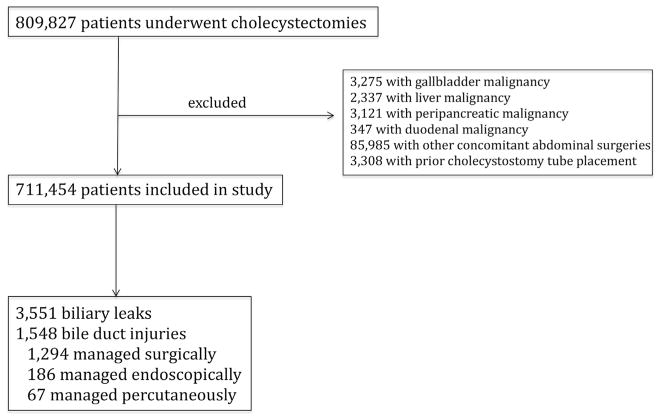
We identified 809,827 patients who underwent cholecystectomies from 2005 to 2014. After excluding patients with periampullary malignancy, those who underwent other concomitant abdominal procedures and those with earlier cholecystostomy tube placement, 711,454 patients were eventually included in the study. Of these, 3,551 (0.50%) patients had a bile leak; 1,548 (0.22%) patients had BDI, of which 1,294 (84%) were managed operatively and 186 (12%) were managed endoscopically (Fig. 1). An additional 5,194 (0.73%) patients underwent endoscopic procedures for retained bile duct stones. Most patients who underwent a cholecystectomy were non-Hispanic white females, with a median age of 47 years (interquartile range 33 to 62 years) (Table 1). Only 3.3% of all patients had a Charlson’s Comorbidity Index score of >3, and most patients had private insurance, followed by Medicare and Medicaid. Half of all cholecystectomies were performed laparoscopically on an elective, outpatient basis, followed by nonelective, inpatient setting. Patients with bile leaks were similar to those without bile leaks or BDIs (Table 1). Patients with a BDI were more likely to be older, Asian, and to have had their cholecystectomy performed in an open, scheduled, inpatient setting (Table 1).
Figure 1.
Flow diagram of the study population.
Table 1.
Demographics for Patients with No Bile Leaks or Bile Duct Injuries, Patients with Bile Leaks, and Patients with Bile Duct Injuries
| Characteristic | Patients with no bile leak or duct injury (n = 706,355) | Patients with bile leak (n = 3,551) | Patients with bile duct injury (n = 1,548) | p Value | |||
|---|---|---|---|---|---|---|---|
|
|
|
|
|||||
| n | % | n | % | n | % | ||
| Age | <0.001 | ||||||
|
| |||||||
| ≤19 y | 251,891 | 35.7 | 1,406 | 39.6 | 427 | 27.7 | |
|
| |||||||
| 39 to 50 y | 129,319 | 18.3 | 662 | 18.7 | 259 | 16.8 | |
|
| |||||||
| 50 to 65 y | 177,337 | 25.1 | 860 | 24.2 | 378 | 24.6 | |
|
| |||||||
| ≥65 y | 147,773 | 20.9 | 623 | 17.5 | 476 | 30.9 | |
|
| |||||||
| Sex, female | 513,467 | 72.7 | 2,646 | 74.5 | 1,025 | 66.6 | <0.001 |
|
| |||||||
| Race | <0.001 | ||||||
|
| |||||||
| Non-Hispanic white | 336,407 | 48.1 | 1,799 | 51.0 | 714 | 46.7 | |
|
| |||||||
| Hispanic | 259,895 | 37.2 | 1,288 | 36.5 | 482 | 31.4 | |
|
| |||||||
| Asian | 49,292 | 7.1 | 229 | 6.5 | 201 | 13.2 | |
|
| |||||||
| Black | 30,792 | 4.4 | 124 | 3.5 | 76 | 5.0 | |
|
| |||||||
| Native American/other | 22,807 | 3.2 | 91 | 2.5 | 56 | 3.7 | |
|
| |||||||
| Charlson Comorbidity Index score >3 | 23,469 | 3.3 | 111 | 3.1 | 88 | 5.7 | <0.001 |
|
| |||||||
| Payer status | <0.001 | ||||||
|
| |||||||
| Private | 386,762 | 54.8 | 1,945 | 54.8 | 694 | 45.1 | |
|
| |||||||
| Medicare | 154,921 | 21.9 | 677 | 19.1 | 468 | 30.4 | |
|
| |||||||
| Medicaid | 109,433 | 15.5 | 627 | 17.7 | 250 | 16.3 | |
|
| |||||||
| Self-pay/non-federal indigent | 51,714 | 7.3 | 291 | 8.2 | 122 | 7.9 | |
|
| |||||||
| Other | 3,403 | 0.5 | 11 | 0.2 | 5 | 0.3 | |
|
| |||||||
| Setting | <0.001 | ||||||
|
| |||||||
| Outpatient | 375,703 | 53.2 | 1,629 | 45.9 | 261 | 16.9 | |
|
| |||||||
| Inpatient | |||||||
|
| |||||||
| Laparoscopic | |||||||
|
| |||||||
| Unscheduled | 253,828 | 35.9 | 1,550 | 43.6 | 310 | 20.0 | |
|
| |||||||
| Scheduled | 41,405 | 5.9 | 201 | 5.7 | 83 | 5.4 | |
|
| |||||||
| Open | |||||||
|
| |||||||
| Unscheduled | 26,131 | 3.7 | 133 | 3.7 | 564 | 36.4 | |
|
| |||||||
| Scheduled | 9,288 | 1.3 | 38 | 1.1 | 330 | ||
|
| |||||||
| Facility performing cholecystectomy | <0.001 | ||||||
|
| |||||||
| No surgical residency | 531,300 | 75.2 | 2,631 | 74.1 | 1,079 | 70.1 | |
|
| |||||||
| Affiliated with surgical residency | 140,237 | 19.9 | 734 | 20.7 | 351 | 22.8 | |
|
| |||||||
| Surgical residency | 34,783 | 4.9 | 186 | 5.2 | 110 | 7.1 | |
Mortality analysis
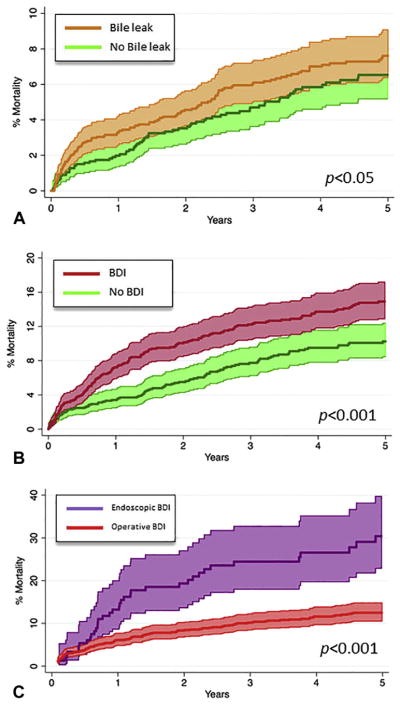
Patients with a bile leak were more likely to die at 1 year (2.4% vs 1.4%; p < 0.001) and 3 years (5.8% vs 4.8%; p < 0.05) when compared with patients without a bile leak (Fig. 2A). This difference persisted on multivariate regression (odds ratio [OR] 1.8; 95% CI 1.4 to 2.3; p < 0.001). Similarly, BDI patients had increased 1-year (7.2% vs 1.3%; p < 0.001) and 5-year mortality rates (14.5% vs 4.8%; p < 0.001), and this difference persisted on multivariate regression (OR 2.0; 95% CI 1.6 to 2.6; p < 0.001) (Fig. 2B). When analyzed in an intention to treat fashion, BDI patients managed operatively had lower 1-year (6.0% vs 15.0%; p < 0.001) and 5-year mortality rates (12.4% vs 31.9%; p < 0.001) when compared with patients managed endoscopically (Fig. 2C). This difference persisted on adjusted analysis (hazard ratio 0.2; 95% CI 0.1 to 0.4; p < 0.001). Propensity scores were used to match patients with bile leaks and BDIs to those without to produce an adjusted mortality curve.
Figure 2.
(A) Longitudinal incidence of mortality for propensity-matched patients with and without bile leaks. (B) Longitudinal incidence of mortality for propensity-matched patients with and without bile duct injuries (BDIs). (C) Longitudinal incidence of mortality for propensity-matched patients with BDIs managed operatively and those managed endoscopically. Shaded areas include 95% CIs.
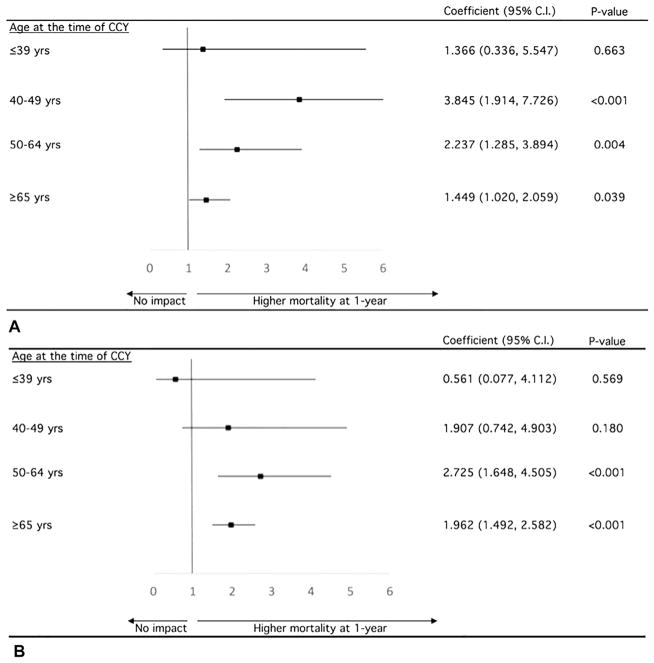
Impact of age on bile leaks and bile duct injury mortality
When stratified by age groups, bile leak was associated with an increased 1-year mortality in patients aged 40 to 49 years (OR 3.85; p < 0.001), 50 to 64 years (OR 2.24; p = 0.004), and 65 years and older (OR 1.45; p = 0.039), but not in patients younger than 40 years old (Fig. 3A). Similarly, BDI was associated with increased 1-year mortality in patients aged 50 to 64 years (OR 2.73, p <0.001) and 65 years and older (OR 1.96; p < 0.001), but not in patients younger than 50 years old (Fig. 3B).
Figure 3.
(A) Adjusted impact of bile leaks on mortality in different age groups. (B) Adjusted impact of bile duct injuries on mortality in different age groups. CCY, cholecystectomy.
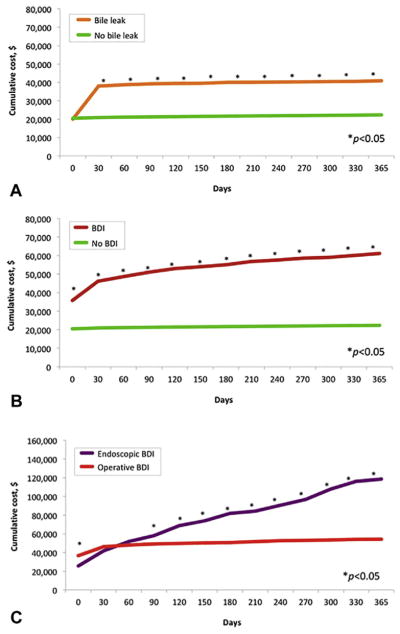
Cost analysis
The cost of the index hospitalization was not different for patients with bile leaks ($20,040) and those without ($20,508; p =0.131) (Fig. 4A). However, patients with bile leaks began to have a higher cumulative cost at 30 days ($38,037 vs $20,907; p <0.001), and the cost differential remained stable up to 1 year. Conversely, patients with BDI had higher cost of index hospitalization when compared with those without BDI ($35,846 vs $20,477; p < 0.001) (Fig. 4B). This cost differential was higher at 90 days ($51,027 vs $21,291; p <0.001), and continued to rise at 1 year ($61,384 vs $22,377; p < 0.001). When analyzing patients with BDIs by management approach (surgical vs endoscopic), operatively managed BDIs were associated with higher cost at the time of repair ($37,698 vs $25,705; p < 0.001) (Fig. 4C). However, endoscopically managed BDIs began to have a higher cumulative cost at 90 days ($56,972 vs $51,183; p < 0.001) and beyond. This difference was even more pronounced at 1 year ($118,245 vs $60,539; p < 0.001).
Figure 4.
(A) Cumulative costs for patients with and without bile leaks. (B) Cumulative costs for patients with and without bile duct injuries (BDIs). (C) Cumulative cost for patients with BDIs managed operatively and those managed endoscopically.
DISCUSSION
In an analysis of an all-capture state database, the contemporary bile leak and BDI rates were 0.50% and 0.22%, respectively. Patients with a bile leak or BDI were almost twice as likely to die within 1 year when compared with patients without a bile leak or BDI. Of note, this impact of bile leaks and BDI on mortality was only observed in older patients, and had no effect on patients younger than 40 years old. Patients with BDIs undergoing an operative repair had a 5-fold higher survival rate when compared with those undergoing endoscopic management. Although operatively managed BDIs were associated with a higher upfront cost, endoscopically managed BDIs began to have a higher cumulative cost after 90 days and beyond, with the differential cost at 1 year being $57,706 more expensive from higher readmission and reintervention rates.
Since the introduction and dissemination of laparoscopic cholecystectomy, the BDI rates have risen to approximately 0.4% to 0.6%, which was significantly higher than BDI rates of 0.1% to 0.2% in the open era.4,5 However, recent studies have suggested that contemporary BDI rates have returned to prelaparoscopy rates. In an analysis of 572,223 patients from the United Kingdom’s National Health Service database, the BDI rate was reported to be 0.09%.6 In the US, Halbert and colleagues11 analyzed 156,958 cholecystectomy patients from 2005 to 2010 from the New York State database and reported a BDI rate of 0.08%. The current analysis assessing 809,827 cholecystectomy patients from 2005 to 2014 in the state of California corroborates these findings, demonstrating a BDI rate of 0.22%. The incidence of bile leaks, however, is less known. Review of institutional databases have reported bile leak rates ranging widely from 0.2% to 4.2%, mainly due to their limited sample sizes.14–17 The current study reports a bile leak rate of 0.50%, which is 2.3 times more common than the incidence of BDIs.
In 2003, Flum and colleagues10 reported a higher overall mortality rate among BDI patients after a decade’s worth of follow-up when compared with patients without BDI (80.5% vs 44.8%, adjusted hazard ratio of 2.8). However, this analysis was performed in an elderly Medicare population and, therefore, is not generalizable, given that up to 70% of patients requiring cholecystectomy are younger than 65 years old. In a descriptive analysis of patients of all ages in New York State, Halbert and colleagues7 reported an overall mortality rate of 20.8% in patients with BDIs, predictably lower than the rate reported by Flum and colleagues. Similarly, Tornqvist and colleagues18 reported a 1-year mortality rate of 3.9% in BDI patients vs 1.1% in patients without BDI in Sweden. In the current analysis, a 2-fold higher adjusted mortality rate was observed in patients of all ages with BDIs when compared with patients with no BDIs. This elevated mortality impact was only observed in older patients, with BDI patients younger than 50 years old surviving just as long as those without BDIs. This finding might be secondary to the fact that younger patients have more reserve to sustain the cumulative physiologic insults of a BDI. In addition, the diminished survival observed in BDI patients has important implications in counseling and setting patient expectations.
The impact of bile leaks on long-term outcomes, on the other hand, have not been explored previously. Most studies assessing bile leaks after cholecystectomy report on its incidence,14 risk factors,15,16 and short-term success rates,17 but not on long-term survival. In an analysis of 57 patients with bile leaks after cholecystectomy, Buanes and colleagues15 reported a mortality rate of 8.8% (5 patients). In the current analysis of 3,551 patients with bile leaks, 2.4% of patients died within 1 year, which was 2-fold higher than patients with no bile leaks. This mortality impact was observed despite adjusting for sepsis and cholangitis, suggesting that even in the absence of overt infection, a bile leak still had a detrimental effect on survival. Similar to BDI, this effect was seen in older patients only, with survival in patients younger than 40 years old not affected by bile leaks.
Although the reintervention and readmission rates after bile leaks and BDIs have been well documented, the resultant added cumulative cost of care has not been assessed previously. Our study demonstrates that patients with bile leaks incur $17,130 more healthcare dollars within the first 30 days than those without a leak, but cost remained fairly stable thereafter. This finding is in line with the observation that bile leaks, once diagnosed and treated, have a very high success rate.19 Conversely, BDI patients incurred $15,269 more healthcare dollars than non-BDI patients during the index hospitalization, and this cost differential only continued to grow with time, increasing to +$39,007 at 1 year.
When costs were analyzed by management approach, the increasing cost differential with time was driven by patients undergoing endoscopic treatment. Although patients managed operatively incurred more upfront cost, the cost curve plateaus after 60 days, secondary to a high success rate, which has been reported to be as high as 85% to 95%.19–26 Patients managed endoscopically, however, continue to incur healthcare cost throughout time, and amass up to $118,245 cumulative dollars by 1 year. More importantly, the current analysis found that BDI patients who underwent operative repair had a 5-fold better adjusted survival rate than BDI patients managed endoscopically. This observation might be mediated through the added physiologic stress that comes with more procedures and, perhaps, episodes of cholangitis related to stent occlusion.19,27–30
This study should be interpreted in the context of its study design. Bile leaks and endoscopically treated BDIs have not previously been defined with ICD-9 codes in an administrative database. Although our definition was established with the consensus of a group of national cholecystectomy experts, with vigorous inclusion and exclusion criteria, additional validation is still required. The survival difference for BDI patients who underwent operative repair over those undergoing endoscopic repair might be secondary to an immortal time bias. Additionally, for BDI patients in the endoscopic group who eventually underwent a surgical repair, we were unable to determine whether they did so because of the failure of endoscopic management, or if endoscopic management was planned as a bridge to operation. Finally, the OSHPD database does not have specific surgeon identifiers and, as such, we were not able to adjust for surgeon experience, which has been shown to impact BDI rates after cholecystectomy.24
CONCLUSIONS
The contemporary BDI rates after cholecystectomy observed in California were lower than those reported in the 1990s. Bile leaks occurred 2.3 times more often than BDIs, and patients with either complication have diminished survival. However, this impact of bile leaks and BDIs was seen in older patients only, with patients younger than 40 years old demonstrating no difference in survival. Surgical repair of BDIs incurred a higher upfront cost when compared with endoscopically managed BDIs, but surgery was associated with superior survival and lower cumulative cost at 1 year.
Supplementary Material
Acknowledgments
Support for this study: This study was supported by the California Office of Statewide Health Planning and Development (Contract #13-4146).
The authors would like to acknowledge the California Office of Statewide Health Planning and Development for access to the state’s cholecystectomy database.
Abbreviations and Acronyms
- BDI
bile duct injury
- OR
odds ratio
- OSHPD
Office of Statewide Health Planning and Development
Footnotes
Disclosure Information: Authors have nothing to disclose. Timothy J Eberlein, Editor-in-Chief, has nothing to disclose.
Presented at the Southern Surgical Association 129th Annual Meeting, Hot Springs, VA, December 2017.
Author Contributions
Study conception and design: Fong, Pitt, Strasberg, Loehrer, Sicklick, Talamini, Lillemoe, Chang
Acquisition of data: Fong, Talamini, Chang
Analysis and interpretation of data: Fong, Pitt, Strasberg, Loehrer, Sicklick, Talamini, Lillemoe, Chang
Drafting of manuscript: Fong, Pitt
Critical revision: Fong, Pitt, Strasberg, Sicklick, Chang
References
- 1.USA Procedure. Ann Arbor, MI: Truven Health Analytics; 2014. Truven Health Analytics (Thomson/Solucient) [Google Scholar]
- 2.Giger UF, Michel JM, Opitz I, et al. Risk factors for perioperative complications in patients undergoing laparoscopic cholecystectomy. Analysis of 22,953 consecutive cases from the Swiss Association of Laparoscopic and Thoracoscopic Surgery database. J Am Coll Surg. 2006;203:723–728. doi: 10.1016/j.jamcollsurg.2006.07.018. [DOI] [PubMed] [Google Scholar]
- 3.Roslyn JJ, Binns GS, Hughes EF, et al. Open cholecystectomy. A contemporary analysis of 42,474 patients. Ann Surg. 1993;218:129–137. doi: 10.1097/00000658-199308000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Archer SB, Brown DW, Smith CD, et al. Bile duct injury during laparoscopic cholecystectomy. Results of a national survey. Ann Surg. 2001;234:549–558. doi: 10.1097/00000658-200110000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gigot J, Etienne J, Aerts R, et al. The dramatic reality of biliary tract injury during laparoscopic cholecystectomy. An anonymous multicenter Belgian survey of 65 patients. Surg Endosc. 1997;11:1171–1178. doi: 10.1007/s004649900563. [DOI] [PubMed] [Google Scholar]
- 6.El-Dhuwaib Y, Slavin J, Corless DJ, et al. Bile duct reconstruction following laparoscopic cholecystectomy in England. Surg Endosc. 2016;30:3516–3525. doi: 10.1007/s00464-015-4641-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Halbert C, Altieri MS, Yang J, et al. Long-term outcomes of patients with common bile duct injury following laparoscopic cholecystectomy. Surg Endosc. 2016;30:4294–4299. doi: 10.1007/s00464-016-4745-9. [DOI] [PubMed] [Google Scholar]
- 8.Barrett M, Asbun HJ, Chien HL, et al. Bile duct injury and morbidity following cholecystectomy. A need for improvement. Surg Endosc. 2017 Sep 15; doi: 10.1007/s00464-017-5847-8. Epub ahead of print. [DOI] [PubMed]
- 9.Sheffield KM, Riall TS, Han Y, et al. Association between cholecystectomy with vs without intraoperative cholangiography and risk of common duct injury. JAMA. 2013;310:812–820. doi: 10.1001/jama.2013.276205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Flum DR, Cheadle A, Prela C, et al. Bile duct injury during cholecystectomy and survival in Medicare beneficiaries. JAMA. 2003;290:2168–2173. doi: 10.1001/jama.290.16.2168. [DOI] [PubMed] [Google Scholar]
- 11.Halbert C, Pagkratis S, Yang J, et al. Beyond the learning curve. Incidence of bile duct injuries following laparoscopic cholecystectomy normalized to open in the modern era. Surg Endosc. 2016;30:2239–2243. doi: 10.1007/s00464-015-4485-2. [DOI] [PubMed] [Google Scholar]
- 12.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies. Development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 13.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45:613–619. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- 14.Kozarek R, Gannan R, Baerg R, et al. Bile leak after laparoscopic cholecystectomy. Diagnostic and therapeutic application of endoscopic retrograde cholangiopancreatography. Arch Intern Med. 1992;152:1040–1043. doi: 10.1001/archinte.152.5.1040. [DOI] [PubMed] [Google Scholar]
- 15.Buanes T, Waage A, Mjaland O, et al. Bile leak after cholecystectomy significance and treatment. Results from the National Norwegian Cholecystectomy Registry. Int Surg. 1996;81:276–279. [PubMed] [Google Scholar]
- 16.Shawhan RR, Porta CR, Bingham JR, et al. Biliary leak rates after cholecystectomy and intraoperative cholangiogram in surgical residency. Mil Med. 2015;180:565–569. doi: 10.7205/MILMED-D-14-00426. [DOI] [PubMed] [Google Scholar]
- 17.Adler DG, Papachristou GI, Taylor LJ, et al. Clinical outcomes in patients with bile leaks treated via ERCP with regard to the timing of ERCP. A large multicenter study. Gastrointest Endosc. 2017;85:766–772. doi: 10.1016/j.gie.2016.08.018. [DOI] [PubMed] [Google Scholar]
- 18.Tornqvist B, Stromberg C, Persson G, et al. Effect of intended intraoperative cholangiography and early detection of bile duct injury on survival after cholecystectomy. Population based cohort study. BMJ. 2012;345:e6457. doi: 10.1136/bmj.e6457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pitt HA, Sherman S, Johnson MS, et al. Improved outcomes of bile duct injuries in the 21st century. Ann Surg. 2013;258:490–499. doi: 10.1097/SLA.0b013e3182a1b25b. [DOI] [PubMed] [Google Scholar]
- 20.Lillemoe KD, Martin SA, Cameron IL, et al. Major bile duct injuries associated with laparoscopic cholecystectomy. Ann Surg. 1997;225:459–471. doi: 10.1097/00000658-199705000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lillemoe KD, Melton GB, Cameron IL, et al. Postoperative bile duct strictures. Management and outcomes in the 1990s. Ann Surg. 2000;232:430–441. doi: 10.1097/00000658-200009000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sicklick JK, Camp MS, Lillemoe KD, et al. Surgical management of bile duct injuries sustained during laparoscopic cholecystectomy. Peroperative results in 200 patients. Ann Surg. 2005;241:786–795. doi: 10.1097/01.sla.0000161029.27410.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Strasberg SM, Herd M, Soper NJ. An analysis of biliary injury during laproscopic cholecystectomy. J Am Coll Surg. 1995;180:101–105. [PubMed] [Google Scholar]
- 24.Winslow ER, Fialkowski EA, Linehan DC, et al. “Sideways”Results of repair of biliary injuries using a policy of side-to-side hepatico-jejunosotomy. Ann Surg. 2009;249:426–434. doi: 10.1097/SLA.0b013e31819a6b2e. [DOI] [PubMed] [Google Scholar]
- 25.Strasberg SM, Helton WS. An analyticl review of vasculobiliary injury in laparascopic and open cholecystectomy. HPB. 2011;13:1–14. doi: 10.1111/j.1477-2574.2010.00225.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schwaitzberg SD, Scott DJ, Jones DB, et al. Threefold increased bile duct injury rate is associated with less surgeon experience in an insurance claims database. More rigorous training in biliary surgery may be needed. Surg Endosc. 2014;28:3068–3073. doi: 10.1007/s00464-014-3580-0. [DOI] [PubMed] [Google Scholar]
- 27.Davids PHP, Tanka AKF, Rauws EAJ, et al. Benign biliary strictures. Surgery or endoscopy? Ann Surg. 1993;217:237–243. doi: 10.1097/00000658-199303000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tocchi A, Mazzoni G, Liotta G, et al. Management of benign biliary strictures. Biliary enteric anastamosis vs endocsopic stenting. Arch Surg. 2000;135:153–157. doi: 10.1001/archsurg.135.2.153. [DOI] [PubMed] [Google Scholar]
- 29.Draganov P, Hoffman B, Marsh W, et al. Long-term outcome in patients with benign biliary strictures treated endoscopically with multiple stents. Gastrointest Endosc. 2002;55:680–686. doi: 10.1067/mge.2002.122955. [DOI] [PubMed] [Google Scholar]
- 30.de Reurer PR, Rauws EA, Vermeulen M, et al. Endoscopic treatment of post-surigical bile duct injuries. Long-term outcomes and predictors of success. Gut. 2007;56:1599–1605. doi: 10.1136/gut.2007.123596. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.