Abstract
The populations of many Appalachian communities have high rates of unhealthy body weight. This study aimed to identify differences in beliefs about obesity between Appalachians and non-Appalachians. Our analyses explored health beliefs and behaviors among US adults aged ≥18 (n = 14 451) who responded to the Health Information National Trends Survey (2011-2014), of whom 1015 (8%) resided within the 420 counties recognized as Appalachian by the Appalachian Regional Commission. Using weighted regression analyses and controlling for sociodemographic characteristics and general health, we determined that self-reported body mass index was higher among Appalachians than among non-Appalachians (B = 0.75, P = .03, 95% confidence interval, 0.08-1.47) and that Appalachians were less likely than non-Appalachians to believe that lifestyle factors were related to obesity (B = –0.37, P = .03, 95% confidence interval, –0.04 to –0.71). Results suggest that Appalachians may regard behavioral prevention differently from non-Appalachians, perhaps with less confidence in the effectiveness of certain behaviors to reduce obesity risk. Future research may determine whether such beliefs could complicate efforts to encourage healthy lifestyles throughout the region.
Keywords: Appalachia, rural health, obesity, preventive medicine, physical activity, healthy eating, smoking, health disparities
Complex geographic and socioeconomic factors underlie the elevated rates of obesity among the 25 million residents of the 13-state Appalachian region. These factors, which include limited availability of nutritious food and recreational facilities, limited access to health care, and low incomes,1–4 may be complicated by health beliefs that potentially undermine the perceived importance of preventive behaviors. For example, some Appalachian residents may endorse beliefs that “everything causes cancer” or have limited understanding of cancer risks.5,6 Other research suggests that Appalachians may overestimate their own vitality and health status and underestimate the adverse health impact of certain behaviors (eg, smoking or drinking soda).7,8 Despite abundant evidence for the high prevalence of obesity in the Appalachian region, the underlying psychosocial factors are poorly understood. To our knowledge, our study is the first to explore Appalachians’ perceptions of the behavioral determinants of obesity.
Methods
We used data from 4 cross-sectional cycles (2011-2014; combined n = 14 451) of the nationally representative Health Information National Trends Survey (HINTS 4). Each cycle consisted of a single-mode mail survey based on a random sample of residential addresses; response rates ranged from 34% to 40%. Addresses located in Central Appalachia were oversampled in 2011 and 2012. A total of 1015 (8%) respondents in the final sample were residents of Appalachia. HINTS 4 was approved by the Westat Institutional Review Board and deemed exempt from institutional review board review by the National Institutes of Health Office of Human Subjects Research Protections. Further details about HINTS development and methodology are available elsewhere.9,10
Measures
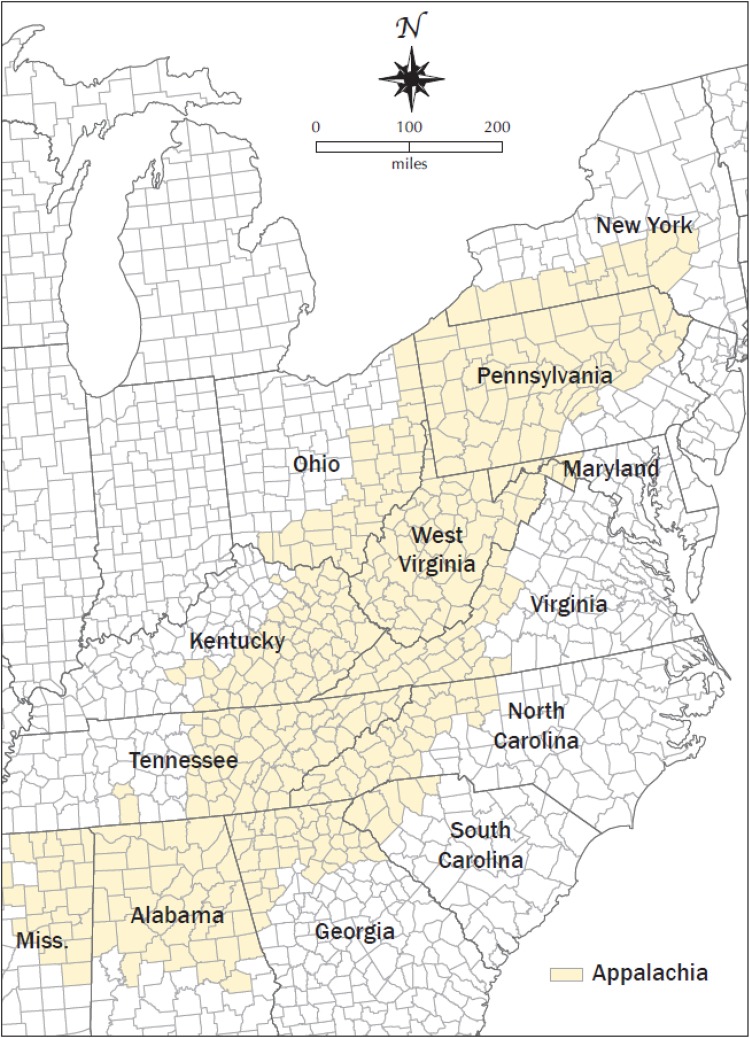
Respondents to 2 cycles of HINTS 4 (2012 and 2014; n = 7307) were asked how much they thought “health behaviors like diet, exercise, and smoking determine whether a person will develop obesity.” Responses were given on a scale from 1 (not at all) to 4 (a lot). Respondents also completed an analogous item assessing the influence of genetics on risk of obesity. Respondents in all cycles reported on their general health (“In general, would you say your health is . . .”) and their self-efficacy for taking care of their health (“Overall, how confident are you about your ability to take good care of your health?”). Other items assessed fruit and vegetable consumption in a typical day (in cups), frequency of soda consumption in a typical week, duration of physical activity in a typical day and frequency of those bouts of physical activity in a typical week, frequency of strength training in a typical week, duration of leisure-time sedentary behavior during the past 30 days (in hours per day), and smoking status (current and lifetime). Sociodemographic questions assessed age (18-29, 30-49, 50-69, and ≥70), sex (male and female), race/ethnicity (non-Hispanic black, non-Hispanic white, Hispanic, and non-Hispanic other), education (<high school, high school or equivalent, some college or technical training, and ≥bachelor’s degree), and annual household income (<$20 000, $20 000-$34 999, $35 000-$49 999, $50 000-$74 999, $75 000-$99 999, and ≥$100 000) (imputed income data are included in the publicly available data set; full HINTS methodology reports are available elsewhere9). Body mass index (BMI) was calculated from self-reported height and weight as weight in kilograms divided by height in meters squared (kg/m2), with <18.5 kg/m2 considered underweight, 18.5-24.9 kg/m2 considered normal, 25.0-29.9 kg/m2 considered overweight, and ≥30.0 kg/m2 considered obese. Residential areas were classified as urban or rural based on 2003 rural-urban continuum codes,11 and residence in Appalachia was determined by using the Appalachian Regional Commission’s designation of counties (Figure).12
Figure.
Counties within the Appalachian region designated in 2011 by the Appalachian Regional Commission.12
Statistical Analyses
We analyzed data using SAS version 9.3.13 In all analyses, we incorporated jackknife replicate weights to estimate accurate variance estimates for statistical modeling. This method allows adjustment for demographic oversampling and survey nonresponse to provide representative estimates of the adult US population. We used weighted Wald χ2 tests to determine sample differences between Appalachians and non-Appalachians. Then we used weighted least-squares regression analyses for continuous outcomes (eg, BMI) and weighted logistic regression analyses for ordinal outcomes (eg, beliefs about obesity) to test differences in BMI, beliefs about obesity, and obesity-related behaviors, controlling for age, sex, race/ethnicity, education, imputed income, rurality, and general health. We considered P < .05 to be significant.
Results
Most respondents were aged 50-69 (n = 6153, 30.6% of the weighted sample), female (n = 8566, 51.6% of the weighted sample), and non-Hispanic white (n = 8108, 66.8% of the weighted sample) (Table 1). Weighted Wald χ2 tests revealed that Appalachian and non-Appalachian samples were not significantly different in terms of age (P = .28) or sex (P = .43), but the 2 groups did differ by race/ethnicity (P < .001; higher proportion of non-Hispanic white respondents in the Appalachian sample), highest level of education completed (P = .003; lower proportion of respondents with ≥bachelor’s degree in the Appalachian sample), annual household income (P < .001; higher proportions of respondents reporting low income levels in the Appalachian sample), and rurality (P < .001; higher proportion of respondents living in rural areas in the Appalachian sample).
Table 1.
Sample distributions from the HINTS 4, cycles 1-4,a by residence in Appalachiab or non-Appalachia, 2011-2014 (n = 14 451)
| Characteristic | Full Sample | Appalachia | Non-Appalachia | P Valued | |||
|---|---|---|---|---|---|---|---|
| No. (%) | 95% CI | No. (%)c | 95% CI | No. (%) | 95% CI | ||
| Age, ye | .27 | ||||||
| 18-29 | 1125 (20.2) | 19.5-20.9 | 74 (20.9) | 14.6-27.2 | 1051 (20.2) | 19.3-21.1 | |
| 30-49 | 4111 (37.2) | 36.5-37.9 | 248 (33.3) | 28.3-38.2 | 3863 (37.6) | 36.7-38.4 | |
| 50-69 | 6153 (30.6) | 30.4-30.8 | 462 (33.3) | 29.1-37.4 | 5691 (30.4) | 30.0-30.8 | |
| ≥70 | 2590 (12.0) | 11.8-12.1 | 196 (12.5) | 10.4-14.6 | 2393 (11.9) | 11.7-12.1 | |
| Sex | .43 | ||||||
| Male | 5563 (48.4) | 48.2-48.6 | 381 (46.5) | 41.6-51.4 | 5182 (48.6) | 48.1-49.1 | |
| Female | 8566 (51.6) | 51.4-51.8 | 610 (53.5) | 48.6-58.4 | 7956 (51.4) | 50.9-51.9 | |
| Race/ethnicity | <.001 | ||||||
| Non-Hispanic black | 2027 (11.0) | 10.8-11.3 | 110 (6.4) | 4.6-8.1 | 1917 (11.44) | 11.1-11.7 | |
| Hispanic | 2023 (15.0) | 14.8-15.2 | 29 (3.6) | 1.1-6.1 | 1994 (16.0) | 15.7-16.3 | |
| Non-Hispanic white | 8018 (66.8) | 66.5-67.2 | 693 (86.6) | 83.1-90.1 | 7325 (65.1) | 64.7-65.6 | |
| Non-Hispanic other | 927 (7.2) | 7.0-7.3 | 45 (3.5) | 1.6-5.4 | 882 (7.5) | 7.2-7.7 | |
| Education | .003 | ||||||
| <High school graduate | 1325 (11.9) | 11.4-12.4 | 119 (13.2) | 10.0-16.4 | 1206 (11.8) | 11.3-12.3 | |
| High school graduate or equivalent | 2929 (21.5) | 20.6-22.4 | 248 (26.2) | 21.6-30.8 | 2681 (21.1) | 20.2-22.0 | |
| Some college or technical training | 4247 (32.9) | 31.9-33.8 | 285 (34.1) | 29.4-38.9 | 3962 (32.8) | 31.8-33.7 | |
| ≥Bachelor’s degree | 5536 (33.7) | 33.2-34.3 | 329 (26.5) | 22.7-30.2 | 5207 (34.4) | 33.7-35.0 | |
| Annual household income, $ | <.001 | ||||||
| <20 000 | 3340 (21.7) | 20.6-22.8 | 263 (25.0) | 20.2-29.8 | 3077 (21.5) | 20.3-22.6 | |
| 20 000-34 999 | 2172 (14.9) | 13.9-15.9 | 164 (15.7) | 11.8-19.6 | 2008 (14.8) | 13.8-15.8 | |
| 35 000-49 999 | 2051 (14.4) | 13.4-15.3 | 153 (16.2) | 12.2-20.2 | 1898 (14.2) | 13.3-15.2 | |
| 50 000-74 999 | 2329 (17.0) | 16.0-18.1 | 173 (20.0) | 15.4-24.5 | 2156 (16.8) | 15.7-17.9 | |
| 75 000-99 999 | 1646 (12.70) | 11.9-13.6 | 101 (10.4) | 7.7-13.1 | 1545 (13.0) | 12.1-13.9 | |
| ≥100 000 | 18.2-20.2 | 133 (12.9) | 10.0-15.7 | 2362 (19.7) | 18.7-20.8 | ||
| Rural or urban designation | <.001 | ||||||
| Rural | 2177 (16.6) | 15.7-17.5 | 394 (40.6) | 35.6-45.7 | 1783 (14.5) | 13.6-15.4 | |
| Urban | 12 274 (83.4) | 82.5-84.3 | 621 (59.4) | 54.3-64.4 | 11 653 (85.5) | 84.6-86.4 | |
b Residence in an Appalachian county was coded according to the Appalachian Regional Commission’s designation.12
c The number is the unweighted sample size and the percentage is the weighted population estimate.
dP values pertain to the results of unadjusted Wald χ2 tests comparing responses from Appalachians and non-Appalachians. P < .05 was considered significant.
e Age is categorized for ease of presentation, but it was included in regression analyses (Table 2) as a continuous variable.
Weighted least-squares regression analysis controlling for sociodemographic characteristics and general health revealed that average BMI was significantly higher among Appalachians (28.6 kg/m2) than among non-Appalachians (27.7 kg/m2) (P = .03) (Table 2). Further, similar ordinal regression analyses revealed that Appalachians were significantly less likely than non-Appalachians to report that health behaviors determine whether a person will develop obesity (P = .03). Appalachians did not differ from non-Appalachians in analogous beliefs about the extent to which genetics influence obesity risk (P = .40), nor did the 2 groups differ significantly in confidence in their ability to take care of their health (P = .74).
Table 2.
Adjusted differencesa between Appalachian and non-Appalachian respondents (n = 14 451) on body mass index, beliefs about obesity, and health behaviors, HINTS 4, cycles 1-4, 2011-2014b
| Continuous Variable | No.c | Weighted Meansd | Be (95% CI) | P Value | |
|---|---|---|---|---|---|
| Appalachian | Non-Appalachian | ||||
| Body mass index, kg/m2 | 11 929 | 28.6 | 27.7 | 0.75 (0.08 to 1.42) | .03 |
| Daily cups of fruit and vegetables | 12 095 | 5.0 | 5.1 | 0.01 (–0.26 to 0.29) | .92 |
| Weekly minutes of physical activity | 6497 | 179.7 | 205.6 | 5.12 (–56.54 to 66.77) | .87 |
| Weekly frequency of strength training, d/wk | 9031 | 0.9 | 1.2 | –0.21 (–0.40 to 0.02) | .03 |
| Daily hours of sedentary behavior | 11 639 | 3.8 | 3.8 | –0.02 (–0.33 to 0.30) | .90 |
| Weighted Percentages | |||||
| Categorical Variable | No. | Appalachian | Non-Appalachian | OR (95% CI) | P Value |
| Think that behaviors influence obesity | 6018 | 0.69 (0.49-0.97) | .03 | ||
| Not at all | 4.9 | 2.6 | |||
| A little | 5.9 | 4.4 | |||
| Somewhat | 20.1 | 14.4 | |||
| A lot | 69.1 | 78.7 | |||
| Think that genes influence obesity a lot | 6013 | 0.90 (0.71-1.15) | .40 | ||
| Not at all | 7.5 | 7.3 | |||
| A little | 24.4 | 23.0 | |||
| Somewhat | 42.2 | 41.4 | |||
| A lot | 26.0 | 28.3 | |||
| Confidence in ability to take care of health | 12 210 | 1.04 (0.82-1.32) | .74 | ||
| Not at all confident | 1.0 | 1.4 | |||
| A little confident | 4.6 | 4.7 | |||
| Somewhat confident | 27.9 | 26.0 | |||
| Very confident | 44.1 | 45.1 | |||
| Completely confident | 22.4 | 22.9 | |||
| Frequency of (non-diet) soda consumption | 5575 | 1.29 (0.85-1.95) | .28 | ||
| I do not drink any regular soda or pop | 35.2 | 39.0 | |||
| <1 day a week | 18.4 | 22.6 | |||
| 1-2 days a week | 13.1 | 14.7 | |||
| 3-4 days a week | 6.9 | 8.6 | |||
| 5-6 days a week | 8.4 | 4.2 | |||
| Every day | 18.0 | 10.8 | |||
| Have smoked ≥100 cigarettes | 12 155 | 45.7 | 40.3 | 1.09 (0.85-1.38) | .50 |
Abbreviations: HINTS, Health Information National Trends Survey; OR, odds ratio.
a Results of separate weighted regression analyses for each variable using listwise deletion. Continuous variables were submitted to linear regression analyses; categorical variables were submitted to ordinal regression analyses.
c Differences in sample size across models are primarily due to the fact that not all variables were included in each of the 4 cycles of HINTS 4. See the Methods section for more information on measure repetition.
d Weighted means are not adjusted for sociodemographic variables or general health.
e Unstandardized regression coefficients, odds ratios, and 95% confidence intervals refer to differences in mean values between Appalachians and non-Appalachians, controlling for sociodemographic variables (age, sex, race/ethnicity, education, household income, and rural-urban designation) and general health. P < .05 was considered significant.
Weighted least-squares regression analyses revealed that Appalachians reported engaging in weekly strength training significantly less often than non-Appalachians (P = .03; Table 2). However, no significant differences were found in daily cups of fruit and vegetables (P = .92), frequency of non-diet soda consumption (P = .28), weekly minutes of physical activity (P = .87), daily hours of sedentary behavior during leisure time in a typical day (P = .90), or smoking status (P = .50).
A subsequent regression analysis revealed no significant association between beliefs about behavioral determinants of obesity and BMI (P = .93), controlling for Appalachian residence, sociodemographic characteristics, and general health. We also found no significant association between beliefs about obesity and BMI moderated by Appalachian residence (P = .37). However, similar models revealed that stronger beliefs that behaviors are related to obesity were associated with greater fruit and vegetable consumption (P < .001) and current nonsmoker status (P < .001).
Discussion
This study provides further context for previously documented disparities in BMI, revealing that Appalachians were less likely than non-Appalachians to believe that health behaviors determine obesity risk, which aligns with lower self-efficacy documented in other health domains.5,6 Consistent with previous research,1–4 residents of Appalachia had a slightly higher average BMI than non-Appalachians. Although BMI was not directly related to beliefs about behavioral determinants of obesity in our study, undetected mediators and moderators may exist; indeed, subsequent analyses revealed associations between fruit and vegetable consumption and nonsmoking status. Longitudinal data may prove useful for exploring the indirect effects of beliefs about obesity on BMI through such health behaviors; the current cross-sectional data source is not well suited to evaluating such mechanisms or to determining causality. Aside from strength training (which is consistent with the scarcity of recreation and fitness facilities in the region14), Appalachians did not differ from non-Appalachians in terms of weight-related behaviors in our study, which is somewhat inconsistent with previous research.1,3,15–17
Notable limitations of our study primarily derived from the features of the data set. Specifically, the self-reported data may be subject to various social and cognitive biases, such as social desirability bias, which could motivate respondents to endorse beliefs or behaviors that they expect to be more socially acceptable (eg, more physical activity or greater consumption of fruit and vegetables). Another limitation of the study design was that the cross-sectional nature of the data did not enable inferences about the temporal order of variables of interest, let alone causality. Finally, one limitation that was specific to the key item assessing beliefs about the behavioral determinants of obesity was the imprecise design of the question stem, which provided “diet, exercise, and smoking” as exemplar behaviors. Although likely meant to aid respondents in understanding the question, this strategy may have introduced excess variability depending on how respondents interpreted the question. Some respondents may have reported on all 3 behaviors collectively, whereas others may have focused their responses on a subset of the behaviors, or other behaviors not mentioned in the stem.
The primary value of our findings may be in hypothesis generation, and future research may overcome the limitations of our study by using more fine-grained measures and/or qualitative methods to explore how life in Appalachia shapes the origins and implications of beliefs about obesity. For example, do some people embrace skepticism about the effectiveness of behavioral prevention to justify unhealthy lifestyles that feel inevitable and thereby reduce cognitive dissonance?18 Or do people who repeatedly fail to lose weight and observe the same failure among their peers in the absence of accessible supporting resources (eg, health care providers, readily available fruit and vegetables, venues for physical activity) learn to doubt the value of preventive health behaviors? Future research may also determine the prevalence of these beliefs across various subregions within Appalachia (ie, southern, central, or northern). Although concerns about sample size and statistical power precluded tests of differences across subregions in our study, it is worth exploring whether environmental or sociocultural differences in southern, central, or northern Appalachia contribute to varying belief patterns or behaviors. Additionally, in light of regional variation in discrepancies between objective and self-reported measures of BMI,19 it will be important to assess social norms and desirability pertaining to BMI among Appalachians. Although preliminary, our study reveals an important discrepancy, suggesting that preventive health behaviors in some domains may be regarded differently among Appalachians. Given the socioeconomic, health, and geographic challenges in Appalachia, public health officials should consider every opportunity to advance evidence-based, behaviorally oriented obesity education and prevention strategies in the region.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The University of Kentucky College of Public Health funded the Appalachian oversample via contract to Westat, Inc.
References
- 1. Behringer B, Friedell GH. Appalachia: where place matters in health. Prev Chronic Dis. 2006;3(4):A113–A117. [PMC free article] [PubMed] [Google Scholar]
- 2. Highest rates of obesity, diabetes in the South, Appalachia, and some tribal lands [press release]. Atlanta, GA: Centers for Disease Control and Prevention; November 19, 2009. https://www.cdc.gov/media/pressrel/2009/r091119c.htm. Accessed June 14, 2017. [Google Scholar]
- 3. Schoenberg NE, Huang B, Seshadri S, Tucker TC. Trends in cigarette smoking and obesity in Appalachian Kentucky. South Med J. 2015;108(3):170–177. [DOI] [PubMed] [Google Scholar]
- 4. Slack T, Myers CA, Martin CK, Heymsfield SB. The geographic concentration of US adult obesity prevalence and associated social, economic, and environmental factors. Obesity (Silver Spring). 2014;22(3):868–874. [DOI] [PubMed] [Google Scholar]
- 5. Serrano KJ, Rice EL, Patel M, Thai C, Blake KD, Vanderpool R. Comparison of cancer beliefs between Appalachians and non-Appalachians and related sociodemographic characteristics. Ann Behav Med. 2017;51(1):S85–S86. [Google Scholar]
- 6. Vanderpool RC, Huang B. Cancer risk perceptions, beliefs, and physician avoidance in Appalachia: results from the 2008 HINTS Survey. J Health Commun. 2010;15(suppl 3):78–91. [DOI] [PubMed] [Google Scholar]
- 7. Griffith BN, Lovett GD, Pyle DN, Miller WC. Self-rated health in rural Appalachia: health perceptions are incongruent with health status and health behaviors. BMC Public Health. 2011;11:229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Miller WC, Griffith BN, Bikman TJ, Meyer CM. Misconceptions about health and disease prevention behaviors of rural Appalachian Americans. Int J Med (Dubai). 2014;2(2):71–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Finney Rutten LJ, Davis T, Beckjord EB, Blake K, Moser RP, Hesse BW. Picking up the pace: changes in method and frame for the Health Information National Trends Survey (2011-2014). J Health Commun. 2012;17(8):979–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. National Cancer Institute. Health Information National Trends Survey. https://hints.cancer.gov. Accessed December 6, 2016.
- 11. US Department of Agriculture, Economic Research Service. Rural-urban continuum codes. https://www.ers.usda.gov/data-products/rural-urban-continuum-codes. Published 2003. Accessed February 3, 2017.
- 12. Appalachian Regional Commission. Subregions in Appalachia. http://www.arc.gov/research/MapsofAppalachia.asp?MAP_ID=31. Published 2009. Accessed October 20, 2017.
- 13. SAS Institute, Inc. SAS Version 9.3. Cary, NC: SAS Institute, Inc; 2011. [Google Scholar]
- 14. US Department of Agriculture, Economic Research Service. Food environment atlas. https://www.ers.usda.gov/foodatlas . Published 2009. Accessed October 13, 2017.
- 15. Fisher JL, Engelhardt HL, Stephens JA, et al. Cancer-related disparities among residents of Appalachia Ohio. J Health Dispar Res Pract. 2008;2(2):61–74. [Google Scholar]
- 16. Wewers ME, Katz M, Paskett ED, Fickle D. Risky behaviors among Ohio Appalachian adults. Prev Chronic Dis. 2006;3(4):A127–A135. [PMC free article] [PubMed] [Google Scholar]
- 17. Vanderpool RC, Huang B, Shelton BJ. Seeking cancer information: an Appalachian perspective. J Health Dispar Res Pract. 2007;2(1):79–100. [Google Scholar]
- 18. Festinger L. A Theory of Cognitive Dissonance. Stanford, CA: Stanford University Press; 1957. [Google Scholar]
- 19. Le A, Judd SE, Allison DB, et al. The geographic distribution of obesity in the US and the potential regional differences in misreporting of obesity. Obesity (Silver Spring). 2014;22(1):300–306. [DOI] [PMC free article] [PubMed] [Google Scholar]