Abstract
Objectives:
Social determinants of health (SDHs) are the complex, structural, and societal factors that are responsible for most health inequities. Since 2003, the National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention (NCHHSTP) has researched how SDHs place communities at risk for communicable diseases and poor adolescent health. We described the frequency and types of SDHs discussed in articles authored by NCHHSTP.
Methods:
We used the MEDLINE/PubMed search engine to systematically review the frequency and type of SDHs that appeared in peer-reviewed publications available in PubMed from January 1, 2009, through December 31, 2014, with a NCHHSTP affiliation. We chose search terms to identify articles with a focus on the following SDH categories: income and employment, housing and homelessness, education and schooling, stigma or discrimination, social or community context, health and health care, and neighborhood or built environment. We classified articles based on the depth of topic coverage as “substantial” (ie, one of ≤3 foci of the article) or “minimal” (ie, one of ≥4 foci of the article).
Results:
Of 862 articles authored by NCHHSTP, 366 (42%) addressed the SDH factors of interest. Some articles addressed >1 SDH factor (366 articles appeared 568 times across the 7 categories examined), and we examined them for each category that they addressed. Most articles that addressed SDHs (449/568 articles; 79%) had a minimal SDH focus. SDH categories that were most represented in the literature were health and health care (190/568 articles; 33%) and education and schooling (118/568 articles; 21%).
Conclusions:
This assessment serves as a baseline measurement of inclusion of SDH topics from NCHHSTP authors in the literature and creates a methodology that can be used in future assessments of this topic.
Keywords: social determinants of health, HIV, sexually transmitted disease, viral hepatitis, tuberculosis
There are social conditions that predispose particular populations to diseases via “the conditions in which people are born, grow, work, live, and age,” as well as “the wider set of forces and systems shaping the conditions of daily life.”1–4 These social conditions result in disparities in health care access, educational achievement, and economic status that influence the health of populations. For example, people of low socioeconomic status are often less likely than those of higher socioeconomic status to adhere to HIV medication regimens. This lack of adherence may be caused by difficulties in maintaining medical appointments (due to lack of transportation and inflexible work schedules) and an inability to pay for prescriptions. Social factors that cause health disparities are generally referred to as social determinants of health (SDHs).5–7 Increasingly, in the past 30 years, public health researchers have examined SDHs and their impact on health outcomes.8–14 SDHs are included among the goals of Healthy People 2020 (HP2020). HP2020 uses the following categories to conceptualize how SDHs affect health: economic stability, education, social or community context, health and health care, and neighborhood or built environment.15 In 2003, the National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention (NCHHSTP) at the Centers for Disease Control and Prevention (CDC) established an Office of Health Disparity to consider how SDHs put particular communities at risk for HIV/AIDS, viral hepatitis, sexually transmitted diseases (STDs), tuberculosis (TB), and poor adolescent health.16,17
To understand the drivers of health disparities and the persistence of diseases among people in certain racial/ethnic minority groups and those of low socioeconomic status, NCHHSTP held external consultations and promoted policy and research investigations of the impact of SDHs.18–20 These efforts culminated in the NCHHSTP’s strategic plan (2010-2015), a document that emphasized SDHs and the reduction of health disparities as a top priority.21 To establish a baseline toward achievement of this priority, we systematically measured the types of SDHs discussed in the peer-reviewed literature available in PubMed with an NCHHSTP affiliation and how frequently these SDHs were discussed.
Methods
We used the MEDLINE database of biomedical and life science references through PubMed to systematically identify articles of interest. We identified all eligible articles in PubMed by using the following search criteria: (1) published in English; (2) published during January 1, 2009–December 31, 2014; and (3) included an author whose affiliation was listed as NCHHSTP (Box). The dates were chosen to correlate with the development and release of the NCHHSTP strategic plan for 2010-2015 that highlighted the importance of SDHs. We included articles that named one of the NCHHSTP divisions in the author’s affiliation. In articles that had 2 or more NCHHSTP authors from multiple CDC centers or divisions, we attributed the article to the division of the highest-ranked author. Search terms included the divisions within NCHHSTP: Division of Adolescent and School Health, Division of HIV/AIDS Prevention, Division of STD Prevention, Division of Tuberculosis Elimination, and Division of Viral Hepatitis. If an article listed only a center affiliation, we attributed the article to the division of the first-listed author. Articles authored by people in the Program Collaboration and Service Integration effort (a program that was designed to integrate interrelated health issues, activities, and prevention strategies to facilitate comprehensive delivery of services among diseases of the center) or by people in offices of the Associate Director of Health Equity were attributed to the Office of the Director.
Box.
PubMed search terms used in a 2-stage search process to (1) identify articles authored by the National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention (NCHHSTP) and (2) identify articles with a focus on the social determinants of health, January 2009 through December 2014.
Search strategy 1: to identify articles authored by and affiliated with NCHHSTP and each division:
((((“centers for disease control and prevention”[Affiliation])) AND (“2009/01/01”[Date - Create]: “2014/12/31”[Date - Create]))) AND (“Division of Adolescent and School Health”)
((((“centers for disease control and prevention”[Affiliation])) AND (“2009/01/01”[Date - Create]: “2014/12/31”[Date - Create]))) AND “Division of Tuberculosis Elimination”)
((((“centers for disease control and prevention”[Affiliation])) AND (“2009/01/01”[Date - Create]: “2014/12/31”[Date - Create]))) AND “Division of HIV/AIDS Prevention”)
((((“centers for disease control and prevention”) AND (“2009/01/01”[Date - Create]: “2014/12/31”[Date - Create]))) AND “Division of STD Prevention”)
((((“centers for disease control and prevention”[Affiliation])) AND (“2009/01/01”[Date - Create]: “2014/12/31”[Date - Create])) AND “Division of Viral Hepatitis”)
(((((((National Center for HIV/AIDS, Hepatitis, STD and TB Prevention) AND (“2009/01/01”[Date - Create]: “2014/12/31”[Date - Create])))) NOT (“Division of STD Prevention”[Affiliation] OR “Division of Viral Hepatitis”[Affiliation] OR “Division of Tuberculosis Elimination”[Affiliation] OR “Division of HIV/AIDS Prevention”[Affiliation] OR “Division of Adolescent and School Health”[Affiliation]))))
Search strategy 2: to identify articles with a focus on the social determinants of health:
Income and employment:
AND ((“poverty”[MeSH Terms] OR “poverty”[All Fields]) OR (“income”[MeSH Terms] OR “income”[All Fields]) OR deprivation[All Fields] OR (“health resources”[MeSH Terms] OR (“health”[All Fields] AND “resources”[All Fields]) OR “health resources”[All Fields] OR “resources”[All Fields]) OR “wealth” [All Fields] OR (material[All Fields] AND “resources”[All Fields] OR “material resources”[All Fields]) OR “wages”[All Fields] OR (“Salary”[All Fields] OR “employment”[All Fields] OR “unemployment”[All Fields]))
Housing and homelessness:
AND (house[All Fields] OR home[All Fields] OR (“homeless persons”[MeSH Terms] OR (“homeless”[All Fields] AND “persons”[All Fields]) OR “homeless persons”[All Fields] OR “homeless”[All Fields]) OR (“housing”[MeSH Terms] OR “housing”[All Fields] OR “residence characteristics”[MeSH Terms] OR (“residence”[All Fields] AND “characteristics”[All Fields]) OR “residence characteristics”[All Fields] OR “foreclosure”[All Fields] OR “home ownership”[All Fields]))
Education and schooling:
AND ((“schools”[MeSH Terms] OR “schools”[All Fields] OR “school”[All Fields]) OR (“education”[Subheading] OR “education”[All Fields])
Stigma or discrimination:
AND (“Stigma”[All Fields] OR “discrimination”[All Fields] OR “segregation”[All Fields] OR “prejudice”[All Fields] OR “prejudice”[MeSH Terms] OR “racism”[All Fields] OR “racism”[MeSH Terms] OR “homophobia”[All Fields])
Social or community context:
AND (“social context”[All Fields] OR “community”[All Fields] OR “cohesion”[All Fields] OR “participation”[All Fields] OR “neighborhood”[All Fields] OR “neighbor”[All Fields] OR “incarceration”[All Fields] OR “jail”[All Fields] OR “institutionalized”[All Fields] OR “prisons”[All Fields] OR “prisons”[MeSH Terms]))
Health and health care:
AND (“health services”[MeSH Terms] OR (“health”[All Fields] AND “services”[All Fields]) OR “health services”[All Fields]) OR (“primary health care”[MeSH Terms] OR (“primary”[All Fields] AND “health”[All Fields] AND “care”[All Fields]) OR “primary health care”[All Fields] OR (“primary”[All Fields] AND “care”[All Fields]) OR “primary care”[All Fields]) OR (“Health Services Accessibility”[All Fields] OR “Health Services Accessibility”[MeSH Terms]) OR “Outpatient Clinics, Hospital”[MeSH] OR “Outpatient Clinics, Hospital”[All Fields] OR (“Ambulatory Care Facilities”[Mesh] AND “Ambulatory Care Facilities”[All Fields]) OR “outpatient”[All Fields] OR “inpatient”[all fields] OR “Appointments and Schedules”[MeSH Terms] OR “Appointments and Schedules”[All Fields] OR (“appointments”[All Fields] AND “schedules”[All Fields]) OR “appointments”[All Fields] OR “schedule”[All Fields]
Neighborhood or built environment:
AND (“neighborhood”[All Fields]) OR “catchment area” OR “block”[All Fields] OR “town”[All Fields] OR (“cities”[MeSH Terms] OR “cities”[All Fields] OR “city”[All Fields]) OR (“censuses”[MeSH Terms] OR “censuses”[All Fields] OR “census”[All Fields]) AND “tract”[All Fields] OR (“environment”[MeSH Terms] OR “environment”[All Fields]) OR (“crime”[MeSH Terms] OR “crime”[All Fields]) OR (“violence”[MeSH Terms] OR “violence”[All Fields]) OR “urban”[All Fields] OR “rural”[All Fields] OR “zoning”[All Fields])
We further subdivided several of the original HP2020 categories to create 7 total categories of SDHs, as opposed to the 5 given in HP2020.15 We made the decision to use 7 categories a priori based on our knowledge of NCHHSTP research and SDH factors that were likely to be associated with particular diseases or divisions. We examined 7 categories of SDHs in this systematic review: income and employment, housing and homelessness, education and schooling, stigma or discrimination, social or community context, health and health care, and neighborhood or built environment. After we identified eligible articles, we searched the article titles and abstracts again in PubMed by using SDH-specific terms that correlated to these 7 categories (Table 1). We included articles in an SDH category if we identified them via PubMed title and abstract search using the terms related to each SDH category (Box).
Table 1.
Categories of social determinants of health used in Healthy People 2020 and categories used in a review of articles authored by NCHHSTP in the peer-reviewed literaturea
| Healthy People 2020 SDH Category | Examples of SDH Category in Healthy People 2020 | SDH Categories Used in a Review of Articles in the Peer-Reviewed Literature by Authors With an NCHHSTP Affiliation |
|---|---|---|
| Economic stability | Poverty, employment status, access to employment, and housing stability (eg, homelessness or foreclosure) | Income and employment Housing and homelessness |
| Education | High school graduation rates, school policies that support health promotion, school environments that are safe and conducive to learning, and enrollment in higher education | Education and schooling |
| Social or community context | Social or community context, family structure, social cohesion, perceptions of discrimination, civic participation, and incarceration/institution | Stigma or discrimination Social or community context |
| Health and health care | Access to health services, including clinical and preventive care, access to primary care (eg, community-based health promotion and wellness programs), and health technology | Health and health care |
| Neighborhood and built environment | Quality of housing, crime and violence, environmental conditions, and access to healthy foods | Neighborhood or built environment |
Abbreviations: NCHHSTP, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention; SDH, social determinant of health.
a Data source: US Department of Health and Human Services, Office of Disease Prevention and Health Promotion.15
We retrieved full-text articles identified by using the SDH search terms and assessed them to ensure that (1) all articles met the eligibility criteria, (2) the content of articles addressed diseases or affiliated health conditions covered by NCHHSTP (eg, HIV/AIDS, STDs, TB, adolescent health, and viral hepatitis), and (3) the articles discussed SDHs. We reviewed each article for each SDH category with which it was identified. We excluded from further analysis articles that were identified via PubMed using SDH search terms but that did not discuss the relevant SDH. To ensure consistency in inclusion or exclusion of identified articles, we searched full-text articles by using Adobe XI Reader (version 11.0.12, Adobe Systems Incorporated) for the same terms used in PubMed.
If an article did address the SDH categories of interest, we described it as having either a “substantial” focus or a “minimal” focus on the SDH category. We classified an article as having a substantial SDH focus if the SDH factor was 1 of 3 or fewer foci of the article. We classified the article as having a minimal SDH focus if the SDH topic was mentioned briefly in the introduction or discussion or was examined as part of 4 or more foci of the article.
Although the HP2020 framework creates separate SDH categories, it is not uncommon for people in a particular population group or area to be disadvantaged in multiple ways. For example, people living in rural areas may be poor and lack medical services.22,23 Given that many SDHs are interrelated, we included articles in every SDH category in which they were identified. This methodology resulted in some articles being counted multiple times. One author (EEF) reviewed and classified articles into minimal or substantial categories.
Results
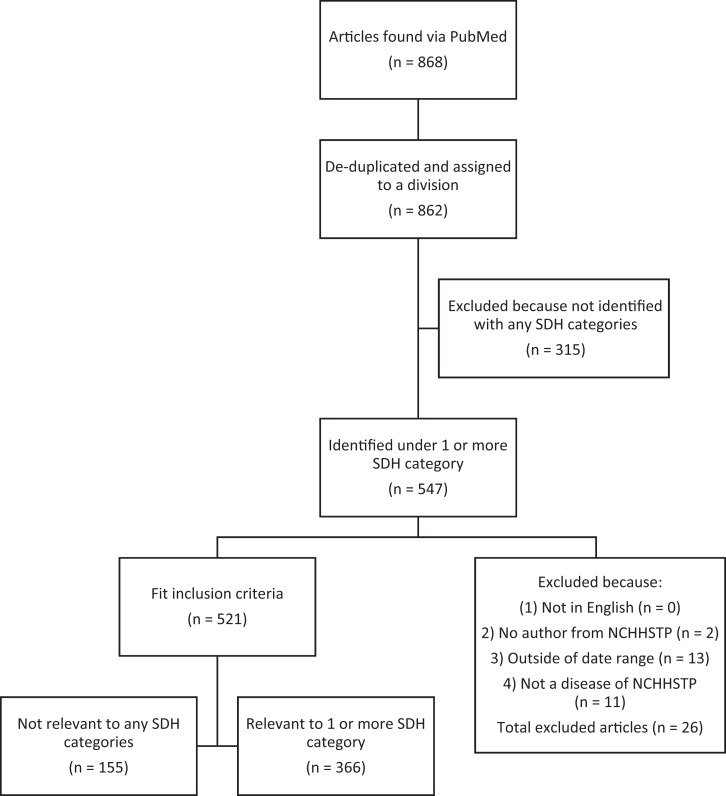
We identified 868 articles as having authors with an NCHHSTP affiliation in the MEDLINE database with publication dates from January 1, 2009, through December 31, 2014. Six articles had authors from multiple divisions within NCHHSTP and were assigned to a single division or the Office of the Director based on the first-listed NCHHSTP author’s affiliation, resulting in a total of 862 unique articles. By using the search terms created for each SDH category, we identified 547 unique articles. We identified some articles in more than one SDH category, resulting in these 547 articles appearing 777 times across all SDH categories (Figure). We excluded the other 315 unique articles from further analysis because no SDH-specific search terms appeared in the title and abstract review.
Figure.
Flowchart of articles with a National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention (NCHHSTP) affiliation that address the social determinants of health (SDHs) in the peer-reviewed literature, United States, 2009-2014. Articles had to address 1 of 7 Healthy People 202015 categories: income and employment, housing and homelessness, education and schooling, stigma or discrimination, social or community context, health and health care, and neighborhood or built environment. Articles could appear in more than 1 SDH category. Numbers refer to the number of unique articles located.
Upon full-text review, 155 articles identified by using SDH search terms did not discuss SDHs. We excluded these articles from further analysis, leaving 366 unique articles, which appeared 568 times across all SDH categories.
The search terms that identified the most articles were those for the SDH categories of health and health care (190/568 articles; 33%) and education and schooling (118/568 articles; 21%). The Division of Adolescent and School Health was the NCHHSTP division that was most closely associated with a particular SDH category: 49 of 52 (94%) published articles focused on education and schooling were authored by someone from the Division of Adolescent and School Health (Table 2). Across all SDH categories, 449 of 568 (79%) relevant articles only briefly discussed the SDH topic and were therefore classified as having a minimal SDH focus.
Table 2.
Frequencya of social determinants of health categories by affiliation of author within NCHHSTP, in a systematic review of the peer-reviewed literature in PubMed, United States, 2009-2014b
| Type of SDH, Frequency (%) | ||||||||
|---|---|---|---|---|---|---|---|---|
| NCHHSTP Division | Frequency of SDH | Income and Employment | Housing and Homelessness | Education and Schooling | Stigma or Discrimination | Social or Community Context | Health and Health Care | Neighborhood or Built Environment |
| Division of Adolescent and School Health | 89 | 3 (3) | 1 (1) | 49 (55) | 1 (1) | 8 (9) | 13 (15) | 14 (16) |
| Division of HIV/AIDS Prevention | 224 | 32 (14) | 12 (5) | 31 (14) | 7 (3) | 44 (20) | 73 (33) | 25 (11) |
| Division of STD Prevention | 110 | 14 (13) | 5 (5) | 14 (13) | 2 (2) | 12 (11) | 54 (49) | 9 (8) |
| Division of Tuberculosis Elimination | 46 | 6 (13) | 10 (22) | 6 (13) | 0 | 7 (15) | 13 (28) | 4 (9) |
| Division of Viral Hepatitis | 71 | 4 (6) | 2 (3) | 15 (21) | 0 | 12 (17) | 28 (39) | 10 (14) |
| Office of the Director | 28 | 3 (11) | 2 (7) | 3 (11) | 0 | 6 (21) | 9 (32) | 5 (18) |
| Total | 568 | 62 (11) | 32 (6) | 118 (21) | 10 (2) | 89 (16) | 190 (33) | 67 (12) |
Abbreviations: NCHHSTP, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention; SDH, social determinant of health; STD, sexually transmitted disease.
a Frequency refers to the number of articles identified for each SDH category and each division; a single article may be counted in more than 1 category if it covered more than 1 SDH topic. Frequencies are the result of a 2-stage search process in PubMed, first searching for articles with NCHHSTP affiliations, and then searching among affiliated articles for SDH categories in which these articles appeared. See Box containing search terms for further details.
b Data source: US Department of Health and Human Services, Office of Disease Prevention and Health Promotion.15
Income and Employment
Of the 62 articles that discussed income and employment, 56 (90%) had a minimal SDH focus17,24–78 and 6 (10%) had a substantial SDH focus.79–84 The identified articles focused on income in various ways, including as a personal median or annual income, being above or below the income threshold for the federal poverty level, household income level, and proportion of households below the federal poverty level in a community. Most articles reported employment as individual employment or unemployment or as the proportion of people unemployed in a community.
Housing and Homelessness
Of the 32 articles that discussed housing or homelessness, 25 (78%) had a minimal focus33,45,63,68,73,78,85–103 and 7 (22%) had a substantial focus.44,79,81,104–107 Articles measured and discussed housing and homelessness in several ways depending on the NCHHSTP division and contents of the identified articles, including if participants were currently marginally housed, had been homeless in the past year, or had a parent in the home. Other discussions of housing included in-home testing for STDs or HIV, households used as the unit of randomization in clinical trials, and the housing vacancy proportion in a census tract.
Education and Schooling
We identified 118 articles in the SDH category of education and schooling. Of the 118 articles, we classified 81 (69%) as having a minimal SDH focus24–26,28,32,33,35,36,38,40,42,45,49,50,59,61,70,73,74,85,108–168 and 37 articles as having a substantial focus on education and schooling, including those that used schools or education levels as a major variable in analysis, examined school-based health interventions, described health programs and policies at school, discussed health training for educators, or discussed in-depth school-based activities (eg, physical education class).37,44,81,169–202 Articles discussed and measured education and school-related factors in various ways, including the level of parental education, level of participant education, activities at school, proportion with a high school degree in a community or census tract, design and use of health education campaigns, and health interventions conducted in school settings.
Stigma or Discrimination
We identified 10 articles that addressed stigma or discrimination, 6 of which had a minimal SDH focus.39,49,94,203–205 The 4 articles that had a substantial SDH focus were evenly distributed between those that discussed stigma and those that discussed discrimination.29,88,115,206 Seven articles discussed stigma related to HIV/AIDS, TB, or STDs, in particular stigma associated with testing and treating disease. Three articles discussed racism, segregation, or racial discrimination.29,39,115
Social or Community Context
We identified 89 articles that addressed social or community context. We included search terms related to jails, prisons, and incarceration in this category, and many articles discussed issues related to incarceration. Most articles (64/89; 72%) covered factors related to the social or community context at minimal depth.28,38,39,44,50,51,61,74,78,84,89,96,101,110,111,117,119,126,127,141,148,149,151,152,158,159,164,168,175,180,189,192,197,198,204,207–235 The 25 articles with a substantial focus on social or community context included those that focused on testing for disease (eg, HIV, STDs) in communities, prevention campaigns or interventions designed for communities or incarcerated populations, and community-level associations.43,45,52,53,87,88,94,106,139,193,236–250 Articles discussing social or community context included those that discussed geographic communities, larger communities composed of racial/ethnic minority groups, and community-based health care organizations. Few articles discussed the importance of social support or group membership (eg, church or social organizations).
Health and Health Care
We identified 190 articles on health and health care, most of which had a minimal SDH focus (162/190; 85%).26,28,42,47,52–54,56,59,64,73,82,84,86,91,93,102,106,116,117,127,128,139,141,144,147,148,151–153,160–162,164,165,167,169,172,174,175,179,183,186,187,192,197,198,202–204,213,217–219,226,229,233,235,236,243–245,247–249,251–347
The 28 articles that had a substantial SDH focus included those that discussed in-depth health care provision, health care disparities, delays or refusal to enter into care, retaining patients in care, and health care costs.31,50,57,74,105,107,124,146,170,208,214,215,223,348–362 The identified articles addressed health and health care in 2 main ways: (1) the use of health care services and/or health care-seeking behaviors and (2) health care access and affordability or health care provision. Additional topics included disease transmission in health care settings and health care workers as an at-risk group.
Neighborhood or Built Environment
The category of neighborhood or built environment included search terms related to violence and crime. Of 67 articles identified as having a focus on neighborhood or built environment, 50 (75%) had a minimal focus17,39,73,84,89,103,105,109,114,116–118,120,127,132,147,171,173,178,179,198,200,203,219,243,252,267,328,341,345,347,356,363–380 and 17 (25%) had a substantial focus.45,81–83,104,119,184,228,359,381–388 In general, articles addressed the neighborhood and/or the built environment in 1 of 3 ways: as violence (especially intimate partner violence), geography (census tracts, multistate areas, regional areas), or urbanicity (the degree to which an area was urban, rural, or suburban).
Discussion
This systematic review is the first to examine the number of articles on SDHs incorporated into research to provide a baseline quantifiable mechanism for determining improvement in SDH research and reducing health disparities. This assessment measured the frequency and depth of articles discussing SDH among authors with an NCHHSTP affiliation, and created a methodology that can be used in future assessments of SDHs in peer-reviewed publications. Most of the identified articles in this systematic review had a minimal focus on SDHs. The lack of articles with a substantial SDH focus is of interest given the importance of SDHs to HIV/AIDS, STDs, TB, and viral hepatitis disease acquisition, treatment, morbidity, and mortality,389–393 as well as the prioritization of health equity and SDHs in the NCHHSTP’s strategic plan (2010-2015). Because the Patient Protection and Affordable Care Act, the subprime mortgage crisis, and US economic recession dominated public and scientific discourse during 2009-2014,394,395 we anticipated that more articles would have an upstream focus on policy areas such as income and employment or housing and homelessness. The lack of articles with a substantial focus on these topics may represent a missed opportunity for in-depth publication of the effects of these social circumstances on diseases of interest to NCHHSTP.
Even in the most well-represented category, health and health care, fewer than 25% of the articles had a substantial focus on SDHs. This lack of substantial focus may be due to our examination of only the peer-reviewed scientific literature produced by NCHHSTP, rather than including SDH concepts in all of NCHHSTP’s work. In this review, we found that most articles identified via PubMed that discussed health and health care focused on routine disease prevention and clinical activities (surveillance, outbreak investigation, and testing or treatment of disease). Research into patient and community SDHs could inform these efforts by identifying factors associated with disease outbreaks and persistence, as well as barriers to implementation and success of disease-fighting programs.
Although each SDH category in this assessment included multiple related factors, such as income and employment, one factor in an SDH category often was covered more extensively than others. For example, in the SDH category stigma or discrimination, articles overwhelmingly focused on stigma (particularly testing or treatment of stigma associated with HIV/AIDS or STDs), with limited focus on discrimination, homophobia, racism, or xenophobia, all of which can increase stigma and disease transmission.396,397 Although the focus on disease-related stigma is important, it is an incomplete representation of the factors that permit and drive health disparities in these diseases.
Limitations
This systematic review had several limitations. First, although we created a comprehensive list of search terms in an effort to cover all components of each SDH category, important components may have been omitted. Second, we examined only articles that were published during 2009-2014 in peer-reviewed journals contained in the MEDLINE database. It is impossible to predict whether the articles not included (eg, internal reports or those in non–peer-reviewed journals) would have contained more articles on SDH topics. Third, reviewer bias in classifying SDH categories during content analysis was possible. Although we checked articles multiple times to confirm categorization as minimal or substantial in focus, a single reviewer made these determinations, which may have resulted in nondifferential misclassification. Fourth, we classified each article as having a minimal or substantial focus based on the depth of discussion within each SDH category under which it was identified rather than based on the overall number of SDHs that were discussed in the article. Had we used a different assessment method, some articles classified as minimal might have been considered substantial. Fifth, this review did not qualify the type of SDH information or discussion beyond categorization of minimal and substantial. We did not assess the translation of substantial or minimal discussion into policy, research, or program interventions in this study. Future work should examine the extent to which the SDH information included in NCHHSTP articles is actionable or contributes to the formation of policy. An examination of actionable SDH information from NCHHSTP articles might be quantified by conducting a review of guidance or policy documents or grantee reports generated after publication of the peer-reviewed article. Finally, both the total number of articles identified and the number of articles identified for each SDH category were likely an underestimate of the actual number of published articles produced by each NCHHSTP division, because certain journals allow only the highest organizational unit (ie, CDC) as the affiliation. Our review included only those articles that listed the center (NCHHSTP) or division affiliation in PubMed.
Conclusions
Knowing the importance of SDHs to the health outcomes of NCHHSTP, we encourage public health departments and other health agencies to allocate resources and time to the topic areas we identified as minimally covered in this analysis. These systematic search methods can serve as a model for other public health agencies that wish to assess the content of their published SDH research.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This publication was supported by cooperative agreement number U36/CCU300430 from the Centers for Disease Control and Prevention (CDC) and the Association of Schools and Programs of Public Health (ASPPH). The findings and conclusions of this publication are those of the authors and do not necessarily represent the official position of CDC or ASPPH.
References
- 1. World Health Organization. Social determinants of health. 2018. http://www.who.int/social_determinants/en. Accessed May 5, 2018.
- 2. McKinlay JB. A case for refocussing upstream—the political economy of illness In: Enelow AJ, Henderson JB, eds. Applying Behavioral Science to Cardiovascular Risk: Proceedings of a Conference. Washington, DC: American Heart Association; 1975:7–17. [Google Scholar]
- 3. McKeown T. The Role of Medicine: Dream, Mirage, or Nemesis? Princeton, NJ: Princeton University Press; 1980. [Google Scholar]
- 4. Rose G. Sick individuals and sick populations. Int J Epidemiol. 1985;14(1):32–38. [DOI] [PubMed] [Google Scholar]
- 5. Blane D. Social determinants of health—socioeconomic status, social class, and ethnicity. Am J Public Health. 1995;85(7):903–905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Marmot M, Wilkinson RG. Social Determinants of Health. 2nd ed New York: Oxford University Press; 2005. [Google Scholar]
- 7. Smith A. Social factors and disease: the medical perspective. BMJ. 1987;294(6576):881–883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Marmot MG, Stansfeld S, Patel C, et al. Health inequalities among British civil servants: the Whitehall II study. Lancet. 1991;337(8754):1387–1393. [DOI] [PubMed] [Google Scholar]
- 9. Williams DR, Jackson PB. Social sources of racial disparities in health. Health Aff (Millwood). 2005;24(2):325–334. [DOI] [PubMed] [Google Scholar]
- 10. Pickett KE, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. J Epidemiol Community Health. 2001;55(2):111–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Semenza JC. Strategies to intervene on social determinants of infectious diseases. Euro Surveill. 2010;15(27):32–39. [DOI] [PubMed] [Google Scholar]
- 12. Acevedo-Garcia D. Residential segregation and the epidemiology of infectious diseases. Soc Sci Med. 2000;51(8):1143–1161. [DOI] [PubMed] [Google Scholar]
- 13. Diaz T, Chu SY, Conti L, et al. Health insurance coverage among persons with AIDS: results from a multistate surveillance project. Am J Public Health. 1994;84(6):1015–1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Nguyen N, Holodniy M. HIV infection in the elderly. Clin Interv Aging. 2008;3(3):453–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. US Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Healthy People 2020: social determinants of health. Updated May 4, 2018 http://www.healthypeople.gov/2020/topicsobjectives2020/overview.aspx?topicid=39. Accessed May 5, 2018.
- 16. Centers for Disease Control and Prevention. Social Determinants of Health Among Persons Disproportionately Affected by HIV/AIDS, Viral Hepatitis, Sexually Transmitted Diseases and Tuberculosis: Impact and Approaches to Eliminate Health Disparities—Green Paper. Atlanta, GA: US Department of Health and Human Services; 2008. [Google Scholar]
- 17. Sharpe TT, Harrison KM, Dean HD. Summary of CDC consultation to address social determinants of health for prevention of disparities in HIV/AIDS, viral hepatitis, sexually transmitted diseases, and tuberculosis. Public Health Rep. 2010;125(suppl 4):11–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Dean HD, Fenton KA. Integrating a social determinants of health approach into public health practice: a five-year perspective of actions implemented by CDC’s National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention. Public Health Rep. 2013;128(suppl 3):5–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Division of HIV/AIDS Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention. The Care and Prevention in the United States (CAPUS) demonstration project. Updated February 9, 2016 http://www.cdc.gov/hiv/prevention/demonstration/capus. Accessed May 5, 2018.
- 20. Division of STD Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention. Community approaches to reducing sexually transmitted diseases. Updated December 6, 2017 http://www.cdc.gov/std/health-disparities/cars.htm. Accessed May 5, 2018.
- 21. Centers for Disease Control and Prevention. National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention strategic plan 2010-2015. February 2010. https://www.cdc.gov/nchhstp/docs/10_nchhstp-strategicplanbooksemi-final508.pdf. Accessed May 5, 2018.
- 22. Centers for Disease Control and Prevention. Establishing a Holistic Framework to Reduce Inequities in HIV, Viral Hepatitis, STDs, and Tuberculosis in the United States. Atlanta, GA: National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention; 2010. [Google Scholar]
- 23. World Health Organization. A Conceptual Framework for Action on the Social Determinants of Health. Geneva: World Health Organization; 2010. [Google Scholar]
- 24. Eaton DK, Brener ND, Kann L, et al. Comparison of paper-and-pencil versus web administration of the Youth Risk Behavior Survey (YRBS): risk behavior prevalence estimates. Eval Rev. 2010;34(2):137–153. [DOI] [PubMed] [Google Scholar]
- 25. Jones SE, Anderson K, Lowry R, Conner H. Risks to health among American Indian/Alaska Native high school students in the United States. Prev Chronic Dis. 2011;8(4):A76. [PMC free article] [PubMed] [Google Scholar]
- 26. Khabbaz RF, Moseley RR, Steiner RJ, Levitt AM, Bell BP. Challenges of infectious diseases in the USA. Lancet. 2014;384(9937):53–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Oster AM, Russell K, Wiegand RE, et al. HIV infection and testing among Latino men who have sex with men in the United States: the role of location of birth and other social determinants. PLoS One. 2013;8(9):e73779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Mizuno Y, Zhu J, Crepaz N, et al. Receipt of HIV/STD prevention counseling by HIV-infected adults receiving medical care in the United States. AIDS. 2014;28(3):407–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Mizuno Y, Borkowf C, Millett GA, Bingham T, Ayala G, Stueve A. Homophobia and racism experienced by Latino men who have sex with men in the United States: correlates of exposure and associations with HIV risk behaviors. AIDS Behav. 2012;16(3):724–735. [DOI] [PubMed] [Google Scholar]
- 30. Millett GA, Ding H, Marks G, et al. Mistaken assumptions and missed opportunities: correlates of undiagnosed HIV infection among black and Latino men who have sex with men. J Acquir Immune Defic Syndr. 2011;58(1):64–71. [DOI] [PubMed] [Google Scholar]
- 31. Blair JM, Fagan JL, Frazier EL, et al. Behavioral and clinical characteristics of persons receiving medical care for HIV infection—Medical Monitoring Project, United States, 2009. MMWR Surveill Summ. 2014;63(5):1–22. [PubMed] [Google Scholar]
- 32. Wejnert C, Le B, Rose CE, Oster AM, Smith AJ, Zhu J. HIV. infection and awareness among men who have sex with men—20 cities, United States, 2008 and 2011. PLoS One. 2013;8(10):e76878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ivy W III, Miles I, Le B, Paz-Bailey G. Correlates of HIV infection among African American women from 20 cities in the United States. AIDS Behav. 2014;18(suppl 3):266–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Broz D, Pham H, Spiller M, et al. Prevalence of HIV infection and risk behaviors among younger and older injecting drug users in the United States, 2009. AIDS Behav. 2014;18(suppl 3):284–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Beer L, Oster AM, Mattson CL, Skarbinski J. Disparities in HIV transmission risk among HIV-infected black and white men who have sex with men, United States, 2009. AIDS. 2014;28(1):105–114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Gust DA, Kretsinger K, Gaul Z, et al. Acceptability of newborn circumcision to prevent HIV infection in the United States. Sex Transm Dis. 2011;38(6):536–542. [DOI] [PubMed] [Google Scholar]
- 37. Miller KS, Forehand R, Wiegand R, et al. Making HIV prevention programming count: identifying predictors of success in a parent-based HIV prevention program for youth. AIDS Educ Prev. 2011;23(1):38–53. [DOI] [PubMed] [Google Scholar]
- 38. Millett GA, Peterson JL, Flores SA, et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012;380(9839):341–348. [DOI] [PubMed] [Google Scholar]
- 39. Millett GA, Jeffries WL IV, Peterson JL, et al. Common roots: a contextual review of HIV epidemics in black men who have sex with men across the African diaspora. Lancet. 2012;380(9839):411–423. [DOI] [PubMed] [Google Scholar]
- 40. Do AN, Rosenberg ES, Sullivan PS, et al. Excess burden of depression among HIV-infected persons receiving medical care in the United States: data from the Medical Monitoring Project and the Behavioral Risk Factor Surveillance System. PLoS One. 2014;9(3):e92842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. DiNenno EA, Oster AM, Sionean C, Denning P, Lansky A. Piloting a system for behavioral surveillance among heterosexuals at increased risk of HIV in the United States. Open AIDS J. 2012;6:169–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Courtenay-Quirk C, Horvath KJ, Ding H, et al. Perceptions of HIV-related websites among persons recently diagnosed with HIV. AIDS Patient Care STDS. 2010;24(2):105–115. [DOI] [PubMed] [Google Scholar]
- 43. Gant Z, Lomotey M, Hall HI, Hu X, Guo X, Song R. A county-level examination of the relationship between HIV and social determinants of health: 40 states, 2006-2008. Open AIDS J. 2012;6:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Raiford JL, Herbst JH, Carry M, Browne FA, Doherty I, Wechsberg WM. Low prospects and high risk: structural determinants of health associated with sexual risk among young African American women residing in resource-poor communities in the South. Am J Community Psychol. 2014;54(3-4):243–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Gant Z, Gant L, Song R, Willis L, Johnson AS. A census tract-level examination of social determinants of health among black/African American men with diagnosed HIV infection, 2005-2009—17 US areas. PLoS One. 2014;9(9):e107701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Wejnert C, Pham H, Krishna N, Le B, DiNenno E. Estimating design effect and calculating sample size for respondent-driven sampling studies of injection drug users in the United States. AIDS Behav. 2012;16(4):797–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Nesheim S, Harris LF, Lampe M. Elimination of perinatal HIV infection in the USA and other high-income countries: achievements and challenges. Curr Opin HIV AIDS. 2013;8(5):447–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Kyser M, Buchacz K, Bush TJ, et al. Factors associated with non-adherence to antiretroviral therapy in the SUN study. AIDS Care. 2011;23(5):601–611. [DOI] [PubMed] [Google Scholar]
- 49. Gust DA, Mosimaneotsile B, Mathebula U, et al. Risk factors for non-adherence and loss to follow-up in a three-year clinical trial in Botswana. PLoS One. 2011;6(4):e18435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Gardner LI, Giordano TP, Marks G, et al. Enhanced personal contact with HIV patients improves retention in primary care: a randomized trial in 6 US HIV clinics. Clin Infect Dis. 2014;59(5):725–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Purcell DW, McCree DH. Recommendations from a research consultation to address intervention strategies for HIV/AIDS prevention focused on African Americans. Am J Public Health. 2009;99(11):1937–1940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Shrestha RK, Sansom SL, Richardson-Moore A, et al. Costs of voluntary rapid HIV testing and counseling in jails in 4 states—Advancing HIV Prevention Demonstration Project, 2003-2006. Sex Transm Dis. 2009;36(suppl 2):S5–S8. [DOI] [PubMed] [Google Scholar]
- 53. Shrestha RK, Sansom SL, Schulden JD, et al. Costs and effectiveness of finding new HIV diagnoses by using rapid testing in transgender communities. AIDS Educ Prev. 2011;23(suppl 3):49–57. [DOI] [PubMed] [Google Scholar]
- 54. Shrestha RK, Begley EB, Hutchinson AB, et al. Costs and effectiveness of partner counseling and referral services with rapid testing for HIV in Colorado and Louisiana, United States. Sex Transm Dis. 2009;36(10):637–641. [DOI] [PubMed] [Google Scholar]
- 55. Shrestha RK, Sansom SL, Laffoon BT, et al. Estimating the cost to U.S. health departments to conduct HIV surveillance. Public Health Rep. 2014;129(6):496–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Shrestha RK, Sansom SL, Farnham PG. Comparison of methods for estimating the cost of human immunodeficiency virus-testing interventions. J Public Health Manag Pract. 2012;18(3):259–267. [DOI] [PubMed] [Google Scholar]
- 57. Gardner LI, Marks G, Craw JA, et al. A low-effort, clinic-wide intervention improves attendance for HIV primary care. Clin Infect Dis. 2012;55(8):1124–1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Meites E, Krishna NK, Markowitz LE, Oster AM. Health care use and opportunities for human papillomavirus vaccination among young men who have sex with men. Sex Transm Dis. 2013;40(2):154–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Leichliter JS, Chandra A, Aral SO. Correlates of self-reported pelvic inflammatory disease treatment in sexually experienced reproductive-aged women in the United States, 1995 and 2006-2010. Sex Transm Dis. 2013;40(5):413–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Leichliter JS, Chesson HW, Sternberg M, Aral SO. The concentration of sexual behaviours in the USA: a closer examination of subpopulations. Sex Transm Infect. 2010;86(suppl 3):iii45–iii51. [DOI] [PubMed] [Google Scholar]
- 61. Aral SO, Leichliter JS. Non-monogamy: risk factor for STI transmission and acquisition and determinant of STI spread in populations. Sex Transm Infect. 2010;86(suppl 3):iii29–iii36. [DOI] [PubMed] [Google Scholar]
- 62. Bradley H, Leichliter JS, Gift TL. Does discussing sexually transmissible infections or HIV with a parent increase condom use among young women using other contraceptive methods? Sex Health. 2013;10(1):82–90. [DOI] [PubMed] [Google Scholar]
- 63. Friedman AL, Bloodgood B. “Something we’d rather not talk about”: findings from CDC exploratory research on sexually transmitted disease communication with girls and women. J Womens Health (Larchmt). 2010;19(10):1823–1831. [DOI] [PubMed] [Google Scholar]
- 64. Owusu-Edusei K, Bohm MK, Kent CK. Diagnostic methodologies for chlamydia screening in females aged 15 to 25 years from private insurance claims data in the United States, 2001 to 2005. Sex Transm Dis. 2009;36(7):419–421. [DOI] [PubMed] [Google Scholar]
- 65. Owusu-Edusei K, Jr, Doshi SR, Apt BS, Gift TL. The direct cost of chlamydial infections: estimates for the employer-sponsored privately insured population in the United States, 2003-2007 [published erratum appears in Sex Transm Dis. 2011;38(9):888]. Sex Transm Dis. 2010;37(8):519–521. [DOI] [PubMed] [Google Scholar]
- 66. Bohm MK, Gift TL, Tao G. Patterns of single and multiple claims of epididymitis among young privately-insured males in the United States, 2001 to 2004. Sex Transm Dis. 2009;36(8):490–492. [DOI] [PubMed] [Google Scholar]
- 67. Bradley H, Satterwhite CL. Prevalence of Neisseria gonorrhoeae infections among men and women entering the National Job Training Program—United States, 2004-2009. Sex Transm Dis. 2012;39(1):49–54. [DOI] [PubMed] [Google Scholar]
- 68. Kurbatova EV, Taylor A, Gammino VM, et al. Predictors of poor outcomes among patients treated for multidrug-resistant tuberculosis at DOTS-plus projects. Tuberculosis (Edinb). 2012;92(5):397–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Dalton T, Cegielski P, Akksilp S, et al. Prevalence of and risk factors for resistance to second-line drugs in people with multidrug-resistant tuberculosis in eight countries: a prospective cohort study [published erratum appears in Lancet. 2012;380(9851):1386]. Lancet. 2012;380(9851):1406–1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Pascopella L, Franks J, Marks SM, et al. Opportunities for tuberculosis diagnosis and prevention among persons living with HIV: a cross-sectional study of policies and practices at four large Ryan White Program-funded HIV clinics. PLoS One. 2014;9(7):e101313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Marks S. Commentary: socio-economic determinants of tuberculosis in Recife, Brazil. Int J Epidemiol. 2009;38(5):1295–1296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Coleman MS, Marienau KJ, Marano N, Marks SM, Cetron MS. Economics of United States tuberculosis airline contact investigation policies: a return on investment analysis. Travel Med Infect Dis. 2014;12(1):63–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Bloss E, Holtz TH, Jereb J, et al. Tuberculosis in indigenous peoples in the U.S., 2003-2008. Public Health Rep. 2011;126(5):677–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Tohme RA, Xing J, Liao Y, Holmberg SD. Hepatitis C testing, infection, and linkage to care among racial and ethnic minorities in the United States, 2009-2010. Am J Public Health. 2013;103(1):112–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Teshale EH, Denniston MM, Drobeniuc J, Kamili S, Teo CG, Holmberg SD. Decline in hepatitis E virus antibody prevalence in the United States from 1988-1994 to 2009-2010. J Infect Dis. 2015;211(3):366–373. [DOI] [PubMed] [Google Scholar]
- 76. Spradling PR, Tong X, Rupp LB, et al. Trends in HCV RNA testing among HCV antibody-positive persons in care, 2003-2010. Clin Infect Dis. 2014;59(7):976–981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Hadler SC, Fuqiang C, Averhoff F, et al. The impact of hepatitis B vaccine in China and in the China GAVI Project. Vaccine. 2013;31(suppl 9):J66–J72. [DOI] [PubMed] [Google Scholar]
- 78. Moonesinghe R, Fleming E, Truman BI, Dean HD. Linear and non-linear associations of gonorrhea diagnosis rates with social determinants of health. Int J Environ Res Public Health. 2012;9(9):3149–3165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Vaughan AS, Rosenberg E, Shouse RL, Sullivan PS. Connecting race and place: a county-level analysis of white, black, and Hispanic HIV prevalence, poverty, and level of urbanization. Am J Public Health. 2014;104(7):e77–e84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Owusu-Edusei K, Jr, Chesson HW, Leichliter JS, Kent CK, Aral SO. The association between racial disparity in income and reported sexually transmitted infections. Am J Public Health. 2013;103(5):910–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Stenger MR, Samuel MC, Anschuetz GL, et al. Neighborhoods at risk: estimating risk of higher Neisseria gonorrhoeae incidence among women at the census tract level. Sex Transm Dis. 2014;41(11):649–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Chesson HW, Kent CK, Owusu-Edusei K, Jr, Leichliter JS, Aral SO. Disparities in sexually transmitted disease rates across the “eight Americas.” Sex Transm Dis. 2012;39(6):458–464. [DOI] [PubMed] [Google Scholar]
- 83. Chesson HW, Owusu-Edusei K, Jr, Leichliter JS, Aral SO. Violent crime rates as a proxy for the social determinants of sexually transmissible infection rates: the consistent state-level correlation between violent crime and reported sexually transmissible infections in the United States, 1981-2010. Sex Health. 2013;10(5):419–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Sharpe TT, Voute C, Rose MA, Cleveland J, Dean HD, Fenton K. Social determinants of HIV/AIDS and sexually transmitted diseases among black women: implications for health equity. J Womens Health (Larchmt). 2012;21(3):249–254. [DOI] [PubMed] [Google Scholar]
- 85. Brener ND, Eaton DK, Kann LK, et al. Behaviors related to physical activity and nutrition among U.S. high school students. J Adolesc Health. 2013;53(4):539–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. O’Leary A, Jemmott JB III, Jemmott LS, et al. Moderation and mediation of an effective HIV risk-reduction intervention for South African adolescents. Ann Behav Med. 2012;44(2):181–191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Sanchez T, Finlayson T, Murrill C, Guilin V, Dean L. Risk behaviors and psychosocial stressors in the New York City house ball community: a comparison of men and transgender women who have sex with men. AIDS Behav. 2010;14(2):351–358. [DOI] [PubMed] [Google Scholar]
- 88. Balaji AB, Oster AM, Viall AH, Heffelfinger JD, Mena LA, Toledo CA. Role flexing: how community, religion, and family shape the experiences of young black men who have sex with men. AIDS Patient Care STDS. 2012;26(12):730–737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Amornkul PN, Vandenhoudt H, Nasokho P, et al. HIV prevalence and associated risk factors among individuals aged 13-34 years in rural western Kenya. PLoS One. 2009;4(7):e6470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Hall HI, Tang T, Westfall AO, Mugavero MJ. HIV care visits and time to viral suppression, 19 U.S. jurisdictions, and implications for treatment, prevention and the National HIV/AIDS Strategy. PLoS One. 2013;8(12):e84318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Campbell JD, Moore D, Degerman R, et al. HIV-infected Ugandan adults taking antiretroviral therapy with CD4 counts >200 cells/μL who discontinue cotrimoxazole prophylaxis have increased risk of malaria and diarrhea. Clin Infect Dis. 2012;54(8):1204–1211. [DOI] [PubMed] [Google Scholar]
- 92. Loosier PS, Dittus PJ. Group differences in risk across three domains using an expanded measure of sexual orientation. J Prim Prev. 2010;31(5-6):261–272. [DOI] [PubMed] [Google Scholar]
- 93. Xu F, Stoner BP, Taylor SN, et al. Use of home-obtained vaginal swabs to facilitate rescreening for Chlamydia trachomatis infections: two randomized controlled trials. Obstet Gynecol. 2011;118(2 pt 1):231–239. [DOI] [PubMed] [Google Scholar]
- 94. Kroeger K, Taylor AW, Marlow HM, et al. Perceptions of door-to-door HIV counselling and testing in Botswana. Sahara J. 2011;8(4):171–178. [DOI] [PubMed] [Google Scholar]
- 95. Winston CA, Navin TR, Becerra JE, et al. Unexpected decline in tuberculosis cases coincident with economic recession—United States, 2009. BMC Public Health. 2011;11:846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Mitruka K, Winston CA, Navin TR. Predictors of failure in timely tuberculosis treatment completion, United States. Int J Tuberc Lung Dis. 2012;16(8):1075–1082. [DOI] [PubMed] [Google Scholar]
- 97. Miramontes R, Winston CA, Haddad MB, Moonan PK. Use of tuberculosis genotyping for postoutbreak monitoring. J Public Health Manag Pract. 2012;18(4):375–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Marks SM, Magee E, Robison V. Patients diagnosed with tuberculosis at death or who died during therapy: association with the human immunodeficiency virus. Int J Tuberc Lung Dis. 2011;15(4):465–470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Manangan L, Elmore K, Lewis B, et al. Disparities in tuberculosis between Asian/Pacific Islanders and non-Hispanic whites, United States, 1993-2006. Int J Tuberc Lung Dis. 2009;13(9):1077–1085. [PubMed] [Google Scholar]
- 100. Cavanaugh JS, Shah NS, Cain KP, Winston CA. Survival among patients with HIV infection and smear-negative pulmonary tuberculosis—United States, 1993-2006. PLoS One. 2012;7(10):e47855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Althomsons SP, Kammerer JS, Shang N, Navin TR. Using routinely reported tuberculosis genotyping and surveillance data to predict tuberculosis outbreaks. PLoS One. 2012;7(11):e48754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Zheteyeva YA, Tosh P, Patel PR, et al. Hepatitis B outbreak associated with a home health care agency serving multiple assisted living facilities in Texas, 2008-2010. Am J Infect Control. 2014;42(1):77–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Myers JE, Bodach S, Cutler BH, Shepard CW, Philippou C, Branson BM. Acceptability of home self-tests for HIV in New York City, 2006. Am J Public Health. 2014;104(12):e46–e48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Espinoza L, Hall HI, Hu X. Diagnoses of HIV infection among Hispanics/Latinos in 40 states and Puerto Rico, 2006-2009. J Acquir Immune Defic Syndr. 2012;60(2):205–213. [DOI] [PubMed] [Google Scholar]
- 105. Wolitski RJ, Kidder DP, Pals SL, et al. Randomized trial of the effects of housing assistance on the health and risk behaviors of homeless and unstably housed people living with HIV. AIDS Behav. 2010;14(3):493–503. [DOI] [PubMed] [Google Scholar]
- 106. Parvez FM, Lobato MN, Greifinger RB. Tuberculosis control: lessons for outbreak preparedness in correctional facilities. J Correct Health Care. 2010;16(3):239–242. [DOI] [PubMed] [Google Scholar]
- 107. Hennessey KA, Bangsberg DR, Weinbaum C, Hahn JA. Hepatitis A seroprevalence and risk factors among homeless adults in San Francisco: should homelessness be included in the risk-based strategy for vaccination? Public Health Rep. 2009;124(6):813–817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Wang LY, Denniston M, Lee S, Galuska D, Lowry R. Long-term health and economic impact of preventing and reducing overweight and obesity in adolescence. J Adolesc Health. 2010;46(5):467–473. [DOI] [PubMed] [Google Scholar]
- 109. Steiner RJ, Michael SL, Hall JE, Barrios LC, Robin L. Youth violence and connectedness in adolescence: what are the implications for later sexually transmitted infections? J Adolesc Health. 2014;54(3):312–318.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Lee SM, Nihiser A, Strouse D, Das B, Michael S, Huhman M. Correlates of children and parents being physically active together. J Phys Act Health. 2010;7(6):776–783. [DOI] [PubMed] [Google Scholar]
- 111. Lowry R, Lee SM, Fulton JE, Demissie Z, Kann L. Obesity and other correlates of physical activity and sedentary behaviors among US high school students. J Obes. 2013;2013:276318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Lowry R, Robin L, Kann L, Galuska DA. Associations of body mass index with sexual risk-taking and injection drug use among US high school students. J Obes. 2014;2014:816071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Foti K, Eaton D. Associations of selected health risk behaviors with self-rated health status among U.S. high school students. Public Health Rep. 2010;125(5):771–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Eaton DK, Foti K, Brener ND, Crosby AE, Flores G, Kann L. Associations between risk behaviors and suicidal ideation and suicide attempts: do racial/ethnic variations in associations account for increased risk of suicidal behaviors among Hispanic/Latina 9th- to 12th-grade female students? Arch Suicide Res. 2011;15(2):113–126. [DOI] [PubMed] [Google Scholar]
- 115. Bogart LM, Elliott MN, Kanouse DE, et al. Bogart et al. respond. Am J Public Health. 2013;103(11):e1–e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Lowry R, Crosby AE, Brener ND, Kann L. Suicidal thoughts and attempts among U.S. high school students: trends and associated health-risk behaviors, 1991-2011. J Adolesc Health. 2014;54(1):100–108. [DOI] [PubMed] [Google Scholar]
- 117. Olsen EO, Hertz MF, Shults RA, Hamburger ME, Lowry R. Healthy People 2010 objectives for unintentional injury and violence among adolescents. Trends from the National Youth Risk Behavior Survey, 1999-2009. Am J Prev Med. 2011;41(6):551–558. [DOI] [PubMed] [Google Scholar]
- 118. Kann L, Olsen EO, McManus T, et al. Sexual identity, sex of sexual contacts, and health-risk behaviors among students in grades 9-12—youth risk behavior surveillance, selected sites, United States, 2001-2009. MMWR Surveill Summ. 2011;60(7):1–133. [PubMed] [Google Scholar]
- 119. Demissie Z, Lowry R, Eaton DK, Hertz MF, Lee SM. Associations of school violence with physical activity among U.S. high school students. J Phys Act Health. 2014;11(4):705–711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Jones SE, Pezzi C, Rodriguez-Lainz A, Whittle L. Health risk behaviors by length of time in the United States among high school students in five sites. J Immigr Minor Health. 2016;18(1):150–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Lowry R, Eaton DK, Foti K, McKnight-Eily L, Perry G, Galuska DA. Association of sleep duration with obesity among US high school students. J Obes. 2012;2012:476914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Eaton DK, McKnight-Eily LR, Lowry R, Perry GS, Presley-Cantrell L, Croft JB. Prevalence of insufficient, borderline, and optimal hours of sleep among high school students—United States, 2007. J Adolesc Health. 2010;46(4):399–401. [DOI] [PubMed] [Google Scholar]
- 123. Steiner RJ, Swartzendruber AL, Rose E, DiClemente RJ. Monitoring knowledge among family, sexually transmitted infections, and sexual partnership characteristics of African American adolescent females. Sex Transm Dis. 2014;41(10):601–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Wechsler H. Addressing youth health disparities: the CDC perspective. Health Promot Pract. 2010;11(suppl 3):7s–8s. [DOI] [PubMed] [Google Scholar]
- 125. Liddon N, Michael SL, Dittus P, Markowitz LE. Maternal underestimation of child’s sexual experience: suggested implications for HPV vaccine uptake at recommended ages. J Adolesc Health. 2013;53(5):674–676. [DOI] [PubMed] [Google Scholar]
- 126. Jones SE, Saraiya M, Miyamoto J, Berkowitz Z. Trends in sunscreen use among U.S. high school students: 1999-2009. J Adolesc Health. 2012;50(3):304–307. [DOI] [PubMed] [Google Scholar]
- 127. Everett Jones S, O’Malley Olsen E, Michael SL, Saraiya M. Association of UV index and sunscreen use among white high school students in the United States. J Sch Health. 2013;83(10):750–756. [DOI] [PubMed] [Google Scholar]
- 128. Foti K, Balaji A, Shanklin S. Uses of Youth Risk Behavior Survey and School Health Profiles data: applications for improving adolescent and school health. J Sch Health. 2011;81(6):345–354. [DOI] [PubMed] [Google Scholar]
- 129. Guy GP, Jr, Berkowitz Z, Everett Jones S, Holman DM, Garnett E, Watson M. Trends in indoor tanning among US high school students, 2009-2013. JAMA Dermatol. 2015;151(4):448–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. O’Malley Olsen E, Eaton DK, Park S, Brener ND, Blanck HM. Comparing methods for assessing beverage intake among high school students. Am J Health Behav. 2014;38(1):114–123. [DOI] [PubMed] [Google Scholar]
- 131. Olsen EO, Shults RA, Eaton DK. Texting while driving and other risky motor vehicle behaviors among US high school students. Pediatrics. 2013;131(6):e1708–e1715. [DOI] [PubMed] [Google Scholar]
- 132. Lowry R, Eaton DK, Brener ND, Kann L. Prevalence of health-risk behaviors among Asian American and Pacific Islander high school students in the U.S., 2001-2007. Public Health Rep. 2011;126(1):39–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Jones SE, Kann L, Pechacek TF. Cigarettes smoked per day among high school students in the U.S., 1991-2009. Am J Prev Med. 2011;41(3):297–299. [DOI] [PubMed] [Google Scholar]
- 134. Foti K, Lowry R. Trends in perceived overweight status among overweight and nonoverweight adolescents. Arch Pediatr Adolesc Med. 2010;164(7):636–642. [DOI] [PubMed] [Google Scholar]
- 135. Everett Jones S, Caraballo RS. Usual source of cigarettes and alcohol among US high school students. J Sch Health. 2014;84(8):493–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Fogel CI, Crandell JL, Neevel AM, et al. Efficacy of an adapted HIV and sexually transmitted infection prevention intervention for incarcerated women: a randomized controlled trial. Am J Public Health. 2015;105(4):802–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. van Griensven F, Thienkrua W, McNicholl J, et al. Evidence of an explosive epidemic of HIV infection in a cohort of men who have sex with men in Thailand. AIDS. 2013;27(5):825–832. [DOI] [PubMed] [Google Scholar]
- 138. Linkins RW, Chonwattana W, Holtz TH, et al. Hepatitis A and hepatitis B infection prevalence and associated risk factors in men who have sex with men, Bangkok, 2006-2008. J Med Virol. 2013;85(9):1499–1505. [DOI] [PubMed] [Google Scholar]
- 139. McCree DH, Millett G, Baytop C, et al. Lessons learned from use of social network strategy in HIV testing programs targeting African American men who have sex with men. Am J Public Health. 2013;103(10):1851–1856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Oster AM, Johnson CH, Le BC, et al. Trends in HIV prevalence and HIV testing among young MSM: five United States cities, 1994-2011. AIDS Behav. 2014;18(suppl 3):S237–S247. [DOI] [PubMed] [Google Scholar]
- 141. Crepaz N, Marshall KJ, Aupont LW, et al. The efficacy of HIV/STI behavioral interventions for African American females in the United States: a meta-analysis. Am J Public Health. 2009;99(11):2069–2078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Imai K, Sutton MY, Mdodo R, Del Rio C. HIV and menopause: a systematic review of the effects of HIV infection on age at menopause and the effects of menopause on response to antiretroviral therapy. Obstet Gynecol Int. 2013;2013:340309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Zabina H, Kissin D, Pervysheva E, et al. Abandonment of infants by HIV-positive women in Russia and prevention measures. Reprod Health Matters. 2009;17(33):162–170. [DOI] [PubMed] [Google Scholar]
- 144. O’Leary A. Are dual-method messages undermining STI/HIV prevention? Infect Dis Obstet Gynecol. 2011;2011:691210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Dunne EF, Sternberg M, Markowitz LE, et al. Human papillomavirus (HPV) 6, 11, 16, and 18 prevalence among females in the United States—National Health and Nutrition Examination Survey, 2003-2006: opportunity to measure HPV vaccine impact? J Infect Dis. 2011;204(4):562–565. [DOI] [PubMed] [Google Scholar]
- 146. Leichliter JS, Lewis DA, Sternberg M, Habel MA, Paz-Bailey G. Health care seeking among men with genital ulcer disease in South Africa: correlates and relationship to human immunodeficiency virus-1 and herpes simplex virus type 2 detection and shedding. Sex Transm Dis. 2011;38(9):865–870. [DOI] [PubMed] [Google Scholar]
- 147. Taylor MM, Ebrahim S, Abiola N, et al. Correlates of syphilis seropositivity and risk for syphilis-associated adverse pregnancy outcomes among women attending antenatal care clinics in the Democratic Republic of Congo. Int J STD AIDS. 2014;25(10):716–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Liddon N, Hood J, Wynn BA, Markowitz LE. Acceptability of human papillomavirus vaccine for males: a review of the literature. J Adolesc Health. 2010;46(2):113–123. [DOI] [PubMed] [Google Scholar]
- 149. Robitz R, Gottlieb SL, De Rosa CJ, et al. Parent attitudes about school requirements for human papillomavirus vaccine in high-risk communities of Los Angeles, California. Cancer Epidemiol Biomarkers Prev. 2011;20(7):1421–1429. [DOI] [PubMed] [Google Scholar]
- 150. Cullen KA, Stokley S, Markowitz LE. Uptake of human papillomavirus vaccine among adolescent males and females: immunization information system sentinel sites, 2009-2012. Acad Pediatr. 2014;14(5):497–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Gottlieb SL, Xu F, Brunham RC. Screening and treating chlamydia trachomatis genital infection to prevent pelvic inflammatory disease: interpretation of findings from randomized controlled trials. Sex Transm Dis. 2013;40(2):97–102. [DOI] [PubMed] [Google Scholar]
- 152. Habel MA, Dittus PJ, De Rosa CJ, Chung EQ, Kerndt PR. Daily participation in sports and students’ sexual activity. Perspect Sex Reprod Health. 2010;42(4):244–250. [DOI] [PubMed] [Google Scholar]
- 153. Forhan SE, Gottlieb SL, Sternberg MR, et al. Prevalence of sexually transmitted infections among female adolescents aged 14 to 19 in the United States. Pediatrics. 2009;124(6):1505–1512. [DOI] [PubMed] [Google Scholar]
- 154. Aral SO, Ward H. Behavioral convergence: implications for mathematical models of sexually transmitted infection transmission. J Infect Dis. 2014;210(suppl 2):S600–S604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Taylor MM, Collier MG, Winscott MM, Mickey T, England B. Reticence to prescribe: utilization of expedited partner therapy among obstetrics providers in Arizona. Int J STD AIDS. 2011;22(8):449–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Finlay A, Lancaster J, Holtz TH, Weyer K, Miranda A, van der Walt M. Patient- and provider-level risk factors associated with default from tuberculosis treatment, South Africa, 2002: a case-control study. BMC Public Health. 2012;12:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Magee E, Tryon C, Forbes A, Heath B, Manangan L. The national tuberculosis surveillance system training program to ensure accuracy of tuberculosis data. J Public Health Manag Pract. 2011;17(5):427–430. [DOI] [PubMed] [Google Scholar]
- 158. Bloss E, Newbill K, Peto H, et al. Challenges and opportunities in a tuberculosis outbreak investigation in southern Mississippi, 2005-2007. South Med J. 2011;104(11):731–735. [DOI] [PubMed] [Google Scholar]
- 159. Powell K, Han D, Hung NV, et al. Prevalence and risk factors for tuberculosis infection among personnel in two hospitals in Viet Nam. Int J Tuberc Lung Dis. 2011;15(12):1643–1649. [DOI] [PubMed] [Google Scholar]
- 160. Byrd KK, Lu PJ, Murphy TV. Baseline hepatitis B vaccination coverage among persons with diabetes before implementing a U.S. recommendation for vaccination. Vaccine. 2012;30(23):3376–3382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Byrd KK, Lu PJ, Murphy TV. Hepatitis B vaccination coverage among health-care personnel in the United States. Public Health Rep. 2013;128(6):498–509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162. Spradling PR, Williams RE, Xing J, Soyemi K, Towers J. Serologic testing for protection against hepatitis B virus infection among students at a health sciences university in the United States. Infect Control Hosp Epidemiol. 2012;33(7):732–736. [DOI] [PubMed] [Google Scholar]
- 163. Liu G, Holmberg SD, Kamili S, Xu F. Racial disparities in the proportion of current, unresolved hepatitis C virus infections in the United States, 2003-2010. Dig Dis Sci. 2014;59(8):1950–1957. [DOI] [PubMed] [Google Scholar]
- 164. Weinbaum CM, Mast EE, Ward JW. Recommendations for identification and public health management of persons with chronic hepatitis B virus infection. Hepatology. 2009;49(suppl 5):S35–S44. [DOI] [PubMed] [Google Scholar]
- 165. Thompson ND, Perz JF, Moorman AC, Holmberg SD. Nonhospital health care-associated hepatitis B and C virus transmission: United States, 1998-2008. Ann Intern Med. 2009;150(1):33–39. [DOI] [PubMed] [Google Scholar]
- 166. Roberts H, Myles RL, Truman BI, Dean HD. Association of employee attributes and exceptional performance rating at a National Center of the US Centers for Disease Control and Prevention, 2011. J Public Health Manag Pract. 2015;21(4):E10–E17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167. Semaan S, Leinhos M, Neumann MS. Public health strategies for prevention and control of HSV-2 in persons who use drugs in the United States. Drug Alcohol Depend. 2013;131(3):182–197. [DOI] [PubMed] [Google Scholar]
- 168. Fitz Harris LF, Toledo L, Dunbar E, Aquino GA, Nesheim SR. Program collaboration and service integration activities among HIV programs in 59 U.S. health departments. Public Health Rep. 2014;129(suppl 1):33–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. Wang LY, Nichols LP, Austin SB. The economic effect of Planet Health on preventing bulimia nervosa. Arch Pediatr Adolesc Med. 2011;165(8):756–762. [DOI] [PubMed] [Google Scholar]
- 170. Wang LY, Vernon-Smiley M, Gapinski MA, Desisto M, Maughan E, Sheetz A. Cost-benefit study of school nursing services. JAMA Pediatr. 2014;168(7):642–648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171. Rasberry CN, Cheung K, Buckley R, et al. Indicators of asthma control among students in a rural, school-based asthma management program. J Asthma. 2014;51(8):876–885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172. Nihiser AJ, Lee SM, Wechsler H, et al. BMI measurement in schools. Pediatrics. 2009;124(suppl 1):S89–S97. [DOI] [PubMed] [Google Scholar]
- 173. Markham CM, Peskin MF, Shegog R, et al. Behavioral and psychosocial effects of two middle school sexual health education programs at tenth-grade follow-up. J Adolesc Health. 2014;54(2):151–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174. Denniston M, Brener N. A comparison of mail and telephone administration of district-level questionnaires for the School Health Policies and Programs Study (SHPPS) 2006: effects on estimates and data quality. J Sch Health. 2010;80(6):304–311. [DOI] [PubMed] [Google Scholar]
- 175. Pitt Barnes S, Robin L, O’Toole TP, Dawkins N, Kettel Khan L, Leviton LC. Results of evaluability assessments of local wellness policies in 6 US school districts. J Sch Health. 2011;81(8):502–511. [DOI] [PubMed] [Google Scholar]
- 176. Brener ND, Wechsler H, Kann L. Challenges in and strategies for the surveillance of school health policies and practices: a commentary. J Sch Health. 2014;84(11):687–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177. Brener ND, Chriqui JF, O’Toole TP, Schwartz MB, McManus T. Establishing a baseline measure of school wellness-related policies implemented in a nationally representative sample of school districts. J Am Diet Assoc. 2011;111(6):894–901. [DOI] [PubMed] [Google Scholar]
- 178. Brener ND, Pejavara A, McManus T. Applying the School Health Index to a nationally representative sample of schools: update for 2006. J Sch Health. 2011;81(2):81–90. [DOI] [PubMed] [Google Scholar]
- 179. Brener ND, Wechsler H, McManus T. How school healthy is your state? A state-by-state comparison of school health practices related to a healthy school environment and health education. J Sch Health. 2013;83(10):743–749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180. Kann L, Kinchen S, Modzelski B, et al. ILI-related school dismissal monitoring system: an overview and assessment. Disaster Med Public Health Prep. 2012;6(2):104–112. [DOI] [PubMed] [Google Scholar]
- 181. Barrios LC, Koonin LM, Kohl KS, Cetron M. Selecting nonpharmaceutical strategies to minimize influenza spread: the 2009 influenza A (H1N1) pandemic and beyond. Public Health Rep. 2012;127(6):565–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182. Brener ND, McManus T, Wechsler H, Kann L. Trends in professional development for and collaboration by health education teachers—41 states, 2000-2010. J Sch Health. 2013;83(10):734–742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183. Rasberry CN, Morris E, Lesesne CA, et al. Communicating with school nurses about sexual orientation and sexual health: perspectives of teen young men who have sex with men. J Sch Nurs. 2015;31(5):334–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184. O’Malley Olsen E, Kann L, Vivolo-Kantor A, Kinchen S, McManus T. School violence and bullying among sexual minority high school students, 2009-2011. J Adolesc Health. 2014;55(3):432–438. [DOI] [PubMed] [Google Scholar]
- 185. Eaton DK, Brener ND, Kann L, et al. Computer availability and principals’ perceptions of online surveys(*). J Sch Health. 2011;81(7):365–373. [DOI] [PubMed] [Google Scholar]
- 186. Balaji AB, Brener ND, McManus T. Variation in school health policies and programs by demographic characteristics of US schools, 2006. J Sch Health. 2010;80(12):599–613. [DOI] [PubMed] [Google Scholar]
- 187. Warren-Jeanpiere L, Jones S, Sutton MY. Health administrator perspectives on human immunodeficiency virus/acquired immunodeficiency syndrome prevention and services at historically black colleges and universities. J Am Coll Health. 2011;59(4):327–329. [DOI] [PubMed] [Google Scholar]
- 188. Sutton MY, Hardnett FP, Wright P, et al. HIV/AIDS knowledge scores and perceptions of risk among African American students attending historically black colleges and universities. Public Health Rep. 2011;126(5):653–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189. Miller KS, Maxwell KD, Fasula AM, Parker JT, Zackery S, Wyckoff SC. Pre-risk HIV-prevention paradigm shift: the feasibility and acceptability of the Parents Matter! program in HIV risk communities. Public Health Rep. 2010;125 (suppl 1):38–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190. Psaros C, Haberer JE, Katabira E, et al. An intervention to support HIV preexposure prophylaxis adherence in HIV-serodiscordant couples in Uganda. J Acquir Immune Defic Syndr. 2014;66(5):522–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191. Sutton MY, Lasswell SM, Lanier Y, Miller KS. Impact of parent-child communication interventions on sex behaviors and cognitive outcomes for black/African-American and Hispanic/Latino youth: a systematic review, 1988-2012. J Adolesc Health. 2014;54(4):369–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192. Smith BD, Kalayil EJ, Patel-Larson A, Chen B, Vaughan M. Retaining clients in an outcome monitoring evaluation study: HIV prevention efforts in community settings. Eval Program Plann. 2012;35(1):16–24. [DOI] [PubMed] [Google Scholar]
- 193. Lasry A, Sansom SL, Hicks KA, Uzunangelov V. Allocating HIV prevention funds in the United States: recommendations from an optimization model. PLoS One. 2012;7(6):e37545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194. O’Leary A, Jemmott JB III, Stevens R, Rutledge SE, Icard LD. Optimism and education buffer the effects of syndemic conditions on HIV status among African American men who have sex with men. AIDS Behav. 2014;18(11):2080–2088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195. Jorgensen CM, Carnes CA. Lessons learned from exploratory research about viral hepatitis. Health Promot Pract. 2013;14(3):364–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196. Smith BD, Jorgensen C, Zibbell JE, Beckett GA. Centers for Disease Control and Prevention initiatives to prevent hepatitis C virus infection: a selective update. Clin Infect Dis. 2012;55(suppl 1):S49–S53. [DOI] [PubMed] [Google Scholar]
- 197. Ward JW, Valdiserri RO, Koh HK. Hepatitis C virus prevention, care, and treatment: from policy to practice. Clin Infect Dis. 2012;55(suppl 1):S58–S63. [DOI] [PubMed] [Google Scholar]
- 198. Ward JW, Lok AS, Thomas DL, El-Serag HB, Kim WR. Report on a single-topic conference on “chronic viral hepatitis—strategies to improve effectiveness of screening and treatment.” Hepatology. 2012;55(1):307–315. [DOI] [PubMed] [Google Scholar]
- 199. Klevens RM, Moorman AC. Hepatitis C virus: an overview for dental health care providers. J Am Dent Assoc. 2013;144(12):1340–1347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200. Jewett A, Al-Tayyib AA, Ginnett L, Smith BD. Successful integration of hepatitis C virus point-of-care tests into the Denver Metro Health Clinic. AIDS Res Treat. 2013;2013:528904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201. Zeremski M, Dimova RB, Zavala R, et al. Hepatitis C virus-related knowledge and willingness to receive treatment among patients on methadone maintenance. J Addict Med. 2014;8(4):249–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202. Ford JV, Barnes R, Rompalo A, Hook EW III. Sexual health training and education in the U.S. Public Health Rep. 2013;128(suppl 1):96–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203. Smith DK, Toledo L, Smith DJ, Adams MA, Rothenberg R. Attitudes and program preferences of African-American urban young adults about pre-exposure prophylaxis (PrEP). AIDS Educ Prev. 2012;24(5):408–421. [DOI] [PubMed] [Google Scholar]
- 204. Joseph HA, Fasula AM, Morgan RL, et al. “The anticipation alone could kill you”: past and potential clients’ perspectives on HIV testing in non-health care settings. AIDS Educ Prev. 2011;23(6):577–594. [DOI] [PubMed] [Google Scholar]
- 205. Mizuno Y, Borkowf CB, Ayala G, Carballo-Dieguez A, Millett GA. Correlates of sexual risk for HIV among US-born and foreign-born Latino men who have sex with men (MSM): an analysis from the Brothers y Hermanos study. J Immigr Minor Health. 2015;17(1):47–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206. Hood JE, Friedman AL. Unveiling the hidden epidemic: a review of stigma associated with sexually transmissible infections. Sex Health. 2011;8(2):159–170. [DOI] [PubMed] [Google Scholar]
- 207. Oster AM, Wiegand RE, Sionean C, et al. Understanding disparities in HIV infection between black and white MSM in the United States. AIDS. 2011;25(8):1103–1112. [DOI] [PubMed] [Google Scholar]
- 208. Bertolli J, Garland PM, Valverde EE, Beer L, Fagan JL, Hart C. Missed connections: HIV-infected people never in care. Public Health Rep. 2013;128(2):117–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209. Hutchinson AB, Patel P, Sansom SL, et al. Cost-effectiveness of pooled nucleic acid amplification testing for acute HIV infection after third-generation HIV antibody screening and rapid testing in the United States: a comparison of three public health settings. PLoS Med. 2010;7(9):e1000342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210. Mansergh G, Koblin BA, McKirnan DJ, et al. An intervention to reduce HIV risk behavior of substance-using men who have sex with men: a two-group randomized trial with a nonrandomized third group. PLoS Med. 2010;7(8):e1000329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211. Prejean J, Tang T, Hall HI. HIV diagnoses and prevalence in the southern region of the United States, 2007-2010. J Community Health. 2013;38(3):414–426. [DOI] [PubMed] [Google Scholar]
- 212. Walker FJ, Llata E, Doshani M, et al. HIV, chlamydia, gonorrhea, and primary and secondary syphilis among American Indians and Alaska Natives within Indian Health Service areas in the United States, 2007-2010. J Community Health. 2015;40(3):484–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213. Sutton MY, Lanier YA, Willis LA, et al. Strengthening the network of mentored, underrepresented minority scientists and leaders to reduce HIV-related health disparities. Am J Public Health. 2013;103(12):2207–2214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214. Beer L, Fagan JL, Valverde E, Bertolli J. Never in Care Project. Health-related beliefs and decisions about accessing HIV medical care among HIV-infected persons who are not receiving care. AIDS Patient Care STDS. 2009;23(9):785–792. [DOI] [PubMed] [Google Scholar]
- 215. Beer L, Fagan JL, Garland P, et al. Medication-related barriers to entering HIV care. AIDS Patient Care STDS. 2012;26(4):214–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216. Higa DH, Crepaz N, Marshall KJ, et al. A systematic review to identify challenges of demonstrating efficacy of HIV behavioral interventions for gay, bisexual, and other men who have sex with men (MSM). AIDS Behav. 2013;17(4):1231–1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217. Fraze JL, Uhrig JD, Davis KC, et al. Applying core principles to the design and evaluation of the “Take Charge. Take the Test” campaign: what worked and lessons learned. Public Health. 2009;123(suppl 1):e23–e30. [DOI] [PubMed] [Google Scholar]
- 218. Collins CB, Jr, Hearn KD, Whittier DN, Freeman A, Stallworth JD, Phields M. Implementing packaged HIV-prevention interventions for HIV-positive individuals: considerations for clinic-based and community-based interventions. Public Health Rep. 2010;125(suppl 1):55–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219. Abdul-Quader AS, Collins C. Identification of structural interventions for HIV/AIDS prevention: the concept mapping exercise. Public Health Rep. 2011;126(6):777–788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220. Collins CB, Jr, Edwards AE, Jones PL, Kay L, Cox PJ, Puddy RW. A comparison of the Interactive Systems Framework (ISF) for Dissemination and Implementation and the CDC Division of HIV/AIDS Prevention’s Research-to-Practice model for behavioral interventions. Am J Community Psychol. 2012;50(3-4):518–529. [DOI] [PubMed] [Google Scholar]
- 221. Neumann MS, O’Donnell L, Doval AS, et al. Effectiveness of the VOICES/VOCES sexually transmitted disease/human immunodeficiency virus prevention intervention when administered by health department staff: does it work in the “real world”? Sex Transm Dis. 2011;38(2):133–139. [DOI] [PubMed] [Google Scholar]
- 222. Raiford JL, Seth P, DiClemente RJ. What girls won’t do for love: human immunodeficiency virus/sexually transmitted infections risk among young African-American women driven by a relationship imperative. J Adolesc Health. 2013;52(5):566–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223. Mgbere O, Khuwaja S, Bell TK, et al. Managing the personal side of health care among patients with HIV/AIDS. J Int Assoc Provid AIDS Care. 2017;16(2):149–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224. Taylor MM, Mickey T, Winscott M, James H, Kenney K, England B. Improving partner services by embedding disease intervention specialists in HIV-clinics. Sex Transm Dis. 2010;37(12):767–770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225. Newman LM, Dowell D, Bernstein K, et al. A tale of two gonorrhea epidemics: results from the STD surveillance network. Public Health Rep. 2012;127(3):282–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226. Mitruka K, Blake H, Ricks P, et al. A tuberculosis outbreak fueled by cross-border travel and illicit substances: Nevada and Arizona. Public Health Rep. 2014;129(1):78–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227. Tohme RA, Holmberg SD. Transmission of hepatitis C virus infection through tattooing and piercing: a critical review. Clin Infect Dis. 2012;54(8):1167–1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228. Suryaprasad AG, White JZ, Xu F, et al. Emerging epidemic of hepatitis C virus infections among young nonurban persons who inject drugs in the United States, 2006-2012. Clin Infect Dis. 2014;59(10):1411–1419. [DOI] [PubMed] [Google Scholar]
- 229. Ward JW. Testing for HCV: the first step in preventing disease transmission and improving health outcomes for HCV-infected individuals. Antivir Ther. 2012;17(7 pt B):1397–1401. [DOI] [PubMed] [Google Scholar]
- 230. Williams IT, Bell BP, Kuhnert W, Alter MJ. Incidence and transmission patterns of acute hepatitis C in the United States, 1982-2006. Arch Intern Med. 2011;171(3):242–248. [DOI] [PubMed] [Google Scholar]
- 231. Holmberg SD. Molecular epidemiology of health care-associated transmission of hepatitis B and C viruses. Clin Liver Dis. 2010;14(1):37–48. [DOI] [PubMed] [Google Scholar]
- 232. Holmberg SD. Hepatitis C virus and the infectious diseases community. Clin Infect Dis. 2012;55(suppl 1):S1–S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233. Averhoff FM, Glass N, Holtzman D. Global burden of hepatitis C: considerations for healthcare providers in the United States. Clin Infect Dis. 2012;55(suppl 1):S10–S15. [DOI] [PubMed] [Google Scholar]
- 234. Ramachandran S, Campo DS, Dimitrova ZE, Xia GL, Purdy MA, Khudyakov YE. Temporal variations in the hepatitis C virus intrahost population during chronic infection. J Virol. 2011;85(13):6369–6380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235. Robinson SJ, Stellato A, Stephens J, Kirby S, Forsythe A, Ivankovich MB. On the road to well-being: the development of a communication framework for sexual health. Public Health Rep. 2013;128(suppl 1):43–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236. Sapiano TN, Moore A, Kalayil EJ, et al. Evaluation of an HIV prevention intervention designed for African American women: results from the SISTA Community-Based Organization Behavioral Outcomes Project. AIDS Behav. 2013;17(3):1052–1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237. Charania MR, Crepaz N, Guenther-Gray C, et al. Efficacy of structural-level condom distribution interventions: a meta-analysis of U.S. and international studies, 1998-2007. AIDS Behav. 2011;15(7):1283–1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238. Collins CB., Jr Evidence based interventions for preventing HIV transmission: commentary on Rotheram-Borus et al. (2009). AIDS Behav. 2009;13(3):414–419; discussion 420-423. [DOI] [PubMed] [Google Scholar]
- 239. An Q, Prejean J, McDavid Harrison K, Fang X. Association between community socioeconomic position and HIV diagnosis rate among adults and adolescents in the United States, 2005 to 2009. Am J Public Health. 2013;103(1):120–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240. Shrestha RK, Sansom SL, Kimbrough L, et al. Cost-effectiveness of using social networks to identify undiagnosed HIV infection among minority populations. J Public Health Manag Pract. 2010;16(5):457–464. [DOI] [PubMed] [Google Scholar]
- 241. VanHandel M, Beltrami JF, MacGowan RJ, Borkowf CB, Margolis AD. Newly identified HIV infections in correctional facilities, United States, 2007. Am J Public Health. 2012;102(suppl 2):S201–S204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242. Jafa K, McElroy P, Fitzpatrick L, et al. HIV transmission in a state prison system, 1988-2005. PLoS One. 2009;4(5):e5416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243. Fasula AM, Fogel CI, Gelaude D, Carry M, Gaiter J, Parker S. Project power: adapting an evidence-based HIV/STI prevention intervention for incarcerated women. AIDS Educ Prev. 2013;25(3):203–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244. Satterwhite CL, Newman D, Collins D, Torrone E. Chlamydia screening and positivity in juvenile detention centers, United States, 2009-2011. Womens Health. 2014;54(8):712–725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245. Peterman TA, Newman DR, Goldberg M, et al. Screening male prisoners for chlamydia trachomatis: impact on test positivity among women from their neighborhoods who were tested in family planning clinics. Sex Transm Dis. 2009;36(7):425–429. [DOI] [PubMed] [Google Scholar]
- 246. Lewis FM, Schillinger JA, Taylor M, et al. Needle in a haystack: the yield of syphilis outreach screening at 5 US sites—2000 to 2007. J Public Health Manag Pract. 2011;17(6):513–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247. Eugene JM, Hoover KW, Tao G, Kent CK. Higher yet suboptimal chlamydia testing rates at community health centers and outpatient clinics compared with physician offices. Am J Public Health. 2012;102(8):e26–e29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248. Parija D, Patra TK, Kumar AM, et al. Impact of awareness drives and community-based active tuberculosis case finding in Odisha, India. Int J Tuberc Lung Dis. 2014;18(9):1105–1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249. Fleming EB, LeBlanc TT, Reid LC. The status of HIV prevention efforts for women in correctional facilities. J Womens Health (Larchmt). 2013;22(12):1005–1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250. Dean HD. Foreword: HIV/AIDS prevention in the Hispanic/Latino community. AIDS Educ Prev. 2009;21(5 suppl):1–2. [DOI] [PubMed] [Google Scholar]
- 251. Farnham PG, Sansom SL, Hutchinson AB. How much should we pay for a new HIV diagnosis? A mathematical model of HIV screening in US clinical settings. Med Decis Making. 2012;32(3):459–469. [DOI] [PubMed] [Google Scholar]
- 252. Hutchinson AB, Farnham PG, Lyss SB, White DA, Sansom SL, Branson BM. Emergency department HIV screening with rapid tests: a cost comparison of alternative models. AIDS Educ Prev. 2011;23(suppl 3):58–69. [DOI] [PubMed] [Google Scholar]
- 253. Lasry A, Carter MW, Zaric GS. Allocating funds for HIV/AIDS: a descriptive study of KwaDukuza, South Africa. Health Policy Plan. 2011;26(1):33–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254. Mansergh G, Valdiserri RO, Yakovchenko V, Koh H. Aligning resources to fight HIV/AIDS in the United States: funding to states through the US Department of Health and Human Services. J Acquir Immune Defic Syndr. 2012;59(5):516–522. [DOI] [PubMed] [Google Scholar]
- 255. Lin F, Lasry A, Sansom SL, Wolitski RJ. Estimating the impact of state budget cuts and redirection of prevention resources on the HIV epidemic in 59 California local health departments. PLoS One. 2013;8(3):e55713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256. Hall HI, Green TA, Wolitski RJ, et al. Estimated future HIV prevalence, incidence, and potential infections averted in the United States: a multiple scenario analysis. J Acquir Immune Defic Syndr. 2010;55(2):271–276. [DOI] [PubMed] [Google Scholar]
- 257. Smith DK, Taylor A, Kilmarx PH, et al. Male circumcision in the United States for the prevention of HIV infection and other adverse health outcomes: report from a CDC consultation [published erratum appears in Public Health Rep. 2010;125(4):517]. Public Health Rep. 2010;125(suppl 1):72–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 258. El Bcheraoui C, Zhang X, Cooper CS, Rose CE, Kilmarx PH, Chen RT. Rates of adverse events associated with male circumcision in U.S. medical settings, 2001 to 2010. JAMA Pediatr. 2014;168(7):625–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259. Linley L, Prejean J, An Q, Chen M, Hall HI. Racial/ethnic disparities in HIV diagnoses among persons aged 50 years and older in 37 US states, 2005-2008. Am J Public Health. 2012;102(8):1527–1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260. Paz-Bailey G, Miller W, Shiraishi RW, Jacobson JO, Abimbola TO, Chen SY. Reaching men who have sex with men: a comparison of respondent-driven sampling and time-location sampling in Guatemala City. AIDS Behav. 2013;17(9):3081–3090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261. Sutton MY, Jones RL, Wolitski RJ, Cleveland JC, Dean HD, Fenton KA. A review of the Centers for Disease Control and Prevention’s response to the HIV/AIDS crisis among blacks in the United States, 1981-2009. Am J Public Health. 2009;99(suppl 2):S351–S359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262. Wolitski RJ, Fenton KA. Sexual health, HIV, and sexually transmitted infections among gay, bisexual, and other men who have sex with men in the United States. AIDS Behav. 2011;15(suppl 1):S9–S17. [DOI] [PubMed] [Google Scholar]
- 263. Duran D, Usman HR, Beltrami J, Alvarez ME, Valleroy L, Lyles CM. HIV counseling and testing among Hispanics at CDC-funded sites in the United States, 2007. Am J Public Health. 2010;100(suppl 1):S152–S158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264. Elmore K, Nelson R, Gant Z, et al. Data harmonization process for creating the National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention Atlas. Public Health Rep. 2014;129(suppl 1):63–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265. Mahle Gray K, Tang T, Shouse L, Li J, Mermin J, Hall HI. Using the HIV surveillance system to monitor the National HIV/AIDS Strategy. Am J Public Health. 2013;103(1):141–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266. Sutton MY, Parks CP. HIV/AIDS prevention, faith, and spirituality among black/African American and Latino communities in the United States: strengthening scientific faith-based efforts to shift the course of the epidemic and reduce HIV-related health disparities. J Relig Health. 2013;52(2):514–530. [DOI] [PubMed] [Google Scholar]
- 267. Sullivan PS, Stephenson R, Grazter B, et al. Adaptation of the African couples HIV testing and counseling model for men who have sex with men in the United States: an application of the ADAPT-ITT framework [published erratum appears in Springerplus. 2014;3:396]. Springerplus. 2014;3:249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268. Herbst JH, Glassman M, Carey JW, et al. Operational research to improve HIV prevention in the United States. J Acquir Immune Defic Syndr. 2012;59(5):530–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269. Stein R, Grimes TS, Malow R, Stratford D, Spielberg F, Holtgrave DR. Introduction to special supplement. Monitoring and evaluation of HIV counseling, testing and referral (CTR) and HIV testing services. AIDS Educ Prev. 2011;23(suppl 3):1–6. [DOI] [PubMed] [Google Scholar]
- 270. Mansergh G, Koblin BA, Sullivan PS. Challenges for HIV pre-exposure prophylaxis among men who have sex with men in the United States. PLoS Med. 2012;9(8):e1001286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271. Woodring JV, Kruszon-Moran D, Oster AM, McQuillan GM. Did CDC’s 2006 revised HIV testing recommendations make a difference? Evaluation of HIV testing in the US household population, 2003-2010. J Acquir Immune Defic Syndr. 2014;67(3):331–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272. Van Handel M, Mulatu MS. Effectiveness of the U.S. National HIV Testing Day campaigns in promoting HIV testing: evidence from CDC-funded HIV testing sites, 2010. Public Health Rep. 2014;129(5):446–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273. Panneer N, Lontok E, Branson BM, et al. HIV and hepatitis C virus infection in the United States: whom and how to test. Clin Infect Dis. 2014;59(6):875–882. [DOI] [PubMed] [Google Scholar]
- 274. Smith DK, Pals SL, Herbst JH, Shinde S, Carey JW. Development of a clinical screening index predictive of incident HIV infection among men who have sex with men in the United States. J Acquir Immune Defic Syndr. 2012;60(4):421–427. [DOI] [PubMed] [Google Scholar]
- 275. Otieno FO, Ndivo R, Oswago S, et al. Evaluation of syndromic management of sexually transmitted infections within the Kisumu Incidence Cohort Study. Int J STD AIDS. 2014;25(12):851–859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276. Charania MR, Marshall KJ, Lyles CM, et al. Identification of evidence-based interventions for promoting HIV medication adherence: findings from a systematic review of U.S.-based studies, 1996-2011. AIDS Behav. 2014;18(4):646–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277. Ivy W III, Dominguez KL, Rakhmanina NY, et al. Premastication as a route of pediatric HIV transmission: case-control and cross-sectional investigations. J Acquir Immune Defic Syndr. 2012;59(2):207–212. [DOI] [PubMed] [Google Scholar]
- 278. Basavaraju SV, Mwangi J, Nyamongo J, et al. Reduced risk of transfusion-transmitted HIV in Kenya through centrally co-ordinated blood centres, stringent donor selection and effective p24 antigen-HIV antibody screening. Vox Sang. 2010;99(3):212–219. [DOI] [PubMed] [Google Scholar]
- 279. Durham MD, Buchacz K, Richardson J, et al. Sexual risk behavior and viremia among men who have sex with men in the HIV Outpatient Study, United States, 2007-2010. J Acquir Immune Defic Syndr. 2013;63(3):372–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280. Vellozzi C, Buchacz K, Baker R, et al. Treatment of hepatitis C virus (HCV) infection in patients coinfected with HIV in the HIV Outpatient Study (HOPS), 1999-2007. J Viral Hepat. 2011;18(5):316–324. [DOI] [PubMed] [Google Scholar]
- 281. Buchacz K, Baker RK, Palella FJ, Jr, et al. AIDS-defining opportunistic illnesses in US patients, 1994-2007: a cohort study. AIDS. 2010;24(10):1549–1559. [DOI] [PubMed] [Google Scholar]
- 282. Patel P, Bush T, Mayer K, et al. Routine brief risk-reduction counseling with biannual STD testing reduces STD incidence among HIV-infected men who have sex with men in care. Sex Transm Dis. 2012;39(6):470–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283. Beer L, Valverde EE, Raiford JL, Weiser J, White BL, Skarbinski J. Clinician perspectives on delaying initiation of antiretroviral therapy for clinically eligible HIV-infected patients. J Int Assoc Provid AIDS Care. 2015;14(3):245–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284. Beer L, Heffelfinger J, Frazier E, et al. Use of and adherence to antiretroviral therapy in a large U.S. sample of HIV-infected adults in care, 2007-2008. Open AIDS J. 2012;6:213–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285. Kamb ML. Congenital syphilis: not gone and all too forgotten. World J Pediatr. 2010;6(2):101–102. [DOI] [PubMed] [Google Scholar]
- 286. Castro AR, Esfandiari J, Kumar S, et al. Novel point-of-care test for simultaneous detection of nontreponemal and treponemal antibodies in patients with syphilis. J Clin Microbiol. 2010;48(12):4615–4619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287. Gottlieb SL, Low N, Newman LM, Bolan G, Kamb M, Broutet N. Toward global prevention of sexually transmitted infections (STIs): the need for STI vaccines. Vaccine. 2014;32(14):1527–1535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288. Llata E, Stenger M, Bernstein K, et al. Prevalence of genital warts among sexually transmitted disease clinic patients—Sexually Transmitted Disease Network, United States, January 2010 to December 2011. Sex Transm Dis. 2014;41(2):89–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289. Torrone EA, Geisler WM, Gift TL, Weinstock HS. Chlamydia trachomatis infection among women 26 to 39 years of age in the United States, 1999 to 2010. Sex Transm Dis. 2013;40(4):335–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290. Hoover JB, Tao G, Heffelfinger JD. Monitoring HIV testing at visits to emergency departments in the United States: very-low rate of HIV testing. J Acquir Immune Defic Syndr. 2013;62(1):90–94. [DOI] [PubMed] [Google Scholar]
- 291. Peterman TA, Gottlieb SL, Berman SM. Commentary: chlamydia trachomatis screening: what are we trying to do? Int J Epidemiol. 2009;38(2):449–451. [DOI] [PubMed] [Google Scholar]
- 292. Tao G, Hoover KW, Leichliter JS, Peterman TA, Kent CK. Self-reported chlamydia testing rates of sexually active women aged 15-25 years in the United States, 2006-2008. Sex Transm Dis. 2012;39(8):605–607. [DOI] [PubMed] [Google Scholar]
- 293. Gottlieb SL, Berman SM, Low N. Screening and treatment to prevent sequelae in women with Chlamydia trachomatis genital infection: how much do we know? J Infect Dis. 2010;201(suppl 2):S156–S167. [DOI] [PubMed] [Google Scholar]
- 294. Habel MA, Leichliter JS. Emergency contraception and risk for sexually transmitted infections among U.S. women. J Womens Health (Larchmt). 2012;21(9):910–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295. Gottlieb SL, Brewer NT, Sternberg MR, et al. Human papillomavirus vaccine initiation in an area with elevated rates of cervical cancer. J Adolesc Health. 2009;45(5):430–437. [DOI] [PubMed] [Google Scholar]
- 296. Torrone EA, Satterwhite CL, Scholes D, Yu O, Berman S, Peterman TA. Estimating chlamydia re-infection rates: an empirical example. Sex Transm Infect. 2013;89(5):388–390. [DOI] [PubMed] [Google Scholar]
- 297. Habel MA, Hood J, Desai S, Kachur R, Buhi ER, Liddon N. Google it: obtaining information about local STD/HIV testing services online. Sex Transm Dis. 2011;38(4):334–338. [DOI] [PubMed] [Google Scholar]
- 298. Kirkcaldy RD, Kidd S, Weinstock HS, Papp JR, Bolan GA. Trends in antimicrobial resistance in Neisseria gonorrhoeae in the USA: the Gonococcal Isolate Surveillance Project (GISP), January 2006-June 2012. Sex Transm Infect. 2013;89(suppl 4):iv5–iv10. [DOI] [PubMed] [Google Scholar]
- 299. Hoover KW, Tao G, Nye MB, Body BA. Suboptimal adherence to repeat testing recommendations for men and women with positive chlamydia tests in the United States, 2008-2010. Clin Infect Dis. 2013;56(1):51–57. [DOI] [PubMed] [Google Scholar]
- 300. Dunne EF, Friedman A, Datta SD, Markowitz LE, Workowski KA. Updates on human papillomavirus and genital warts and counseling messages from the 2010 sexually transmitted diseases treatment guidelines. Clin Infect Dis. 2011;53(suppl 3):S143–S152. [DOI] [PubMed] [Google Scholar]
- 301. Grant LA, Dunne EF, Chesson H, Markowitz LE. Considerations for human papillomavirus (HPV) vaccination of mid-adult women in the United States. Vaccine. 2011;29(13):2365–2370. [DOI] [PubMed] [Google Scholar]
- 302. Liddon NC, Hood JE, Leichliter JS. Intent to receive HPV vaccine and reasons for not vaccinating among unvaccinated adolescent and young women: findings from the 2006-2008 National Survey of Family Growth. Vaccine. 2012;30(16):2676–2682. [DOI] [PubMed] [Google Scholar]
- 303. Workowski KA, Berman S. Sexually transmitted diseases treatment guidelines, 2010 [published erratum appears in MMWR Recomm Rep. 2011;60(1):18]. MMWR Recomm Rep. 2010;59(RR-12):1–110. [PubMed] [Google Scholar]
- 304. Gottlieb SL, Brewer NT, Smith JS, Keating KM, Markowitz LE. Availability of human papillomavirus vaccine at medical practices in an area with elevated rates of cervical cancer. J Adolesc Health. 2009;45(5):438–444. [DOI] [PubMed] [Google Scholar]
- 305. Bradley H, Asbel L, Bernstein K, et al. HIV testing among patients infected with Neisseria gonorrhoeae: STD Surveillance Network, United States, 2009-2010. AIDS Behav. 2013;17(3):1205–1210. [DOI] [PubMed] [Google Scholar]
- 306. Koumans EH, Lane SD, Aubry R, et al. Evaluation of Syracuse Healthy Start’s program for abnormal flora management to reduce preterm birth among pregnant women. Matern Child Health J. 2011;15(7):1020–1028. [DOI] [PubMed] [Google Scholar]
- 307. Hood JE, MacKellar D, Spaulding A, et al. Client characteristics and gender-specific correlates of testing HIV positive: a comparison of standalone center versus mobile outreach HIV testing and counseling in Botswana. AIDS Behav. 2012;16(7):1902–1916. [DOI] [PubMed] [Google Scholar]
- 308. Hogben M, Hood J, Collins D, McFarlane M. Assessing the role of prevention partnerships in STD prevention: a review of comprehensive STD prevention systems progress reports. Sex Transm Infect. 2013;89(7):590–594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309. Peterman TA, Newman DR, Collins DE, Doshi SR, Berman SM. Sexually transmitted diseases program performance measures: how are they performing? Sex Transm Dis. 2011;38(7):610–616. [DOI] [PubMed] [Google Scholar]
- 310. Xu F, Stoner BP, Taylor SN, et al. “Testing-only” visits: an assessment of missed diagnoses in clients attending sexually transmitted disease clinics. Sex Transm Dis. 2013;40(1):64–69. [DOI] [PubMed] [Google Scholar]
- 311. Tao G, Hoover KW, Kent CK. 2009 cervical cytology guidelines and chlamydia testing among sexually active young women. Obstet Gynecol. 2010;116(6):1319–1323. [DOI] [PubMed] [Google Scholar]
- 312. Owusu-Edusei K, Jr, Tejani MN, Gift TL, Kent CK, Tao G. Estimates of the direct cost per case and overall burden of trichomoniasis for the employer-sponsored privately insured women population in the United States, 2001 to 2005. Sex Transm Dis. 2009;36(6):395–399. [DOI] [PubMed] [Google Scholar]
- 313. Owusu-Edusei K, Jr, Chesson HW, Gift TL. The economic burden of pediculosis pubis and scabies infections treated on an outpatient basis in the United States: evidence from private insurance claims data, 2001-2005. Sex Transm Dis. 2009;36(5):297–299. [DOI] [PubMed] [Google Scholar]
- 314. Owusu-Edusei K, Jr, Peterman TA, Ballard RC. Serologic testing for syphilis in the United States: a cost-effectiveness analysis of two screening algorithms. Sex Transm Dis. 2011;38(1):1–7. [DOI] [PubMed] [Google Scholar]
- 315. Owusu-Edusei K, Jr, Roby TM, Chesson HW, Gift TL. Productivity costs of nonviral sexually transmissible infections among patients who miss work to seek medical care: evidence from claims data. Sex Health. 2013;10(5):434–437. [DOI] [PubMed] [Google Scholar]
- 316. Owusu-Edusei K, Jr, Hoover KW, Tao G. Estimating the direct outpatient medical cost per episode of primary and secondary syphilis in the United States: insured population perspective, 2003-2007. Sex Transm Dis. 2011;38(3):175–179. [DOI] [PubMed] [Google Scholar]
- 317. Owusu-Edusei K, Jr, Flagg EW, Gift TL. Hospitalization cost per case of neonatal herpes simplex virus infection from claims data. J Pediatr Nurs. 2015;30(2):346–352. [DOI] [PubMed] [Google Scholar]
- 318. Owusu-Edusei K, Jr, Introcaso CE, Chesson HW. Hospitalization cost of congenital syphilis diagnosis from insurance claims data in the United States. Sex Transm Dis. 2013;40(3):226–229. [DOI] [PubMed] [Google Scholar]
- 319. Bohm MK, Newman L, Satterwhite CL, Tao G, Weinstock HS. Pelvic inflammatory disease among privately insured women, United States, 2001-2005. Sex Transm Dis. 2010;37(3):131–136. [DOI] [PubMed] [Google Scholar]
- 320. Cain KP, Garman KN, Laserson KF, et al. Moving toward tuberculosis elimination: implementation of statewide targeted tuberculin testing in Tennessee. Am J Respir Crit Care Med. 2012;186(3):273–279. [DOI] [PubMed] [Google Scholar]
- 321. Iademarco MF, Koh WJ. 2011: the year in review. Part II: tuberculosis and lung disease. Int J Tuberc Lung Dis. 2012;16(10):1291–1299. [DOI] [PubMed] [Google Scholar]
- 322. Whitworth WC, Hamilton LR, Goodwin DJ, et al. Within-subject interlaboratory variability of QuantiFERON-TB gold in-tube tests. PLoS One. 2012;7(9):e43790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323. Lobue P, Menzies D. Treatment of latent tuberculosis infection: an update. Respirology. 2010;15(4):603–622. [DOI] [PubMed] [Google Scholar]
- 324. Shepardson D, Marks SM, Chesson H, et al. Cost-effectiveness of a 12-dose regimen for treating latent tuberculous infection in the United States. Int J Tuberc Lung Dis. 2013;17(12):1531–1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 325. Gammino VM, Taylor AB, Rich ML, et al. Bacteriologic monitoring of multidrug-resistant tuberculosis patients in five DOTS-Plus pilot projects. Int J Tuberc Lung Dis. 2011;15(10):1315–1322. [DOI] [PubMed] [Google Scholar]
- 326. Wallace RM, Kammerer JS, Iademarco MF, Althomsons SP, Winston CA, Navin TR. Increasing proportions of advanced pulmonary tuberculosis reported in the United States: are delays in diagnosis on the rise? Am J Respir Crit Care Med. 2009;180(10):1016–1022. [DOI] [PubMed] [Google Scholar]
- 327. Cain KP, McCarthy KD, Heilig CM, et al. An algorithm for tuberculosis screening and diagnosis in people with HIV. N Engl J Med. 2010;362(8):707–716. [DOI] [PubMed] [Google Scholar]
- 328. Bharaswadkar S, Kanchar A, Thakur N, et al. Tuberculosis management practices of private practitioners in Pune municipal corporation, India. PLoS One. 2014;9(6):e97993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329. Thompson ND, Perz JF. Eliminating the blood: ongoing outbreaks of hepatitis B virus infection and the need for innovative glucose monitoring technologies. J Diabetes Sci Technol. 2009;3(2):283–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330. Thompson ND, Hellinger WC, Kay RS, et al. Healthcare-associated hepatitis C virus transmission among patients in an abdominal organ transplant center. Transpl Infect Dis. 2009;11(4):324–329. [DOI] [PubMed] [Google Scholar]
- 331. Ward JW, Hu DJ, Alter MJ, et al. Transforming strategies for the prevention of chronic HBV and HCV infections. J Fam Pract. 2010;59(4 suppl):S23–S28. [PubMed] [Google Scholar]
- 332. Smith BD, Drobeniuc J, Jewett A, et al. Evaluation of three rapid screening assays for detection of antibodies to hepatitis C virus. J Infect Dis. 2011;204(6):825–831. [DOI] [PubMed] [Google Scholar]
- 333. Smith BD, Teshale E, Jewett A, et al. Performance of premarket rapid hepatitis C virus antibody assays in 4 national human immunodeficiency virus behavioral surveillance system sites. Clin Infect Dis. 2011;53(8):780–786. [DOI] [PubMed] [Google Scholar]
- 334. Ward JW, Averhoff FM, Koh HK. World hepatitis day: a new era for hepatitis control. Lancet. 2011;378(9791):552–553. [DOI] [PubMed] [Google Scholar]
- 335. Spradling PR, Richardson JT, Buchacz K, et al. Trends in hepatitis C virus infection among patients in the HIV Outpatient Study, 1996-2007. J Acquir Immune Defic Syndr. 2010;53(3):388–396. [DOI] [PubMed] [Google Scholar]
- 336. Spradling PR, Richardson JT, Buchacz K, Moorman AC, Brooks JT. Prevalence of chronic hepatitis B virus infection among patients in the HIV Outpatient Study, 1996-2007. J Viral Hepat. 2010;17(12):879–886. [DOI] [PubMed] [Google Scholar]
- 337. Holmberg SD, Lu M, Rupp LB, et al. Noninvasive serum fibrosis markers for screening and staging chronic hepatitis C virus patients in a large US cohort. Clin Infect Dis. 2013;57(2):240–246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338. Byrd KK, Santibanez TA, Chaves SS. Predictors of hepatitis A vaccination among young children in the United States. Vaccine. 2011;29(17):3254–3259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339. Roberts HW, Utuama OA, Klevens M, Teshale E, Hughes E, Jiles R. The contribution of viral hepatitis to the burden of chronic liver disease in the United States. Am J Gastroenterol. 2014;109(3):387–393. [DOI] [PubMed] [Google Scholar]
- 340. Mahajan R, Moorman AC, Liu SJ, Rupp L, Klevens RM. Use of the International Classification of Diseases, 9th Revision, coding in identifying chronic hepatitis B virus infection in health system data: implications for national surveillance. J Am Med Inform Assoc. 2013;20(3):441–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341. Fischer GE, Bialek SP, Homan CE, Livingston SE, McMahon BJ. Chronic liver disease among Alaska-Native people, 2003-2004. Am J Gastroenterol. 2009;104(2):363–370. [DOI] [PubMed] [Google Scholar]
- 342. Mahajan R, Liu SJ, Klevens RM, Holmberg SD. Indications for testing among reported cases of HCV infection from enhanced hepatitis surveillance sites in the United States, 2004-2010. Am J Public Health. 2013;103(8):1445–1449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343. Beckett GA, Block JM, Cohen C, McMahon BJ. The role of primary care physician assistants in managing chronic hepatitis B. Jaapa. 2014;27(3):51–54. [DOI] [PubMed] [Google Scholar]
- 344. Steiner RJ, Aquino G, Fenton KA. Enhancing HIV/AIDS, viral hepatitis, sexually transmitted disease, and tuberculosis prevention in the United States through program collaboration and service integration: the case for broader implementation. Sex Transm Dis. 2013;40(8):663–668. [DOI] [PubMed] [Google Scholar]
- 345. Ivankovich MB, Fenton KA, Douglas JM., Jr Considerations for national public health leadership in advancing sexual health. Public Health Rep. 2013;128(suppl 1):102–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346. Begley E, VanHandel M. Provision of test results and posttest counseling at STD clinics in 24 health departments: U.S., 2007. Public Health Rep. 2012;127(4):432–439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347. Beltran VM, Harrison KM, Hall HI, Dean HD. Collection of social determinant of health measures in U.S. national surveillance systems for HIV, viral hepatitis, STDs, and TB. Public Health Rep. 2011;126(suppl 3):41–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348. Sweeney P, Gardner LI, Buchacz K, et al. Shifting the paradigm: using HIV surveillance data as a foundation for improving HIV care and preventing HIV infection. Milbank Q. 2013;91(3):558–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349. Hall HI, Frazier EL, Rhodes P, et al. Differences in human immunodeficiency virus care and treatment among subpopulations in the United States. JAMA Intern Med. 2013;173(14):1337–1344. [DOI] [PubMed] [Google Scholar]
- 350. Lanier Y, Sutton MY. Reframing the context of preventive health care services and prevention of HIV and other sexually transmitted infections for young men: new opportunities to reduce racial/ethnic sexual health disparities. Am J Public Health. 2013;103(2):262–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351. Voetsch AC, Heffelfinger JD, Yonek J, et al. HIV screening practices in U.S. hospitals, 2009-2010. Public Health Rep. 2012;127(5):524–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 352. Reed JB, Hanson D, McNaghten AD, et al. HIV testing factors associated with delayed entry into HIV medical care among HIV-infected persons from eighteen states, United States, 2000-2004. AIDS Patient Care STDS. 2009;23(9):765–773. [DOI] [PubMed] [Google Scholar]
- 353. Cohen SM, Hu X, Sweeney P, Johnson AS, Hall HI. HIV viral suppression among persons with varying levels of engagement in HIV medical care, 19 US jurisdictions. J Acquir Immune Defic Syndr. 2014;67(5):519–527. [DOI] [PubMed] [Google Scholar]
- 354. Farnham PG. Do reduced inpatient costs associated with highly active antiretroviral therapy (HAART) balance the overall cost for HIV treatment? Appl Health Econ Health Policy. 2010;8(2):75–88. [DOI] [PubMed] [Google Scholar]
- 355. Gust DA, Shinde S, Pals SL, Hardnett F, Chen RT, Sanchez T. Correlates of health attitudes among homosexual and bisexual men [published erratum appears in J Epidemiol Glob Health. 2013;3(4):293]. J Epidemiol Glob Health. 2013;3(1):31–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356. Taylor MM, Reilley B, Yellowman M, Anderson L, de Ravello L, Tulloch S. Use of expedited partner therapy among chlamydia cases diagnosed at an urban Indian health centre, Arizona. Int J STD AIDS. 2013;24(5):371–374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 357. Hoover KW, Tao G, Berman S, Kent CK. Utilization of health services in physician offices and outpatient clinics by adolescents and young women in the United States: implications for improving access to reproductive health services. J Adolesc Health. 2010;46(4):324–330. [DOI] [PubMed] [Google Scholar]
- 358. Tao G, Hoover KW. Differences in access to healthcare and utilisation of HIV and sexually transmissible infection services between men who have sex with men and men who have sex only with women: results of the 2006-10 National Survey of Family Growth in the United States. Sex Health. 2013;10(4):363–368. [DOI] [PubMed] [Google Scholar]
- 359. Owusu-Edusei K, Jr, Doshi SR. Assessing spatial gaps in sexually transmissible infection services and morbidity: an illustration with Texas county-level data from 2007. Sex Health. 2012;9(4):334–340. [DOI] [PubMed] [Google Scholar]
- 360. Owusu-Edusei K, Jr, Doshi SR. County-level sexually transmitted disease detection and control in Texas: do sexually transmitted diseases and family planning clinics matter? Sex Transm Dis. 2011;38(10):970–975. [DOI] [PubMed] [Google Scholar]
- 361. Haderxhanaj LT, Dittus PJ, Loosier PS, Rhodes SD, Bloom FR, Leichliter JS. Acculturation, sexual behaviors, and health care access among Hispanic and non-Hispanic white adolescents and young adults in the United States, 2006-2010. J Adolesc Health. 2014;55(5):716–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362. Collier MG, Tong X, Xu F. Hepatitis A hospitalizations in the United States, 2002-2011. Hepatology. 2015;61(2):481–485. [DOI] [PubMed] [Google Scholar]
- 363. Mizuno Y, Purcell DW, Latka MH, et al. Is sexual serosorting occurring among HIV-positive injection drug users? Comparison between those with HIV-positive partners only, HIV-negative partners only, and those with any partners of unknown status. AIDS Behav. 2010;14(1):92–102. [DOI] [PubMed] [Google Scholar]
- 364. Page MJ, Harrison KM, Wei X, Hall HI. Federal funding for reporting cases of HIV infection in the United States, 2006. Public Health Rep. 2010;125(5):718–727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 365. Mizuno Y, Purcell DW, Metsch LR, Gomez CA, Knowlton AR, Latka MH. Is injection serosorting occurring among HIV-positive injection drug users? Comparison by injection partner’s HIV status. J Urban Health. 2011;88(6):1031–1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 366. Masciotra S, Luo W, Youngpairoj AS, et al. Performance of the Alere Determine HIV-1/2 Ag/Ab Combo Rapid Test with specimens from HIV-1 seroconverters from the US and HIV-2 infected individuals from Ivory Coast. J Clin Virol. 2013;58(suppl 1):e54–e58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367. Conley L, Bush T, Darragh TM, et al. Factors associated with prevalent abnormal anal cytology in a large cohort of HIV-infected adults in the United States. J Infect Dis. 2010;202(10):1567–1576. [DOI] [PubMed] [Google Scholar]
- 368. Ackers ML, Greenberg AE, Lin CY, et al. High and persistent HIV seroincidence in men who have sex with men across 47 U.S. cities. PLoS One. 2012;7(4):e34972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369. Sorensen SW, Sansom SL, Brooks JT, et al. A mathematical model of comprehensive test-and-treat services and HIV incidence among men who have sex with men in the United States. PLoS One. 2012;7(2):e29098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 370. Hardnett FP, Pals SL, Borkowf CB, Parsons J, Gomez C, O’Leary A. Assessing mediation in HIV intervention studies. Public Health Rep. 2009;124(2):288–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 371. O’Leary A, Horvath KJ, Simon Rosser BR. Associations between partner-venue specific personal responsibility beliefs and transmission risk behavior by HIV-positive men who have sex with men (MSM). AIDS Behav. 2013;17(5):1855–1861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 372. Dunne EF, Nielson CM, Hagensee ME, et al. HPV 6/11, 16, 18 seroprevalence in men in two US cities. Sex Transm Dis. 2009;36(11):671–674. [DOI] [PubMed] [Google Scholar]
- 373. Shah S, Demissie M, Lambert L, et al. Intensified tuberculosis case finding among HIV-infected persons from a voluntary counseling and testing center in Addis Ababa, Ethiopia. J Acquir Immune Defic Syndr. 2009;50(5):537–545. [DOI] [PubMed] [Google Scholar]
- 374. Berzkalns A, Bates J, Ye W, et al. The road to tuberculosis (Mycobacterium tuberculosis) elimination in Arkansas; a re-examination of risk groups. PLoS One. 2014;9(3):e90664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 375. Warner AE, Schaefer MK, Patel PR, et al. Outbreak of hepatitis C virus infection associated with narcotics diversion by an hepatitis C virus-infected surgical technician. Am J Infect Control. 2015;43(1):53–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 376. Teo CG. Much meat, much malady: changing perceptions of the epidemiology of hepatitis E. Clin Microbiol Infect. 2010;16(1):24–32. [DOI] [PubMed] [Google Scholar]
- 377. Collier MG, Khudyakov YE, Selvage D, et al. Outbreak of hepatitis A in the USA associated with frozen pomegranate arils imported from Turkey: an epidemiological case study. Lancet Infect Dis. 2014;14(10):976–981. [DOI] [PubMed] [Google Scholar]
- 378. Klevens RM, Miller JT, Iqbal K, et al. The evolving epidemiology of hepatitis A in the United States: incidence and molecular epidemiology from population-based surveillance, 2005-2007. Arch Intern Med. 2010;170(20):1811–1818. [DOI] [PubMed] [Google Scholar]
- 379. Holtzman D, Barry V, Ouellet LJ, et al. The influence of needle exchange programs on injection risk behaviors and infection with hepatitis C virus among young injection drug users in select cities in the United States, 1994-2004. Prev Med. 2009;49(1):68–73. [DOI] [PubMed] [Google Scholar]
- 380. Forbi JC, Purdy MA, Campo DS, et al. Epidemic history of hepatitis C virus infection in two remote communities in Nigeria, West Africa. J Gen Virol. 2012;93(pt 7):1410–1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 381. Raiford JL, Seth P, Braxton ND, DiClemente RJ. Masculinity, condom use self-efficacy and abusive responses to condom negotiation: the case for HIV prevention for heterosexual African-American men. Sex Health. 2013;10(5):467–469. [DOI] [PubMed] [Google Scholar]
- 382. Seth P, Wingood GM, Robinson LS, Raiford JL, DiClemente RJ. Abuse impedes prevention: the intersection of intimate partner violence and HIV/STI risk among young African American women. AIDS Behav. 2015;19(8):1438–1445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 383. Nasrullah M, Oraka E, Breiding MJ, Chavez PR. HIV testing and intimate partner violence among non-pregnant women in 15 US states/territories: findings from Behavioral Risk Factor Surveillance System survey data. AIDS Behav. 2013;17(7):2521–2527. [DOI] [PubMed] [Google Scholar]
- 384. Oster AM, Sternberg M, Nebenzahl S, et al. Prevalence of HIV, sexually transmitted infections, and viral hepatitis by urbanicity, among men who have sex with men, injection drug users, and heterosexuals in the United States. Sex Transm Dis. 2014;41(4):272–279. [DOI] [PubMed] [Google Scholar]
- 385. Hall HI, Espinoza L, Benbow N, Hu YW. Epidemiology of HIV infection in large urban areas in the United States. PLoS One. 2010;5(9):e12756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 386. Friedman SR, West BS, Tempalski B, et al. Do metropolitan HIV epidemic histories and programs for people who inject drugs and men who have sex with men predict AIDS incidence and mortality among heterosexuals? Ann Epidemiol. 2014;24(4):304–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 387. Torrone EA, Bertolli J, Li J, et al. Increased HIV and primary and secondary syphilis diagnoses among young men—United States, 2004-2008. J Acquir Immune Defic Syndr. 2011;58(3):328–335. [DOI] [PubMed] [Google Scholar]
- 388. Chesson HW, Sternberg M, Leichliter JS, Aral SO. Changes in the state-level distribution of primary and secondary syphilis in the USA, 1985-2007. Sex Transm Infect. 2010;86(suppl 3):iii58–iii62. [DOI] [PubMed] [Google Scholar]
- 389. Rourke SB, Sobota M, Tucker R, et al. Social determinants of health associated with hepatitis C co-infection among people living with HIV: results from the Positive Spaces, Healthy Places study. Open Med. 2011;5(3):e120–e131. [PMC free article] [PubMed] [Google Scholar]
- 390. Rasanathan K, Sivasankara Kurup A, Jaramillo E, Lonnroth K. The social determinants of health: key to global tuberculosis control. Int J Tuberc Lung Dis. 2011;15(suppl 2):S30–S36. [DOI] [PubMed] [Google Scholar]
- 391. Hogben M, Leichliter JS. Social determinants and sexually transmitted disease disparities. Sex Transm Dis. 2008;35(suppl 12):S13–S18. [DOI] [PubMed] [Google Scholar]
- 392. Adimora AA, Schoenbach VJ. Social context, sexual networks, and racial disparities in rates of sexually transmitted infections. J Infect Dis. 2005;191(suppl 1):S115–S122. [DOI] [PubMed] [Google Scholar]
- 393. Holtgrave DR, Crosby RA. Social determinants of tuberculosis case rates in the United States. Am J Prev Med. 2004;26(2):159–162. [DOI] [PubMed] [Google Scholar]
- 394. US House of Representatives, 111th Congress, 2d Session. Compilation of Patient Protection and Affordable Care Act as amended through November 1, 2010, including Patient Protection and Affordable Care Act health-related portions of the Health Care and Education Reconciliation Act of 2010. 2010. http://purl.fdlp.gov/GPO/gpo16534. Accessed May 6, 2018.
- 395. Suhrcke M, Stuckler D, Suk JE, et al. The impact of economic crises on communicable disease transmission and control: a systematic review of the evidence. PLoS One. 2011;6(6):e20724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 396. Nieblas R, Hughes L, Andrews R, Relf M. Reframing and understanding the HIV epidemic in MSM: masculinity, racism, and homophobia. J Assoc Nurses AIDS Care. 2015;26(5):514–519. [DOI] [PubMed] [Google Scholar]
- 397. Han CS, Ayala G, Paul JP, Boylan R, Gregorich SE, Choi KH. Stress and coping with racism and their role in sexual risk for HIV among African American, Asian/Pacific Islander, and Latino men who have sex with men. Arch Sex Behav. 2015;44(2):411–420. [DOI] [PMC free article] [PubMed] [Google Scholar]