Abstract
Background Direct quantitative measurement of GFR (mGFR) remains a specialized task primarily performed in research settings. Multiple formulas for estimating GFR have been developed that use the readily available endogenous biomarkers creatinine and/or cystatin C. However, eGFR formulas have limitations, and an accurate mGFR is necessary in some clinical situations and for certain patient populations. We conducted a prospective, open-label study to evaluate a novel rapid technique for determining plasma volume and mGFR.
Methods We developed a new exogenous biomarker, visible fluorescent injectate (VFI), consisting of a large 150-kD rhodamine derivative and small 5-kD fluorescein carboxymethylated dextrans. After a single intravenous injection of VFI, plasma volume and mGFR can be determined on the basis of the plasma pharmacokinetics of the rhodamine derivative and fluorescein carboxymethylated dextrans, respectively. In this study involving 32 adults with normal kidney function (n=16), CKD stage 3 (n=8), or CKD stage 4 (n=8), we compared VFI-based mGFR values with values obtained by measuring iohexol plasma disappearance. VFI-based mGFR required three 0.5-ml blood draws over 3 hours; iohexol-based mGFR required five samples taken over 6 hours. Eight healthy participants received repeat VFI injections at 24 hours.
Results VFI-based mGFR values showed close linear correlation with the iohexol-based mGFR values in all participants. Injections were well tolerated, including when given on consecutive days. No serious adverse events were reported. VFI-based mGFR was highly reproducible.
Conclusions The VFI-based approach allows for the rapid determination of mGFR at the bedside while maintaining patient safety and measurement accuracy and reproducibility.
Keywords: Biomarker, FAST BioMedical, acute kidney injury, chronic kidney disease, fluorescent glomerular filtration rate measurement, kidney function
The best index of renal function remains the GFR.1 Its measurement relies on an ideal filtration marker that is neither absorbed nor secreted by the nephron and does not alter kidney function. To date, urinary clearance during a continuous infusion of inulin is considered the gold standard for such a measurement.1 In clinical practice, inulin-based measurement of GFR (mGFR) is difficult to perform, expensive, and injectable inulin is presently not available in all countries, including the United States. Thus, clinicians rely primarily on eGFR formulas using levels of readily available endogenous markers such as creatinine2,3 and cystatin C.4 Despite their marked contribution to patient care, eGFR formulas have significant limitations. In this study, we present the results of a novel biomarker showing very promising results for the measurement of GFR and plasma volume at the bedside.
Methods
Study Design
This was a phase 2b, prospective, open-label study (clinicaltrials.gov identifier NCT03095391) conducted at two sites: the University of Alabama at Birmingham and the Clinical Research Organization ICON. Four cohorts (of eight participants each) were enrolled between June 13, 2017 and August 30, 2017. All participants provided written informed consent and the study adhered to the Declaration of Helsinki. The study aimed to assess the safety and tolerability of visible fluorescent injectate (VFI) and to compare the GFRs determined by FAST mGFR technology (VFI mGFR) with iohexol clearance. VFI consisted of 12 mg of FD003 and 35 mg of FD001 (150 and 5 kD conjugated dextrans, respectively). VFI was infused intravenously over 30 seconds and blood samples were subsequently collected at 15, 60, and 170 minutes. Blood plasma was diluted at 250 µl of plasma to 2.0 ml of a fluorescence-enhancing reagent and analyzed on a Turner Trilogy filter fluorimeter to determine the concentrations of FD001 and FD003, respectively. Plasma volume was determined using the early time point, and the concentration of the small dextran GFR marker at time zero was calculated from the measured plasma volume. The four time points (0, 15, 60, and 170 minutes) were then fitted using a two-compartment model and the resulting area under the curve was calculated. The use of the time point 0 determination helped to better resolve the shape of the clearance curve. mGFR was calculated and adjusted to body surface area for comparison with iohexol clearance. For iohexol clearance determination, 5 ml of Omnipaque 300 was infused over 2 minutes and blood samples were taken at 120, 150, 180, 210, and 320 minutes. The University of Minnesota Advanced Research and Diagnostic Laboratory analyzed the samples. This iohexol method uses the Brochner–Mortensen method of calculation, and has proven to be an accurate comparator.5
Cohorts one and two consisted of healthy volunteers, and cohorts three and four included patients with CKD stage 3 and 4, respectively, with variable degrees of proteinuria. Eligible participants had to be 18–75 years old, with a body mass index ≥18 and ≤40 kg/m2. Men and women agreed to use medically acceptable methods of contraception (except for participants who were confirmed sterile or postmenopausal females).
All participants underwent VFI mGFR determination within 21 days of screening. Cohort two received an additional VFI dose 24 hours after the first injection. Cohorts two, three, and four had iohexol-based GFR determination as well. Participants were followed for 21(±1) days from their last VFI injection. All visits were conducted in the clinical research unit.
Study Variables
Demographics, medical and surgical history (including concomitant medication use), height, weight, vital signs, and physical examinations were documented. Laboratory tests included chemistry, hematology, hepatic function panel, follicular stimulating hormone (women only), creatinine phosphokinase, HIV, and hepatitis C and B serologies, as well as urine pregnancy tests and drug screens. Twelve-lead electrocardiograms were obtained. eGFR for eligibility were determined using the CKD Epidemiology Collaboration equation.3 Participants were assessed for adverse and serious adverse events at each encounter.
Statistical Analyses
A descriptive analysis of study results was reported. Correlation between FAST mGFR and iohexol GFR was determined using Pearson correlation. Bland–Altman analysis determined the limits of agreement.6
Results
Thirty three participants were screened and consented. One participant from cohort three had to be withdrawn as no intravenous access could be secured to conduct the study, leaving 32 participants enrolled and included in the current analysis. Baseline characteristics of all participants are shown in Table 1. The mean age was 56.1 years (range 19–75), and 56% were women. There was diverse racial and ethnic representation, with 41% white, 31% black, and 9% Hispanic participants.
Table 1.
Baseline characteristics of participants in all four cohorts
| Cohort | Participant ID | Race | Ethnicity | Sex | Age, yr | Weight, kg | Height, cm |
|---|---|---|---|---|---|---|---|
| Cohort 1 | 1009 | White | Hispanic or Latino | F | 19 | 59 | 158 |
| 1010 | White | Hispanic or Latino | M | 64 | 92 | 171 | |
| 1011 | White | Hispanic or Latino | M | 58 | 92 | 176 | |
| 1012 | Black | Not Hispanic or Latino | F | 47 | 91 | 176 | |
| 1013 | White | Not Hispanic or Latino | F | 69 | 83 | 163 | |
| 1014 | White | Hispanic or Latino | F | 51 | 82 | 160 | |
| 1015 | Black | Not Hispanic or Latino | F | 30 | 74 | 171 | |
| 1016 | White | Hispanic or Latino | F | 48 | 65 | 153 | |
| Cohort 2 | 1001 | White | Not Hispanic or Latino | M | 24 | 74.6 | 171.5 |
| 1002 | White | Hispanic or Latino | F | 69 | 59.2 | 152.1 | |
| 1003 | White | Not Hispanic or Latino | M | 62 | 76.8 | 168.5 | |
| 1004 | White | Not Hispanic or Latino | M | 34 | 79.5 | 175.4 | |
| 1005 | White | Hispanic or Latino | F | 75 | 63.6 | 152 | |
| 1006 | White | Not Hispanic or Latino | F | 50 | 85.7 | 169.8 | |
| 1007 | White | Not Hispanic or Latino | F | 61 | 57.1 | 164 | |
| 1008 | White | Hispanic or Latino | M | 68 | 70 | 160 | |
| Cohort 3 | 2001 | White | Not Hispanic or Latino | M | 68 | 110.3 | 192.2 |
| 2004 | White | Not Hispanic or Latino | F | 52 | 68.1 | 161.6 | |
| 2005 | White | Not Hispanic or Latino | M | 74 | 102.4 | 177.5 | |
| 2006 | White | Not Hispanic or Latino | F | 70 | 76.4 | 156.5 | |
| 2007 | White | Not Hispanic or Latino | M | 73 | 103.5 | 179.8 | |
| 1017 | White | Hispanic or Latino | M | 70 | 105.6 | 169 | |
| 1018 | Black | Not Hispanic or Latino | M | 53 | 114.8 | 173.9 | |
| 2016 | Black | Not Hispanic or Latino | F | 62 | 76.6 | 165.6 | |
| Cohort 4 | 2003 | Black | Not Hispanic or Latino | M | 59 | 84.3 | 184.4 |
| 2009 | Black | Not Hispanic or Latino | M | 69 | 147 | 194.5 | |
| 2010 | White | Not Hispanic or Latino | F | 74 | 88.7 | 165.7 | |
| 2011 | Black | Not Hispanic or Latino | F | 43 | 92.4 | 160.8 | |
| 2012 | Black | Not Hispanic or Latino | F | 49 | 90.1 | 161 | |
| 2014 | White | Not Hispanic or Latino | M | 49 | 86.4 | 179.2 | |
| 2015 | Black | Not Hispanic or Latino | F | 57 | 98.9 | 161.2 | |
| 2017 | Black | Not Hispanic or Latino | F | 46 | 88.9 | 177.8 |
F, female; M, male.
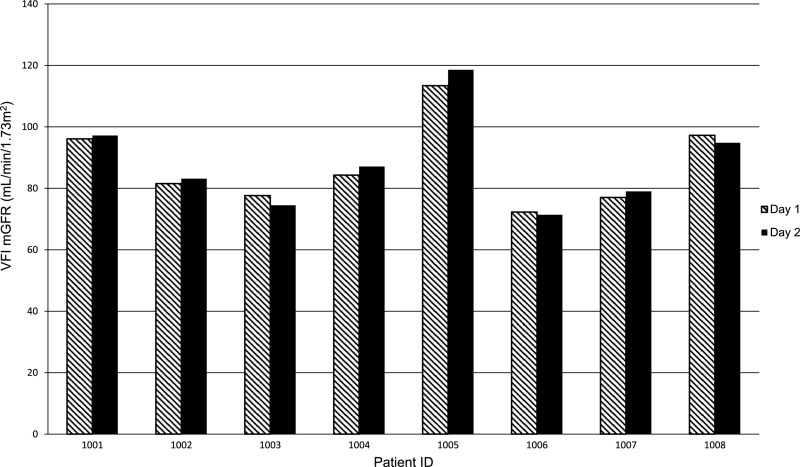
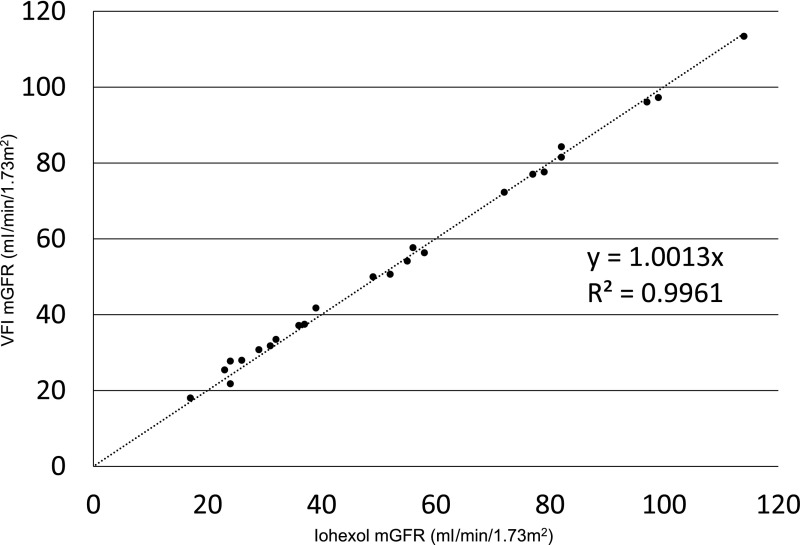
VFI administration was well tolerated across all ranges of kidney function and no serious adverse events were reported. The 24-hour repeat VFI mGFR assessment in eight healthy participants (cohort two) showed reliable reproducibility within 5% of baseline GFR values (Figure 1, Table 2). VFI mGFR required three 0.5-ml blood draws over 2.5 hours and were compared with iohexol mGFR on the basis of plasma disappearance studies, using samples taken over 6 hours. Across all cohorts, the VFI mGFR showed near perfect linear correlation when compared with iohexol mGFR, with a coefficient correlation value of 0.996 (Figure 2). Next, a Bland–Altman analysis was performed (Supplemental Figure 1) and confirmed agreement between the two measures of GFR, with a mean difference of −0.49 ml/min (95% confidence interval, −3.65 to +2.68). A representative normalized comparison of the GFR curves for a normal and CKD stage 4 participants is shown in Supplemental Figure 2.
Figure 1.
Repeat measurements of VFI mGFR in cohort two participants show very good reproducibility. The dashed line represents VFI mGFR values adjusted for body surface area, obtained on day 1. The solid black line represents VFI mGFR values adjusted for body surface area obtained on day 2, after the second VFI injection at 24 hours. The results show reliable reproducibility within 5% of baseline mGFR values. The VFI mGFR numerical values are provided in Table 2.
Table 2.
Comparison of VFI mGFR with iohexol mGFR, and eGFR by CKD-EPI and MDRD formulas in all four cohorts
| Cohort | Participant ID | Iohexol mGFR, ml/min per 1.73 m2 | FAST mGFR, ml/min per 1.73 m2 | Creatinine, mg/dl | CKD-EPI eGFR, ml/min per 1.73 m2 | MDRD eGFR, ml/min per 1.73 m2 | FAST PV, ml |
| Cohort 1: healthy participants | 1009 | N/A | 111 | 0.6 | 133 | 129 | 2115 |
| 1010 | 73 | 1.1 | 71 | 67 | 3050 | ||
| 1011 | 87 | 1.0 | 83 | 77 | 3187 | ||
| 1012 | 112 | 0.7 | 120 | 109 | 3443 | ||
| 1013 | 77 | 0.7 | 89 | 83 | 2775 | ||
| 1014 | 89 | 0.7 | 101 | 88 | 3057 | ||
| 1015 | 113 | 0.7 | 135 | 119 | 2649 | ||
| 1016 | 102 | 0.6 | 108 | 107 | 2667 | ||
| Cohort 2: healthy participants; repeat VFI dose | 1001 | 97 | 96 | 0.9 | 119 | 104 | 2632 |
| 97 | 119 | 104 | |||||
| 1002 | 82 | 82 | 0.7 | 89 | 83 | 2294 | |
| 83 | 89 | 83 | |||||
| 1003 | 79 | 78 | 0.7 | 101 | 114 | 3226 | |
| 74 | 101 | 114 | |||||
| 1004 | 82 | 84 | 1.1 | 87 | 77 | 2487 | |
| 87 | 87 | 77 | |||||
| 1005 | 114 | 113 | 0.5 | 95 | 120 | 2457 | |
| 119 | 95 | 120 | |||||
| 1006 | 72 | 72 | 0.7 | 101 | 89 | 2462 | |
| 71 | 101 | 89 | |||||
| 1007 | 77 | 77 | 0.8 | 80 | 73 | 2335 | |
| 79 | 80 | 73 | |||||
| 1008 | 99 | 97 | 0.6 | 103 | 134 | 2457 | |
| 95 | 103 | 134 | |||||
| Cohort 3: 30≤eGFR<60 ml/min per 1.73 m2 | 2001 | 58 | 56 | 1.4 | 51 | 50 | 3609 |
| 2004 | 36 | 37 | 1.1 | 58 | 52 | 2247 | |
| 2005 | 52 | 51 | 1.2 | 59 | 59 | 3288 | |
| 2006 | 56 | 58 | 1.0 | 57 | 55 | 2224 | |
| 2007 | 55 | 54 | 1.4 | 49 | 69 | 4181 | |
| 2016 | 37 | 37 | 1.8 | 34 | 35 | 2505 | |
| 1017 | 39 | 42 | 1.5 | 46 | 46 | 3347 | |
| 1018 | 49 | 50 | 1.9 | 46 | 45 | 3458 | |
| Cohort 4: 15≤eGFR<30 ml/min per 1.73 m2 | 2003 | 32 | 33 | 2.9 | 26 | 39 | 3631 |
| 2009 | 17 | 18 | 3.4 | 20 | 22 | 6234 | |
| 2010 | 29 | 31 | 1.7 | 29 | 29 | 3042 | |
| 2011 | 24 | 28 | 3.2 | 20 | 19 | 3204 | |
| 2012 | 23 | 25 | 2.7 | 23 | 23 | 3057 | |
| 2014 | 24 | 22 | 3.3 | 21 | 20 | 3556 | |
| 2015 | 31 | 32 | 2.2 | 28 | 28 | 2899 | |
| 2017 | 26 | 28 | 2.6 | 25 | 24 | 3409 |
CKD EPI, CKD Epidemiology Collaboration Equation; MDRD, Modification of Diet in Renal Disease equation; FAST PV, visible fluorescent injectate–based plasma volume measurement; N/A, not applicable.
Figure 2.
Linear correlation of VFI mGFR (ml/min per 1.73 m2) and iohexol mGFR (ml/min per 1.73 m2) show a coefficient of determination of R2=0.996. VFI mGFR adjusted for body surface area correlated linearly with iohexol mGFR adjusted for body surface area.
Discussion
The gold standard for measuring GFR is inulin clearance; however, the need for a continuous infusion and multiple blood and urine collections limit its use even in research settings. Other methods using chromium 51-EDTA, iothalamate, and iohexol are acceptable alternatives but remain cumbersome, as they require specialized laboratory determinations and their assays can be expensive to perform.1 In clinical practice, physicians have turned to endogenous biomarkers, such as creatinine, which are readily available. Creatinine-based eGFR formulas are widely used and represent the basis for many diagnostic and management guidelines.2–4,7 Despite its widespread use, eGFR has limitations in special populations (those with abnormal muscle mass or body surface area), during changes in metabolism (like pregnancy), and when GFR is not steady (during growth, AKI, or after consumption of a high-protein diet).8 Additionally, eGFR is least accurate when creatinine is normal and does not allow for the measurement of renal reserve.9,10 Since the initial introduction of the Modification of Diet in Renal Disease eGFR equation,2 many reiterations of the creatinine-based formula have been published, addressing some of the equation imprecisions across the GFR range, full-age spectrum, and different racial and ethnic backgrounds.3,11 Other endogenous biomarkers have been explored as alternatives. Of particular interest is cystatin C (which does not share the inherent limitations of creatinine), especially after the standardization of its assay.11,12 Estimating equations are practical but do not supersede the need for a direct measurement of GFR.13 The search for a practical and safe exogenous biomarker that will allow a rapid assessment of GFR has been long in the making. Technical advances allowed the measurement of fluorescence intensity decay after a bolus injection of a fluorescence-labeled marker into rodents.14 These measurements correlated well with kidney function. Subsequently, using a single bolus of two distinct fluorescence-labeled conjugates (one rapidly filtered by the kidneys and another confined to the vascular space) into rats markedly improved the accuracy of these measurements,14,15 and they proved reproducible in larger animal models.16 The results of our phase 2b study show VFI to be a safe biomarker that allows the accurate, rapid, and reproducible measurement of GFR at the bedside in healthy volunteers and across a wide range of CKD. Determining the time point 0 concentration (using the large dextran molecule) improves the measurement accuracy and reduces the time and number of blood draws needed. Additionally, our technique uses a two-compartment model instead of a one-compartment model (as for iohexol and iothalamate), allowing us to measure vascular and not extracellular clearance of the marker. Therefore, less time is needed to generate an mGFR value even at more advanced stages of CKD. Further confirmatory testing in patients with CKD stage 5 is needed. Patients with very large body weights may require a longer time for the VFI to reach steady state, and future studies will determine whether mGFR generation will need an additional time point in that patient population. The fluorescent dyes in VFI allow a rapid read-out, whereas measuring GFR with iohexol or iothalamate requires time-consuming assay analysis using HPLC or mass spectrometry. The two-marker injectate is a promising biomarker for measurement of GFR. This novel technique will potentially allow clinicians to detect early renal function and reserve loss across a wider spectrum of patients, hence introducing earlier treatments to prevent renal loss. It will also allow for identification of hyperfiltration and earlier mitigating therapy. The ability to measure GFR may also change participant selection in research studies and allow for more accurate and timely outcome measures.
Disclosures
D.V.R. received research funding from FAST BioMedical. D.M. is an employee of FAST BioMedical. R.M.S. is a paid consultant for FAST BioMedical and TdB Consultancy, which collaborates with FAST BioMedical on dextran development. E.S.R. is an employee of FAST BioMedical. J.C.S. received research funding from FAST BioMedical to perform assays. E.D. received research funding from FAST BioMedical. J.S.S. is a cofounder, President, Director, and stockholder in FAST BioMedical. J.M. is the Chief Executive Officer and stock owner in FAST BioMedical. T.C. received research funding from FAST BioMedical. B.A.M. is a cofounder, partial owner, and Medical Director of FAST BioMedical.
Supplementary Material
Acknowledgments
D.M., E.S.R., J.S.S., and B.A.M. designed the study; D.V.R., T.C., and E.D. carried out the experiments; D.M., B.A.M., D.V.R., and J.C.S. analyzed the data; E.S.R. made the figures; D.V.R. drafted the manuscript and D.M., R.M.S., T.C., E.S.R., J.C.S., E.D., J.S.S., J.M., and B.A.M. revised the manuscript; all authors approved the final version of the manuscript.
This research was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under award UL1TR001417, and the Small Business Innovation Research phase 2b grant 1R44DK093274-04.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
This article contains supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2018020160/-/DCSupplemental.
References
- 1.Soveri I, Berg UB, Björk J, Elinder CG, Grubb A, Mejare I, et al.; SBU GFR Review Group : Measuring GFR: A systematic review. Am J Kidney Dis 64: 411–424, 2014 [DOI] [PubMed] [Google Scholar]
- 2.Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D; Modification of Diet in Renal Disease Study Group : A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Ann Intern Med 130: 461–470, 1999 [DOI] [PubMed] [Google Scholar]
- 3.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al.; CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration) : A new equation to estimate glomerular filtration rate. Ann Intern Med 150: 604–612, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Inker LA, Schmid CH, Tighiouart H, Eckfeldt JH, Feldman HI, Greene T, et al.; CKD-EPI Investigators : Estimating glomerular filtration rate from serum creatinine and cystatin C. N Engl J Med 367: 20–29, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brochner-Mortensen J : A Simple Method for the Determination of Glomerular Filtration Rate. Scand J Clin Lab Invest 30: 271–274, 1972 [DOI] [PubMed] [Google Scholar]
- 6.Bland JM, Altman DG : Measuring agreement in method comparison studies. Stat Methods Med Res 8: 135–160, 1999 [DOI] [PubMed] [Google Scholar]
- 7.Kidney Disease: Improving Global Outcomes (KDIGO) Anemia Work Group : KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl 3: 136–150, 2013 [Google Scholar]
- 8.Filler G, Lee M: Educational review: Measurement of GFR in special populations [published online ahead of print December 7, 2017]. Pediatr Nephrol 10.1007/s00467-017-3852-8 [DOI] [PubMed] [Google Scholar]
- 9.Levey AS, Inker LA, Matsushita K, Greene T, Willis K, Lewis E, et al.: GFR decline as an end point for clinical trials in CKD: A scientific workshop sponsored by the National Kidney Foundation and the US Food and Drug Administration. Am J Kidney Dis 64: 821–835, 2014 [DOI] [PubMed] [Google Scholar]
- 10.Molitoris BA: Rethinking CKD evaluation: Should we be quantifying basal or stimulated GFR to maximize precision and sensitivity? Am J Kidney Dis 69: 675–683, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pottel H, Hoste L, Dubourg L, Ebert N, Schaeffner E, Eriksen BO, et al.: An estimated glomerular filtration rate equation for the full age spectrum. Nephrol Dial Transplant 31: 798–806, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grubb A, Blirup-Jensen S, Lindström V, Schmidt C, Althaus H, Zegers I; IFCC Working Group on Standardisation of Cystatin C (WG-SCC) : First certified reference material for cystatin C in human serum ERM-DA471/IFCC. Clin Chem Lab Med 48: 1619–1621, 2010 [DOI] [PubMed] [Google Scholar]
- 13.Agarwal R: Glomerular filtration rate estimating equations: Practical, yes, but can they replace measured glomerular filtration rate? Nephrol Dial Transplant 32: 405–407, 2017 [DOI] [PubMed] [Google Scholar]
- 14.Yu W, Sandoval RM, Molitoris BA: Rapid determination of renal filtration function using an optical ratiometric imaging approach. Am J Physiol Renal Physiol 292: F1873–F1880, 2007 [DOI] [PubMed] [Google Scholar]
- 15.Wang E, Sandoval RM, Campos SB, Molitoris BA: Rapid diagnosis and quantification of acute kidney injury using fluorescent ratio-metric determination of glomerular filtration rate in the rat. Am J Physiol Renal Physiol 299: F1048–F1055, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang E, Meier DJ, Sandoval RM, Von Hendy-Willson VE, Pressler BM, Bunch RM, et al.: A portable fiberoptic ratiometric fluorescence analyzer provides rapid point-of-care determination of glomerular filtration rate in large animals. Kidney Int 81: 112–117, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.