Abstract
Objectives:
Broad-spectrum antibiotics are frequently prescribed for children with upper respiratory tract infections (URI). Excessive use of broad-spectrum antibiotics leads to the emergence of resistant bacteria. This study aimed to identify factors associated with prescribing broad-spectrum antibiotics among children younger than 18 years presenting with URI in outpatient settings.
Methods:
We conducted a cross-sectional analysis of the National Ambulatory Medical Care Survey (NAMCS) and the National Hospital Ambulatory Medical Care Survey-Outpatient Departments (NHAMCS-OPD) between 2006 and 2010. Descriptive statistics of visits from children with URI were estimated. Simple and multiple logistic regression analyses were used to identify socio-demographic and clinical characteristics associated with broad-spectrum antibiotic prescribing. We also completed a stratified analysis by age (⩽2 vs >2).
Results:
A total of 4013 outpatient visits for children with URI from both NAMCS and NHAMCS-0PD data were examined. Broad-spectrum antibiotics were prescribed in 39% of the visits, accounting for an estimated 6.8 million visits annually. Multivariable analysis showed that visits in the South region (odds ratio [OR] = 2.38; 95% confidence interval [CI]: 1.38-4.10) compared with the West region and visits with diagnoses of acute sinusitis (OR = 2.77; 95% CI: 1.65-4.63) and acute otitis media (OR = 1.90; 95% CI: 1.32-2.74) compared with those with acute pharyngitis were associated with greater odds of broad-spectrum antibiotic prescribing.
Conclusions:
The prescribing of broad-spectrum antibiotics is common for children with URI in ambulatory care settings. Diagnosis and management of URI remain a critical area for awareness campaigns promoting judicious use of antibiotics.
Keywords: Antibiotics, respiratory tract infections, pediatrics, prescribing patterns
Introduction
Antibiotics are among the most common drugs prescribed to children in ambulatory care settings.1 Upper respiratory tract infections (URIs) account for more than 70% of pediatric outpatient visits in which antibiotics are prescribed.2,3 Upper respiratory tract infections are multiple diseases characterized by inflammation of the upper part of the respiratory tract, including sinusitis, pharyngitis, otitis media, and rhinitis (common cold). In 2006, these conditions jointly were the most frequent acute diagnosis in the ambulatory care settings in the United States.4
Most types of URIs are not indications for antibiotics as they are usually caused by viruses.5 The use of antibiotics in viral URIs has been declining, whereas the inappropriate use of antibiotics for bacterial URI has increased.2,6–8 Increased broad-spectrum antibiotic use in conditions that should be treated by narrow-spectrum antibiotics warrants great concern.1 Excessive and inappropriate use of broad-spectrum antibiotics leads to the development of new resistant strains of microorganisms.9 Therefore, it is especially significant to avoid antibiotic misuse in children as they represent a large reservoir for resistant bacteria.10
The dramatic increase in the prevalence of antimicrobial-resistant pathogens represents a public health threat that has gained attention from several national organizations. The Centers for Disease Control and Prevention (CDC) has led substantial efforts to raise awareness about antibiotic use and resistance. In the early 2000s, CDC launched a campaign, known as “Get Smart,” aimed to reduce antibiotic resistance by, in part, encouraging providers to adhere to appropriate prescribing guidelines.3 Along with the national efforts to promote appropriate prescribing behaviors, it is important to capture the patterns of broad-spectrum antibiotics prescribing and identify the factors associated with it. Previous studies suggested a substantial increase in the use of broad-spectrum antibiotics during the past 2 decades.6,10–12 However, few studies were conducted to identify factors associated with prescribing broad-spectrum antibiotics for children with URI among ambulatory care settings.2,10 In this study, we sought to describe the patterns of prescribing broad-spectrum antibiotics for children with URI on a national level. In addition, we sought to comprehensively evaluate factors associated with broad-spectrum antibiotic prescribing during pediatric outpatient visits, aiming to better inform where future efforts for judicious use of antibiotics may be needed.
Methods
Study design and data source
This was a cross-sectional study design of publicly available data from the National Ambulatory Medical Care Survey (NAMCS) and the National Hospital Ambulatory Medical Care Survey (NHAMCS) between 2006 and 2010. These 2 national surveys are conducted annually by the National Center for Health Statistics.13 The NAMCS samples visit to physician offices, whereas the NHAMCS samples visits to hospital outpatient departments (OPD) and emergency departments (ED). These surveys use multistage stratified probability sampling so nationally representative estimates can be formed from the data generated.13 The focus of this study is only on office-based and hospital-based outpatient visits so ED visits are not included. When taken together, these surveys can be incorporated to produce nationally representative samples of ambulatory care visits.
The NAMCS uses a 3-stage probability sampling method to capture data on visits to nonfederal employed office-based physicians.13 The first stage of sampling is the selection of 112 primary sampling units (PSUs). Within each of the 112 PSUs, physician practices are stratified and randomly assigned to a 1-week reporting period. The final stage is a systematic random sample of visits to the assigned practices. The NHAMCS, on the other hand, is a 4-stage probability sampling of ambulatory visits made to nonfederal short-stay hospitals located in the 50 states and the District of Columbia.13 The survey consists of 2 components: OPD component and ED component. The first stage of sampling comprises 112 geographic PSUs. Second stage is sampling of hospitals within PSUs. In the third stage, clinics within OPD in addition to emergency services are selected, and in the final stage, patient visits to these settings are sampled. The survey is a 4-week reporting period, during which the assigned physicians collect data for visits.
Data collected for NHAMCS are nearly identical for NAMCS, with some differences for ED component. Data in both surveys are recorded by physicians. The information collected in these surveys include patients’ demographic characteristics, symptoms, diagnoses, medications prescribed, and other practice related variables. Both NAMCS and NHAMCS collect data on up to 3 unique diagnoses and up to 8 medications prescribed for each visit. Also, information on diagnostic procedures, insurance type, and providers’ specialty are collected as well.
Study population and identification of URI-related visits
Ambulatory care visits made by children aged 6 months to less than 18 years between 2006 and 2010 were eligible for inclusion in the study. During this period, visits of children diagnosed with URI were identified from NAMCS and NHAMCS-OPD components. In both data sets, up to 3 distinct diagnoses were made for each visit in accordance with criteria from the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). Acute bacterial conditions of URI, for which narrow-spectrum antibiotics are the first-line therapy according to the clinical practice guidelines,14 were included in this study. These conditions are acute otitis media (ICD-9-CM: 381-382), acute sinusitis (ICD-9-CM: 461), and acute pharyngitis (ICD-9-CM: 034, 462-463). Chronic types of URI, such as chronic bronchitis and chronic sinusitis, were excluded from the study because these conditions are usually complicated, and narrow-spectrum antibiotics are not typically indicated for their treatment.14 For the same reason, visits that were coded as a chronic problem, using the “major reason for this visit” item on the survey, were excluded from the study as well. As antibiotics are not beneficial in viral URIs,14 visits with viral URI diagnoses were excluded from the study. Infants less than 6 months of age were not included in the study because at this age, the guidelines recommendations differ considerably from older children.14
Outcome measurement
The outcome of interest in our study was the utilization of broad-spectrum antibiotics for URI diagnoses within pediatric ambulatory care settings from 2006 to 2010. Factors associated with prescribing broad-spectrum antibiotics were identified using a binary outcome. The outcome was coded as whether a broad-spectrum antibiotic was prescribed or not (ie, yes versus no). Starting in 2006, the NAMCS and NHAMCS incorporated Multum Lexicon system to classify medications.15 The Multum Lexicon is a comprehensive database that includes all prescription drugs available in the US market.16 Under this system, medications are coded based on their generic components and therapeutic classes. There are 3 levels of therapeutic classes. Using Multum therapeutic category level 1 of anti-infective, relevant antibiotics were identified. Broad-spectrum antibiotics were defined to encompass amoxicillin-clavulanate, second- and third-generation cephalosporins, and macrolides.
Covariates
Physician and patient characteristics were considered for the analysis. Patient age was divided into 3 categories: <2 years, 2 to <6 years, and 6 to <18 years. Race was categorized as white, black, and other. Geographic regions included Northeast, Midwest, South, and West. Insurance type was categorized as private, public, and self-pay/other. Metropolitan statistical area (MSA) was coded as MSA and non-MSA. Physician specialty was recoded into family doctor, pediatrician, and other. Setting type categorized as physician office (NAMCS) and hospital outpatient department (NHAMCS-OPD) was also considered in our study. Because severe symptoms might influence physician’s decision, visits in which fever (ie, temperature ⩾100.4°F) was recorded were identified and considered for analysis.
Statistical analysis
Descriptive analysis of demographic and clinical characteristics of ambulatory care visits over the 5-year study period was conducted. Patient visits’ weights were used in providing national estimates. Simple and multiple logistic regressions were used to identify factors associated with prescribing broad-spectrum antibiotic. A simple binary logistic regression was performed for each of the covariates to evaluate association with broad-spectrum antibiotic prescribing. Factors that were nominally associated with the outcome (P < .25) were used in the multivariate model. These variables were further evaluated in the multiple regression analysis. The URI-specific diagnosis and fever were included in the final model regardless of their bivariable association with the outcome. We also conducted a multivariable stratified analysis where all factors were further evaluated among those 2 years or younger versus those older than 2 years. A P value of less than .05 (2-tailed) was considered statistically significant. All statistical analyses were conducted using SAS software version 9.4.
Results
Patterns of broad-spectrum antibiotic prescribing
A total of 4013 outpatient visits for children with URI from both NAMCS and NHAMCS-0PD data were included. Of them, 46% were visits from persons younger than 2 years. Most of the study visits were from patients who were white (85.6%), had private insurance (63.6%), and were diagnosed with acute otitis media (71.5%) (Table 1). Over the 5-year study period, 39% of the children with URIs received prescriptions for broad-spectrum antibiotics that represent an estimated average of 6.8 million visits annually. Visits in which broad-spectrum antibiotics were dispensed occurred most commonly among children <2 years (3.5 million visits), those with private insurance (4.5 million visits), and visits from patients with acute otitis media (5.2 million visits) (Table 1). Broad-spectrum antibiotics were frequently prescribed for patients <2 years with URI, accounting for 43% of all visits made by this age group (Table 1). Other characteristics with high frequency of prescribing broad-spectrum antibiotics included visits in the South (47%) and visits from patients with acute sinusitis (46.6%).
Table 1.
Demographic and clinical characteristics of the pediatric visits with URI, from 2006 to 2010.
| Characteristic | Proportion of visits, % (N = 4013) | Estimated annual visits with a BSA prescription (in millions) | Percentage of visits with a BSA prescriptiona, % |
|---|---|---|---|
| Age, y | |||
| <2 | 46.4 | 3.5 | 43.0 |
| 2 to <6 | 26.1 | 1.8 | 39.6 |
| 6 to <18 | 27.5 | 1.5 | 32.2 |
| Gender | |||
| Male | 51.4 | 3.6 | 40.2 |
| Female | 48.6 | 3.2 | 38.0 |
| Race | |||
| White | 85.6 | 5.9 | 39.7 |
| Black | 10.1 | 0.7 | 39.5 |
| Other | 4.3 | 0.2 | 27.7 |
| Region | |||
| Northeast | 15.4 | 0.9 | 33.4 |
| Midwest | 22.7 | 1.4 | 35.7 |
| South | 42.9 | 3.5 | 46.9 |
| West | 18.9 | 0.9 | 30.1 |
| MSA status | |||
| MSA | 86.4 | 5.9 | 39.7 |
| Non-MSA | 13.6 | 0.8 | 35.8 |
| Setting type | |||
| Physician office | 89.2 | 6.2 | 39.6 |
| Hospital outpatient | 10.8 | 0.6 | 35.1 |
| Physician specialty | |||
| General/family doctor | 24.5 | 1.5 | 35.7 |
| Pediatrician | 63.8 | 4.7 | 42.6 |
| Other | 11.7 | 0.6 | 27.7 |
| Insurance typeb | |||
| Public | 31.6 | 0.2 | 28.7 |
| Private | 63.6 | 4.5 | 41.6 |
| Self-pay/other | 4.8 | 1.9 | 35.7 |
| Feverc | |||
| Yes | 50.5 | 1.8 | 39.0 |
| No | 49.5 | 1.9 | 41.7 |
| URI-specific diagnosis | |||
| Acute otitis media | 71.5 | 5.2 | 41.4 |
| Acute sinusitis | 9.9 | 0.8 | 46.6 |
| Acute pharyngitis | 18.6 | 0.9 | 26.5 |
Abbreviations: BSA, broad-spectrum antibiotic; MSA, metropolitan statistical area; URI, upper respiratory tract infection.
As a percentage of the total number of visits within individual characteristics.
About 2% of visits were missing information about method of payment (N = 3916).
Body temperature was not recorded in 1822 visits (N = 2191).
Prescribing of broad-spectrum antibiotics increased from 39.5% of visits in 2006 to 45.8% of visits in 2008 but then dropped to 33% of visits in 2010 (Figure 1). This favorable overall reduction was attributable mainly to a substantial decrease in the prescribing of macrolides by more than half from about 700 000 visits in 2006 to nearly 300 000 visits in 2010 (Figure 2). Also, the prescribing of amoxicillin-clavulanate and second/third-generation cephalosporins decreased between 2006 and 2010 by about 40% and 20%, respectively. Over the 5-year study period, the most commonly prescribed antibiotic class was second/third-generation cephalosporins, comprising 39% of all visits in which broad-spectrum antibiotics were prescribed.
Figure 1.
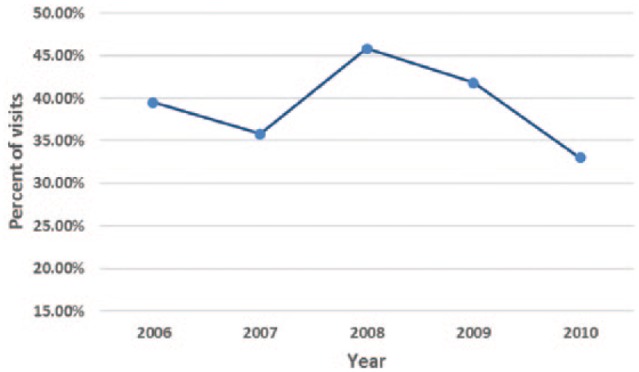
Trends in prescribing broad-spectrum antibiotics in outpatient visits for children with URI between 2006 and 2010.
Figure 2.
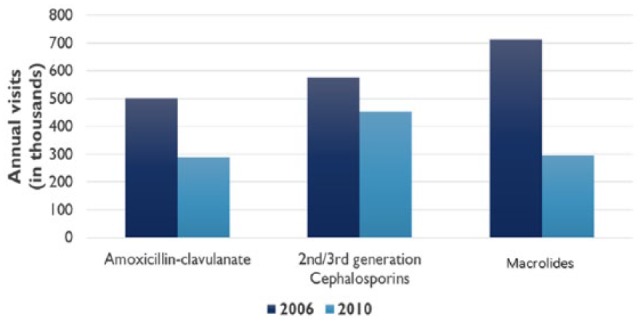
Change in prescribing broad-spectrum antibiotics between 2006 and 2010 by class of antibiotics.
Factors associated with broad-spectrum antibiotic prescribing
Table 2 shows an association between demographic and clinical factors and broad-spectrum antibiotic prescribing. The variables that were associated with the use of broad-spectrum antibiotics in the bivariable analysis were age groups, region, physician specialty, insurance type, and URI-specific diagnosis (P < .05). The odds of patients aged 6 to <18 years to receive broad-spectrum antibiotics were nearly 40% lower compared with patients younger than 2 years (unadjusted odds ratio [OR]: 0.63; 95% confidence interval [CI]: 0.47-0.84). Visits in the South were about 2 times more likely to result in a broad-spectrum antibiotic prescription than those visits in the West (unadjusted OR: 2.06; 95% CI: 1.42-2.98). General/family physicians (unadjusted OR: 0.75; 95% CI: 0.57-0.98) and other physician specialties (unadjusted OR: 0.52; 95% CI: 0.34-0.79) were less likely to prescribe broad-spectrum antibiotics than pediatricians. Likewise, visits with public insurance (unadjusted OR: 0.78; 95% CI: 0.61-0.99) and visits with self-pay/other (unadjusted OR: 0.56; 95% CI: 0.37-0.86) were less likely to result in a broad-spectrum antibiotic prescription than those with private insurance. Patients with acute otitis media (unadjusted OR: 1.96; 95% CI: 1.41-2.72) and those with acute sinusitis (unadjusted OR: 2.42; 95% CI: 1.47-3.95) were more likely to be prescribed broad-spectrum antibiotics compared with those with acute pharyngitis. Sex, race, MSA status, setting type, and fever were not significantly associated with broad-spectrum antibiotic prescribing according to the bivariable analysis (P > .05). Sex and MSA were excluded from the multivariable model because they were not nominally associated with the outcome (P > .25). Fever was predetermined to be entered into the multivariable model regardless of its nominal bivariable association with broad-spectrum antibiotic prescribing (P = .45).
Table 2.
Factors associated with prescribing broad-spectrum antibiotics for children with URI in outpatient visits.
| Factor | Bivariable association with prescribing BSA (P value) | Unadjusted OR (95% CI) | Adjusted OR (95% CI) |
|---|---|---|---|
| Age groups, y | .0021 | ||
| <2 | 1 | 1 | |
| 2 to <6 | 0.87 (0.67-1.12) | 1.17 (0.79-1.71) | |
| 6 to <18 | 0.63 (0.47-0.84) | 0.72 (0.49-1.07) | |
| Sex | .3541 | ||
| Male | 1 | * | |
| Female | 0.91 (0.75-1.11) | ||
| Race | .1112 | ||
| White | 1 | 1 | |
| Black | 0.99 (0.70-1.41) | 0.73 (0.41-1.30) | |
| Other | 0.58 (0.37-0.92) | 1.01 (0.51-2.03) | |
| Region | <.0001 | ||
| West | 1 | 1 | |
| Midwest | 1.29 (0.87-1.91) | 1.56 (0.91-2.67) | |
| Northeast | 1.16 (0.76-1.79) | 1.49 (0.77-2.91) | |
| South | 2.06 (1.42-2.98) | 2.38 (1.38-4.10) | |
| MSA status | .3610 | ||
| Non-MSA | 1 | * | |
| MSA | 1.18 (0.83-1.69) | ||
| Setting type | .2121 | ||
| NAMCS | 1 | 1 | |
| NHAMCS (OPD) | 0.83 (0.61-1.12) | 0.91 (0.64-1.28) | |
| Physician specialty | .0013 | ||
| Pediatrician | 1 | 1 | |
| General/family doctor | 0.75 (0.57-0.98) | 0.83 (0.59-1.15) | |
| Other | 0.52 (0.34-0.79) | 0.68 (0.42-1.09) | |
| Insurance type | .0094 | ||
| Private | 1 | 1 | |
| Public | 0.78 (0.61-0.99) | 0.76 (0.56-1.04) | |
| Self-pay/other | 0.56 (0.37-0.86) | 0.66 (0.38-1.15) | |
| Fever | .4464 | ||
| No | 1 | 1 | |
| Yes | 0.89 (0.67-1.19) | 0.99 (0.72-1.34) | |
| Diagnosis | <.0001 | ||
| Acute pharyngitis | 1 | 1 | |
| Acute otitis media | 1.96 (1.41-2.72) | 1.90 (1.32-2.74) | |
| Acute sinusitis | 2.42 (1.47-3.95) | 2.77 (1.65-4.63) |
Abbreviations: CI, confidence interval; MSA, Metropolitan Statistical Area; OR, odds ratio; URI, upper respiratory tract infection.
Not entered into the multivariable model.
The multivariable model showed visits in the South compared with those in the West (adjusted OR: 2.38; 95% CI: 1.38-4.10) to be a significant predictor of prescribing broad-spectrum antibiotics. Visits for acute otitis media (adjusted OR: 1.90; 95% CI: 1.32-2.74) and visits for acute sinusitis (adjusted OR: 2.77; 95% CI: 1.65-4.63) compared with those for acute pharyngitis were also significant predictors of prescribing broad-spectrum antibiotics (Table 2). Age, physician specialty, and type of insurance were no longer significantly associated with broad-spectrum antibiotic prescribing in the multivariable model.
In the multivariable stratified analysis, we found that visits for acute sinusitis among patients 2 years or younger were much more likely to result in a broad-spectrum antibiotic prescription compared with visits for acute pharyngitis (adjusted OR: 3.55; 95% CI: 1.26-9.98) (Table 3). Among visits from patients older than 2 years, we found that sex, race, region, and URI-specific diagnosis were independently associated with broad-spectrum antibiotic prescribing (Table 3). In this age group, women compared with men (adjusted OR: 0.60; 95% CI: 0.39-0.93) and black compared with white (adjusted OR: 0.38; 95% CI: 0.15-0.93) were less likely to receive broad-spectrum antibiotics. In addition, we found that visits in the South compared with those in the West (adjusted OR: 3.95; 95% CI: 2.09-7.47), visits for acute otitis media compared with those for acute pharyngitis (adjusted OR: 2.18; 95% CI: 1.35-3.53), and visits for acute sinusitis compared with those for acute pharyngitis (adjusted OR: 2.29; 95% CI: 1.12-4.73) were more likely to result in a broad-spectrum antibiotic prescription.
Table 3.
Multivariable stratified analysis by age (⩽2 vs >2).
| Factor | ⩽2 y |
>2 y |
||
|---|---|---|---|---|
| Adjusted OR | 95% CI | Adjusted OR | 95% CI | |
| Femalea | 1.36 | 0.92-2.03 | 0.60 | 0.39-0.93 |
| Fever (yes) | 1.07 | 0.69-1.64 | 1.01 | 0.65-1.55 |
| Race | ||||
| White | 1 | 1 | 1 | 1 |
| Blacka | 0.96 | 0.49-1.89 | 0.38 | 0.15-0.93 |
| Other | 0.61 | 0.24-1.59 | 1.66 | 0.69-3.99 |
| Physician specialty | ||||
| Pediatrician | 1 | 1 | 1 | 1 |
| General/family doctor | 0.65 | 0.40-1.07 | 0.90 | 0.57-1.43 |
| Other specialties | 0.65 | 0.35-1.21 | 0.51 | 0.09-2.78 |
| Insurance type | ||||
| Private | 1 | 1 | ||
| Public | 0.87 | 0.54-1.39 | 0.64 | 0.39-1.03 |
| Self-pay/other | 0.62 | 0.29-1.29 | 0.66 | 0.28-1.57 |
| Region | ||||
| West | 1 | 1 | 1 | 1 |
| Midwest | 1.78 | 0.85-3.73 | 1.41 | 0.69-2.89 |
| Northeast | 1.06 | 0.44-2.58 | 1.72 | 0.76-3.89 |
| Southa | 1.56 | 0.72-3.35 | 3.95 | 2.09-7.47 |
| Setting type (NAMCS vs NHAMCS-OPD) | 1.27 | 0.82-1.97 | 0.90 | 0.55-1.48 |
| MSA status (MSA vs non-MSA) | 0.92 | 0.58-1.46 | 0.86 | 0.43-1.71 |
| Diagnosis | ||||
| Acute pharyngitis | 1 | 1 | 1 | 1 |
| Acute otitis mediaa | 2.12 | 0.84-5.30 | 2.18 | 1.35-3.53 |
| Acute sinusitisb | 3.55 | 1.26-9.98 | 2.29 | 1.12-4.73 |
Abbreviations: CI, confidence interval; MSA, Metropolitan Statistical Area; OR, odds ratio.
Independently associated with broad-spectrum antibiotic prescribing among >2 years.
Independently associated with broad-spectrum antibiotic prescribing in both age groups.
Discussion
In this study, we examined the use of broad-spectrum antibiotics for children with URI during ambulatory care visits using a nationally representative data set. From 2006 to 2010, we found that the prescribing of broad-spectrum antibiotics for children with URI was very common in the US ambulatory care settings, ranging from 33% to 45.8% of visits (Figure 1). Acute otitis media was the primary driver of broad-spectrum antibiotic prescribing, with an estimated average of 5.2 million visits annually. We found that 41.2% of all pediatric patient visits for acute otitis media resulted in a prescription for a broad-spectrum antibiotic (Table 1). A previous study between 1998 and 2004 also reported that about 41% of acute otitis media patients received a broad-spectrum antibiotic.10 These results indicate that continuing education programs about the diagnosis and management of acute otitis media remain a critical area for promoting judicious use of antibiotics. Although acute sinusitis was not as common as acute otitis media, we found that broad-spectrum antibiotics were prescribed in nearly 47% of all visits for acute sinusitis. Furthermore, the multivariable analysis showed that visits for acute sinusitis as well as those for acute otitis media had increased odds of receiving broad-spectrum antibiotics compared with visits for acute pharyngitis. Streptococcus pneumoniae is the leading cause of both acute otitis media and acute sinusitis in the United States.8,17 The American Academy of Pediatrics (AAP) clinical practice guidelines recommend amoxicillin as the first-line therapy for most uncomplicated cases of both infections.18,19 In addition, a recent study by Gerber et al20 found that treatment with broad-spectrum antibiotics was not associated with better clinical outcomes in children with URI when compared with treatment with narrow-spectrum antibiotics.
Our findings showed an encouraging downward trend in the use of broad-spectrum antibiotics, especially between 2008 and 2010 (Figure 1). Several studies have reported substantial increases in the use of macrolides for pediatric patients during the past decade.2,8,10,12,21 In contrast to previous studies, we found that the prescribing of macrolides decreased by more than half between 2006 and 2010 (Figure 2). Likewise, prescriptions for amoxicillin-clavulanate decreased between 2006 and 2010 by about 40% despite the fact that visits for URI remained steady over the study period. Second/third-generation cephalosporins were the most commonly prescribed broad-spectrum antibiotics for children with URI in our study. Results from a recent study showed increases in the use of third-generation cephalosporins in 3 health plans between 2000 and 2010.22 Ultimately, any additional decline in broad-spectrum antibiotic dispensing rates will most likely be driven by better adherence to evidence-based clinical practice guidelines for diagnosis and management of these common childhood infections.
In this study, we explored the association between range of characteristics and broad-spectrum antibiotic prescribing. As previously mentioned, the multivariable analysis revealed that visits for acute otitis media and those for acute sinusitis were more likely to result in a broad-spectrum antibiotic prescription compared with visits for acute pharyngitis. In addition, we found that visits in the South were associated with higher rates of broad-spectrum antibiotic prescribing compared with visits in the West. Visits in the South were also found to be associated with higher rates of broad-spectrum antibiotic prescribing in previous studies.2,10 Although the explanation for this association is uncertain, higher prevalence of penicillin resistance among strains of S pneumoniae in the southeastern and southcentral regions23 could explain the higher rates of broad-spectrum antibiotic prescribing in the South. More studies to explore regional associations between broad-spectrum antibiotic prescribing and resistance trends are recommended. Our findings showed that fever was not a significant predictor of prescribing broad-spectrum antibiotics for children with URI. For visits made by children with urinary tract infections, however, Copp et al24 concluded that fever was a significant predictor of broad-spectrum antibiotic prescribing.
In the stratified analysis, we found that acute sinusitis was significantly associated with higher rates of broad-spectrum antibiotic prescribing in both age groups. A finding of interest in our study is that among visits from children older than 2 years, black patients were less likely to receive broad-spectrum antibiotics compared with white patients. A previous study that analyzed visits for acute otitis media from 1998 to 2004 has reported that non-white patients were less likely to receive broad-spectrum antibiotics than white patients.10 This finding may raise concerns about racial differences in the quality of care provided for children in outpatient visits.
There are several limitations in our study that need to be acknowledged. First, the NAMCS and NHAMCS data sets do not contain certain clinical factors that could have justified a provider’s choice of antibiotic. For example, we were unable to take into consideration allergy to penicillin, which is a reason not to prescribe amoxicillin. Second, diagnoses in the NAMCS and NHAMCS data sets are coded according to the ICD-9-CM, and therefore misclassification bias may occur. Finally, it is important to emphasize that multiple visits by the same individual is possible. However, as the reporting period in NAMCS is 1 week and in NHAMCS is 4 weeks, the likelihood of repeated visit by the same patient at a given practice is low.
Conclusions
In conclusion, the prescribing of broad-spectrum antibiotics is common for children with URI in ambulatory care settings, especially for children 24 months of age and younger. Efforts to decrease broad-spectrum antibiotics use should continue and focus more toward certain conditions and age groups. Diagnosis and management of URI in children remain a critical area for awareness programs promoting appropriate use of antibiotics.
Footnotes
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: All authors have contributed to this publication and hold themselves jointly and individually responsible for the content.
ORCID iD: Mohammad S Alzahrani  https://orcid.org/0000-0001-9028-9415
https://orcid.org/0000-0001-9028-9415
References
- 1. Chai G, Governale L, McMahon AW, et al. Trends of outpatient prescription drug utilization in US children, 2002-2010. Pediatrics. 2012;130:23–31. doi: 10.1542/peds.2011-2879. [DOI] [PubMed] [Google Scholar]
- 2. Hersh AL, Shapiro DJ, Pavia AT, et al. Antibiotic prescribing in ambulatory pediatrics in the United States. Pediatrics. 2011;128:1053–1061. doi: 10.1542/peds.2011-1337. [DOI] [PubMed] [Google Scholar]
- 3. Centers for Disease Control and Prevention. Get smart campaign. http://www.cdc.gov/getsmart/campaign-materials/about-campaign.html. Published 2013. Accessed May 2, 2015.
- 4. Cherry DK, Hing E, Woodwell DA, et al. National Ambulatory Medical Care Survey: 2006 summary. Natl Health Stat Report. 2008;3:1–39. [PubMed] [Google Scholar]
- 5. Hersh AL, Jackson MA, Hicks LA, et al. Principles of judicious antibiotic prescribing for upper respiratory tract infections in pediatrics. Pediatrics. 2013;132:1146–1154. doi: 10.1542/peds.2013-3260. [DOI] [PubMed] [Google Scholar]
- 6. Grijalva CG, Nuorti JP, Griffin MR. Antibiotic prescription rates for acute respiratory tract infections in US ambulatory settings. JAMA. 2009;302:758–766. doi: 10.1001/jama.2009.1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mainous AG, 3rd, Hueston WJ, Davis MP, et al. Trends in antimicrobial prescribing for bronchitis and upper respiratory infections among adults and children. Am J Public Health. 2003;93:1910–1914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Shapiro DJ, Gonzales R, Cabana MD, et al. National trends in visit rates and antibiotic prescribing for children with acute sinusitis. Pediatrics. 2011;127:28–34. doi: 10.1542/peds.2010-1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Goossens H, Ferech M, Stichele R, et al. Outpatient antibiotic use in Europe and association with resistance: a cross-national database study. Lancet. 2005;365:579–587. doi:S0140-6736(05)17907-0. [DOI] [PubMed] [Google Scholar]
- 10. Coco AS, Horst MA, Gambler AS. Trends in broad-spectrum antibiotic prescribing for children with acute otitis media in the United States, 1998-2004. BMC Pediatr. 2009;9:41. doi: 10.1186/1471-2431-9-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Steinman MA, Gonzales R, Linder JA, et al. Changing use of antibiotics in community-based outpatient practice, 1991-1999. Ann Intern Med. 2003;138:525–533. doi: 10.7326/0003-4819-138-7-200304010-00008. [DOI] [PubMed] [Google Scholar]
- 12. Stille CJ, Andrade SE, Huang SS, et al. Increased use of second-generation macrolide antibiotics for children in nine health plans in the United States. Pediatrics. 2004;114:1206–1211. doi: 10.1542/peds.2004-0311. [DOI] [PubMed] [Google Scholar]
- 13. Centers for Disease Control and Prevention. About the ambulatory health care surveys. https://www.cdc.gov/nchs/ahcd/about_ahcd.htm. Published 2009. Accessed January 1, 2015.
- 14. Wong DM, Blumberg DA, Lowe LG. Guidelines for the use of antibiotics in acute upper respiratory tract infections. Am Fam Physician. 2006;74:956–966. [PubMed] [Google Scholar]
- 15. Centers for Disease Control and Prevention. Trend analysis using NAMCS and NHAMCS drug data. http://www.cdc.gov/nchs/ahcd/trend_analysis.htm. Updated 2010. Accessed January 1, 2015.
- 16. Centers for Disease Control and Prevention. The new ambulatory care drug database system. http://www2.cdc.gov/drugs/applicationnav1.asp. Updated 2012. Accessed January 1, 2015.
- 17. Centers for Disease Control and Prevention. Geographic variation in penicillin resistance in Streptococcus pneumonia-selected sites, United States, 1997. MMWR Morb Mortal Wkly Rep. 1999;48:656–661. http://www.ncbi.nlm.nih.gov/pubmed/10488781. Accessed April 30, 2017. [PubMed] [Google Scholar]
- 18. American Academy of Pediatrics. Diagnosis and management of acute otitis media. Pediatrics. 2004;113 http://pediatrics.aappublications.org/content/113/5/1451. [DOI] [PubMed] [Google Scholar]
- 19. American Academy of Pediatrics. Subcommittee on management of sinusitis and committee on quality improvement. Clinical Practice guideline: management of sinusitis. Pediatrics. 2001;108:798–808. http://www.ncbi.nlm.nih.gov/pubmed/11533355. Accessed April 30, 2017. [DOI] [PubMed] [Google Scholar]
- 20. Gerber JS, Ross RK, Bryan M, et al. Association of broad- vs narrow-spectrum antibiotics with treatment failure, adverse events, and quality of life in children with acute respiratory tract infections. JAMA. 2017;318:2325–2336. doi: 10.1001/jama.2017.18715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Halasa NB, Griffin MR, Zhu Y, et al. Decreased number of antibiotic prescriptions in office-based settings from 1993 to 1999 in children less than five years of age. Pediatr Infect Dis J. 2002;21:1023–1028. doi: 10.1097/01.inf.0000036085.65178.e1. [DOI] [PubMed] [Google Scholar]
- 22. Vaz LE, Kleinman KP, Raebel MA, et al. Recent trends in outpatient antibiotic use in children. Pediatrics. 2014;133:375–385. http://pediatrics.aappublications.org/content/133/3/375. Accessed May 1, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Doern GV, Brown SD. Antimicrobial susceptibility among community-acquired respiratory tract pathogens in the USA: data from PROTEKT US 2000-01. J Infect. 2004;48:56–65. http://www.ncbi.nlm.nih.gov/pubmed/14667792. Accessed March 13, 2018. [DOI] [PubMed] [Google Scholar]
- 24. Copp HL, Shapiro DJ, Hersh AL. National ambulatory antibiotic prescribing patterns for pediatric urinary tract infection, 1998-2007. Pediatrics. 2011;127:1027–1033. doi: 10.1542/peds.2010-3465. [DOI] [PMC free article] [PubMed] [Google Scholar]


