Abstract
Introduction
Key population (KP) members frequently experience violence that violates their human rights, increases their risk of HIV, and acts as a barrier to access and uptake of HIV services. To be effective, HIV programmes for members of KPs need to prevent and respond to violence against them. We describe a violence prevention and response strategy led by the national KP programme in Kenya and examine trends in reports of and responses to violence (provision of support to an individual who reports violence within 24 hours of receiving the report).
Methods
Quarterly programme monitoring data on the number of reports of violence and the number of responses to violence from 81 implementing partners between October 2013 and September 2017 were aggregated annually and analysed using simple trend analysis. Reports of violence relative to KP members reached, expressed as a percentage, and the percentage of reports of violence that received a response were also examined.
Results and Discussion
Between 2013 and 2017, annual reports of violence increased from 4171 to 13,496 cases among female sex workers (FSWs), 910 to 1122 cases among men who have sex with men (MSM) and 121 to 873 cases among people who inject drugs (PWID). Reports of violence relative to KP members reached increased among FSWs (6.2% to 9.7%; p < 0.001) and PWID (2.1% to 6.0%; p < 0.001) and decreased among MSM (10.0% to 4.2%; p < 0.001). During the same period, timely responses to reports of violence increased from 53% to 84% (p < 0.001) among FSWs, 44% to 80% (p < 0.001) among MSM and 37% to 97% (p < 0.001) among PWID.
Conclusions
Over the past four years in Kenya, there has been an increase in violence reporting among FSWs and PWID and an increase in violence response among all KPs. This case study demonstrates that violence against KP members can be effectively addressed under the leadership of the national government, even in an environment where KP members’ behaviours are criminalized. Creating an enabling environment to promote wellbeing and safety for KP members is a critical enabler for HIV prevention programmes to achieve 95‐95‐95 goals.
Keywords: key populations, violence response, Government of Kenya, HIV, enabling environment
1. Introduction
The HIV Prevention 2020 Roadmap provides guidance and demonstrates commitment from African countries to accelerate interventions to reduce new HIV infections by 75% 1. In Africa, the proportion of new infections among key populations (KPs), defined as female sex workers (FSWs), men who have sex with men (MSM), and people who inject drugs (PWID), is substantial 2. Greater investment in KP programmes can improve the effectiveness of HIV interventions 3. However, punitive laws related to sex work, same‐sex sexual practices and drug use; stigma and discrimination in community and healthcare settings; and violence hinder access to and uptake of HIV‐related services among KPs 4, 5, 6. In such environments, UNAIDS has called upon governments to create an enabling environment and develop pragmatic solutions to ensure that KPs can organize to reduce risk and prevent HIV, while simultaneously increasing access to prevention programmes 1.
Kenya has a mixed and geographically heterogeneous HIV epidemic, with an estimated national adult HIV prevalence of 5.9% 7, and an estimated 33% of all new infections occurring among KP members 8. In Nairobi, HIV prevalence is 6.1% among adults, 29.3% among FSWs, 18.2% among MSM and 18.7% among PWID 7, 9. The KP programme is led by the National AIDS and STI Control Programme (NASCOP) and the National AIDS Control Council (NACC) within the Ministry of Health and implemented by 81 partners primarily funded by PEPFAR and the Global Fund. NACC and NASCOP, in collaboration with KP‐led organizations, have developed policies 10 and guidelines 11 to support KP programme implementation. The programme has been scaled up to reach an average of 139,041 FSWs in 33 counties, 26,972 MSM in 29 counties and 14,527 PWID in 16 counties quarterly 12. A national population‐based survey conducted by NASCOP with 5,353 KPs in 2017 found that, in the last three months, 88% of FSWs, 80% of MSM and 84% of PWID were met by a peer educator; 85% of FSWs, 76% of MSM and 74% of PWID received an HIV test; and 74% of FSWs, 68% of MSM and 72% of PWID accessed services from a programme site 13.
Research in Kenya has found that physical, sexual and emotional violence against KPs is common and frequently perpetrated by sex work clients, police, religious leaders, intimate partners and strangers 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24. A survey conducted by NASCOP in 2017 found that 22% of FSWs, 14% of MSM and 12% of PWID experienced physical or sexual violence, while 48% of FSWs, 20% of MSM and 44% of PWID experienced police violence in the past six months 13. Each population has unique experiences with violence: violence against FSWs is often physical violence perpetrated by clients and regular sex partners, while violence against MSM is often “opportunistic aggression” perpetrated by strangers 15. Furthermore, MSM who engage in sex work are two times more at risk of violence than those who do not 25. Violence against PWID is often associated with cocaine or heroin use and includes arbitrary police sweeps, beatings, harassment, bribery, remand, and imprisonment 20. Across populations, violence is fuelled by gender inequalities and stigma and discrimination against persons perceived to depart from conventional gender and sexual norms and identities 26, 27, 28. The Kenyan legal system and county by‐laws that criminalize behaviours related to sex work, same‐sex sexual practices and drug use also legitimize violence, stigma and discrimination against KPs 29, 30, 31, 32.
Violence against KP members increases HIV risk and decreases HIV service uptake 33, 34, 35, 36, 37. Studies in Kenya show that violence and HIV are linked through intermediate risk factors such as unprotected sex and unsafe injecting practices 20, 38, 39. One study found that female and male sex workers who anticipate sexual violence or experience physical violence are more likely to avoid or delay HIV services than those who do not 24. Experiencing violence or fear of violence can also result in KPs prioritizing their safety over less immediate concerns such as HIV 40, 41. Furthermore, modelling in Kenya suggests that eliminating sexual violence against FSWs could avert 17% of new HIV infections among FSWs and their clients over 10 years 38.
The Kenyan national KP programme has prioritized violence as a key structural barrier to HIV‐related services 11, and adopted strategies to address violence against KPs in the National Guidelines for HIV/STI Programming with KPs 11. The KP programme posits that increasing violence reporting by KP members and improving responses to violence by implementing partners will reduce violence and thereby reduce new HIV infections among KP members in the long run 3, 11, 42. In this paper, we describe a violence prevention and response strategy adopted by the KP programme and examine trends in reports of and responses to violence.
2. Methods
2.1. Data Source
Eighty‐one implementing partners who serve FSWs, MSM and PWID, and operate in primarily urban areas, collected individual‐level service utilization data monthly (number of KPs reached, number of reports of violence and number of responses to violence) and submitted quarterly, aggregate‐level information to NASCOP as part of routine programme monitoring between October 2013 and September 2017. A report of violence is defined as a KP member disclosing violence — such as sexual assault, physical assault, verbal abuse, discrimination and arbitrary arrest — to a violence response team member via a helpline, a peer educator during outreach or a clinician during a facility visit. A response to violence is defined as a violence response team member, peer educator or clinician providing first‐line support within 24 hours of receiving the report to the individual who disclosed violence. First‐line support includes active listening, providing key messages and information on rights, safety planning, and providing services directly or through referrals.
2.2. Analysis
Number of KPs reached, number of reports of violence and number of responses to violence were aggregated annually and analysed. The rates of increase in KP members reached and reports of violence were analysed using the reported numbers in 2013 to 2014 as the reference year, and then dividing the numbers from subsequent reporting years over the reference year. The 2013 to 2014 period was selected as the reference year as it was before the violence prevention and response strategy was introduced in 2014 to 2015. Reports of violence relative to KP members reached, expressed as a percentage, and the percentage of reports of violence that received a response were also calculated. A chi square test was used to determine whether changes in violence reporting and response over time were statistically significant.
2.3. Ethics approval
These data were collected through routine programme monitoring and cannot be linked to any individual. Ethical approval to conduct secondary data analysis was received from the Kenyatta National Hospital — University of Nairobi Ethical Review Committee, number P647/11/2017.
2.4. Violence prevention and response strategy
The national KP programme developed a violence prevention and response strategy (Figure 1) and complementary protocol 43, in consultation with KP‐led organizations, to guide NASCOP, NACC and implementing partners to develop and implement a violence prevention and response plan. Although the national KP programme has a two‐pronged strategy that includes violence prevention, this paper focuses on violence response.
Figure 1.
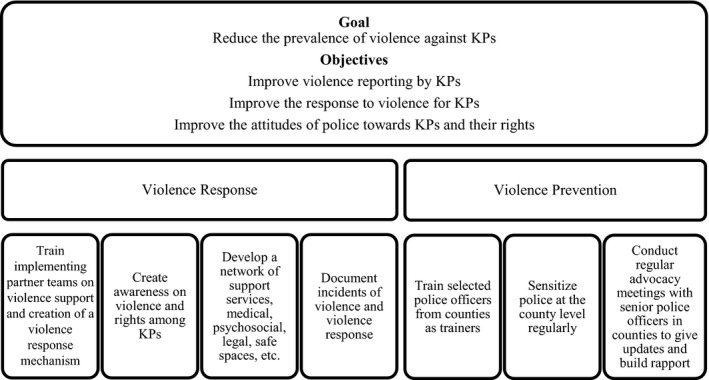
Two‐pronged strategy to address violence against key populations (KPs) in Kenya.
Building implementing partner knowledge and skills to support KP victims of violence is central to violence response. Implementing partners were trained using a national curriculum developed by NASCOP 44, and in turn, educated KPs on violence and their rights using NASCOP‐supported communication materials during outreach and clinical services. Implementing partners conducted educational events at drop‐in centres to encourage reporting and service seeking and to set up mechanisms to effectively and efficiently respond to violence. Some implementing partners have violence response teams that manage 24‐hour helplines. The violence response teams consist of peer educators, peer paralegals and outreach workers that are supported by clinicians, advocacy officials and programme managers. Each implementing partner developed a network of services to ensure that post‐violence support (clinical, psychosocial, legal and safety) could be provided directly or through referral. KP members are encouraged to report violence by calling violence response team helplines, disclosing to a peer educator during outreach or disclosing to a clinician during a facility visit. When violence is disclosed, the violence response team member, peer educator or clinician seeks information about the incident and provides first‐line support. They assess the situation and, in collaboration with the victim, develop a response and support plan that includes further post‐violence support, per need and client preferences. They also document the incident of violence in a standard national format. In Kenya, the goal is to initiate post‐violence support within 24 hours of receiving a report.
3. Results and Discussion
Between 2013 and 2014 (reference year) and 2016 to 2017, the annual number of KP members reached increased from 67,432 to 139,041 among FSWs, 9118 to 26,972 among MSM and 5856 to 14,527 among PWID (Tables 1, 2, 3). During the same period, the annual number of reports of violence increased from 4171 to 13,496 among FSWs, 910 to 1122 among MSM and 121 to 873 among PWID. Reports of violence relative to KP members reached increased among FSWs (6.2% to 9.7%; p < 0.001) and PWID (2.1% to 6.0%; p < 0.001) and decreased among MSM (10.0% to 4.2%; p < 0.001). The percentage of reports of violence that received a response increased among all KPs: 53% to 84% among FSWs (p < 0.001), 37% to 97% among PWID (p < 0.001) and 44% to 80% among MSM (p < 0.001).
Table 1.
Annual data on programme reach, reports of violence and responses to violence by FSWs in Kenya, October 2013 through September 2017
| Indicator | Oct 2013 to Sept 2014a | Oct 2014 to Sept 2015 | Oct 2015 to Sept 2016 | Oct 2016 to Sept 2017 |
|---|---|---|---|---|
| Number of FSWs reached | 67432 | 88327 | 113096 | 139041 |
| Number of FSW reports of violence | 4171 | 5341 | 11707 | 13496 |
| Rate of increase in number of FSWs reached | 1.0 | 1.3 | 1.7 | 2.1 |
| Rate of increase in number of FSW reports of violence | 1.0 | 1.3 | 2.8 | 3.2 |
| FSW reports of violence relative to FSWs reached, expressed as a percentage | 6.2 | 6.0 | 10.4 | 9.7b |
| Percent of responses to FSW reports of violence | 53 | 65 | 74 | 84b |
Reference year
p < 0.001
Table 2.
Annual data on programme reach, reports of violence and responses to violence by MSM in Kenya, October 2013 through September 2017
| Indicator | Oct 2013 to Sept 2014a | Oct 2014 to Sept 2015 | Oct 2015 to Sept 2016 | Oct 2016 to Sept 2017 |
|---|---|---|---|---|
| Number of MSM reached | 9118 | 12106 | 16680 | 26972 |
| Number of MSM reports of violence | 910 | 849 | 1026 | 1122 |
| Rate of increase in number of MSM reached | 1.0 | 1.3 | 1.8 | 3.0 |
| Rate of increase in number of MSM reports of violence | 1.0 | 0.9 | 1.1 | 1.2 |
| MSM reports of violence relative to MSM reached, expressed as a percentage | 10.0 | 7.0 | 6.2 | 4.2b |
| Percent of responses to MSM reports of violence | 44 | 77 | 86 | 80b |
Reference year
p < 0.001
Table 3.
Annual data on programme reach, reports of violence and responses to violence by PWID in Kenya, October 2013 through September 2017
| Indicator | Oct 2013 to Sept 2014a | Oct 2014 to Sept 2015 | Oct 2015 to Sept 2016 | Oct 2016 to Sept 2017 |
|---|---|---|---|---|
| Number of PWID reached | 5856 | 7001 | 10990 | 14527 |
| Number of PWID reports of violence | 121 | 533 | 839 | 873 |
| Rate of increase in number of PWID reached | 1.0 | 1.2 | 1.9 | 2.5 |
| Rate of increase in number of PWID reports of violence | 1.0 | 4.4 | 6.9 | 7.2 |
| PWID reports of violence relative to PWID reached, expressed as a percentage | 2.1 | 7.6 | 7.6 | 6.0 b |
| Percent of responses to PWID reports of violence | 37 | 48 | 89 | 97b |
Reference year
p < 0.001
Violence response is relatively new in KP programmes, and it is vital to monitor whether such activities result in expected outcomes 45. In the absence of validated and internationally agreed‐upon indicators specific to violence against KPs, projects such as the Avahan AIDS Initiative in India collected data on reports of and responses to violence to monitor programme effectiveness 5, 6. Programmatic data on reports of violence are important because violence cannot be redressed if unreported 46, and reporting is a critical first step to link victims to post‐violence support 5, 6. Reports of violence over time also provide useful information about programme outcomes as increased reporting often occurs when KPs understand that violence was committed, know their rights, have an enabling environment to disclose violence and seek support, and have confidence in the response mechanism 5, 6, 46, 47. Programmatic data on responses to violence are also important as they show whether KPs who reported violence received critical post‐violence support such as post‐exposure prophylaxis 48. These data can also inform processes to address violence within the programme and guide the development of policies relevant to KPs 49.
Among FSWs and PWID, the increase in reports of violence relative to individuals reached may be due to the introduction of the national violence prevention and response strategy in 2014 to 2015. This is in line with global literature that shows that programmes tend to see an uptick in reports of violence after a programme monitoring system is established 5 and victims are sensitized 46. The increase in responses to reports of violence may also help explain this rise as FSWs and PWID may be more likely to report violence if they have social proof that their peers have received a positive response upon disclosing violence 50.
Among MSM, the decrease in reports of violence relative to individuals reached tells a different story. MSM‐serving organisations in Kenya established a system to ensure safety and security among MSM, sensitized police and religious leaders and conducted community outreach beginning in 2010 in reaction to violence against MSM in Mtwapa 23. This system was strengthened in anticipation of a backlash when Uganda's Anti‐Homosexuality Act was passed in 2014 23. This longer‐term effort, coupled with the high percentage of reports of violence in the reference year and decreases in reports in subsequent years, suggest that an uptick in reporting occurred before the strategy was introduced and that the decrease in reports of violence may reflect actual decreases in violence.
These programmatic data alone, however, have limited ability to show trends in actual violence. Fortunately, in Kenya, there is supplemental information on prevalence of physical/sexual violence and police violence against KP members from national population‐based surveys conducted 2014 to 2017 13. According to the surveys, prevalence of physical/sexual violence stayed static among FSWs, increased among PWID and decreased among MSM while police violence increased among FSWs and decreased among PWID and MSM 13. Programmatic and population‐based data offer useful information on their own and in relation to one another. For example, even at peak reporting, programmatic data on reports of violence have not reached the level of violence found in the surveys. This suggests that KPs may still be underreporting violence to implementing partners, for example, because there are remaining barriers to reporting, such as perceived stigma against victims 51, or because KPs are more equipped to address violence through their own networks without implementing partners 52.
3.1. Limitations
These programmatic data do not provide a full account of violence experienced by KPs in Kenya. For example, as the data were reported in aggregate on a quarterly basis, we were not able to conduct advanced statistical analysis, including exploring whether violence outcomes are related to HIV outcomes. As mentioned previously, programmatic data are limited in tracking actual violence and could overestimate violence (if some KPs report multiple incidents of violence) or underestimate violence (if KPs do not report violence they experience).
Going forward, it will be important to continue to collect and triangulate programmatic and population‐based data to analyse trends, including types of violence and perpetrators, over time. To address challenges in interpreting violence data, there is also a need for refined metrics and research to explore whether violence prevention and response interventions in KP programmes are having the intended effects, including specific questions on KP members’ experiences and satisfaction with violence prevention and response services. Future research also needs to explore whether an increase in responses to violence corresponds with an increase in HIV service uptake and whether those who report violence are more likely to re‐test or adhere to antiretroviral drugs than those who do not report violence.
4. Conclusions
The programmatic data from the national KP programme show that reports of violence relative to individuals reached increased among FSWs and PWID but decreased among MSM while the percent of reports of violence that received a response increased among all KPs. These data suggest that FSWs and PWID have the desire and ability to report violence, that MSM are seeing decreases in violence and that implementing partners are responding to reports of violence in a timely manner. This paints an overall positive picture of the impacts of the national violence prevention and response strategy and emphasizes the need for multiple sources of information to triangulate data and observe changes that may not become immediately apparent in programmatic or population‐based data alone.
In most parts of Africa, where sex work, same‐sex sexual practices and drug use are criminalized, implementing HIV programmes for KPs can be a challenge. However, Kenya has shown that with government leadership, it is not only possible to implement a robust key population programme, but also to address violence to help create an enabling environment for KPs to access HIV‐related services and thus enable the country to move more effectively towards meeting the 95‐95‐95 global targets.
Funding
This publication is made possible by the support of BMGF under grant ID OPP 1032367 as well as the American People through USAID under cooperative agreement number AID‐OAA‐A‐14‐00045. The views expressed herein are those of the authors and do not necessarily reflect the official policy or position of BMGF, USAID, or the U.S. government.
Authors’ contributions
PB and GJM were involved equally in the development of this manuscript. HKM, PB, TMK, JMM, RTM and SJM designed and implemented the intervention. PB and SKI were involved in analysing the quantitative data. RLD, SM, HKM and BEO were involved in reviewing and finalizing the manuscript. All authors have reviewed and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Acknowledgements
The authors would like to acknowledge all the implementing partners including KP‐led organizations who report every quarter to NASCOP. We also thank all the peer educators and outreach workers from KP communities who provide support to KP victims of violence and build their confidence to report violence. Their efforts in documentation provide evidence to the implementing partners and the country to advocate for effective violence prevention and response. Acknowledgements are also due to the Key Populations Technical Support Unit (TSU) housed within NASCOP, Ministry of Health, which supports implementation of KP‐related national strategies. The TSU project is implemented by the University of Manitoba with funding support from the Bill & Melinda Gates Foundation (BMGF) and the U.S. Agency for International Development (USAID), through the LINKAGES project implemented by FHI 360.
Bhattacharjee, P. , Morales, G. J. , Kilonzo, T. M. , Dayton, R. L. , Musundi, R. T. , Mbole, J. M. , Malaba, S. J. , Ogwang, B. E. , Isac, S. K. , Moses, S. and Musyoki, H. K. Can a national government implement a violence prevention and response strategy for key populations in a criminalized setting? A case study from Kenya. J Int AIDS Soc. 2018;21(S5):e25122
References
- 1. Joint United Nations Programme on HIV/AIDS . HIV prevention 2020 road map. Geneva: Joint United Nations Programme on HIV/AIDS; 2017. [Google Scholar]
- 2. Kharsany AB, Karim QA. HIV Infection and AIDS in Sub‐Saharan Africa: current status, challenges and opportunities. Open AIDS J. 2016;10:34–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. World Health Organization . Consolidated guidelines on HIV prevention, diagnosis, treatment and care for key populations – 2016 update. Geneva: World Health Organization; 2016. [Google Scholar]
- 4. United Nations Office on Drugs and Crime, International Network of People Who Use Drugs, Joint United Nations Programme on HIV/AIDS, United Nations Development Programme, United Nations Population Fund, World Health Organization, et al . Implementing comprehensive HIV and HCV programmes with people who inject drugs: practical guidance for collaborative interventions. Vienna: United Nations Office on Drugs and Crime; 2017. [Google Scholar]
- 5. United Nations Population Fund, Global Forum on MSM & HIV, United Nations Development Programme, World Health Organization, U.S. Agency for International Development, World Bank . Implementing comprehensive HIV and STI Programmes with men who have sex with men: practical guidance for collaborative interventions. New York: United Nations Population Fund; 2015. [Google Scholar]
- 6. World Health Organization, United Nations Population Fund, Joint United Nations Programme on HIV/AIDS, Global Network of Sex Work Projects, World Bank, United Nations Development Programme . Implementing comprehensive HIV/STI programmes with sex workers: practical approaches from collaborative interventions. Geneva: World Health Organization; 2013. [Google Scholar]
- 7. National AIDS Control Council . Kenya HIV estimates 2015. Nairobi: Government of Kenya; 2016. [Google Scholar]
- 8. National AIDS Control Council . Kenya HIV prevention response and modes of transmission analysis, final report. Nairobi: Government of Kenya; 2009. [Google Scholar]
- 9. National AIDS and STI Control Programme . 2010–2011 Integrated biological and behavioural surveillance survey among key populations in Nairobi and Kisumu, Kenya. Nairobi: Government of Kenya, Ministry of Public Health and Sanitation; 2014a. [Google Scholar]
- 10. National AIDS Control Council, National AIDS and STI Control Programme . Policy for prevention of HIV infections among key populations in Kenya. Nairobi: Government of Kenya; 2016. [Google Scholar]
- 11. National AIDS and STI Control Programme . National guidelines for HIV/STI programming with key populations. Nairobi: Government of Kenya; 2014b. [Google Scholar]
- 12. National AIDS and STI Control Programme . Quarterly programme monitoring report, September 2017. Nairobi: Government of Kenya; 2017a. [Google Scholar]
- 13. National AIDS and STI Control Programme . Third national behavioural assessment of key populations in Kenya, polling booth survey report. Nairobi: Government of Kenya; 2017b. [Google Scholar]
- 14. Parcesepe AM, L'Engle KL, Martin SL, Green S, Suchindran C, Mwarogo P. Early sex work initiation and violence against female sex workers in Mombasa, Kenya. J Urban Health. 2016;93(6):1010–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Micheni M, Rogers S, Wahome E, Darwinkel M, van der Elst E, Gichuru E, et al. Risk of sexual, physical and verbal assaults on men who have sex with men and female sex workers in coastal Kenya. AIDS. 2015;29(Suppl 3):S231–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Guise A, Dimova M, Ndimbii J, Clark P, Rhodes T. A qualitative analysis of transitions to heroin injection in Kenya: implications for HIV prevention and harm reduction. Harm Reduct J. 2015;12:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Muraguri N, Tun W, Okal J, Broz D, Raymond HF, Kellogg T, et al. HIV and STI prevalence and risk factors among male sex workers and other men who have sex with men in Nairobi, Kenya. J Acquir Immune Defic Syndr. 2015;68(1):91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Scorgie F, Vasey K, Harper E, Richter M, Nare P, Maseko S, et al. Human rights abuses and collective resilience among sex workers in four African countries: a qualitative study. Global Health. 2013;9(1):33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Chersich MF, Luchters SM, Malonza IM, Mwarogo P, King'ola N, Temmerman M. Heavy episodic drinking among Kenyan female sex workers is associated with unsafe sex, sexual violence and sexually transmitted infections. Int J STD AIDS. 2007;18(11):764–9. [DOI] [PubMed] [Google Scholar]
- 20. Kageha E. Drug laws and human rights in Kenya: disharmony in the law and training recommendations to law enforcement. Amsterdam: Mainline Foundation; 2015. [Google Scholar]
- 21. FIDA Kenya . Documenting human rights violations of sex workers in Kenya: A report based on findings of a study conducted in Nairobi, Kisumu, Busia, Nanyuki, Mombasa and Malindi towns in Kenya. Nairobi: FIDA Kenya; 2008. [Google Scholar]
- 22. Onyango‐Ouma W, Birungi H, Geibel S. Understanding the HIV/STI risks and prevention needs of men who have sex with men in Nairobi, Kenya. Horizons final technical report Washington, DC: Population Council; 2005. [Google Scholar]
- 23. Human Rights Watch . The issue is violence: Attacks on LGBT peole on Kenya's coast. Human Rights Watch and PEMA Kenya; 2015. [Google Scholar]
- 24. Nyblade L, Mbote D, Barker C, Stockton M, Mwai D, Oneko T, et al. editors. Anticipated and experienced violence among male and female sex workers in Kenya and their relationship to utilization of general and HIV‐specific health services. 21st International AIDS Conference; 2016 July 18‐22; Durban, South Africa.
- 25. Laibon R, Kiptoo M, Ngure K, Hauck M, Memiah P, Mathenge J. Prevalence and factors associated with sexual violence among male sex workers (MSW) on antiretroviral therapy in Nairobi, Kenya. Int J Sci: Basic Appl Res. 2016;30(1):76–85. [Google Scholar]
- 26. LINKAGES . The nexus of gender and HIV among sex workers in Kenya. Durham (NC): FHI 360; 2016a. [Google Scholar]
- 27. LINKAGES . The nexus of gender and HIV among people who inject drugs in Kenya. Durham (NC): FHI 360; 2016b. [Google Scholar]
- 28. LINKAGES . The nexus of gender and HIV among men who have sex with men in Kenya. Durham (NC): FHI 360; 2016c. [Google Scholar]
- 29. National AIDS Control Council . Policy analysis and advocacy decision model for services for key populations in Kenya. Nairobi: Government of Kenya; 2014. [Google Scholar]
- 30. Okal J, Chersich MF, Tsui S, Sutherland E, Temmerman M, Luchters S. Sexual and physical violence against female sex workers in Kenya: a qualitative enquiry. AIDS Care. 2011;23(5):612–8. [DOI] [PubMed] [Google Scholar]
- 31. Avert . HIV and AIDS in Kenya 2017 . Available from: https://www.avert.org/professionals/hiv-around-world/sub-saharan-africa/kenya[cited: 8 April 2018].
- 32. Sida . The rights of LGBTI people in Kenya 2015. Available from: https://www.sida.se/globalassets/sida/eng/partners/human-rights-based-approach/lgbti/rights-of-lgbt-persons-kenya.pdf[cited: 8 April 2018].
- 33. Gardsbane D. Gender‐based violence and HIV: technical brief. Arlington (VA): U.S. Agency for International Development, AIDSTAR‐One; 2010. [Google Scholar]
- 34. Decker MR, Crago A‐L, Chu SK, Sherman SG, Seshu MS, Buthelezi K, et al. Human rights violations against sex workers: burden and effect on HIV. Lancet. 2015;385(9963):186–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Flint A. Gender, violence and the spread of HIV/AIDS. HIV/AIDS in Sub‐Saharan Africa. London: Palgrave Macmillan; 2011. [Google Scholar]
- 36. Beattie TS, Bhattacharjee P, Isac S, Mohan H, Simic‐Lawson M, Ramesh B, et al. Declines in violence and police arrest among female sex workers in Karnataka state, south India, following a comprehensive HIV prevention programme. J Int AIDS Soc. 2015;18(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Shaw SY, Lorway RR, Deering KN, Avery L, Mohan HL, Bhattacharjee P, et al. Factors associated with sexual violence against men who have sex with men and transgendered individuals in Karnataka, India. PLoS ONE. 2012;7(3):e31705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Shannon K, Strathdee SA, Goldenberg SM, Duff P, Mwangi P, Rusakova M, et al. Global epidemiology of HIV among female sex workers: influence of structural determinants. Lancet. 2015;385(9962):55–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Decker MR, Wirtz AL, Pretorius C, Sherman SG, Sweat MD, Baral SD, et al. Estimating the impact of reducing violence against female sex workers on HIV epidemics in Kenya and Ukraine: a policy modeling exercise. Am J Reprod Immunol. 2013;69(Suppl 1):122–32. [DOI] [PubMed] [Google Scholar]
- 40. Bekker LG, Johnson L, Cowan F, Overs C, Besada D, Hillier S, et al. Combination HIV prevention for female sex workers: what is the evidence? Lancet. 2015;385(9962):72–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. World Health Organization . Violence against women and HIV/AIDS: critical intersections – violence against sex workers and HIV prevention. Information Bulletin Series, Number 3 Geneva: World Health Organization; 2005. [Google Scholar]
- 42. Joint United Nations Programme on HIV/AIDS . Global AIDS Monitoring 2017: indicators for monitoring the 2016 United Nations Political Declaration on HIV and AIDS. Geneva: Joint United Nations Programme on HIV/AIDS; 2016. [Google Scholar]
- 43. National AIDS Control Council . National AIDS and STI Control Programme, National violence prevention and response protocol. Nairobi: Government of Kenya; 2017. [Google Scholar]
- 44. National AIDS and STI Control Programme . Responding to violence against key populations HIV services: training manual and reference guide. Nairobi: Government of Kenya; 2016. [Google Scholar]
- 45. Bloom SS. Violence against women and girls: a compendium of monitoring and evaluation indicators. Chapel Hill (NC): MEASURE Evaluation; 2008. [Google Scholar]
- 46. Mahapatra B, Battala M, Porwal A, Saggurti N. Non‐disclosure of violence among female sex workers: evidence from a large scale cross‐sectional survey in India. PLoS ONE. 2014;9(5):e98321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. United Nations . Indicators to measure violence against women: report of the expert group meeting. Geneva: United Nations; 2007. [Google Scholar]
- 48. World Health Organization . Responding to intimate partner violence and sexual violence against women: WHO clinical and policy guidelines. Geneva: World Health Organization; 2013. [PubMed] [Google Scholar]
- 49. Fawole OI, Dagunduro AT. Prevalence and correlates of violence against female sex workers in Abuja, Nigeria. Afr Health Sci. 2014;14(2):299–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Vedantam S. Why #MeToo happened in 2017: National Public Radio; 2017. Podcast. Available from: https://www.npr.org/2018/02/07/583910310/why-metoo-happened-in-2017[cited: 20 April 2018]
- 51. Dutton MA. Battered women's strategic response to violence: the role of context In: Future interventions with battered women and their families. Edelson JL, Eiskovits ZC. (eds). London: Sage Publications; 1996. [Google Scholar]
- 52. Kundu NK. SANGRAM's collectives: engaging communities in India to demand their rights. Arlington (VA): AIDSTAR‐One; 2011. [Google Scholar]


