Abstract
As hybrid closed-loop (HCL) insulin delivery systems permeate clinical practice, it is critical to ensure all with diabetes are afforded the opportunity to benefit from this technology. Indeed, due to the suboptimal control achieved by the vast majority of youth with type 1 diabetes (T1D), pediatric patients are positioned to see the greatest benefit from automated insulin delivery systems. To ensure these systems are well poised to deliver the promise of more targeted control, it is essential to understand the unique characteristics and factors of childhood. Herein, the developmental and physiological needs of youth with T1D are reviewed and consideration is given to how HCL could address these issues. Studies of HCL technologies in youth are briefly reviewed. As future-generation closed-loop systems are being devised, features that could make this technology more attractive to youth and to their families are discussed. Integration of HCL has the potential to minimize the burden of this chronic medical condition while improving glycemic control and ultimately allowing our pediatric patients to fulfill the primary goal of childhood, to be a kid.
Introduction
“Children are not small adults” is a phrase that every pediatric practitioner becomes well aware of during training. Indeed, the developmental changes that are the hallmark of this stage of life will never be recapitulated. In growing children with type 1 diabetes (T1D), the burden of having to constantly adjust insulin needs is a never-ending challenge, especially when growth and development accelerate during puberty. It is not surprising that the summit of suboptimal control of T1D is observed in adolescence (1). Pivotal trials of new drugs and technologies for diabetes are typically carried out first in adults, not only to avoid unnecessary exposure of children to unexpected adverse effects of new therapies but also because near-optimal control of T1D is much more common in adults than in children and adolescents. Thus, it is of utmost importance to consider factors that require special attention during childhood.
In our youngest patients, the inability to communicate needs may lead caregivers to adopt a strategy of constant vigilance (2). Despite such vigilance, it was reported that 90% of hypoglycemic events detected by blinded continuous glucose monitoring (CGM) in infants and toddlers occurred without concomitant symptoms of hypoglycemia detected by their caregivers (3). Due to unpredictable changes in appetite and food intake, many families of young children administer meal boluses after instead of before eating, even at the expense of greater postprandial hyperglycemia and the suboptimal glycemic control that this approach is associated with (4). Nighttime is often the worst time for parents of young children with diabetes due to fears about hypoglycemia, which leads to disturbed sleep patterns secondary to the need to monitor overnight blood glucose levels two or more times per night (5,6).
School-aged children are in the care of numerous adults throughout the day: parents, teachers, coaches, after-school caretakers, and school bus drivers. The competency of these adults to care for a child with diabetes can be quite variable (7). Furthermore, nearly 45% of parents indicated that their school-aged children themselves were the primary person taking care of their diabetes during school days (7). Fear of hypoglycemia may prompt parents to set higher target blood glucose levels especially during school hours (8,9).
The insulin resistance of puberty is not the only challenge faced by adolescents with T1D (10). Adolescence is a stage of tumultuous emotional upheaval, during which teenagers vie for autonomy. Unfortunately, such autonomy is too often expressed by the refusal to engage in the daily tasks of diabetes treatment, and “diabetes burnout” is all too common in this age-group. This increases the need for continued parental and clinician support to encourage teens to help develop and maintain their commitment to treatment goals (11). While toddlers may not have the communication skills necessary to assist with their care, teenagers often lack desire to communicate with their parents and friends about their condition.
Why Is Integration of Pumps and Sensors in Youth With T1D Critical?
Paradoxically, most advances in diabetes technology that began with the introduction of insulin pump therapy 40 years ago (8,9) have increased rather than decreased the burdens of managing T1D. Despite evidence that these new devices could lower HbA1c levels and reduce the risks of diabetic ketoacidosis and severe hypoglycemia, their uptake in youth with diabetes was markedly delayed (12). It was not until the turn of the century that use of pump therapy became commonplace in the pediatric population. Even now, epidemiological data from T1D registries in the U.S. and Europe indicate that ∼50% of youth with T1D use insulin pumps (13). Moreover, a small percentage of youth with T1D were using CGM consistently and effectively until very recently because the burdens and hassles of using these devices outweighed the benefits perceived by parents and children alike (1,14).
Despite the checkered early history of pump and CGM use in pediatrics, there is now clear evidence that times are changing. More recent T1D Exchange registry data indicate a steady increase in pump use and an even more impressive four- to fivefold jump in use of CGM in children and adolescents (15). Why the change? Insulin pumps keep getting smarter, with the integration of bolus calculators and insulin on board features to help prevent stacking of doses, and CGM devices have become so accurate that sensor glucose values can replace the need for confirmatory blood glucose meter measurements. Nevertheless, the most important breakthrough has been the successful integration of both pumps and sensors into a single system that can provide feedback control of the rates of insulin delivery. Pediatric providers now have transformational devices available that can improve clinical outcomes with less effort required by the patient and their families. Furthermore, these devices have the opportunity to minimize human error, such as inaccurate carbohydrate counting, that often occurs in clinical practice.
Why Hybrid Closed-Loop Rather Than Full Closed-Loop Delivery?
It is important to note that the first generation of artificial pancreas systems will use a hybrid, semiautomatic approach instead of functioning as a fully closed-loop insulin delivery system (16). With hybrid closed-loop (HCL) devices, overnight and between-meal insulin infusion rates are varied automatically in response to changes in sensor glucose values. However, the maximum hourly insulin infusion rate is severely limited in order to mitigate patient injury due to overdelivery of insulin due to a system malfunction. Consequently, as in open-loop treatment, premeal boluses sufficient to cover the carbohydrate content of meals still have to be manually administered by the patient.
Benefits of HCL Control in Pediatrics
It is clear that many of the special challenges in managing diabetes borne by parents of young children with T1D will be alleviated with the use of the first-generation HCL systems. Importantly, parents can be reassured that automated suspension of basal insulin based on a predicted low sensor glucose level will mitigate the risk of hypoglycemia. Conversely, in older children and adolescents who may forget, whether consciously or subconsciously, to take premeal boluses, the HCL system will automatically increase between-meal insulin infusion rates to minimize postmeal hyperglycemia, albeit to a limited extent. With constant growth and development, a key feature of childhood, use of HCL systems that use adaptive algorithms for changing insulin needs will provide patients with a seamless means of reaching prescribed glycemic targets.
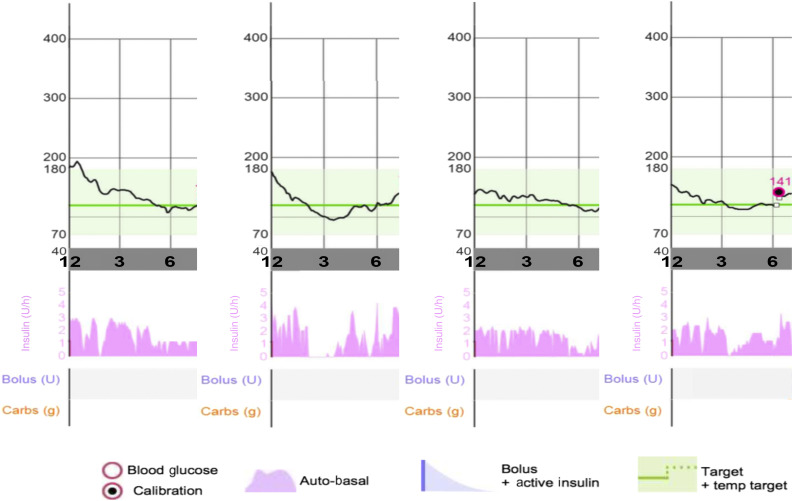
Perhaps the most important feature of HCL systems is their ability to automatically regulate overnight insulin infusion rates based on changes in sensor glucose values. Einstein defined insanity as doing the same thing over and over again and expecting a different result. However, in T1D patients receiving open-loop therapy, insanity is doing the same thing over and over again and always getting a different result. Because so many factors alter insulin requirements during the night, almost every night in the life of a patient with T1D receiving fixed overnight basal rates has been an adventure. In contrast, as illustrated in Fig. 1, HCL systems are able to vary insulin infusion rates from night to night and during different times of the night to mitigate both hyper- and hypoglycemic excursions; namely, doing something different every night but always getting a good result. Moreover, patients and parents may benefit from improved sleep patterns, as the need for intermittent overnight blood glucose meter measurements and sensor alarms will be minimized. Indeed, improved sleep has been endorsed by participants in studies of HCL insulin delivery that assessed the psychosocial impact of system use (17–20).
Figure 1.
Four nights (12 a.m.–7 a.m.) in a single patient using the 670G system. In each panel, sensor glucose tracing is represented as the black line, with the system set point of 120 mg/dL (6.7 mmol/L) denoted by the solid green line. The target range of 70–180 mg/dL (3.9–10 mmol/L) is shaded in light green. The lower panel displays in pink the variable automated basal insulin delivery (Auto-basal) that is driven by the sensor glucose values. Carbs, carbohydrates; temp, temporary; U, units.
Studies of HCL Therapy in Youth
Over the last decade, studies of HCL devices in youth rapidly progressed from short-term safety and feasibility studies conducted in clinical research facilities to assessments of these investigational devices in more transitional environments afforded by camps and hotels (21–27). The vast majority of these studies demonstrated the superiority of closed-loop insulin delivery as compared with either conventional pump therapy or sensor-augmented pump therapy, with decreased frequency of hypoglycemia and increased time in target range, especially during the night (21,22,24–27). These studies set the stage for testing HCL devices in the real world (21–30). During most of the free-living outpatient studies, there was a 10–20% increase in time in target range with a concomitant reduction in frequency of hypoglycemia.
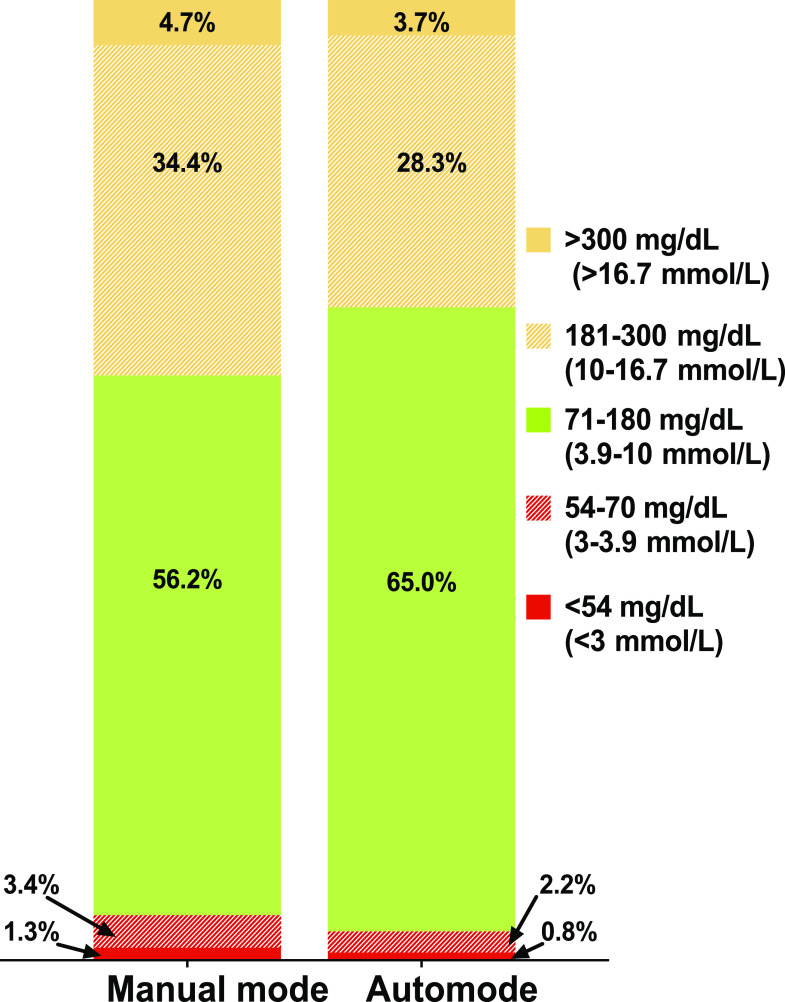
In 2016, the U.S. Food and Drug Administration approved the first HCL system, the Medtronic MiniMed 670G system, based on a 3-month, single-arm study that included 30 adolescents (defined as those aged 14–21 years: mean ± SD age 16.5 ± 2.29 years) and 94 adults (defined as age 22–75 years: mean ± SD age 44.6 ± 12.79 years) with T1D (28). In both age-groups, there were no episodes of diabetic ketoacidosis or severe hypoglycemia. Furthermore, time in range increased, and HbA1c was reduced by 0.6% (6.6 mmol/mol) in adolescents and 0.5% (5.5 mmol/mol) in adults (P < 0.001 compared with baseline values in both groups) (29). More recently, the same design was used in a pediatric study of 105 participants aged 7–13 years (30). Once again, HCL control in these younger patients resulted in a reduction in HbA1c (from 7.9% [62.3 mmol/mol] to 7.5% [58.8 mmol/mol], P < 0.001) and an increase in time in target range (Fig. 2) (30). Ongoing studies will assess the use of this system in 2- to 6-year-olds. Additionally, numerous trials of closed-loop insulin delivery in youth are being conducted (Table 1).
Figure 2.
Comparison of time in target ranges during the 2-week run-in phase using open-loop pump settings to data from the 3-month HCL period for pediatric participants (aged 7–13 years old) in the 670G trial (30).
Table 1.
Studies from ClinicalTrials.gov of closed-loop insulin delivery in youth with T1D
| Study title | Age for inclusion | Environment* | ClinicalTrials.gov identifier | Device | Duration of closed-loop treatment |
|---|---|---|---|---|---|
| Safety Evaluation of the Hybrid Closed Loop (HCL) System in Pediatric Subjects With Type 1 Diabetes | 2–13 years | Free living | NCT02660827 | Medtronic 670G | Single-arm, nonrandomized 2-week run-in with usual pump settings, then 3-month HCL use |
| Comparison of Two Closed-Loop Strategies for Glucose Control in Type 1 Diabetes: The DREMED Trial-2 | 12–25 years | Segment 1: inpatient; segments 2 and 3: transitional (camp) | NCT02776696 | HCL vs. advanced HCL system | Segment 1: two 36-h inpatient admissions; segment 2: RCT with 2 days on each treatment; segment 3: randomized parallel design for 12 days on one of four HCL systems |
| Glycemic Control and the Brain in Children With Type 1 Diabetes | 14–17 years | Free living | NCT03428932 | Medtronic 670G | 6-month RCT of usual care vs. HCL |
| Cross-over Study to Evaluate the Safety and Efficacy of Night Closed-loop Control Using the MD-Logic Automated Insulin Delivery System Compared to Sensor Augmented Pump Therapy in Poorly Controlled Patients With Type 1 Diabetes | 10–18 years | Free living, nighttime closed-loop control | NCT02733211 | MD-Logic Automated Insulin Delivery System | 4-week crossover study of closed-loop insulin delivery overnight vs. SAP |
| The Artificial Pancreas in Very Young Children With T1D - Pilot (KidsAP01) | 1–7 years | Free living | NCT03101865 | FlorenceM closed-loop system | 3-week comparison of HCL using standard concentration insulin vs. diluted insulin |
| Closed Loop From Onset in Type 1 Diabetes (CLOuD) | 10–18 years | Free living | NCT02871089 | FlorenceM closed-loop system | 2-year RCT of HCL vs. usual care (injection therapy) |
| Adolescence and Diabetes: Can an Automated Closed Loop System Improve Control? (SPIDIMAN2) | 12–18 years | Free living | NCT03300934 | FD2 closed-loop system | 28-day two-period crossover study of HCL vs. pump therapy |
| Fuzzy Logic Automated Insulin Regulation (FLAIR) | 14–30 years | Free living | NCT03040414 | Medtronic 670G vs. advanced HCL system (PID + Fuzzy Logic) | 3-month RCT with crossover between the two study conditions |
| Closed-loop Control of Glucose Levels (Artificial Pancreas) for 15 Weeks in Adolescents and Adults With Type 1 Diabetes | ≥12 years | Free living | NCT02846857 | Dual-hormone vs. single-hormone closed-loop system | 15-week RCT of SAP vs. single-hormone closed-loop vs. dual-hormone closed-loop |
| Multi-center Trial in Adult and Pediatric Patients With Type 1 Diabetes Using Hybrid Closed Loop System at Home | 2–80 years | Free living | NCT02748018 | Medtronic 670G | 6-month RCT of HCL vs. usual care followed by 6-month continuation phase |
| Day and Night Closed-loop in Young People With Type 1 Diabetes (DAN05) | 6–18 years | Free living | NCT02925299 | FlorenceM | 6-month RCT of HCL vs. usual care |
| The International Diabetes Closed Loop (iDCL) Trial: Protocol 1 | ≥14 years | Free living | NCT02985866 | Artificial Pancreas with inControl Diabetes Management Platform | 3-month RCT of HCL vs. SAP therapy |
| Safety and Efficacy of Artificial Pancreas With and Without a Meal Detection Module on Glycemic Control in Adolescents With Type 1 Diabetes After a Missed Bolus | 12–18 years | Inpatient | NCT02909829 | Closed-loop insulin delivery with a meal-detection mode | 9 h of HCL on three visits |
| International Diabetes Closed Loop (iDCL) Trial: Research Site Training Protocol | 14–74 years | Free living | NCT02844517 | inControl Diabetes Management Platform | 2 weeks of HCL use |
| Clinical Startup of the 670G Closed Loop Insulin Delivery System (670Gstartup) | ≥7 years | Free living | NCT03017482 | Medtronic 670G | Observational up to 1 year post–HCL initiation |
| Home Testing of Day and Night Closed Loop With Pump Suspend Feature (APCam11) | ≥6 years | Free living | NCT02523131 | FlorenceM | 3-month RCT of HCL vs. pump suspend feature vs. insulin pump therapy |
| Insulet Artificial Pancreas Free-Living IDE3 | 2–65 years | Transitional | NCT03216460 | Insulet automated glucose control system | 5-day/4-night HCL |
PID, proportional integral derivative; RCT, randomized controlled trial; SAP, sensor-augmented pump.
*Defined as inpatient, research unit–based, transitional environment in hotels and camps, or free-living outpatient studies.
Performance of the 670G System: Insights From Clinical Practice Data
Ensuring these systems perform well in rigorous clinical trials is essential; yet, the true test of these devices is how they work once integrated into clinical practice. With over 15,000 users identified through CareLink data uploads from 17 March 2017 through 31 December 2017, the effectiveness of this technology could be explored (31). An 8.5% increase in time in target range, defined as 70–180 mg/dL (3.9–10.0 mmol/L) (P < 0.001) was observed after switching from open-loop mode to HCL insulin delivery with the 670G, primarily due to a reduction in time spent >180 mg/dL (10 mmol/L) (31). When the data are further parsed based on time of day, the rise in time in target range is 11% for the overnight period (10 p.m.–7 a.m.) and 15% for the early morning hours (3 a.m.–6 a.m.). It is also very revealing that patients in clinical practice used HCL insulin delivery 80% of the time, thus endorsing their desire to have their glucose sensors automatically drive the 670G pump the vast majority of time (31).
New Features to Promote HCL Use in Pediatrics
To have these devices used by as many youth with T1D as possible, it will be important for manufacturers to incorporate the desires of patients and their families in the next generation of systems. Families have grown accustomed to remote monitoring of CGM data; many will seek closed-loop insulin delivery systems that afford this option (32). Parents of infants and toddlers value insulin pump systems that have incorporated remote bolusing features, and similar functions should be incorporated in HCL systems. While limited access to various system features may be desired for youngsters, as children mature and display greater understanding of their own condition, the use of passcodes or variable access categories may allow the system to “grow” with them (32). Other focus groups have expressed the desire for these devices to be more discreet (33).
In young children being treated with low total daily doses of insulin, use of diluted insulin may improve glycemic control and variability. Elleri et al. (34) reported that use of diluted insulin during overnight closed-loop control in 3- to 6-year-olds reduced rates of hypoglycemia and tended toward reduced glycemic variability as compared with standard insulin strength. Additionally, analysis of the data from that study demonstrated reduced interindividual variability in time to peak insulin action with diluted insulin (35). The reduced interindividual variability could be attributed to a reduction of mechanical delivery errors and more consistent absorption due to the larger volume of the subcutaneous deposit (35). Hvorka and colleagues are conducting an open-label, randomized crossover assessment of diluted insulin as compared with commercially available insulin preparations in children aged 1–7 years (NCT03101865).
In the midst of the era of personalized medicine, allowing for customization of these systems will also assist with their adoption. While the first commercially available closed-loop system alters basal insulin delivery to achieve a prefixed target of 120 mg/dL (6.7 mmol/L), with correction boluses targeting a glucose of 150 mg/dL (8.3 mmol/L), systems currently in development provide the option to alter this parameter. For pediatric patients, having alerts that are customizable is critical; for some, distinct auditory tones are desired, while others want to make sure alarms are discreet. As alerts may be missed overnight while asleep, determining strategies to amplify alerts or send the signal to other devices may improve reaction to system alarms. Simplifying meal announcement strategies will also reduce burden; some systems in development have adopted the approach of meal size rather than discrete carbohydrate content entry to address this. Finally, strategies to help manage glucose during exercise will be critical, as physical activity is a cornerstone of care. While closed-loop insulin delivery has been shown to reduce overnight hypoglycemia (36), automated insulin delivery without an exercise adaptation is not sufficient to mitigate hypoglycemia during physical activity. The first commercially available HCL system has a temporary target that increases the system set point from 120 mg/dL (6.7 mmol/L) to 150 mg/dL (8.3 mmol/L) in half-hour increments to a maximum duration of 12 h, and it is recommended that patients initialize this higher target 1–2 h prior to commencing exercise. Yet, some may find that this does not suffice to prevent hypoglycemia, and spontaneous exercise may make alteration of insulin delivery less feasible. Consensus guidelines to assist with glucose management in those with T1D have been developed based on starting glycemia and type of exercise (37), and feasibility studies have shown that consumption of supplemental carbohydrates during HCL insulin delivery may help mitigate hypoglycemia that may occur during physical activity (38). Various strategies to announce exercise are being explored for future iterations of HCL systems and will be fundamental to providing our youth the ability to participate fully in sports programs.
While first-generation systems will require a hybrid approach and meal announcement, it is anticipated that future generations of closed-loop artificial pancreas systems will be able to automatically deliver the full amount of insulin required for carbohydrate intake. Dual-hormone systems are also being explored, whether it be through the addition of glucagon in hopes of more closely approximating normal physiological function by infusing glucagon when sensor glucose levels trend low or through the addition of other adjunctive therapies, such as pramlintide or liraglutide (26,39,40).
Conclusions
The approval of the first HCL device for T1D has opened the door for other systems that are potentially beneficial for youth of all ages, and ensuring that our youth are not left behind in this technological revolution will be critical. It is essential to recognize the unique factors that must be considered in the development of closed-loop systems for youth while also conducting studies and seeking regulatory approval for these systems in the pediatric population. As childhood is a time of both physical and mental development, a system that can adjust insulin delivery in real time based on sensor glucose readings will more closely mimic normal physiology than what can be achieved with quarterly health care visits. Furthermore, as described by participants in HCL studies, waking with fasting glucose levels close to target range may allow for better sleep and an improved start to the day (20), a finding that has been corroborated by youth and their parents (19). As Sir William Osler said, “The good physician treats the disease, the great physician treats the patient who has the disease.” When caring for our youth with T1D, it is critical to remember first and foremost that our patients are kids. Closed-loop insulin delivery holds the promise to improve glycemic control while reducing the burden of this chronic medical condition, allowing pediatric patients with T1D to just be kids.
Article Information
Acknowledgments. For his continued mentorship, support, guidance, and critical editorial skills, the author would like to thank Dr. William Tamborlane (Department of Pediatrics, Yale School of Medicine) for his assistance on this manuscript and in her career development. Additionally, for their review of the manuscript and comments, the author is grateful to both Dr. Michelle Van Name and Dr. Alfonso Galderisi (Department of Pediatrics, Yale School of Medicine). The author thanks the participants and their families as well as the health care professionals and staff at all of the research centers who take part in studies of closed-loop insulin delivery in youth. Furthermore, she is appreciative to all the academic centers, industry partners, and regulators who have been involved in the development and approval of diabetes technologies. Additionally, the author thanks the Yale Children’s Diabetes Clinic, the Hospital Research Unit, which is part of the Yale Center for Clinical Investigation, and the dedicated nursing staff of the Hospital Research Unit, whose support has allowed the staff to be involved in closed-loop therapy from its inception.
Funding. This publication was made possible through the support of grants from JDRF (5-ECR-2014-112-A-N) and the National Institutes of Health (UL1-TR-000142, P30-DK-45735).
Duality of Interest. J.L.S is a consultant for Medtronic Diabetes and is on the medical advisory board for Bigfoot Biomedical, Eli Lilly, and Insulet. No other potential conflicts of interest relevant to this article were reported.
Prior Presentation. Parts of this article were presented at the 78th Scientific Sessions of the American Diabetes Association, Orlando, FL, 23 June 2018.
Footnotes
References
- 1.Miller KM, Foster NC, Beck RW, et al.; T1D Exchange Clinic Network . Current state of type 1 diabetes treatment in the U.S.: updated data from the T1D Exchange clinic registry. Diabetes Care 2015;38:971–978 [DOI] [PubMed] [Google Scholar]
- 2.Sullivan-Bolyai S, Deatrick J, Gruppuso P, Tamborlane W, Grey M. Constant vigilance: mothers’ work parenting young children with type 1 diabetes. J Pediatr Nurs 2003;18:21–29 [DOI] [PubMed] [Google Scholar]
- 3.Sundberg F, Forsander G. Detection and treatment efficacy of hypoglycemic events in the everyday life of children younger than 7 yr. Pediatr Diabetes 2014;15:34–40 [DOI] [PubMed] [Google Scholar]
- 4.Peters A, Van Name MA, Thorsted BL, Piltoft JS, Tamborlane WV. Postprandial dosing of bolus insulin in patients with type 1 diabetes: a cross-sectional study using data from the T1D Exchange Registry. Endocr Pract 2017;23:1201–1209 [DOI] [PubMed] [Google Scholar]
- 5.Jaser SS, Lord JH, Simmons JH, Malow BA. Brief report: sleep disturbances in young children with type 1 diabetes. Diabetes Res Clin Pract 2016;120:232–234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Van Name MA, Hilliard ME, Boyle CT, et al. . Nighttime is the worst time: parental fear of hypoglycemia in young children with type 1 diabetes. Pediatr Diabetes 2018;19:114–120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Driscoll KA, Volkening LK, Haro H, et al. . Are children with type 1 diabetes safe at school? Examining parent perceptions. Pediatr Diabetes 2014;16:613–620 [DOI] [PubMed] [Google Scholar]
- 8.Patton SR, Dolan LM, Henry R, Powers SW. Parental fear of hypoglycemia: young children treated with continuous subcutaneous insulin infusion. Pediatr Diabetes 2007;8:362–368 [DOI] [PubMed] [Google Scholar]
- 9.Van Name MA, Miller KM, Commissariat PV, et al. CGM increases parental comfort with lower glucose levels in young children with type 1 diabetes (T1D). Abstract presented at the 10th International Meeting of Pediatric Endocrinology, 14–17 September 2017, Washington, DC [Google Scholar]
- 10.Caprio S, Plewe G, Diamond MP, et al. . Increased insulin secretion in puberty: a compensatory response to reductions in insulin sensitivity. J Pediatr 1989;114:963–967 [DOI] [PubMed] [Google Scholar]
- 11.Laffel LM, Vangsness L, Connell A, Goebel-Fabbri A, Butler D, Anderson BJ. Impact of ambulatory, family-focused teamwork intervention on glycemic control in youth with type 1 diabetes. J Pediatr 2003;142:409–416 [DOI] [PubMed] [Google Scholar]
- 12.Karges B, Schwandt A, Heidtmann B, et al. . Association of insulin pump therapy vs insulin injection therapy with severe hypoglycemia, ketoacidosis, and glycemic control among children, adolescents, and young adults with type 1 diabetes. JAMA 2017;318:1358–1366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sherr JL, Hermann JM, Campbell F, et al.; T1D Exchange Clinic Network, the DPV Initiative, and the National Paediatric Diabetes Audit and the Royal College of Paediatrics and Child Health registries . Use of insulin pump therapy in children and adolescents with type 1 diabetes and its impact on metabolic control: comparison of results from three large, transatlantic paediatric registries. Diabetologia 2016;59:87–91 [DOI] [PubMed] [Google Scholar]
- 14.Tamborlane WV, Beck RW, Bode BW, et al.; Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group . Continuous glucose monitoring and intensive treatment of type 1 diabetes. N Engl J Med 2008;359:1464–1476 [DOI] [PubMed] [Google Scholar]
- 15.DeSalvo D, Miller K, Hermann J, et al. Continuous glucose monitoring (CGM) and glycemic control among youth with type 1 diabetes (T1D): international comparison from the T1D Exchange (T1DX) and the DPV initiative. Abstract presented at the 43rd Annual Conference of the International Society for Pediatric and Adolescent Diabetes, 18–21 October 2017, Innsbruck, Austria [Google Scholar]
- 16.Weinzimer SA, Steil GM, Swan KL, Dziura J, Kurtz N, Tamborlane WV. Fully automated closed-loop insulin delivery versus semiautomated hybrid control in pediatric patients with type 1 diabetes using an artificial pancreas. Diabetes Care 2008;31:934–939 [DOI] [PubMed] [Google Scholar]
- 17.Barnard KD, Wysocki T, Allen JM, et al. . Closing the loop overnight at home setting: psychosocial impact for adolescents with type 1 diabetes and their parents. BMJ Open Diabetes Res Care 2014;2:e000025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barnard KD, Wysocki T, Thabit H, et al.; Angela Consortium . Psychosocial aspects of closed- and open-loop insulin delivery: closing the loop in adults with type 1 diabetes in the home setting. Diabet Med 2015;32:601–608 [DOI] [PubMed] [Google Scholar]
- 19.Barnard KD, Wysocki T, Ully V, et al. . Closing the loop in adults, children and adolescents with suboptimally controlled type 1 diabetes under free living conditions: a psychosocial substudy. J Diabetes Sci Technol 2017;11:1080–1088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kovatchev B, Cheng P, Anderson SM, et al. . Feasibility of long-term closed-loop control: a multicenter 6-month trial of 24/7 automated insulin delivery. Diabetes Technol Ther 2017;19:18–24 [DOI] [PubMed] [Google Scholar]
- 21.Phillip M, Battelino T, Atlas E, et al. . Nocturnal glucose control with an artificial pancreas at a diabetes camp. N Engl J Med 2013;368:824–833 [DOI] [PubMed] [Google Scholar]
- 22.Ly TT, Breton MD, Keith-Hynes P, et al. . Overnight glucose control with an automated, unified safety system in children and adolescents with type 1 diabetes at diabetes camp. Diabetes Care 2014;37:2310–2316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ly TT, Roy A, Grosman B, et al. . Day and night closed-loop control using the integrated Medtronic hybrid closed-loop system in type 1 diabetes at diabetes camp. Diabetes Care 2015;38:1205–1211 [DOI] [PubMed] [Google Scholar]
- 24.Ly TT, Buckingham BA, DeSalvo DJ, et al. . Day-and-night closed-loop control using the unified safety system in adolescents with type 1 diabetes at camp. Diabetes Care 2016;39:e106–e107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ly TT, Keenan DB, Roy A, et al. . Automated overnight closed-loop control using a proportional-integral-derivative algorithm with insulin feedback in children and adolescents with type 1 diabetes at diabetes camp. Diabetes Technol Ther 2016;18:377–384 [DOI] [PubMed] [Google Scholar]
- 26.Russell SJ, Hillard MA, Balliro C, et al. . Day and night glycaemic control with a bionic pancreas versus conventional insulin pump therapy in preadolescent children with type 1 diabetes: a randomised crossover trial. Lancet Diabetes Endocrinol 2016;4:233–243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Del Favero S, Boscari F, Messori M, et al. . Randomized summer camp crossover trial in 5- to 9-year-old children: outpatient wearable artificial pancreas is feasible and safe. Diabetes Care 2016;39:1180–1185 [DOI] [PubMed] [Google Scholar]
- 28.Bergenstal RM, Garg S, Weinzimer SA, et al. . Safety of a hybrid closed-loop insulin delivery system in patients with type 1 diabetes. JAMA 2016;316:1407–1408 [DOI] [PubMed] [Google Scholar]
- 29.Garg SK, Weinzimer SA, Tamborlane WV, et al. . Glucose outcomes with the in-home use of a hybrid closed-loop insulin delivery system in adolescents and adults with type 1 diabetes. Diabetes Technol Ther 2017;19:155–163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Buckingham B, Shulman D, Forlenza G, et al. Glycemic outcomes during MiniMed 670G system use in children with T1D (Abstract). Diabetes Technol Ther 2018;20(Suppl. 1):A19 [Google Scholar]
- 31.Agrawal P, Stone M, Cordero T, Lee S, Shin J, Kaufman F. Real-world use of the MiniMed 670G hybrid closed-loop system (Abstract). Diabetes Technol Ther 2018;20(Suppl. 1):A18–A19 [Google Scholar]
- 32.Gildersleeve R, Riggs SL, Cherñavvsky DR, Breton MD, DeBoer MD. Improving the safety and functionality of an artificial pancreas system for use in younger children: input from parents and physicians. Diabetes Technol Ther 2017;19:660–674 [DOI] [PubMed] [Google Scholar]
- 33.Naranjo D, Suttiratana SC, Iturralde E, et al. . What end users and stakeholders want from automated insulin delivery systems. Diabetes Care 2017;40:1453–1461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Elleri D, Allen JM, Tauschmann M, et al. . Feasibility of overnight closed-loop therapy in young children with type 1 diabetes aged 3-6 years: comparison between diluted and standard insulin strength. BMJ Open Diabetes Res Care 2014;2:e000040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ruan Y, Elleri D, Allen JM, et al. . Pharmacokinetics of diluted (U20) insulin aspart compared with standard (U100) in children aged 3-6 years with type 1 diabetes during closed-loop insulin delivery: a randomised clinical trial. Diabetologia 2015;58:687–690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sherr JL, Cengiz E, Palerm CC, et al. . Reduced hypoglycemia and increased time in target using closed-loop insulin delivery during nights with or without antecedent afternoon exercise in type 1 diabetes. Diabetes Care 2013;36:2909–2914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Riddell MC, Gallen IW, Smart CE, et al. . Exercise management in type 1 diabetes: a consensus statement. Lancet Diabetes Endocrinol 2017;5:377–390 [DOI] [PubMed] [Google Scholar]
- 38.Patel NS, Van Name MA, Cengiz E, et al. . Mitigating reductions in glucose during exercise on closed-loop insulin delivery: the Ex-Snacks study. Diabetes Technol Ther 2016;18:794–799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Weinzimer SA, Sherr JL, Cengiz E, et al. . Effect of pramlintide on prandial glycemic excursions during closed-loop control in adolescents and young adults with type 1 diabetes. Diabetes Care 2012;35:1994–1999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sherr JL, Patel NS, Michaud CI, et al. . Mitigating meal-related glycemic excursions in an insulin-sparing manner during closed-loop insulin delivery: the beneficial effects of adjunctive pramlintide and liraglutide. Diabetes Care 2016;39:1127–1134 [DOI] [PMC free article] [PubMed] [Google Scholar]