Abstract
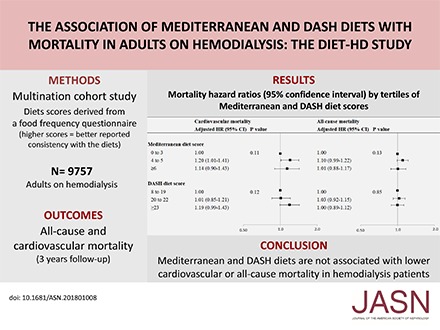
Background Mediterranean and Dietary Approaches to Stop Hypertension (DASH) diets associate with lower cardiovascular and all-cause mortality in the general population, but the benefits for patients on hemodialysis are uncertain.
Methods Mediterranean and DASH diet scores were derived from the GA2LEN Food Frequency Questionnaire within the DIET-HD Study, a multinational cohort study of 9757 adults on hemodialysis. We conducted adjusted Cox regression analyses clustered by country to evaluate the association between diet score tertiles and all-cause and cardiovascular mortality (the lowest tertile was the reference category).
Results During the median 2.7-year follow-up, 2087 deaths (829 cardiovascular deaths) occurred. The adjusted hazard ratios (95% confidence intervals) for the middle and highest Mediterranean diet score tertiles were 1.20 (1.01 to 1.41) and 1.14 (0.90 to 1.43), respectively, for cardiovascular mortality and 1.10 (0.99 to 1.22) and 1.01 (0.88 to 1.17), respectively, for all-cause mortality. Corresponding estimates for the same DASH diet score tertiles were 1.01 (0.85 to 1.21) and 1.19 (0.99 to 1.43), respectively, for cardiovascular mortality and 1.03 (0.92 to 1.15) and 1.00 (0.89 to 1.12), respectively, for all-cause mortality. The association between DASH diet score and all-cause death was modified by age (P=0.03); adjusted hazard ratios for the middle and highest DASH diet score tertiles were 1.02 (0.81 to 1.29) and 0.70 (0.53 to 0.94), respectively, for younger patients (≤60 years old) and 1.05 (0.93 to 1.19) and 1.08 (0.95 to 1.23), respectively, for older patients.
Conclusions Mediterranean and DASH diets did not associate with cardiovascular or total mortality in hemodialysis.
Keywords: Dietary patterns, Mediterranean diet, DASH diet, mortality, hemodialysis, end-stage kidney disease
Patients treated with hemodialysis experience a very high mortality risk. The annualized incidence of mortality is 10%–20%, which is at least ten times higher than that in the general population. Cardiovascular disease accounts for about 40% of deaths.1–5 Despite decades of research, there is no high-quality evidence that specific treatments or preventative strategies reduce mortality in this setting.6–10 Accordingly, there is an unmet need for effective interventions that reduce cardiovascular events and mortality among the hemodialysis population.
Lifestyle modification, including healthy diets and exercise, has beneficial effects on cardiovascular risk factors, such as hypertension, insulin resistance, and dyslipidemia, in the general population.11–13 Recommended diets, including the Mediterranean and the Dietary Approaches to Stop Hypertension (DASH) diets, which emphasize the intake of fruits, vegetables, fish, and low-fat dairy and reduced intake of meat, refined sugars, salt, and saturated fat, are associated with 10%–30% lower risk of cardiovascular disease and mortality in the general population.14–18 These benefits may be attributed to improved serum lipids, BP, insulin resistance, inflammation, oxidative stress, arterial stiffness, and endothelial function.19–22
Emerging evidence suggests that these diets may also improve survival in the CKD population. A recent systematic review of observational studies showed that dietary patterns resembling the Mediterranean and DASH diets were associated with 30% lower all-cause mortality among patients with mild to moderate CKD.23 However, for patients treated with chronic hemodialysis, the benefits of Mediterranean and DASH diets have not been examined.23,24 We evaluated the association between these dietary patterns and the risk of death (cardiovascular and all-cause mortality) among adults treated with hemodialysis.
Methods
Study Design
The Dietary Intake, Death and Hospitalization in Adult with ESKD Treated with Hemodialysis (DIET-HD) Study is a multinational, prospective cohort study that aimed to evaluate the association between diet and clinical outcomes for adults treated with long-term hemodialysis. The study protocol has been described in detail elsewhere.25 This study was reported according to the Strengthening the Reporting of Observational Studies in Epidemiology guidelines.26
Study Population
Consecutive patients treated in selected clinics within a private dialysis provider network in Europe (France, Germany, Italy, Hungary, Poland, Portugal, Romania, Spain, Sweden, and Turkey) and South America (Argentina) were invited to participate. Patients were included if they were adults treated with hemodialysis for at least 90 days. They were excluded if they were unable to complete the Food Frequency Questionnaire (FFQ), had a life expectancy <6 months, or were likely to receive a kidney transplant within 6 months of baseline data collection. Ethics approval was obtained from all relevant institutional ethics committees, and the study was conducted according to the Declaration of Helsinki. All participants provided written informed consent before data collection.
Covariates of Interests
Baseline characteristics (sociodemographic, clinical, and dialysis related) within 1 month of enrolment were extracted from an administrative centralized patient database using data linkage. All clinical sites adhered to the same standard operating procedures in assessing and recording the variables of interest.
Dietary Assessment
Dietary intake of 260 foods grouped in 32 sections was ascertained using the Global Allergy and Asthma European Network (GA2LEN) FFQ27 administered during a routine hemodialysis treatment. The GA2LEN FFQ was specifically designed to facilitate international comparisons in dietary intake using a single common and standardized instrument.27 Data from the FFQ were entered into an electronic database using optical character recognition and linked to baseline and outcomes data within the centralized patient database. Patients reported how often they had consumed the foods during the previous year using eight predefined options (rarely or never; one to three times per month; one, two to four, or five to six times per week; one, two to three, or four or more times per day). Responses to the individual food items were combined to compute the total intake of each food group related to the Mediterranean and DASH diets. The frequency of reported food intake was converted into daily grams using standard food portion sizes following the recommendations from the United Kingdom Food Standards Agency.28 Macro- and micronutrient intake was derived using McCance and Widdowson Food Composition Tables.29
Assessment of Mediterranean and DASH Diets
Population-based quality scores reflecting the Mediterranean and DASH diets were calculated from the FFQ using standardized indices derived on the basis of data from the general population. Higher scores indicated food intake more consistent with these diets.30,31
The Mediterranean diet score was applicable to both Mediterranean and non-Mediterranean countries and ranked participants according to the intake of nine food components (grams per day).30 For vegetables, fruit, legumes, cereals, and fish and the ratio of monounsaturated and polyunsaturated fatty acids to saturated fatty acids (putative beneficial components), an intake at or above the sex-specific median was scored as one, and an intake below the sex-specific median was scored as zero. Reverse scoring was used for dairy and meat (putative detrimental components). Consumption of alcohol from 10 to 50 g/d for men and from 5 to 25 g/d for women was scored one; otherwise, the score was assigned as zero. The component scores were summed to obtain an overall diet score that ranged from zero to nine, with higher scores indicating better reported consistency with a Mediterranean diet. (Supplemental Table 1).
For the DASH diet score, participants were ranked on the intake of eight food components (servings per day).31 The intake of vegetables, fruits, legumes, and low-fat dairy products was scored from one to five on the basis of distribution in sex-specific quintiles. The lowest quintile was scored as one, and the highest quintile was scored as five. Reverse scoring was used for red and processed meat and sodium. Compared with the previously developed score, the intake of sweetened beverages and whole grains was too low to be ranked in quintiles. Therefore, the intake of sweetened beverages was scored from one to three on the basis of distribution in sex-specific tertiles (the lowest tertile was scored as three, and the highest was scored as one). The consumption of whole grains was scored as one, whereas no whole grain consumption was scored as zero. The overall diet score ranged from seven to 34, with higher scores indicating better reported consistency with a DASH diet (Supplemental Table 2).
Outcomes
Cardiovascular mortality was defined as sudden death or death attributed to acute myocardial infarction, pericarditis, atherosclerotic heart disease, cardiomyopathy, cardiac arrhythmia, cardiac arrest, valvular heart disease, pulmonary edema, or congestive cardiac failure. All-cause mortality was death from any cause. The causes of death were obtained from the death certificates, which were filled in and adjudicated by the participants’ treating clinicians without any knowledge of the diet scores. The causes of death were recorded according to the United States coding for the ESKD population and collected in a centralized database that was linked via deterministic linkage using the same identifier in the FFQ data.
Statistical Methods
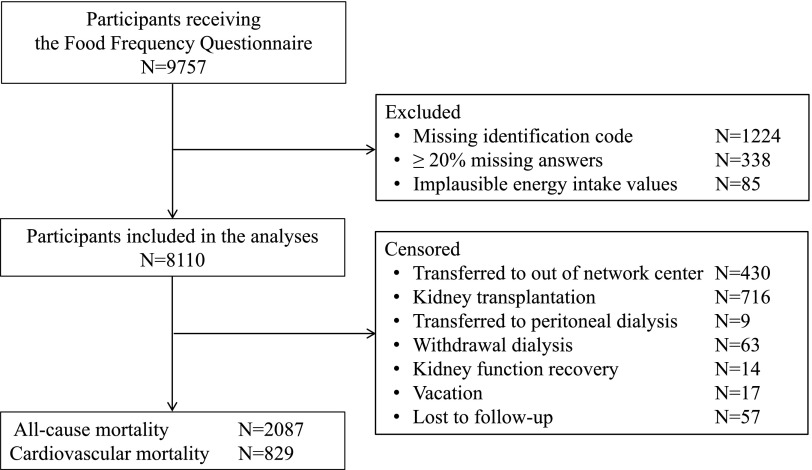
Participants were excluded if their FFQ contained an erroneous or missing identification code that prevented data linkage with their baseline and outcomes data, 20% or more missing response data, or biologically implausible values for total energy intake (above or below 3 SD from the log-transformed mean) (Figure 1).
Figure 1.
Study flow chart showing the process resulting in the inclusion of 8110 participants in analyses and all censoring details.
Continuous variables at baseline were summarized using means and SDs or medians and interquartile ranges as appropriate to their distribution. Categorical variables were calculated using frequencies and percentages. Restricted cubic splines were used to determine the linearity between diets scores and mortality, and no deviance from linearity was observed. Person-time for each participant was calculated from the date of the FFQ administration to the date of cardiovascular or all-cause mortality. In the time to event analyses for all-cause mortality, patients who had left the dialysis network, underwent kidney transplantation, transferred to peritoneal dialysis, had withdrawn from dialysis, had recovery of kidney function, went on vacation outside the network, were lost to follow-up, or survived until the end of the follow-up period were censored. For analyses of cardiovascular mortality, patients who had died from noncardiovascular causes were also censored. Univariable and multivariable Cox proportional hazard regression analyses were fitted using a random effect model (frailty model) to account for clustering of mortality risk within countries. Mediterranean and DASH diet scores were categorized into tertiles to be used in the models on the basis of their distribution. To assess the contribution of each food component of the Mediterranean and DASH diets, we simultaneously modeled each component individually as a continuous variable. Results were presented as hazard ratios (HRs) and the associated 95% confidence intervals (95% CIs) using the lowest tertile as the reference category. Ordinal trends in cardiovascular and mortality risk across diet scores tertiles were tested by modeling a categorical variable with the median value for each score tertile. The proportional hazards assumption in Cox models was assessed by fitting log (time)-dependent covariates in the multivariable model. Effect modification of the association between diet scores and outcomes by prespecified covariates (age, sex, smoking history, and myocardial infarction) was tested by introducing interactions terms in the multivariable model.
Backward elimination was used to select covariates for inclusion in the multivariable models, retaining those (aside from energy intake, sex, and physical activity) that predicted cardiovascular or all-cause mortality (P<0.05) or with a clinically meaningful effect on the HR for these outcomes of the diet score (≥10%). Analyses of cardiovascular mortality were, therefore, adjusted for age, sex, daily physical activity, education (secondary versus none/primary), diabetes, smoking (current or former versus never), myocardial infarction, vascular access type (fistula versus graft/catheter), body mass index (categories according to the World Health Organization), albumin (tertiles), Charlson comorbidity score (quartiles), serum phosphorus, calcium, hemoglobin, urea clearance (Kt/V), and energy intake (per 1000-kcal/d increase). In addition to these variables, analyses of all-cause mortality were also adjusted for having a life partner, being waitlisted for transplant, and time on dialysis. For each categorical variable, an extra category was included for missing data in the multivariable model when necessary (education, smoking, diabetes, myocardial infarction, serum albumin, and body mass index). A complete patient analysis was also conducted including only those patients with complete data for diet scores, covariates, and outcomes.
The potential relevance of competing events (death from other causes and kidney transplantation for the analysis of cardiovascular mortality; kidney transplantation for the analysis of all-cause mortality) was considered using a stratified proportional subdistribution hazard model. Finally, to reduce the risk of reverse causality, the multivariable random effect analyses were repeated after excluding the first 12 months of follow-up in sensitivity analyses. All analyses were conducted using SAS 9.4 (SAS Inc.). A two-tailed P<0.05 was used as an indication of statistical significance.
Results
Overall, 9757 patients on hemodialysis were recruited between January 2014 and January 2015. The final patient assessment occurred for outcome data on June 27, 2017; 8110 (83%) were included in the analyses after exclusion of patients with an erroneous or missing identification code (n=1224; 13%) and those with insufficient or implausible dietary responses (n=423; 4%) (Figure 1).
Baseline Characteristics
The mean age of participants was 63.1 years old (SD=15.0 years old). Overall, more than one half were men (58%), nearly one third (33%) were former or current smokers, 15% engaged in daily physical activity, 32% had diabetes, and 12% had a history of myocardial infarction. Participants’ median time on hemodialysis was 3.6 years (interquartile range, 1.7–6.8) (Table 1). The mean (SD) values of the Mediterranean and DASH diet scores were 4.1 (1.6) on a zero- to nine-point scale and 20.5 (3.7) on a seven- to 34-point scale, respectively. The distributions of diet scores were similar among countries. The Mediterranean diet score ranged from 3.0 (1.4) in Germany to 5.3 (1.5) in Italy; the DASH diet score ranged from 18.2 (3.4) in Sweden to 23.1 (3.2) in Turkey (Supplemental Table 3).
Table 1.
Baseline characteristics of participants
| Variable | No. of Participants with Data | Mean (SD), Median (IQR), or n (%) |
|---|---|---|
| Sociodemographic | ||
| Age, yr | 8110 | 63.1 (15.0) |
| ≤60 | 3059 (37.7) | |
| >60 | 5051 (62.3) | |
| Men | 8110 | 4691 (57.8) |
| Country | 8110 | |
| Portugal | 1777 (21.9) | |
| Argentina | 1204 (14.9) | |
| Turkey | 1107 (13.7) | |
| Spain | 1041 (12.8) | |
| Romania | 1000 (12.3) | |
| Hungary | 554 (6.8) | |
| Italy | 543 (6.7) | |
| Poland | 434 (5.4) | |
| France | 221 (2.7) | |
| Germany | 178 (2.2) | |
| Sweden | 51 (0.6) | |
| Married/life partner | 6095 | 4127 (67.7) |
| Secondary education | 6090 | 2699 (44.3) |
| Daily physical activity | 6199 | 934 (15.1) |
| Waitlisted for transplant | 8094 | 1496 (18.5) |
| Clinical characteristics | ||
| Current or former smoker | 6280 | 2068 (32.9) |
| Body mass index, kg/m2 | 7872 | |
| Underweight (<18.5) | 365 (4.6) | |
| Normal range (18.5–24.9) | 3309 (42.0) | |
| Preobese (25.0–29.9) | 2659 (33.8) | |
| Obese (≥30.0) | 1539 (19.6) | |
| Hypertension | 7320 | 6219 (85.0) |
| Diabetes | 7283 | 2332 (32.0) |
| Angina | 6965 | 1030 (14.8) |
| Congestive heart failure | 7275 | 1388 (19.1) |
| Myocardial infarction | 7239 | 838 (11.6) |
| Stroke | 7233 | 634 (8.8) |
| Pulmonary disease | 8110 | 940 (11.6) |
| Depression | 7221 | 757 (10.5) |
| Gastrointestinal disease | 8110 | 1763 (21.7) |
| Cancer | 8110 | 1045 (12.9) |
| Charlson comorbidity score | 8110 | 6 (4–8) |
| Medications | ||
| Antihypertensive | 8110 | 2471 (39.4) |
| Statin | 6225 | 2316 (37.2) |
| Laboratory variables | ||
| Albumin, g/L | 6167 | 39.8 (3.8) |
| Phosphorus, mg/dl | 7869 | 4.7 (1.4) |
| Calcium, mg/dl | 7870 | 8.9 (0.7) |
| Hemoglobin, g/dl | 7869 | 11.1 (1.3) |
| Dialysis characteristics | ||
| Arteriovenous fistula | 8051 | 6481 (80.5) |
| Time on dialysis, yr | 8108 | 3.6 (1.7–6.8) |
| Kt/V urea | 7818 | 1.7 (0.3) |
| Dietary intake (self-reported servings per day) | ||
| Cereals | 8108 | 2.3 (1.2–3.3) |
| Fruits | 8107 | 2.5 (1.4–4.4) |
| Vegetables | 8109 | 3.6 (2.2–5.9) |
| Legumes and nuts | 8110 | 0.3 (0.1–0.6) |
| Dairy | 8110 | 1.4 (0.6–2.4) |
| Fish and white meat | 8110 | 0.6 (0.3–1.1) |
| Read meat and meat products | 8110 | 1.1 (0.6–1.9) |
| Sweets and sweetened drinks | 8110 | 2.4 (1.2–4.1) |
Body mass index categories are defined according to the World Health Organization. Antihypertensive medications are angiotensin-converting enzyme or angiotensin II receptor blocker. IQR, interquartile range.
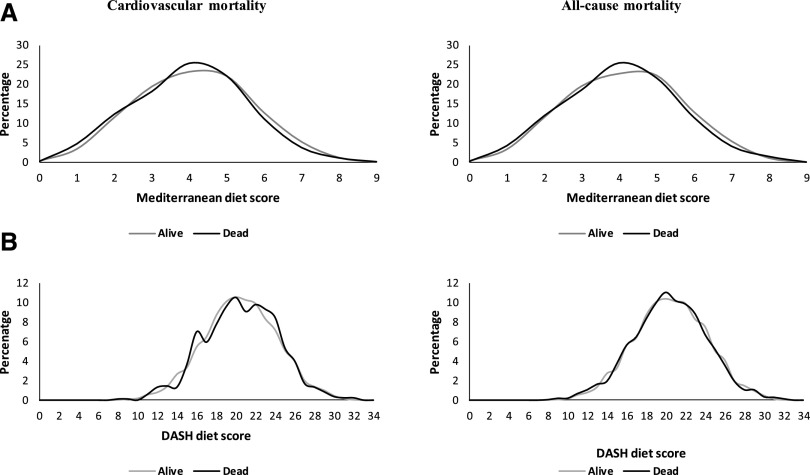
Cardiovascular Mortality
During a median follow-up of 2.7 years (18,666 person-years), there were 2087 deaths (26%), of which 829 (40%) were attributable to cardiovascular causes (Supplemental Table 4). The distributions of the Mediterranean (Figure 2A) and DASH (Figure 2B) diet scores among patients who died from cardiovascular causes were similar to those of patients who survived until the end of the follow-up (Figure 2). Overall, there was no evidence of an association between Mediterranean or DASH diet and cardiovascular mortality. Compared with patients in the lowest Mediterranean diet score tertile (zero to three), the adjusted HRs for cardiovascular mortality among those in the middle (four to five) and highest (six or more) score tertiles were 1.20 (95% CI, 1.01 to 1.41) and 1.14 (95% CI, 0.90 to 1.43), respectively (P value per trend =0.11). Compared with patients in the lowest DASH diet score tertile (eight to 19), the adjusted HRs for cardiovascular mortality among those in the middle (20–22) and highest (≥23) tertiles were 1.01 (95% CI, 0.85 to 1.21) and 1.19 (95% CI, 0.99 to 1.43), respectively (P value per trend =0.12). Similar findings were observed when considering the competing risk of other causes of death and kidney transplantation on cardiovascular mortality and in sensitivity analyses, omitting those cardiovascular deaths (n=334 of 829) that occurred in the first 12 months of follow-up (Table 2). There was no interaction between prespecified covariates and Mediterranean or DASH diet score on cardiovascular mortality. Supplemental Tables 5 and 6 show the associations of the Mediterranean and DASH diet individual food components with mortality. The intake of dairy was the only measure that predicted cardiovascular mortality, and it was associated with a higher risk.
Figure 2.
(A) Mediterranean and (B) Dietary Approaches to Stop Hypertension (DASH) diet score distributions in patients who died from cardiovascular or any cause were similar to those in patients who survived to the end of follow-up. Percentage of cardiovascular (left plots) and all-cause mortality (right plots) were plotted against Mediterranean (top plots) and DASH (bottom plots) diet scores in patients who died and in patients who survived to the end of follow-up.
Table 2.
Mortality hazard ratios (95% confidence intervals) by tertiles of Mediterranean and Dietary Approaches to Stop Hypertension diet scores
| Model | Mediterranean Diet Score | DASH Diet Score | ||||||
|---|---|---|---|---|---|---|---|---|
| 0–3 | 4–5 | ≥6 | P Value | 8–19 | 20–22 | ≥23 | P Value | |
| Cardiovascular mortality | ||||||||
| Univariable random effect | Reference | 1.16 (0.99 to 1.35) | 1.08 (0.87 to 1.33) | 0.18 | Reference | 1.08 (0.91 to 1.29) | 1.30 (1.09 to 1.55) | 0.01 |
| Multivariable random effecta | Reference | 1.20 (1.01 to 1.41) | 1.14 (0.90 to 1.43) | 0.11 | Reference | 1.01 (0.85 to 1.21) | 1.19 (0.99 to 1.43) | 0.12 |
| Multivariable competing riska | Reference | 1.17 (0.99 to 1.39) | 1.15 (0.91 to 1.45) | 0.18 | Reference | 1.01 (0.84 to 1.21) | 1.20 (0.99 to 1.45) | 0.11 |
| Multivariable patient completea | Reference | 1.06 (0.82 to 1.39) | 1.03 (0.73 to 1.45) | 0.89 | Reference | 0.84 (0.63 to 1.11) | 0.91 (0.69 to 1.21) | 0.46 |
| Sensitivity analysisa | Reference | 1.19 (0.96 to 1.47) | 1.03 (0.76 to 1.40) | 0.23 | Reference | 1.06 (0.85 to 1.33) | 1.05 (0.83 to 1.34) | 0.85 |
| All-cause mortality | ||||||||
| Univariable random effect | Reference | 1.12 (1.01 to 1.23) | 1.02 (0.89 to 1.16) | 0.05 | Reference | 1.10 (0.99 to 1.22) | 1.13 (1.01 to 1.26) | 0.07 |
| Multivariable random effectb | Reference | 1.10 (0.99 to 1.22) | 1.01 (0.88 to 1.17) | 0.13 | Reference | 1.03 (0.92 to 1.15) | 1.00 (0.89 to 1.12) | 0.85 |
| Multivariable competing riskb | Reference | 1.10 (0.99 to 1.22) | 1.02 (0.88 to 1.18) | 0.16 | Reference | 1.03 (0.92 to 1.15) | 1.00 (0.89 to 1.13) | 0.85 |
| Multivariable patient completeb | Reference | 1.07 (0.91 to 1.26) | 0.96 (0.77 to 1.18) | 0.39 | Reference | 1.10 (0.93 to 1.29) | 0.93 (0.78 to 1.11) | 0.16 |
| Sensitivity analysisb | Reference | 1.06 (0.93 to 1.21) | 0.98 (0.82 to 1.18) | 0.50 | Reference | 0.98 (0.86 to 1.13) | 0.90 (0.78 to 1.05) | 0.35 |
DASH, Dietary Approaches to Stop Hypertension.
Adjusted for country (fixed effect in competing risk analysis and random effect in all others), sex, daily physical activity, education (secondary versus none/primary), diabetes, smoking (current or former versus never), myocardial infarction, vascular access type (fistula versus graft/catheter), body mass index (categories according to the World Health Organization), albumin (tertiles), Charlson comorbidity score (quartiles), age, phosphorus, calcium, hemoglobin, Kt/V, and energy intake (1000-kcal/d increase).
All above adjustments plus adjusted for having a life partner, time on dialysis, and being waitlisted for transplantation. Sensitivity analyses excluded the first 12 months of follow-up (786 all-cause deaths of 2087 and 334 cardiovascular deaths of 829 were excluded).
All-Cause Mortality
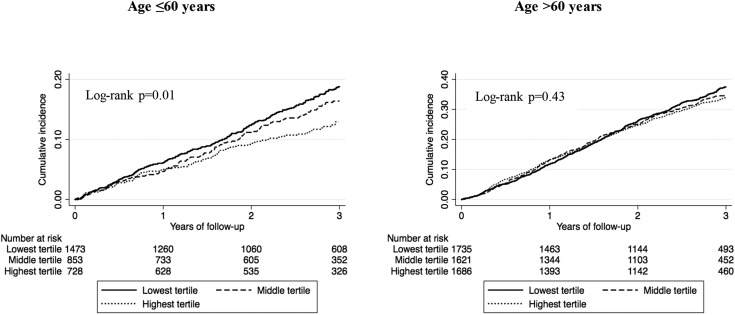
The overall distributions of the Mediterranean (Figure 2A) and DASH (Figure 2B) diet scores in patients who died from any cause were similar to those in patients who survived to the end of follow-up (Figure 2). Compared with patients in the lowest Mediterranean diet score tertile, the adjusted HRs for all-cause mortality among those in the middle and highest tertiles were 1.10 (95% CI, 0.99 to 1.22) and 1.01 (95% CI, 0.88 to 1.17), respectively (P value per trend =0.13) (Table 2). There was no statistically significant interaction between age and Mediterranean diet score on mortality (P=0.69 [diet score as continuous variable]; P=0.06 [as tertiles]). Compared with patients in the lowest DASH diet score tertile, the adjusted HRs for all-cause mortality among those in the middle and highest tertiles were 1.03 (95% CI, 0.92 to 1.15) and 1.00 (95% CI, 0.89 to 1.12), respectively (P value per trend =0.85) (Table 2). The association between DASH diet score and all-cause death was modified by age (P value for interaction <0.01 [score as continuous variable] and P=0.03 [as tertiles]). For younger patients (age ≤60 years old), the 3-year cumulative incidences of all-cause death across tertiles of DASH diet score were 19, 17, and 13 deaths per 100,000 persons-days in ascending order from the lowest to the highest tertile (log rank P=0.01). For older participants (age >60 years old), the 3-year cumulative incidences of all-cause death were similar across tertiles of DASH diet score (41, 40, and 38 deaths for 100,000 persons-days; log rank P=0.45) (Figure 3). For the younger participants, the adjusted HRs for all-cause death were 1.02 (95% CI, 0.81 to 1.29) and 0.70 (95% CI, 0.53 to 0.94) in the middle and highest tertiles, respectively; among the older participants, the corresponding estimates were 1.05 (95% CI, 0.93 to 1.19) and 1.08 (95% CI, 0.95 to 1.23) in the middle and highest tertiles, respectively (Supplemental Table 7). Similar findings were observed when considering the competing risk of kidney transplantation on all-cause mortality and in sensitivity analysis omitting those all-cause deaths (n=786 of 2087) that occurred in the first 12 months of follow-up (Supplemental Table 7, Table 2). Associations between individual diets food components and all-cause mortality were all nonsignificant (Supplemental Tables 5 and 6).
Figure 3.
Kaplan–Meier estimates of all-cause mortality by tertiles of Dietary Approaches to Stop Hypertension scores stratified by age groups showing an association between higher DASH diet scores and lower risk of all-cause mortality in younger (aged ≤ 60 years), but not in older patients. Log-rank test compares the risk of all-cause mortality across tertiles of DASH diet score in patients aged 60 years or younger (curves on the left) and in older patients (curves on the right).
Complete Patient Analyses
Similar findings were observed in the complete patient analyses, which included 3889 and 3480 participants for cardiovascular and all-cause mortality, respectively (Supplemental Table 7, Table 2).
Discussion
In this study involving 8110 patients on hemodialysis with 2087 deaths (829 cardiovascular related) followed for a median period of almost 3 years, the Mediterranean and DASH diet scores were generally low and consistent across a range of European countries. There was no evidence that higher Mediterranean or DASH diet scores were associated with lower risk of cardiovascular or all-cause mortality. Excluding participants who died in the first 12 months of follow-up did not alter the association between diets scores and cardiovascular or all-cause mortality. Age was a significant effect modifier of the relationship between DASH diet score and all-cause mortality but not cardiovascular mortality.
The observed absence of cardiovascular benefits associated with Mediterranean or DASH dietary patterns among patients on hemodialysis is consistent with evidence that other cardiovascular interventions of proven benefit for those populations with similarly high cardiovascular risk (including BP lowering and statins) are not observed to improve outcomes in the long-term dialysis setting. Coronary heart disease and atherosclerosis are complex disease processes involving multiple etiologies and pathways. In the general population, cardioprotective mechanisms of the Mediterranean and DASH diets are largely driven by improved lipid, glycemic, and BP control.22,32 In the hemodialysis populations, it has been shown that nontraditional risk factors, including malnutrition, oxidative stress, inflammation, altered calcium-phosphate regulation, and endothelial dysfunction, may dominate the pathogenesis of cardiovascular disease.33,34 Therefore, the physiologic changes associated with the DASH and Mediterranean diets may not sufficiently modify the cardiovascular pathobiology for patients on hemodialysis to improve clinical outcomes. Residual confounding from unmeasured factors may have masked any associations between the Mediterranean and DASH diets with cardiovascular mortality. Also, the relatively short follow-up may have precluded detection of any significant cardiovascular mortality benefit of these diets.
Although age was a significant modifier of the association between DASH diet score and all-cause mortality, this finding should be interpreted with caution. Given the higher comorbid burden of other diseases, such as cancer and infections, among older individuals, a ceiling effect of age may be present, such that dietary factors may influence survival to a lesser extent among older adults. Survival bias may exist in the elderly, because only those who have survived the selective pressures and burden of CKD could be included in the study. Such survivorship is not dependent on a single factor, such as diet, but many other inter-related features, including behavioral, genetic, and other lifestyle influences. Given that the findings were limited only to DASH diet and all-cause mortality, the observed association may also simply due to chance alone.
This study has provided new insights into the epidemiology of overall dietary patterns in patients on hemodialysis and their association with cardiovascular and all-cause mortality.23,24 This methodologic approach is a departure from much of the existing research in the setting of hemodialysis, which has focused predominantly on the roles of individual nutrients, such as protein, phosphate, sodium, and potassium, rather than whole dietary patterns on clinical outcomes.23,34 Clinical practice guidelines suggest individual nutrient restriction to improve outcomes in CKD,35–37 leading to dietary complexity and challenging adherence.38 In addition, the paucity of evidence supporting the restriction of targeted nutrients to improve morbidity, mortality, and quality of life in people on hemodialysis indicates that exploring the potential benefits of a whole dietary approach in the hemodialysis setting is warranted.39–41
This study has several strengths. The DIET-HD Study is the largest study conducted in patients on hemodialysis that assessed the effect of diet as a potential novel determinant of health, which has been identified as a research priority by patients with CKD, their caregivers, and health care professionals.42 The inclusion of a diverse range of countries with specific dietary characteristics, including those from the Mediterranean region as well as those in northern and eastern European areas and Scandinavia, also enhances the generalizability of the findings.
This study has several potential limitations. First, measurement errors may exist due to the self-reported nature of the FFQ. The FFQ did not include portion size, and it has been validated only in the general population against plasma phospholipid fatty acids but not with other dietary assessment methods. In addition, it is difficult to estimate and quantify precisely the sodium intake using an FFQ (salt intake used in cooking and at the table). This may have affected the evaluation of the DASH diet score and its association with cardiovascular mortality, in which sodium intake might play an important role in the ESKD population. Second, despite the high response rate to the FFQ, the exclusion of 17% of patients with FFQs that had a missing or erroneous identification code and incomplete or implausible answers may have resulted in a selection bias. Third, because of a single dietary measurement at baseline, it was not possible to measure any change in dietary habits and patterns over time, which may have occurred particularly in relation to the changing comorbid status of an individual on hemodialysis.
In conclusion, there was no evidence of an association between Mediterranean and DASH diets and cardiovascular or all-cause mortality in patients on hemodialysis. Dietary patterns that are protective in the general population do not predict better clinical outcomes in patients on hemodialysis.
Disclosures
None.
Supplementary Material
Acknowledgments
We are grateful to the Global Asthma and Allergy Network of Excellence (GA2LEN) for facilitating the use of the GA2LEN Food Frequency Questionnaire.
Each author contributed important intellectual content during manuscript drafting or revision, approved the final version of the manuscript, and agreed to be accountable for all aspects of the work.
We thank the provider of renal services Diaverum for covering overhead costs for study coordinators in each contributing country and material printing.
The Dietary Intake, Death and Hospitalization in Adult with ESKD Treated with Hemodialysis Study investigators and dieticians (Diaverum) are as follows. Argentina: A. Badino, L. Petracci, C. Villareal, M. Soto, M. Arias, F. Vera, V. Quispe, S. Morales, D. Bueno, R. Bargna, G. Peñaloza, L. Alcalde, J. Dayer, A. Milán, N. Centurión, A. Ramos, E. De Orta, S. Menardi, N. Austa Bel, E. Marileo, N. Junqueras, C. Favalli, R. Trioni, G. Valle, M. López, C. Marinaro, A. Fernandez, J. Corral, E. Nattiello, S. Marone, J. García, G. Carrizo, P. González, O. Delicia, M. Maza, M. Chauque, J. Mora, D. Grbavac, L. López, M. Alonso, C. Villalba, M. Simon, M. Cernadas, C. Moscatelli, I. Vilamajó, C. Tursky, M. Martínez, F. Villalba, D. Pereira, S. Araujo, H. López, V. Alonso, B. Vázquez, M. Rapetti, S. Raña, M. Capdevila, C. Ljubich, M. Acosta, M. Coombes, V. Doria, M. Ávila, D. Cáceres, E. Geandet, C. Romero, E. Morales, C. Recalde, S. Marone, M. Casanú, B. Lococo, O. Da Cruz, C. Focsaner, D. Galarce, L. Albarracín, E. Vescovo, M. Gravielle, D. Florio, L. Baumgart, M. Corbalán, V. Aguilera, O. Hermida, C. Galli, L. Ziombra, A. Gutierrez, S. Frydelund, A. Hardaman, A. Maciel, M. Arrigo, C. Mato Mira, J. Leibovich, R. Paparone, E. Muller, A. Malimar, I. Leocadio, W. Cruz, S. Tirado, A. Peñalba, R. Cejas, S. Mansilla, C. Campos, E. Abrego, P. Chávez, G. Corpacci, A. Echavarría, C. Engler, P. Vergara, M. Hubeli, G. Redondo, and B. Noroña. France: C. Boriceanu, M. Lankester, J.L. Poignet, Y. Saingra, M. Indreies, J. Santini, A. Mahi, A. Robert, P. Bouvier, T. Merzouk, F. Villemain, A. Pajot, F. Tollis, M. Brahim-Bounab, A. Benmoussa, S. Albitar, M.C. Guimont, P. Ciobotaru, A. Guerin, and M. Diaconita. Germany: S.H. Hoischen, J. Saupe, I. Ullmann, S. Grosser, J. Kunow, S. Grueger, D. Bischoff, J. Benders, P. Worch, T. Pfab, N. Kamin, M. Roesch, and M. May. Hungary: K. Albert, I. Csaszar, E. Kiss, D. Kosa, A. Orosz, J. Redl, L. Kovacs, E. Varga, M. Szabo, K. Magyar, E. Zajko, A. Bereczki, J. Csikos, E. Kerekes, A. Mike, K. Steiner, E. Nemeth, K. Tolnai, A. Toth, J. Vinczene, S.z. Szummer, E. Tanyi, and M. Szilvia. Italy: A.M. Murgo, N. Sanfilippo, N. Dambrosio, C. Saturno, G. Matera, M. Benevento, V. Greco, G. di Leo, S. Papagni, F. Alicino, A. Marangelli, F. Pedone, A.V. Cagnazzo, R. Antinoro, M.L. Sambati, C. Donatelli, F. Ranieri, F. Torsello, P. Steri, C. Riccardi, A. Flammini, L. Moscardelli, E. Boccia, M. Mantuano, R. Di Toro Mammarella, M. Meconizzi, R. Fichera, A. D’Angelo, G. Latassa, A. Molino, M. Fici, A. Lupo, G. Montalto, S. Messina, C. Capostagno, G. Randazzo, S. Pagano, G. Marino, D. Rallo, A. Maniscalco, O.M. Trovato, C. Strano, A. Failla, A. Bua, S. Campo, P. Nasisi, A. Salerno, S. Laudani, F. Grippaldi, D. Bertino, D.V. Di Benedetto, A. Puglisi, S. Chiarenza, M. Lentini Deuscit, C.M. Incardona, G. Scuto, C. Todaro, A. Dino, D. Novello, and A. Coco. Poland: E. Bocheńska-Nowacka, A. Jaroszyński, J. Drabik, M. Wypych-Birecka, D. Daniewska, M. Drobisz, K. Doskocz, G. Wyrwicz-Zielińska, A. Kosicki, W. Ślizień, P. Rutkowski, S. Arentowicz, S. Dzimira, M. Grabowska, J. Ostrowski, A. Całka, T. Grzegorczyk, W. Dżugan, M. Mazur, M. Myślicki, M. Piechowska, and D. Kozicka. Portugal: V. de Sá Martins, L. Aguiar, A.R. Mira, B. Velez, and T. Pinheiro. Romania: E. Agapi, C.L. Ardelean, A. Baidog, G. Bako, M. Barb, A. Blaga, E. Bodurian, V. Bumbea, E. Dragan, D. Dumitrache, L. Florescu, N. Havasi, S. Hint, R. Ilies, A.G.M. Mandita, R.I. Marian, S.L. Medrihan, L. Mitea, S. Mitea, R. Mocanu, D.C. Moro, M. Nitu, M.L. Popa, M. Popa, E. Railean, A.R. Scuturdean, K. Szentendrey, C.L. Teodoru, and A. Varga. Spain: M. García, M. Olaya, V. Abujder, J. Carreras, A. López, F. Ros, G. Cuesta, A. García, E. Orero, E. Ros, S. Bea, J.L. Pizarro, S. Luengo, A. Romero, M. Navarro, L. Cermeño, A. Rodriguez, D. Lopez, A. Barrera, F. Montoya, J. Tajahuerce, M. Carro, M.Q. Cunill, S. Narci, T. Ballester, M.J. Soler, S. Traver, P.P. Buta, L. Cucuiat, L. Rosu, I. Garcia, C.M. Gavra, R. Gonzalez, S. Filimon, M. Peñalver, V. Benages, M.I. Cardo, E. García, P. Soler, E. Fernnandez, F. Popescu, R. Munteanu, E. Tanase, F. Sagau, D. Prades, S. Esteller, E. Gonzalez, R. Martinez, A. Diago, J. Torres, E. Perez, C. Garcia, I. Lluch, J. Forcano, M. Fóns, A. Rodríguez, N.A. Millán, J. Fernández, B. Ferreiro, M. Otero, V. Pesqueira, S. Abal, R. Álvarez, C. Jorge, I. Rico, J. de Dios Ramiro, L. Duzy, A. Soto, J.L. Lopez, Y. Diaz, I. Herrero, M. Farré, C. Blasco, S. Ferrás, M.J. Agost, C. Miracle, and J. Farto. Sweden: J. Goch, K.S. Katzarski, and A. Wulcan.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
See related editorial, “Diet Patterns—A Neglected Aspect of Hemodialysis Care,” on pages 1581–1582.
This article contains supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2018010008/-/DCSupplemental.
References
- 1.de Jager DJ, Grootendorst DC, Jager KJ, van Dijk PC, Tomas LM, Ansell D, et al. : Cardiovascular and noncardiovascular mortality among patients starting dialysis. JAMA 302: 1782–1789, 2009. 10.1001/jama.2009.1488 [DOI] [PubMed] [Google Scholar]
- 2.Neovius M, Jacobson SH, Eriksson JK, Elinder CG, Hylander B: Mortality in chronic kidney disease and renal replacement therapy: A population-based cohort study. BMJ Open 4: e004251, 2014. 10.1136/bmjopen-2013-004251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Registry ERA-EDTA : ERA-EDTA Registry Annual Report, 2014. Available at: http://www.era-edta-reg.org/files/annualreports/pdf/AnnRep2014.pdf. Accessed February 1, 2018
- 4.Thompson S, James M, Wiebe N, Hemmelgarn B, Manns B, Klarenbach S, et al. : Alberta Kidney Disease Network : Cause of death in patients with reduced kidney function. J Am Soc Nephrol 26: 2504–2511, 2015. 10.1681/ASN.2014070714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.US Renal Data System : USRDS Annual Data Report: Atlas of Chronic Kidney Disease and End-Stage Renal Disease in the United States, Besthesda, MD, National Institute of Diabetes and Digestive and Kidney Diseases, 2015 [Google Scholar]
- 6.Chertow GM, Block GA, Correa-Rotter R, Drüeke TB, Floege J, Goodman WG, et al. : EVOLVE Trial Investigators : Effect of cinacalcet on cardiovascular disease in patients undergoing dialysis. N Engl J Med 367: 2482–2494, 2012. 10.1056/NEJMoa1205624 [DOI] [PubMed] [Google Scholar]
- 7.Cooper BA, Branley P, Bulfone L, Collins JF, Craig JC, Fraenkel MB, et al. : IDEAL Study : A randomized, controlled trial of early versus late initiation of dialysis. N Engl J Med 363: 609–619, 2010. 10.1056/NEJMoa1000552 [DOI] [PubMed] [Google Scholar]
- 8.Eknoyan G, Beck GJ, Cheung AK, Daugirdas JT, Greene T, Kusek JW, et al. : Hemodialysis (HEMO) Study Group : Effect of dialysis dose and membrane flux in maintenance hemodialysis. N Engl J Med 347: 2010–2019, 2002. 10.1056/NEJMoa021583 [DOI] [PubMed] [Google Scholar]
- 9.Palmer SC, Craig JC, Navaneethan SD, Tonelli M, Pellegrini F, Strippoli GF: Benefits and harms of statin therapy for persons with chronic kidney disease: A systematic review and meta-analysis. Ann Intern Med 157: 263–275, 2012. 10.7326/0003-4819-157-4-201208210-00007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Palmer SC, Di Micco L, Razavian M, Craig JC, Perkovic V, Pellegrini F, et al. : Effects of antiplatelet therapy on mortality and cardiovascular and bleeding outcomes in persons with chronic kidney disease: A systematic review and meta-analysis. Ann Intern Med 156: 445–459, 2012. 10.7326/0003-4819-156-6-201203200-00007 [DOI] [PubMed] [Google Scholar]
- 11.Dickinson HO, Mason JM, Nicolson DJ, Campbell F, Beyer FR, Cook JV, et al. : Lifestyle interventions to reduce raised blood pressure: A systematic review of randomized controlled trials. J Hypertens 24: 215–233, 2006. 10.1097/01.hjh.0000199800.72563.26 [DOI] [PubMed] [Google Scholar]
- 12.Shrestha P, Ghimire L: A review about the effect of life style modification on diabetes and quality of life. Glob J Health Sci 4: 185–190, 2012. 10.5539/gjhs.v4n6p185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Franklin BA, Durstine JL, Roberts CK, Barnard RJ: Impact of diet and exercise on lipid management in the modern era. Best Pract Res Clin Endocrinol Metab 28: 405–421, 2014. 10.1016/j.beem.2014.01.005 [DOI] [PubMed] [Google Scholar]
- 14.Estruch R, Ros E, Salas-Salvadó J, Covas MI, Corella D, Arós F, et al. : PREDIMED Study Investigators : Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med 368: 1279–1290, 2013. 10.1056/NEJMoa1200303 [DOI] [PubMed] [Google Scholar]
- 15.Salehi-Abargouei A, Maghsoudi Z, Shirani F, Azadbakht L: Effects of Dietary Approaches to Stop Hypertension (DASH)-style diet on fatal or nonfatal cardiovascular diseases–incidence: A systematic review and meta-analysis on observational prospective studies. Nutrition 29: 611–618, 2013. 10.1016/j.nut.2012.12.018 [DOI] [PubMed] [Google Scholar]
- 16.Sofi F, Macchi C, Abbate R, Gensini GF, Casini A: Mediterranean diet and health status: An updated meta-analysis and a proposal for a literature-based adherence score. Public Health Nutr 17: 2769–2782, 2014. 10.1017/S1368980013003169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen ST, Maruthur NM, Appel LJ: The effect of dietary patterns on estimated coronary heart disease risk: Results from the Dietary Approaches to Stop Hypertension (DASH) trial. Circ Cardiovasc Qual Outcomes 3: 484–489, 2010. 10.1161/CIRCOUTCOMES.109.930685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.de Lorgeril M, Renaud S, Mamelle N, Salen P, Martin JL, Monjaud I, et al. : Mediterranean alpha-linolenic acid-rich diet in secondary prevention of coronary heart disease. Lancet 343: 1454–1459, 1994. 10.1016/S0140-6736(94)92580-1 [DOI] [PubMed] [Google Scholar]
- 19.Shen J, Wilmot KA, Ghasemzadeh N, Molloy DL, Burkman G, Mekonnen G, et al. : Mediterranean dietary patterns and cardiovascular health. Annu Rev Nutr 35: 425–449, 2015. 10.1146/annurev-nutr-011215-025104 [DOI] [PubMed] [Google Scholar]
- 20.Delgado-Lista J, Perez-Martinez P, Garcia-Rios A, Perez-Caballero AI, Perez-Jimenez F, Lopez-Miranda J: Mediterranean diet and cardiovascular risk: Beyond traditional risk factors. Crit Rev Food Sci Nutr 56: 788–801, 2016. 10.1080/10408398.2012.726660 [DOI] [PubMed] [Google Scholar]
- 21.Hummel SL, Seymour EM, Brook RD, Kolias TJ, Sheth SS, Rosenblum HR, et al. : Low-sodium dietary approaches to stop hypertension diet reduces blood pressure, arterial stiffness, and oxidative stress in hypertensive heart failure with preserved ejection fraction. Hypertension 60: 1200–1206, 2012. 10.1161/HYPERTENSIONAHA.112.202705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Siervo M, Lara J, Chowdhury S, Ashor A, Oggioni C, Mathers JC: Effects of the Dietary Approach to Stop Hypertension (DASH) diet on cardiovascular risk factors: A systematic review and meta-analysis. Br J Nutr 113: 1–15, 2015. 10.1017/S0007114514003341 [DOI] [PubMed] [Google Scholar]
- 23.Kelly JT, Palmer SC, Wai SN, Ruospo M, Carrero JJ, Campbell KL, et al. : Healthy dietary patterns and risk of mortality and ESRD in CKD: A meta-analysis of cohort studies. Clin J Am Soc Nephrol 12: 272–279, 2017. 10.2215/CJN.06190616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Palmer SC, Maggo JK, Campbell KL, Craig JC, Johnson DW, Sutanto B, et al.: Dietary interventions for adults with chronic kidney disease. Cochrane Database Syst Rev 4: CD011998, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Palmer SC, Ruospo M, Campbell KL, Garcia Larsen V, Saglimbene V, Natale P, et al. DIET-HD Study investigators : Nutrition and dietary intake and their association with mortality and hospitalisation in adults with chronic kidney disease treated with haemodialysis: Protocol for DIET-HD, a prospective multinational cohort study. BMJ Open 5: e006897, 2015. 10.1136/bmjopen-2014-006897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative : The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J Clin Epidemiol 61: 344–349, 2008. 10.1016/j.jclinepi.2007.11.008 [DOI] [PubMed] [Google Scholar]
- 27.Garcia-Larsen V, Luczynska M, Kowalski ML, Voutilainen H, Ahlström M, Haahtela T, et al. GA2LEN-WP 1.2 ‘Epidemiological and Clinical Studies’ : Use of a common food frequency questionnaire (FFQ) to assess dietary patterns and their relation to allergy and asthma in Europe: Pilot study of the GA2LEN FFQ. Eur J Clin Nutr 65: 750–756, 2011. 10.1038/ejcn.2011.15 [DOI] [PubMed] [Google Scholar]
- 28.Food Standards Agency, Food Portion Sizes (Maff Handbook), 1994. Available at: https://www.amazon.co.uk/Food-Portion-Sizes-Maff-Handbook/dp/0112429610. Accessed February 1, 2018
- 29.Finglas PM, Roe MA, Pinchen HM, Berry R, Church SM, Dodhia SK, et al. : The McCance and Widdowsons’s The Composition of Foods, 7th Ed., London, Public Health England, 2014 [Google Scholar]
- 30.Trichopoulou A, Orfanos P, Norat T, Bueno-de-Mesquita B, Ocké MC, Peeters PH, et al. : Modified Mediterranean diet and survival: EPIC-elderly prospective cohort study. BMJ 330: 991, 2005. 10.1136/bmj.38415.644155.8F [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fung TT, Chiuve SE, McCullough ML, Rexrode KM, Logroscino G, Hu FB: Adherence to a DASH-style diet and risk of coronary heart disease and stroke in women. Arch Intern Med 168: 713–720, 2008. 10.1001/archinte.168.7.713 [DOI] [PubMed] [Google Scholar]
- 32.D’Elia L, Rossi G, Ippolito R, Cappuccio FP, Strazzullo P: Habitual salt intake and risk of gastric cancer: A meta-analysis of prospective studies. Clin Nutr 31: 489–498, 2012. 10.1016/j.clnu.2012.01.003 [DOI] [PubMed] [Google Scholar]
- 33.Hu J, La Vecchia C, Morrison H, Negri E, Mery L; Canadian Cancer Registries Epidemiology Research Group : Salt, processed meat and the risk of cancer. Eur J Cancer Prev 20: 132–139, 2011. 10.1097/CEJ.0b013e3283429e32 [DOI] [PubMed] [Google Scholar]
- 34.Ash S, Campbell KL, Bogard J, Millichamp A: Nutrition prescription to achieve positive outcomes in chronic kidney disease: A systematic review. Nutrients 6: 416–451, 2014. 10.3390/nu6010416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fouque D, Vennegoor M, ter Wee P, Wanner C, Basci A, Canaud B, et al. : EBPG guideline on nutrition. Nephrol Dial Transplant 22[Suppl 2]: ii45–ii87, 2007. 10.1093/ndt/gfm020 [DOI] [PubMed] [Google Scholar]
- 36.Jindal K, Chan CT, Deziel C, Hirsch D, Soroka SD, Tonelli M, et al.; Canadian Society of Nephrology Committee for Clinical Practice Guidelines : Hemodialysis clinical practice guidelines for the Canadian Society of Nephrology. J Am Soc Nephrol 17[Suppl 1]: S1–S27, 2006 [DOI] [PubMed] [Google Scholar]
- 37.Kalantar-Zadeh K, Fouque D: Nutritional management of chronic kidney disease. N Engl J Med 377: 1765–1776, 2017. 10.1056/NEJMra1700312 [DOI] [PubMed] [Google Scholar]
- 38.Palmer SC, Hanson CS, Craig JC, Strippoli GF, Ruospo M, Campbell K, et al. : Dietary and fluid restrictions in CKD: A thematic synthesis of patient views from qualitative studies. Am J Kidney Dis 65: 559–573, 2015. 10.1053/j.ajkd.2014.09.012 [DOI] [PubMed] [Google Scholar]
- 39.Liu Z, Su G, Guo X, Wu Y, Liu X, Zou C, et al.: Dietary interventions for mineral and bone disorder in people with chronic kidney disease. Cochrane Database Syst Rev 9: CD010350, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McMahon EJ, Campbell KL, Bauer JD, Mudge DW: Altered dietary salt intake for people with chronic kidney disease. Cochrane Database Syst Rev 2: CD010070, 2015 [DOI] [PubMed] [Google Scholar]
- 41.Naylor HL, Jackson H, Walker GH, Macafee S, Magee K, Hooper L, et al. British Dietetic Association : British Dietetic Association evidence-based guidelines for the protein requirements of adults undergoing maintenance haemodialysis or peritoneal dialysis. J Hum Nutr Diet 26: 315–328, 2013. 10.1111/jhn.12052 [DOI] [PubMed] [Google Scholar]
- 42.Tong A, Crowe S, Chando S, Cass A, Chadban SJ, Chapman JR, et al. : Research priorities in CKD: Report of a national workshop conducted in Australia. Am J Kidney Dis 66: 212–222, 2015. 10.1053/j.ajkd.2015.02.341 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.