Abstract
Evidence has suggested that dysregulation of the dopaminergic system may play a significant role in the pathogenesis of attention-deficit/hyperactivity disorder (ADHD) in children. Manganese, a neurotoxicant, has been reported to exert its neurotoxicity by affecting the dopaminergic system. However, the association between peripheral manganese levels and ADHD has not been comprehensively reviewed. This study aimed to investigate the association between peripheral manganese levels and ADHD in children. An electronic search was performed on databases including PubMed, ProQuest, ClinicalKey, Cochrane Library, ClinicalTrials.gov, Embase, Web of Science, and ScienceDirect with last search on March 25th, 2018. As per the inclusion criteria, human observational studies investigating peripheral manganese levels in children with ADHD and controls were included. The meta-analysis was performed using a random-effects model, and possible confounders were examined by subgroup analysis. In total, four articles with 175 ADHD children and 999 controls were recruited. The manganese levels were significantly higher in ADHD children than in controls (p=0.033), when studies investigating blood levels and those investigating hair levels were included. However, when only studies investigating blood levels were included, there was no significant difference between ADHD children and controls (p=0.076). Our results support higher peripheral manganese levels in children diagnosed with ADHD than those in controls. Further primary studies are needed to clarify this association.
Keywords: meta-analysis, manganese, ADHD, pediatric psychiatry, review
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is defined as “a persistent pattern of inattention and/or hyperactivity-impulsivity that interferes with functioning or development”.1 ADHD can be categorized into three subtypes: predominantly inattentive, predominantly hyperactive-impulsive, and combined.2 The prevalence of ADHD is estimated to be 5.29% in children worldwide.3 Inattention refers to wandering off task, lacking persistence, having difficulty sustaining focus, and being disorganized and is not due to defiance or lack of comprehension. Impulsivity refers to excessive motor activity when it is not appropriate, or excessive fidgeting, tapping, or talkativeness.1 Further, it may cause impairments in social communication and functional limitations of effective communication, social participation, or academic achievement.1
Although the exact pathogenesis of ADHD remains unknown, it has been found that people with ADHD have smaller brain volumes of specific structures, such as the prefrontal cortex and basal ganglia,2 or have higher exposure to environmental pollution, such as lead4 or polybrominated diphenyl ethers.5 One of the most widely postulated pathogeneses of ADHD is the “dopamine hypothesis”,2 attributing ADHD to a dysregulation of the dopaminergic system. A review article has shown that ADHD patients have decreased availability of dopamine receptor isoforms and increased dopamine transporter (DAT) binding compared with controls.6 The most widely used medication for ADHD, methylphenidate with its derivatives, is postulated to have its effects by blocking DAT and promoting dopamine release.6
In previous studies, manganese (elemental symbol: Mn), an environmental heavy metal element, has been found to cause neurologic toxicity to humans.7,8 It can be present in contaminated water, pesticides, batteries, and glass, among others, and then be ingested by humans.9–11 High concentration of manganese has been found in the basal ganglia of manganese-intoxicated rats.12 After exposure to manganese, decreased long-term dopamine efflux in rats13 and attenuated dopaminergic neurotransmission in humans14 have also been reported. In epidemiological studies, higher levels of manganese in the hair and blood samples from children with ADHD have been found.15,16 Another study has shown decreased intelligence quotient (IQ) in children with increased hair concentration of manganese.17 There have been no studies investigating the postmortem levels of in vivo manganese in ADHD patients found in the literature, by using the same search strategy as the current meta-analysis.
Therefore, as a neurotoxin affecting dopaminergic neurotransmission, manganese may play a role in the pathogenesis of ADHD in those exposed to the metal. Among the four datasets in the literature studying “blood” manganese levels, two16,18 showed a significantly positive association between blood manganese level and ADHD, while the other two18,19 revealed insignificant results. Three of the four datasets used case–control design, while the other dataset used cross-sectional design. Another case–control study showed a trend of positive association between “hair” manganese level and ADHD without statistical significance.20 Difference in study design (case–control vs cross-sectional), source of manganese level (ie, blood vs hair), and population (described in the “Discussion” section) may contribute to the heterogeneity of the study results. Although there are two previous meta-analyses17,21 mentioning the possible relationship between manganese exposure and ADHD in children, they did not directly calculate the association. Therefore, the aim of the current study is to summarize the literature for the possible association between peripheral manganese levels and ADHD in children via a thorough meta-analysis.
Methods
We followed the Meta-analysis Of Observational Studies in Epidemiology (MOOSE) guidelines22 (Figure S1). This preliminary meta-analysis followed an a priori defined but unpublished protocol. The Institutional Review Board of the Tri-Service General Hospital (TSGHIRB: B-105-12) approved the study.
Eligibility criteria
Inclusion criteria were the following: (a) observational studies, including a cohort or cross-sectional study design comparing peripheral levels of manganese in children with ADHD and controls; and (b) trials in humans. We excluded preclinical studies, review articles, meeting abstracts, and non-human studies; furthermore, to increase the specificity of the effect of manganese on ADHD, we excluded those studies that collected manganese sample sources further away from the diagnosis of ADHD (eg, collecting manganese when ADHD children were just delivered).
Search strategy and study selection
Two well-trained authors (JH Shih and PT Tseng) performed a systematic literature search from inception until August 30th, 2017 and updated search at March 25th, 2018. The following keywords were used in our search on PubMed, ProQuest, ClinicalKey, Cochrane Library, ScienceDirect, and ClinicalTrials.gov platforms: “(Manganese OR Mn) AND (ADHD OR attention-deficit/hyperactivity disorder)”. A similar search was conducted in Embase and Web of Science databases. The reference lists of included articles and recent reviews were also hand-searched to identify additional articles.17,21,23–25
Two authors (JH Shih and PT Tseng) independently screened the titles and abstracts of all retrieved results for potential eligibility. Both authors reviewed the full text of potentially eligible papers, and a final list of included studies was achieved. Any inconsistencies were resolved through discussion with a third reviewer (MK Wu).
Data extraction
The primary outcomes were the difference in manganese levels in children with ADHD compared to control groups (calculated as Hedges’ g statistic and corresponding 95% CIs and p-values). We did not choose difference in mean as the effect sizes (ESs) of our primary outcome due to presumed different units used in each study. The control groups were defined as those without ADHD. In addition, due to potential confounding effect of specific medication (eg, methylphenidate) on manganese,18 we did not include the data of manganese level in children with ADHD who had been clearly described as receiving such medication. If data were available, we prefer to choose control groups as healthy (asymptomatic) individuals. When data were not available from the included studies, we contacted the primary authors to request the original data. We contacted the authors via email on two occasions if required (a second email was sent a week later if no response was received following an initial email). If there were no relevant data in the paper regarding manganese levels, wherever possible, we attempted to use another compatible statistical parameter (eg, p-value and sample sizes) to estimate the ESs according to the protocol in the Comprehensive Meta-Analysis manuals and guidance on the Comprehensive Meta-Analysis website (https://www.meta-analysis.com/downloads/Meta-analysis%20Converting%20among%20effect%20sizes.pdf) to covert and pool the ESs into Hedges’ g.
The variables of interest included manganese levels, mean age, gender distribution (in the form of % females), mean body mass index, cognitive performance (in the form of mean IQ), parental tobacco smoking and alcohol consumption, and the type of assay used for detection of manganese levels.
Methodological quality appraisal
We used the modified Newcastle–Ottawa Scale (NOS) to evaluate the quality of the included studies. In brief, the modified NOS was based on a version previously used in a meta-analysis study published in British Journal of Psychiatry in 2013, and score ranges from 0 to 6 (Table S1).26
Meta-analysis procedure
Given the anticipated heterogeneity in the basic population of study, we conducted the meta-analyses with a random-effects model rather than a fixed-effects one.27 As aforementioned, the primary ES was estimated as Hedges’ g with 95% CI to compare manganese levels in children with ADHD and controls. Subgroup analyses were conducted to determine whether results differed as we grouped them according to the sample sources (eg, blood, hair). We performed subgroup analyses whenever data from at least two independent data-sets were available. In addition, to overcome the limitation of the meta-analysis that we could not adjust the potential confounding effect by clinical variables, we collected the adjusted OR provided by the recruited articles to calculate the pooled adjusted OR.
Sensitivity test, heterogeneity, publication bias, and meta-regression
We performed sensitivity test with “one-study removal” test to evaluate if the results of the meta-analysis were obtained from any outliers within the recruited studies or not.28 Heterogeneity was assessed by the Cochran Q test and its corresponding p-value.29 The I2 statistic was interpreted as the proportion of heterogeneity a study estimates that is due to heterogeneity.30 We performed meta-regression analyses with unrestricted maximum likelihood random effects when data on each potential moderator were provided by at least five different studies. We assessed publication bias via the inspection of funnel plots31 and with the Egger’s regression test.32 When evidence of publication bias was found, the Duval and Tweedie’s trim-and-fill procedure, which is a validated model to estimate an ES, was employed.33 The current meta-analysis was conducted using the Comprehensive Meta-Analysis software, version 3 (BioStat, Frederick, MD, USA). The threshold for statistical significance was set at a two-tailed p-value <0.05.
Results
Study selection
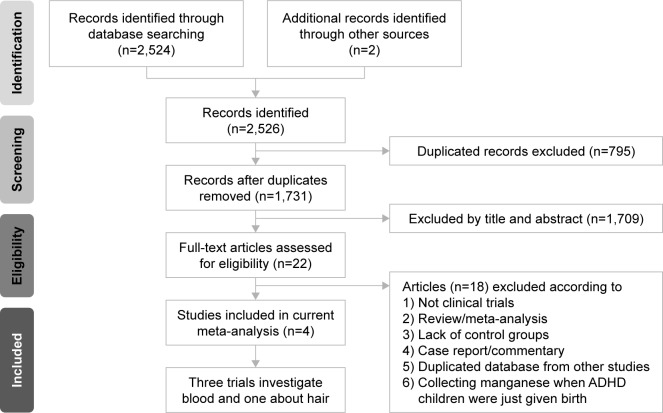
Figure 1 summarizes study selection process. In brief, a total of 22 studies entered the full-text review stage. Eighteen articles were excluded for various reasons (Figure 1). A list of excluded articles is presented in Table S2. In total, four articles met the inclusion criteria, the details of which are summarized in Table 1.16,18–20
Figure 1.
The flowchart of meta-analysis.
Abbreviation: ADHD, attention-deficit hyperactivity disorder.
Table 1.
Characteristics of the recruited studies
| Study | Criteria of ADHD | Sample source | Comparison | Subject | Mean age | Female (%) | Cognitive function
|
ADHD subtype
|
Parental history of ADHD | Country | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ADHD (IQ) | Control (IQ) | Inattentive | Hyperactive | Combined | |||||||||
| Shin et al20 | DSM-IV | Hair | ADHD | 40 | 9.4±3.0 | 15.0 | 101.8±14.9 | 112.4±10.4 | N/A | N/A | N/A | Not mentioned | Republic of Korea |
| Control | 43 | 10.3±3.1 | 16.3 | ||||||||||
| Hong et al19 | DISC-IV | Blood | ADHD | 43 | 9.1±0.8 | 16.3 | 106.1±13.8 | 111.0±14.2 | N/A | N/A | N/A | Not mentioned | Republic of Korea |
| Control | 847 | 9.1±0.7 | 48.5 | ||||||||||
| Yousef et al16 | DSM-IV | Blood | ADHD | 18 | 8.3±1.8 | N/A | N/A | N/A | 38.9% | 33.3% | 27.8% | Not mentioned | United Arab Emirates |
| Control | 74 | ||||||||||||
| Farias et al18 | DSM-IV | Blood | ADHD-combined | 50 | 8.0±1.2 | 14.0 | 102.0±14.0 | 101.0±17.0 | 33.0% | 0.0% | 67.0% | Not mentioned | Brazil |
| ADHD-inattentive | 24 | 9.0±1.4 | 21.0 | 93.0±10.0 | |||||||||
| ADHD-combined and Mx | 21 | 9.0±1.8 | 19.0 | 98.0±14.0 | |||||||||
| ADHD-inattentive and Mx | 11 | 10.0±1.7 | 0.0 | 97.0±10.0 | |||||||||
| Control | 35 | 9.0±1.2 | 20.0 | ||||||||||
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; DISC-IV, Diagnostic Interview Schedule for Children Version IV; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; IQ, intelligence quotient; Mx, medication; N/A, not available.
Among the included studies, four provided comparison of the peripheral manganese levels in children with ADHD and controls (children with ADHD: n=175, mean age=8.8, mean female proportion=16.0%; controls without ADHD: n=999, mean age=9.1, mean female proportion=45.9%).16,18–20 Two of them provided the data of adjusted OR for the association between manganese levels and ADHD.16,20
Characteristics and methodological quality of included studies
Among the recruited studies, the diagnosis of ADHD was made according to widely acceptable criteria, including the Diagnostic and Statistical Manual of Mental Disorders (DSM)16,18,20 or Diagnostic Interview Schedule for Children Version IV.19 In addition, the sample sources ranged from peripheral blood16,18,19 to hair sample.20 The assays used to detect manganese levels included inductively coupled plasma mass spectrometry and graphite furnace atomic absorption spectrometry (Table S1). Regarding the methodological quality of included studies, the average NOS score was 15.5 with a SD of 1.0 (Table S1).
Meta-analysis of overall differences in manganese levels in children with ADHD and controls without ADHD
Overall
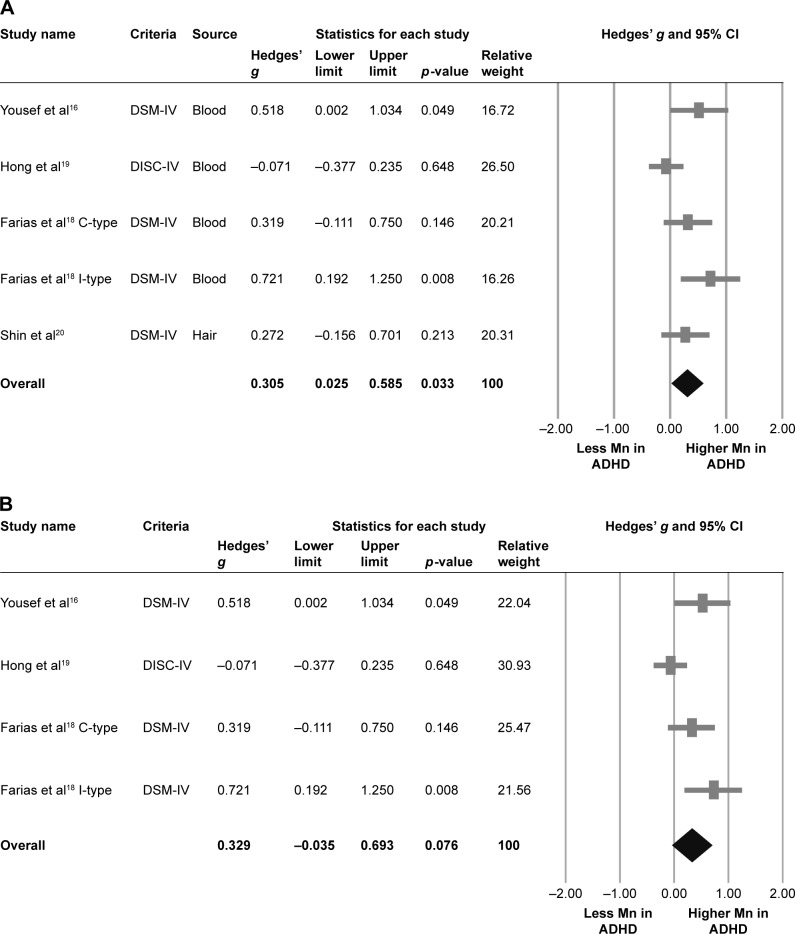
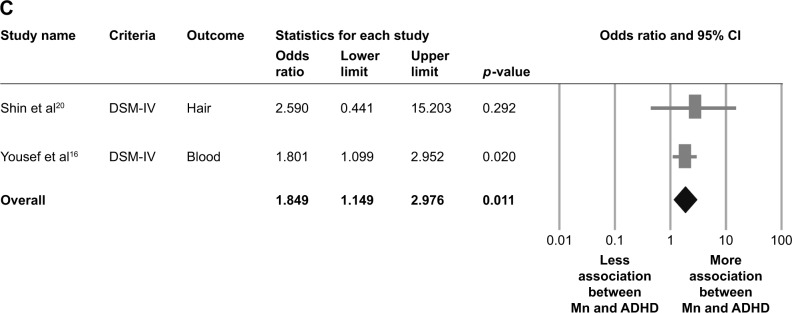
Four articles provided five datasets in this part of meta-analysis.16,18–20 The meta-analysis suggested that overall manganese levels, either in blood or in hair, in children diagnosed with ADHD were significantly higher than those in controls (k=5, Hedges’ g=0.305, 95% CI=0.025–0.585, p=0.033) (Figure 2A) without significant evidence of heterogeneity (Q value=8.419, df=4, I2=52.486%, p=0.077, tau=0.229), but significant publication bias via inspection of funnel plot and Egger’s regression was found (t=10.525, df=3, p=0.002). The significant results of the meta-analysis changed to insignificant after refilling two potential missing data to the left side of means according to Duval and Tweedie’s trim-and-fill test (Hedges’ g=0.145, 95% CI=−0.140 to 0.430).
Figure 2.
Meta-analysis of (A) overall manganese levels in ADHD children and controls, (B) blood manganese levels in ADHD children and controls, and (C) pooled adjusted OR for the association between manganese levels and ADHD.
Notes: (A) There were significantly higher overall manganese levels in ADHD children than those in controls (Hedges’ g=0.305, 95% CI=0.025–0.585, p=0.033). (B) There were no significantly different blood manganese levels in ADHD children and controls (Hedges’ g=0.329, 95% CI=−0.035 to 0.693, p=0.076). (C) There was a significant association between manganese levels and diagnosis of ADHD as shown by pooled adjusted OR (OR=1.849, 95% CI=1.149–2.976, p=0.011).
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; C-type, combined type; DISC-IV, Diagnostic Interview Schedule for Children Version IV; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; I-type, inattention type.
Sensitivity test
The significant results of the meta-analysis changed to insignificant after removing any one of the recruited studies, which might be due to smaller sample sizes after removal of one of the recruited studies. However, the significant results of the meta-analysis changed to more predominantly significant after removing the data from Hong et al (Hedges’ g=0.425, 95% CI=0.191–0.660, p<0.001).19
Meta-regression
The meta-regression could be performed only on association between ESs and mean age due to lack of data. To be specific, there was no significant association between ESs and mean age (p=0.656).
Meta-analysis of differences in manganese levels in children with ADHD and controls without ADHD in blood samples
Blood manganese
Three articles provided four datasets in this part of meta-analysis.16,18,19 The meta-analysis suggested that the blood manganese levels in children diagnosed with ADHD and controls without ADHD were not significantly different, but a trend of higher blood manganese levels in ADHD children compared to controls was observed (k=4, Hedges’ g=0.329, 95% CI=−0.035 to 0.693, p=0.076) (Figure 2B) with significant evidence of heterogeneity (Q value=8.394, df=3, I2=64.260%, p=0.039, tau=0.295) and significant publication bias via inspection of funnel plot and Egger’s regression (t=9.335, df=2, p=0.011). However, the results of the meta-analysis did not change after refilling according to Duval and Tweedie’s trim-and-fill test.
Sensitivity test
The insignificant results of the meta-analysis changed to significant after removing the data from Hong et al (Hedges’ g=0.491, 95% CI=0.210–0.771, p=0.001).
Meta-regression
All the meta-regression procedures were not performed because there were less than five datasets.
Meta-analysis of differences in manganese levels in children with ADHD and controls without ADHD in hair samples
Hair manganese
Only one article provided one dataset in this part of meta-analysis.20 Therefore, the meta-analysis was not done due to lack of enough datasets. However, in the research results according to the description in the article by Shin et al,20 the authors indicated that the proportion of abnormal manganese levels, either higher or lower, in children with ADHD was significantly higher than those in controls (p=0.039).
Meta-analysis of overall adjusted OR for the association between manganese levels and diagnosis of ADHD
Two articles provided two datasets in this part of meta-analysis.16,20 The meta-analysis of the adjusted ORs indicated significant association between manganese levels and the diagnosis of ADHD (k=2, adjusted OR=1.849, 95% CI=1.149–2.976, p=0.011) (Figure 2C) without significant evidence of heterogeneity (Q value=0.150, df=1, I2<0.001%, p=0.698, tau<0.001).
Discussion
To the best of our knowledge, this is the first meta-analysis to investigate the relationship between peripheral manganese levels and ADHD in children. The results of the current meta-analysis showed significantly higher overall (ie, in blood or hair) peripheral manganese levels in children diagnosed with ADHD than those in controls, with no significant heterogeneity. Among the four included studies with five datasets in total, our results are consistent with two datasets,16,18 but not with the other three.18–20 However, among the three studies mentioned,18–20 two18,20 also showed a trend of positive association (p=0.146 and 0.213, respectively), though not significant, which may be due to small number of cases. Sensitivity test showed that the results became insignificant after removing any one of the included studies, which may also be due to small number of cases. Subgroup analysis showed a trend of higher “blood” manganese levels in ADHD children than in controls, though not significant (p=0.076). However, the results changed to significant after removing the data from Hong et al.19 The change from insignificance to significance may have been due to the difference in the study designs. Among the four studies included in the current meta-analysis, the study by Hong et al19 used cross-sectional design, while the other three studies16,18,20 used case–control design. Moreover, the study by Hong et al19 used Diagnostic Interview Schedule for Children Version IV, while the other studies used DSM criteria.16,18,20
Although the meta-analysis was not done in the “hair” subgroup due to the availability of only one dataset, the result of this article showed that the hair manganese levels were significantly higher in ADHD children than in controls. To overcome the potential confounding effects, we performed a meta-analysis of overall adjusted ORs, which revealed a significantly positive association (adjusted OR=1.849, p=0.011) between manganese levels and ADHD in children, with no significant heterogeneity.
A comparison of the two previous meta-analyses17,21 mentioning the association between manganese and ADHD and the current study is summarized in Table 2. In the two studies, the one by Rodríguez-Barranco et al17 calculated only the association between manganese exposure and IQ, and the other by Scassellati et al21 did not perform a meta-analysis for manganese exposure.
Table 2.
Comparison of previous and current meta-analyses
| Study | Study designs included | Manganese exposure measure | Observed effect |
|---|---|---|---|
| Scassellati et al21 | Case–control | N/A | N/A |
| Rodríguez-Barranco et al17 | Case–control, cohort, cross-sectional | Blood, cord blood, hair, placenta, tooth, water | Full-scale IQ, performance IQ, verbal IQ |
| Current study | Case–control, cross-sectional | Blood, hair | ADHD |
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; IQ, intelligence quotient; N/A, not available.
Since “dopamine hypothesis”2 is currently the most widely postulated etiologic scheme for ADHD, disrupted dopamine neurotransmission caused by manganese exposure found in several previous studies13,14 has prompted us to perform this study. Our study results also support the positive association between peripheral manganese levels and ADHD. Although there have been no studies investigating the effect of removing excessive manganese from children with ADHD, the results of our current study suggest that this treatment approach may be promising.
Because manganese levels in children (biological monitoring) are affected by environmental manganese levels, such as in soil, water, and food, it would be difficult to thoroughly investigate. Therefore, we chose blood and hair levels as an indicator of internal dose.
The current study has several limitations. First, although our main results showed higher manganese levels in children diagnosed with ADHD than those in controls, significant publication bias and heterogeneity were found. Further, the results changed to insignificant after refilling two potential missing data by using Duval and Tweedie’s trim-and-fill test (Hedges’ g=0.145, 95% CI=−0.140 to 0.430). The publication bias may be overcome when more primary researches are published. The heterogeneity might be due to the difference in study designs. Among the four included studies, the study by Hong et al19 used cross-sectional design, while the other three studies16,18,20 used matched case–control design. Another source of heterogeneity may have come from the fact that Farias et al18 had two datasets of different diagnostic criteria, which were ADHD-combined type (C-type) and ADHD-inattentive type (I-type), respectively. Further, the four included studies investigated different populations: in terms of countries, for example, their subjects were from United Arab Emirates,16 Brazil,18 and Republic of Korea.19,20 Second, due to the small number of eligible studies, we had to combine the results from blood and hair samples, which could be a source of bias. Third, there were only two datasets provided with adjusted ORs, so the potential confounding factors may not have been addressed well enough. Fourth, due to difficulties in experimental designing and ethical concerns, few studies34,35 provided central nervous system (CNS) concentrations of manganese, and none of them studied the relations between CNS manganese concentrations and ADHD. Although CNS concentrations are likely to provide more accurate information for manganese neurotoxicity, only blood or hair concentrations were available for this meta-analysis. Fifth, although eligible articles studied manganese levels in blood and hair, there have been no well-validated biomarkers for manganese exposure in children.36 Moreover, hair samples are susceptible to exogenous contamination.36 Sixth, although we provided evidences of higher manganese levels in ADHD children than in controls, we could not provide further detailed information about “to what extent” the manganese levels were higher than controls. Because the peripheral samples of manganese and method of detection in each included study were different from the others, we could not directly count and pool the difference in mean manganese levels between ADHD children and controls in each study. Seventh, although two of the studies provided information about ADHD subtype,16,18 there was still limited information about the correlation between peripheral manganese levels and ADHD subtype. Therefore, we could not derive further evidence about the correlation between peripheral manganese levels and ADHD subtype. Finally, because there had been limited articles included in the current meta-analysis, the subjects distribution was as restricted as only from three countries, including United Arab Emirates,16 Brazil,18 and Republic of Korea.19,20 Therefore, when clinicians apply our results into clinical practice, they should pay more attention about the applicability due to limited number of countries included and regional bias.
Conclusion
The results of this meta-analysis support higher peripheral manganese levels in children diagnosed with ADHD than those in controls. Further studies are warranted to replicate these findings, especially in other countries and in different ADHD subtypes, and to quantify the degree of the association for it to be useful in clinical settings.
Supplementary materials
Whole flowchart of the meta-analysis.
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; N/A, not available.
Table S1.
Results of Newcastle–Ottawa Scale scores of recruited studies
| Study | Criteria | Source | Sample method | Newcastle–Ottawa Scale
|
Country | ||||
|---|---|---|---|---|---|---|---|---|---|
| Selection | Performance | Detection | Information | Total | |||||
| Shin et al1 | DSM-IV | Hair | Inductively coupled plasma mass spectrometry | 1 | 5 | 4 | 5 | 15 | Republic of Korea |
| Hong et al2 | DISC-IV | Blood | Graphite furnace atomic absorption spectrometry | 3 | 5 | 5 | 4 | 17 | Republic of Korea |
| Yousef et al3 | DSM-IV | Blood | N/A | 2 | 5 | 4 | 4 | 15 | United Arab Emirates |
| Farias et al4 | DSM-IV | Blood | Graphite furnace atomic absorption spectrometry | 2 | 5 | 4 | 4 | 15 | Brazil |
Abbreviations: DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; DISC-IV, Diagnostic Interview Schedule for Children Version IV; N/A, not available.
Table S2.
Excluded studies and reasons
| Not related to manganese and ADHD (n=4) |
| Konstantopoulos et al5 |
| Hu et al6 |
| Konrad et al7 |
| Han et al8 |
| Meta-analysis (n=2) |
| Rodríguez-Barranco et al9 |
| Scassellati et al10 |
| Review articles (n=3) |
| Zeng et al11 |
| Grandjean and Landrigan12 |
| Lucchini et al13 |
| Not definite diagnosis of ADHD (n=5) |
| Hong et al14 |
| Bouchard et al15 |
| Lucchini et al16 |
| Chan et al17 |
| Ericson et al18 |
| Compare treatment effect of micronutrient but not related to manganese and ADHD (n=1) |
| Rucklidge et al19 |
| Use the same data sample sources of Hong et al2 (n=1) |
| Bhang et al20 |
| Lack of control (n=1) |
| Liu et al21 |
| Collecting manganese when ADHD children were just given birth (n=1) |
| Ode A et al22 |
Abbreviation: ADHD, attention-deficit/hyperactivity disorder.
References
- 1.Shin DW, Kim EJ, Lim SW, Shin YC, Oh KS, Kim EJ. Association of hair manganese level with symptoms in attention-deficit/hyperactivity disorder. Psychiatry Investig. 2015;12(1):66–72. doi: 10.4306/pi.2015.12.1.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hong SB, Kim JW, Choi BS, et al. Blood manganese levels in relation to comorbid behavioral and emotional problems in children with attention-deficit/hyperactivity disorder. Psychiatry Res. 2014;220(1–2):418–425. doi: 10.1016/j.psychres.2014.05.049. [DOI] [PubMed] [Google Scholar]
- 3.Yousef S, Adem A, Zoubeidi T, Kosanovic M, Mabrouk AA, Eapen V. Attention deficit hyperactivity disorder and environmental toxic metal exposure in the United Arab Emirates. J Trop Pediatr. 2011;57(6):457–460. doi: 10.1093/tropej/fmq121. [DOI] [PubMed] [Google Scholar]
- 4.Farias AC, Cunha A, Benko CR, et al. Manganese in children with attention-deficit/hyperactivity disorder: relationship with methylphenidate exposure. J Child Adolesc Psychopharmacol. 2010;20(2):113–118. doi: 10.1089/cap.2009.0073. [DOI] [PubMed] [Google Scholar]
- 5.Konstantopoulos K, Vogazianos P, Thodi C, Nikopoulou-Smyrni P. A normative study of the Children’s Color Trails Test (CCTT) in the Cypriot population. Child Neuropsychol. 2015;21(6):751–758. doi: 10.1080/09297049.2014.924491. [DOI] [PubMed] [Google Scholar]
- 6.Hu D, Wang YX, Chen WJ, et al. Associations of phthalates exposure with attention deficits hyperactivity disorder: a case-control study among Chinese children. Environ Pollut. 2017;229:375–385. doi: 10.1016/j.envpol.2017.05.089. [DOI] [PubMed] [Google Scholar]
- 7.Konrad K, Gauggel S, Schurek J. Catecholamine functioning in children with traumatic brain injuries and children with attention-deficit/hyperactivity disorder. Brain Res Cogn Brain Res. 2003;16(3):425–433. doi: 10.1016/s0926-6410(03)00057-0. [DOI] [PubMed] [Google Scholar]
- 8.Han JY, Kwon HJ, Ha M, et al. The effects of prenatal exposure to alcohol and environmental tobacco smoke on risk for ADHD: a large population-based study. Psychiatry Res. 2015;225(1–2):164–168. doi: 10.1016/j.psychres.2014.11.009. [DOI] [PubMed] [Google Scholar]
- 9.Rodríguez-Barranco M, Lacasaña M, Aguilar-Garduño C, et al. Association of arsenic, cadmium and manganese exposure with neurodevelopment and behavioural disorders in children: a systematic review and meta-analysis. Sci Total Environ. 2013;454–455:562–577. doi: 10.1016/j.scitotenv.2013.03.047. [DOI] [PubMed] [Google Scholar]
- 10.Scassellati C, Bonvicini C, Faraone SV, Gennarelli M. Biomarkers and attention-deficit/hyperactivity disorder: a systematic review and meta-analyses. J Am Acad Child Adolesc Psychiatry. 2012;51(10):1003–1019.e20. doi: 10.1016/j.jaac.2012.08.015. [DOI] [PubMed] [Google Scholar]
- 11.Zeng X, Xu X, Boezen HM, Huo X. Children with health impairments by heavy metals in an e-waste recycling area. Chemosphere. 2016;148:408–415. doi: 10.1016/j.chemosphere.2015.10.078. [DOI] [PubMed] [Google Scholar]
- 12.Grandjean P, Landrigan PJ. Neurobehavioural effects of developmental toxicity. Lancet Neurol. 2014;13(3):330–338. doi: 10.1016/S1474-4422(13)70278-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lucchini R, Placidi D, Cagna G, et al. Manganese and developmental neurotoxicity. Adv Neurobiol. 2017;18:13–34. doi: 10.1007/978-3-319-60189-2_2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hong SB, Im MH, Kim JW, et al. Environmental lead exposure and attention deficit/hyperactivity disorder symptom domains in a community sample of South Korean school-age children. Environ Health Perspect. 2015;123(3):271–276. doi: 10.1289/ehp.1307420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bouchard M, Laforest F, Vandelac L, Bellinger D, Mergler D. Hair manganese and hyperactive behaviors: pilot study of school-age children exposed through tap water. Environ Health Perspect. 2007;115(1):122–127. doi: 10.1289/ehp.9504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lucchini RG, Zoni S, Guazzetti S, et al. Inverse association of intellectual function with very low blood lead but not with manganese exposure in Italian adolescents. Environ Res. 2012;118:65–71. doi: 10.1016/j.envres.2012.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chan TJ, Gutierrez C, Ogunseitan OA. Metallic burden of deciduous teeth and childhood behavioral deficits. Int J Environ Res Public Health. 2015;12(6):6771–6787. doi: 10.3390/ijerph120606771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ericson JE, Crinella FM, Clarke-Stewart KA, et al. Prenatal manganese levels linked to childhood behavioral disinhibition. Neurotoxicol Teratol. 2007;29(2):181–187. doi: 10.1016/j.ntt.2006.09.020. [DOI] [PubMed] [Google Scholar]
- 19.Rucklidge J, Johnstone J, Harrison R, Boggis A. Micronutrients reduce stress and anxiety in adults with attention-deficit/hyperactivity disorder following a 7.1 earthquake. Psychiatry Res. 2011;189(2):281–287. doi: 10.1016/j.psychres.2011.06.016. [DOI] [PubMed] [Google Scholar]
- 20.Bhang SY, Cho SC, Kim JW, et al. Relationship between blood manganese levels and children’s attention, cognition, behavior, and academic performance – a nationwide cross-sectional study. Environ Res. 2013;126:9–16. doi: 10.1016/j.envres.2013.05.006. [DOI] [PubMed] [Google Scholar]
- 21.Liu W, Huo X, Liu D, Zeng X, Zhang Y, Xu X. S100β in heavy metal-related child attention-deficit hyperactivity disorder in an informal e-waste recycling area. Neurotoxicology. 2014;45:185–191. doi: 10.1016/j.neuro.2014.10.013. [DOI] [PubMed] [Google Scholar]
- 22.Ode A, Rylander L, Gustafsson P, et al. Manganese and selenium concentrations in umbilical cord serum and attention deficit hyperactivity disorder in childhood. Environ Res. 2015;137:373–381. doi: 10.1016/j.envres.2015.01.001. [DOI] [PubMed] [Google Scholar]
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 2.Kliegman R, Behrman RE, Nelson WE. Nelson Textbook of Pediatrics. 20th ed. Atlanta, GA: Elsevier; 2016. [Google Scholar]
- 3.Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry. 2007;164(6):942–948. doi: 10.1176/ajp.2007.164.6.942. [DOI] [PubMed] [Google Scholar]
- 4.Huang S, Hu H, Sánchez BN, et al. Childhood blood lead levels and symptoms of attention deficit hyperactivity disorder (ADHD): a cross-sectional study of Mexican children. Environ Health Perspect. 2016;124(6):868–874. doi: 10.1289/ehp.1510067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lam J, Lanphear BP, Bellinger D, et al. Developmental PBDE exposure and IQ/ADHD in childhood: a systematic review and meta-analysis. Environ Health Perspect. 2017;125(8):086001. doi: 10.1289/EHP1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cortese S. The neurobiology and genetics of attention-deficit/hyperactivity disorder (ADHD): what every clinician should know. Eur J Paediatr Neurol. 2012;16(5):422–433. doi: 10.1016/j.ejpn.2012.01.009. [DOI] [PubMed] [Google Scholar]
- 7.Aschner M, Guilarte TR, Schneider JS, Zheng W. Manganese: recent advances in understanding its transport and neurotoxicity. Toxicol Appl Pharmacol. 2007;221(2):131–147. doi: 10.1016/j.taap.2007.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Guilarte TR, Chen MK, McGlothan JL, et al. Nigrostriatal dopamine system dysfunction and subtle motor deficits in manganese-exposed non-human primates. Exp Neurol. 2006;202(2):381–390. doi: 10.1016/j.expneurol.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 9.Grant K, Goldizen FC, Sly PD, et al. Health consequences of exposure to e-waste: a systematic review. Lancet Glob Health. 2013;1(6):e350–e361. doi: 10.1016/S2214-109X(13)70101-3. [DOI] [PubMed] [Google Scholar]
- 10.Heacock M, Kelly CB, Asante KA, et al. E-waste and harm to vulnerable populations: a growing global problem. Environ Health Perspect. 2016;124(5):550–555. doi: 10.1289/ehp.1509699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Klaassen CD, Casarett LJ, Doull J. Casarett and Doull’s Toxicology: The Basic Science of Poisons. 8th ed. New York, NY: McGraw-Hill Education/Medical; 2013. [Google Scholar]
- 12.Morello M, Canini A, Mattioli P, et al. Sub-cellular localization of manganese in the basal ganglia of normal and manganese-treated rats: an electron spectroscopy imaging and electron energy-loss spectroscopy study. Neurotoxicology. 2008;29(1):60–72. doi: 10.1016/j.neuro.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 13.McDougall SA, Reichel CM, Farley CM, et al. Postnatal manganese exposure alters dopamine transporter function in adult rats: potential impact on nonassociative and associative processes. Neuroscience. 2008;154(2):848–860. doi: 10.1016/j.neuroscience.2008.03.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen P, Chen Z, Li A, et al. Catalytic metalloporphyrin protects against paraquat neurotoxicity in vivo. Biomed Environ Sci. 2008;21(3):233–238. doi: 10.1016/S0895-3988(08)60035-5. [DOI] [PubMed] [Google Scholar]
- 15.Liu W, Huo X, Liu D, Zeng X, Zhang Y, Xu X. S100β in heavy metal-related child attention-deficit hyperactivity disorder in an informal e-waste recycling area. Neurotoxicology. 2014;45:185–191. doi: 10.1016/j.neuro.2014.10.013. [DOI] [PubMed] [Google Scholar]
- 16.Yousef S, Adem A, Zoubeidi T, Kosanovic M, Mabrouk AA, Eapen V. Attention deficit hyperactivity disorder and environmental toxic metal exposure in the United Arab Emirates. J Trop Pediatr. 2011;57(6):457–460. doi: 10.1093/tropej/fmq121. [DOI] [PubMed] [Google Scholar]
- 17.Rodríguez-Barranco M, Lacasaña M, Aguilar-Garduño C, et al. Association of arsenic, cadmium and manganese exposure with neurodevelopment and behavioural disorders in children: a systematic review and meta-analysis. Sci Total Environ. 2013;454–455:562–577. doi: 10.1016/j.scitotenv.2013.03.047. [DOI] [PubMed] [Google Scholar]
- 18.Farias AC, Cunha A, Benko CR, et al. Manganese in children with attention-deficit/hyperactivity disorder: relationship with methylphenidate exposure. J Child Adolesc Psychopharmacol. 2010;20(2):113–118. doi: 10.1089/cap.2009.0073. [DOI] [PubMed] [Google Scholar]
- 19.Hong SB, Kim JW, Choi BS, et al. Blood manganese levels in relation to comorbid behavioral and emotional problems in children with attention-deficit/hyperactivity disorder. Psychiatry Res. 2014;220(1–2):418–425. doi: 10.1016/j.psychres.2014.05.049. [DOI] [PubMed] [Google Scholar]
- 20.Shin DW, Kim EJ, Lim SW, Shin YC, Oh KS, Kim EJ. Association of hair manganese level with symptoms in attention-deficit/hyperactivity disorder. Psychiatry Investig. 2015;12(1):66–72. doi: 10.4306/pi.2015.12.1.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Scassellati C, Bonvicini C, Faraone SV, Gennarelli M. Biomarkers and attention-deficit/hyperactivity disorder: a systematic review and meta-analyses. J Am Acad Child Adolesc Psychiatry. 2012;51(10):1003.e20–1019.e20. doi: 10.1016/j.jaac.2012.08.015. [DOI] [PubMed] [Google Scholar]
- 22.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in epidemiology (MOOSE) group. JAMA. 2000;283(15):2008–2012. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 23.Zeng X, Xu X, Boezen HM, Huo X. Children with health impairments by heavy metals in an e-waste recycling area. Chemosphere. 2016;148:408–415. doi: 10.1016/j.chemosphere.2015.10.078. [DOI] [PubMed] [Google Scholar]
- 24.Grandjean P, Landrigan PJ. Neurobehavioural effects of developmental toxicity. Lancet Neurol. 2014;13(3):330–338. doi: 10.1016/S1474-4422(13)70278-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lucchini R, Placidi D, Cagna G, et al. Manganese and developmental neurotoxicity. Adv Neurobiol. 2017;18:13–34. doi: 10.1007/978-3-319-60189-2_2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Anglin RE, Samaan Z, Walter SD, McDonald SD. Vitamin D deficiency and depression in adults: systematic review and meta-analysis. Br J Psychiatry. 2013;202:100–107. doi: 10.1192/bjp.bp.111.106666. [DOI] [PubMed] [Google Scholar]
- 27.Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1(2):97–111. doi: 10.1002/jrsm.12. [DOI] [PubMed] [Google Scholar]
- 28.Tobias A. Assessing the influence of a single study in meta-analysis. Stata Tech Bull. 1999;47:15–17. [Google Scholar]
- 29.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 30.Borenstein M, Higgins JP, Hedges LV, Rothstein HR. Basics of meta-analysis: I2 is not an absolute measure of heterogeneity. Res Synth Methods. 2017;8(1):5–18. doi: 10.1002/jrsm.1230. [DOI] [PubMed] [Google Scholar]
- 31.Higgins JP, Green S. 10.4.3.1 Recommendations on testing for funnel plot asymmetry. In: Higgins JP, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. 5.1.0 ed. Cochrane Library; 2011. [Accessed July 02, 2018]. Available from: http://handbook-5-1.cochrane.org/chapter_10/10_4_3_1_recommendations_on_testing_for_funnel_plot_asymmetry.htm. [Google Scholar]
- 32.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56(2):455–463. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 34.Franěk T, Kotaška K, Průša R. Manganese and selenium concentrations in cerebrospinal fluid of seriously ill children. J Clin Lab Anal. 2017;31(6):e22122. doi: 10.1002/jcla.22122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Romarís EM, Cervantes II, López JM, Marcén JF. Concentration of calcium and magnesium and trace elements (zinc, copper, iron and manganese) in cerebrospinal fluid: a try of a pathophysiological classification. J Trace Elem Med Biol. 2011;25(Suppl 1):S45–S49. doi: 10.1016/j.jtemb.2010.10.009. [DOI] [PubMed] [Google Scholar]
- 36.Eastman RR, Jursa TP, Benedetti C, Lucchini RG, Smith DR. Hair as a biomarker of environmental manganese exposure. Environ Sci Technol. 2013;47(3):1629–1637. doi: 10.1021/es3035297. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Whole flowchart of the meta-analysis.
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; N/A, not available.
Table S1.
Results of Newcastle–Ottawa Scale scores of recruited studies
| Study | Criteria | Source | Sample method | Newcastle–Ottawa Scale
|
Country | ||||
|---|---|---|---|---|---|---|---|---|---|
| Selection | Performance | Detection | Information | Total | |||||
| Shin et al1 | DSM-IV | Hair | Inductively coupled plasma mass spectrometry | 1 | 5 | 4 | 5 | 15 | Republic of Korea |
| Hong et al2 | DISC-IV | Blood | Graphite furnace atomic absorption spectrometry | 3 | 5 | 5 | 4 | 17 | Republic of Korea |
| Yousef et al3 | DSM-IV | Blood | N/A | 2 | 5 | 4 | 4 | 15 | United Arab Emirates |
| Farias et al4 | DSM-IV | Blood | Graphite furnace atomic absorption spectrometry | 2 | 5 | 4 | 4 | 15 | Brazil |
Abbreviations: DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; DISC-IV, Diagnostic Interview Schedule for Children Version IV; N/A, not available.
Table S2.
Excluded studies and reasons
| Not related to manganese and ADHD (n=4) |
| Konstantopoulos et al5 |
| Hu et al6 |
| Konrad et al7 |
| Han et al8 |
| Meta-analysis (n=2) |
| Rodríguez-Barranco et al9 |
| Scassellati et al10 |
| Review articles (n=3) |
| Zeng et al11 |
| Grandjean and Landrigan12 |
| Lucchini et al13 |
| Not definite diagnosis of ADHD (n=5) |
| Hong et al14 |
| Bouchard et al15 |
| Lucchini et al16 |
| Chan et al17 |
| Ericson et al18 |
| Compare treatment effect of micronutrient but not related to manganese and ADHD (n=1) |
| Rucklidge et al19 |
| Use the same data sample sources of Hong et al2 (n=1) |
| Bhang et al20 |
| Lack of control (n=1) |
| Liu et al21 |
| Collecting manganese when ADHD children were just given birth (n=1) |
| Ode A et al22 |
Abbreviation: ADHD, attention-deficit/hyperactivity disorder.