Abstract
Leprosy is a neglected disease. The insidious onset of leprosy results in its late diagnosis and therefore the spread of the disease. Characterization of leprosy in areas with higher risk and collection of enough information about these spots to adopt more effective controlling measures are of great importance. In the present study, data for every patient who either referred to the health care center for leprosy or had had similar leprous symptoms between 2002 and 2016 were collected. Forty-two new cases of leprosy were identified with 28 of them being Iranian and 14 from Afghanistan. All patients were older than 15. 26.2% of the patients were women and 73.8% were men. According to World Health Organization (WHO) protocol, 36 patients (85.7%) were diagnosed to have been affected by the Multi Bacillary form; and among those patients, 61.9%, 19.05%, and 19.05% suffered from grade 1, 0, and 2 of the disease, respectively. There was a significant relationship between disability grading and sex (P=0.032), with grade 1 disability happening more often in men. Another significant relationship was also observed between Multi Bacillary form and nationality (P=0.011) indicating that Multi Bacillary form is more common among Iranians. With 0.02 leprosy cases in 10000 people, Iran is at elimination phase of the disease; however, identification of new cases in our region demands constant controlling programs and establishment of strict policies. Fortunately, the few numbers of patients diagnosed with leprosy in Northeast of Iran shows successful implementation of such policies under the scrutiny of the public health authorities.
Keywords: Leprosy , Epidemiology , Incidence , Iran
What’s Known
The status of different forms of leprosy in different parts of the world such as Brazil, Nepal, and Ethiopia, but more importantly in Iran.
The different rates of male to female patients’ affection by different forms of leprosy in Iran compared with some other countries.
What’s New
The status of new cases of leprosy in the Northeast of Iran which is important in controlling the disease and managing preventing programs. Our results suggested a significant relationship between disability-grading and sex (P=0.032) as well as a significant relationship between Multi Bacillary form of the disease and nationality (P=0.011)
Introduction
Leprosy (Hansen’s disease) is a chronic disease caused by Mycobacterium leprae. It is one of those nine Mycobacteriums that can affect skin with neurodegenerative complications and it has not been cultured yet. Bratschi et al. reported different routes of transmission for Mycobacterium leprae in a systematic review article as: 1- human to human via aerosols and droplet, 2- direct inoculation into skin by direct contact, 3- environmental and zoonotic reservoirs (e.g. contact armadillo with human) and low socio-economic status (bad housing, contaminated water supply, low educational status, and food shortage) leading to a poor body immune system and higher risk of dealing with environmental reservoirs.1-3
Leprosy primarily disturbs the skin and then the peripheral nerves. It may also strike the eyes and the thin tissue inside of the nose. Leprosy is characterized by disfiguring skin sores, lumps, or bumps that do not disappear after several weeks or months. Nerve damage can cause muscle weakness resulting in loss of feeling in the arms and legs.4 The degree of the disability of a leprous patient is classified from 0 to 2 by WHO; Grade 0 indicates no impairment; Grade 1 shows loss of sensation in the hand, eyes, or foot, and by reaching grade 2 the visible impairment will be noticed. Another valid scoring system to describe the level of impairment in patients with leprosy is EHF score (Eyes, Hands, Feet) which combines indicators of physical damage and the EHF Sum Score obtained by adding the maximum grade for each of six body sites (eyes, hands, and feet) ranging from 0 to 12.5
"Elimination of Leprosy as a Public Health Problem by the Year 2000” was a strategic program set by WHO in 1991 in order to decrease the prevalence of leprosy to less than one case per 10000 population. Collected data by WHO from 102 countries revealed that the number of those affected by leprosy in Southeast Asia and America was 8.38 and 3.78 cases per 10000 people in 2013. Accordingly, WHO has proposed a new strategy: Global Leprosy Strategy 2016-2020 “Accelerating towards a leprosy-free world”.6-8
In line with the policies of WHO against leprosy and to raise awareness of the disease, more studies in endemic areas are needed to be conducted as well as setting control and prevention programs. In Iran, almost 50 years ago, the provinces of East Azerbaijan, Gilan, West Azerbaijan and Khorasan were known as four main sites with the highest number of leprosy patients.9
In the present study, we investigated new leprosy cases in the Northeast of Iran over the past 15 years to help increase public understanding of the disease and establishment of policies to eradicate leprosy for good from this region.
Patients and Methods
This research is a cross-sectional study. All patients suspicious of having leprosy in the Northeast of Iran were referred to special health centers where diagnostic bacteriological tests for leprosy were performed in their microbiological laboratories from 2002 to 2016.
Patients whose clinical findings proved the presence of the disease in them were referred to microbiology laboratory after a full examination by physicians. Skin biopsy was done from the serous layer of skin lesions by scratch rubbing method for each patient; for those without suitable skin lesion, samples from exterior parts of the eyebrows, earlobe, and nose pliers were taken. To stain the smears, hot Ziehl-Neelsen method was used.10 All patients’ information such as age, sex, occupation, marital status, nationality, clinical manifestations, and disabilities were evaluated and recorded.
Results
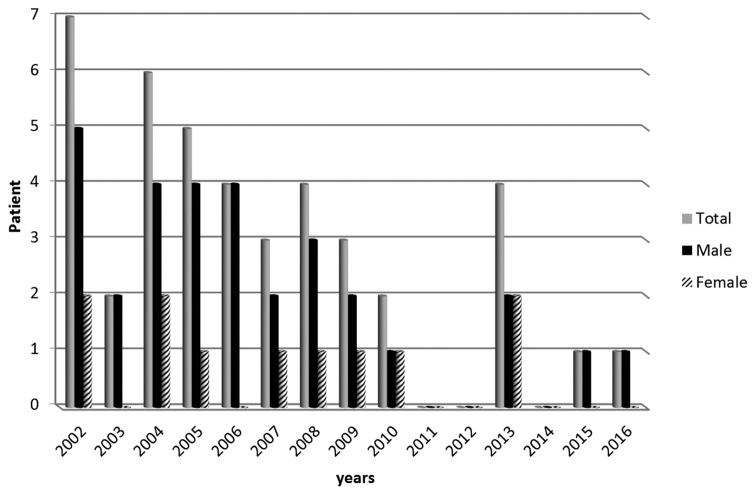
Forty-two new leprosy cases were identified within 15 years (2002-2016). Thirty-one patients (73.7%) were men and 11 (26.3%) were women. figure 1 shows total and the number of leprosy cases reported from 2002 to2016 based on sex. All patients were older than 20. Twenty patients aged between 20 and 40, 11 of them between 40 and 60 and 11 patients were older than 60. Twenty-eight of the cases (66.7%) were from Iran while 14 (33.3%) were from Afghanistan. According to WHO protocol, 36 (85.7%) patients were infected with Multi Bacillary form. The rest of them (6, 14.3%) were infected with Pauci Bacillary form. Among those patients, 61.9%, 19.05%, and 19.05% suffered from grade 1, 0 and 2 of the disease, respectively. Correlations between disability grading, type of leprosy (Multi Bacillary and Pauci Bacillary leprosy), and sex are demonstrated in Table 1.
Figure1.
The figure shows frequency of new leprosy cases reported during 2002 and 2016 among different sexes.
Table 1.
Relation of disability grading with sex and types of leprosy (Multi Bacillary and Pauci Bacillary leprosy)
| Sex | Type of leprosy | |||
|---|---|---|---|---|
| Male | Female | Multi Bacillary | Pauci Bacillary | |
| Disability | 7 | 1 | 6 | 2 |
| Grade0 | ||||
| Graed1 | 21 | 5 | 23 | 3 |
| Grade2 | 3 | 5 | 7 | 1 |
| Total in group | 31 | 11 | 36 | 6 |
| Total | 42 | 42 | ||
The analysis of data was performed using version 21 SPSS software. There was a significant relationship between disability grading and sex (P=0.032), with grade 1 disability happening more often in men. Another significant relationship was observed between Multi Bacillary form and nationality (P=0.011) indicating that Multi Bacillary form is more common among Iranians. No significant relationship was found between the type of leprosy and disability grading.
Discussion
Our results suggest that among all the patients considered in this study, 73.7% were men and 26.3% were women which is in agreement with the results of two other studies carried out in Azerbaijan, Iran, with 69% and 68% male patients, and another study performed in Kurdistan, Iran, with 64.4% male patients.11-13 Among those newly affected leprosy cases, women have hold a variable percentage changing from 6.50% in Ethiopia to 59.11% in Central Africa. Leprosy is usually more common in men than women. Different studies reported a higher number of male leprosy patients in Brazil, Canada, India, Philippines, Nepal, Hawaii, Venezuela, Cameroon, Ethiopia, and Iran.14-16 One likely assumption about why the disease is more common in men is that testosterone can facilitate bacterial growth and increase the load of bacteria in men.15
In the present study, 36 (85.7%) patients were infected with Multi Bacillary form while the rest (6, 14.3%) suffered from Pauci Bacillary form. This is similar to the results of another study performed in Kurdistan province, Iran, in which 70% of patients were infected with Multi Bacillary form. The percent of patients with Multi Bacillary leprosy who have been recently affected by it has differed from 32.7% in Comoros in Africa to 95.04% in the Philippines. Multi Bacillary leprosy is more common in Asia whereas Pauci Bacillary leprosy is more dominant in Africa.13,14
Our results showed that 34 (81%) patients were diagnosed with a grade of disability. Rad et al. reported 154 (84%) leprous patients with disability in Kurdistan, Iran.13 Among patients, 61.9% of them showed grade 1 disability and the percent of patients with grades 0 and 2 disability was equal to 19.05%. The proportion of Grade 2 disability in leprosy patients has ranged from 1.45% in Liberia to 22.8% in China.14 Disabilities can be prevented by early diagnosis and multiple drug therapy (MDT) which consists of dapsone, rifampicin, and clofazimine.8,13
In this study, 16.6% (6/36) of patients with multi Bacillary form suffered from grade 0 disability, 63.8% (23/36) from grade 1, and 19.5% (7.36) from grade 2 disability. It has been reported that in Kurdistan, Iran, 18.3% patients with multi bacillary leprosy had grade 0 disability, 34.1% suffered from grade 1 and 47.6% from grade 2 disability. It seems that early diagnosis and proper treatment has made grade 2 diability among patients in Khorasan to become less prevalent compared to Kurdistan.13
Leprosy is an ancient disease the threat of which to human health still exists. To control and avoid the disease, it is essential to identify its endemic spots. Therefore, a brief introduction to leprosy endemic regions is vital to reach such goal. Based on WHO reports, Bangladesh, Brazil, China, Congo, India, Ethiopia, Indonesia, Madagascar, Mozambique, Myanmar, Nepal, Nigeria, The Philippines, Sri Lanka, Sudan, and the United Republic of Tanzania are the most common endemic regions for leprosy. The highest incidence rate of infection was reported in India (126913 new cases), and then 31044 and 16856 new cases were reported from Brazil and Indonesia, respectively. 3 countries including India, Brazil, and Indonesia are the regions where leprosy is most prevalent by approximately having 81% of newly identified leprosy patients every year worldwide.6
Different studies have been performed to determine the status of leprosy in Iran within the past few years. Several studies were carried out in Tabriz, Shiraz, and Bandar Abbas during 1960-1970. The number of patients diagnosed with leprosy in Iran was 12000 in 1964, 4852 in 1965, and 450 in 1970.8 The majority of newly affected Iranian patients with leprosy have lived in East Azerbaijan, Gilan, West Azerbaijan, Khorasan, Kurdistan, and Kermanshah provinces whereas several provinces of Iran have been totally leprosy-free including Hamadan, Chahar Mahal Bakhtiari, Khuzestan, Isfahan, Semnan, and Kerman.8 The most important reason for carrying out this study is that Khorasan was the 4th main site of leprosy in Iran. In our study, 42 new leprosy cases were investigated in the Northeast of Iran during 2002-2016.
In order to effectively eliminate leprosy, diagnosis of the disease was done immediately, usually based on clinical findings. The diagnosis was confirmed after the patient was referred to a laboratory and additional tests were performed such as skin biopsy and slit skin. To decrease the transmission of leprosy via patients, early treatment was done by MDT method. Leprosy is an infectious disease and it is suggested that family members and neighbors of leprous patients must be screened because the bacteria has an average incubation period of three to five years with the possibility of even ranging from two to seven years.15,17
Conclusion
Although leprosy has become less prevalent within the recent decades, its eradication is yet to be achieved. The results of this study can be used to increase the efficacy of eradication programs in Iran albeit more studies are recommended to be performed in different parts of the country not only to get more data on the status of the disease in Iran but to orchestrate efficient controlling strategies against the disease and towards a leprosy-free society.
Acknowledgement
The authors would like to thank health care authorities for providing valuable information for this study.
Conflict of Interest:None declared.
References
- 1.Bratschi MW, Steinmann P, Wickenden A, Gillis TP. Current knowledge on Mycobacterium leprae transmission: a systematic literature review. Lepr Rev. 2015;86:142–55. [PubMed] [Google Scholar]
- 2.Entezarmahdi R, Majdzadeh R, Foroushani AR, Nasehi M, Lameei A, Naieni KH. Inequality of leprosy disability in iran, clinical or socio-economic inequality: an extended concentration index decomposition approach. Int J Prev Med. 2014;5:414–23. [ PMC Free Article] [PMC free article] [PubMed] [Google Scholar]
- 3.Martinez AN, Talhari C, Moraes MO, Talhari S. PCR-based techniques for leprosy diagnosis: from the laboratory to the clinic. PLoS Negl Trop Dis. 2014;8:e2655. doi: 10.1371/journal.pntd.0002655. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Monot M, Honore N, Garnier T, Zidane N, Sherafi D, Paniz-Mondolfi A, et al. Comparative genomic and phylogeographic analysis of Mycobacterium leprae. Nat Genet. 2009;41:1282–9. doi: 10.1038/ng.477. [DOI] [PubMed] [Google Scholar]
- 5.De Souza VTC, Junior W, De Jesus AMR, De Oliveira DT, Raptis HA, De Freitas PHL, et al. Is the WHO disability grading system for leprosy related to the level of functional activity and social participation? Lepr Rev. 2016;8:191–200. [PubMed] [Google Scholar]
- 6.Noriega LF, Chiacchio ND, Noriega AF, Pereira GA, Vieira ML. Leprosy: ancient disease remains a public health problem nowadays. An Bras Dermatol. 2016;91:547–8. doi: 10.1590/abd1806-4841.20164861. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Strategy GL. Strategy 2016–2020 Accelerating towards a leprosy free-world. WHO SEARO/Department of Control of Neglected Tropical Diseases, New Delhi. 2016 [Google Scholar]
- 8.Azizi MH, Bahadori M. A history of leprosy in Iran during the 19th and 20th centuries. Arch Iran Med. 2011;14:425–30. [PubMed] [Google Scholar]
- 9.Nasseri K, Ko YH. Epidemiology of leprosy in Iran. Int J Lepr Other Mycobact Dis. 1977;45:355–9. [PubMed] [Google Scholar]
- 10.Naveed T, Shaikh ZI, Anwar MI. Diagnostic accuracy of slit skin smears in leprosy. Pakistan Armed Forces Medical Journal. 2015;65:649–52. [Google Scholar]
- 11.Golforoushan F, Razi A, Azimi H, Herischi H. Review of ten-yrs leprosy cases in Azerbaijan, Northwest of Iran. Iran J Med Sci. 2006;31:103–5. [Google Scholar]
- 12.Golfurushan F, Sadeghi M, Goldust M, Yosefi N. Leprosy in Iran: an analysis of 195 cases from 1994-2009. J Pak Med Assoc. 2011;61:558–61. [PubMed] [Google Scholar]
- 13.Rad F, Ghaderi E, Moradi G, Salimzadeh H. The study of disability status of live leprosy patients in Kurdistan province of Iran. Pak J Med Sci. 2007;23:857–861. [Google Scholar]
- 14.Suzuki K, Akama T, Kawashima A, Yoshihara A, Yotsu RR, Ishii N. Current status of leprosy: epidemiology, basic science and clinical perspectives. J Dermatol. 2012;39:121–9. doi: 10.1111/j.1346-8138.2011.01370.x. [DOI] [PubMed] [Google Scholar]
- 15.Nobre ML, Illarramendi X, Dupnik KM, Hacker MA, Nery JA, Jeronimo SM, et al. Multibacillary leprosy by population groups in Brazil: Lessons from an observational study. PLoS Negl Trop Dis. 2017;11:e0005364. doi: 10.1371/journal.pntd.0005364. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ramos JM, Martinez-Martin M, Reyes F, Lemma D, Belinchon I, Gutierrez F. Gender differential on characteristics and outcome of leprosy patients admitted to a long-term care rural hospital in South-Eastern Ethiopia. Int J Equity Health. 2012;11:56. doi: 10.1186/1475-9276-11-56. [ PMC Free Article] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Davoodian P, Dadvand H, Raz-Nahan M, Baghestani S, Mahbubi A, Bageri A. Case finding survey for leprosy in Iran: Bandar Abbas and Minab. Lepr Rev. 2009;80:441–4. [PubMed] [Google Scholar]