Abstract
Background:
Isolated tearing and avulsions of the distal biceps femoris sustained during sporting activities are uncommon.
Purpose:
To systematically review the literature to identify distal biceps femoris tears and avulsions experienced during sporting activities to determine injury prevalence, sporting activities/mechanisms, management, and time to return to sport.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A systematic review was conducted investigating studies published between January 1970 and December 2017 that reported on athletes sustaining tears and avulsions of the distal biceps femoris during sporting activity. The review followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines and used the PubMed, Biosis Previews, SPORTDiscus, PEDro, and EMBASE databases. Inclusion criteria were studies reporting on (1) partial or complete tears and avulsions of the distal biceps femoris with documented sporting activity causing injury, (2) injury management (operative vs nonoperative), and (3) patient outcome. Exclusion criteria consisted of studies reporting on (1) distal biceps femoris injuries without tearing, (2) injuries secondary to nonsporting activities (mechanical falls, trauma), (3) concomitant injuries to adjacent structures about the knee, and (4) studies not reporting injury management or patient outcomes. Sporting activities, injury characteristics, management, and time to return to sport were analyzed.
Results:
A total of 22 athletes with isolated distal biceps femoris tears or avulsions were identified. Injuries were predominantly associated with noncontact knee hyperextension with concurrent hip flexion during soccer or track and field, most commonly isolated to the musculotendinous junction. Injuries were treated surgically in 91% (20/22) of athletes. Mean (±SD) overall time to return to sport was 4.9 ± 3.3 months, and for athletes who underwent operative repair, there were no significant postoperative differences based on injury location (musculotendinous junction vs avulsion, P = .25) or injury severity (partial vs complete injury, P = .13).
Conclusion:
Isolated distal biceps femoris injuries occurred primarily via noncontact mechanisms. The majority of cases were treated surgically, with successful return to sport at preinjury levels. No significant difference in return to sport was appreciated based on injury location or severity. Further studies are necessary to determine the impact of treatment method.
Keywords: biceps femoris, distal hamstrings, return to sport, avulsion, tearing, knee hyperextension
Injuries to the hamstrings are among the most frequently reported injuries in sports,10,34 accounting for a significant loss of time from competition5 and carrying high rates of recurrent injury.12,15,36 Due to increased prevalence, injuries to the proximal hamstrings are more commonly reported in the literature,4,9,10,14 while the majority of injuries to the distal hamstring are limited to small case series and case reports. As the most powerful flexor in the leg and an important dynamic stabilizer of the knee,21,32 the biceps femoris is the most commonly injured element of the distal hamstring.14,19 Injuries range from small sprains and muscle tears to partial or complete tearing of the musculotendinous junction or avulsions off the fibular head.20
Although isolated ruptures and avulsions of the distal biceps femoris are believed to occur primarily in patients with preexisting tendinopathy or dystrophic alterations within the tendon,1 injuries in young, healthy athletes participating in sport have been reported. Sporting activities commonly cited in athletes who experience tearing of the distal biceps femoris involve running, jumping, kicking, and rapid acceleration.1,5,9,21,34 Injuries to the biceps femoris have been reported in isolation or with concomitant injuries to the adjacent ligaments within the knee.31 Although surgical repair is generally advocated to restore the native anatomic features while minimizing loss of function and strength, no consensus on optimal management with regard to successful return to sport has been reported.21
The purpose of this study was to systematically review the literature to gain a better understanding of isolated tears and avulsions to the distal biceps femoris sustained in athletes participating in sport. We sought to define (1) the prevalence of isolated distal biceps femoris tears or avulsions sustained during sporting activities; (2) the mechanisms and sporting activities responsible for injury; and (3) outcomes and return-to-sport times based on management (operative vs nonoperative), tear location (musculotendinous junction vs avulsion), and extent of tearing (partial vs complete). Drawing on the available literature, we hypothesized a low prevalence of injuries occurring primarily during kicking and running, treated predominantly with operative management.
Methods
A systematic review was performed according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines using the PRISMA checklist.22 We identified all articles related to individuals sustaining isolated partial or complete tears or avulsions to the distal biceps femoris during sporting activities in studies between January 1970 and December 2017. A sporting activity was considered as one in which the athlete was in competition against fellow athletes. Two reviewers (D.M.K., K.B.M.) independently conducted the literature search in December 2017 using the following databases: PubMed, Biosis Previews, SPORTDiscus, PEDro, and EMBASE. A combination of the following search terms was used: distal hamstring AND biceps femoris AND sport AND athlete AND tear AND rupture.
Inclusion criteria for articles consisted of English language or English language translations, human subjects sustaining diagnosed isolated tears or avulsions of the distal biceps femoris with reported sporting activity causing injury, treatment (operative vs nonoperative), and patient outcome. The exclusion criteria were as follows: hamstring injuries without evidence of tearing or avulsion; athletes with distal biceps femoris injuries with concomitant injuries to the cruciate ligaments, collateral ligaments, distal semimembranosus or distal semitendinosus tendons2; injuries secondary to nonsporting activities (jogging,13 mechanical falls, trauma, or all activities not meeting the definition of a sporting activity); and studies not reporting injury treatment or patient outcomes.
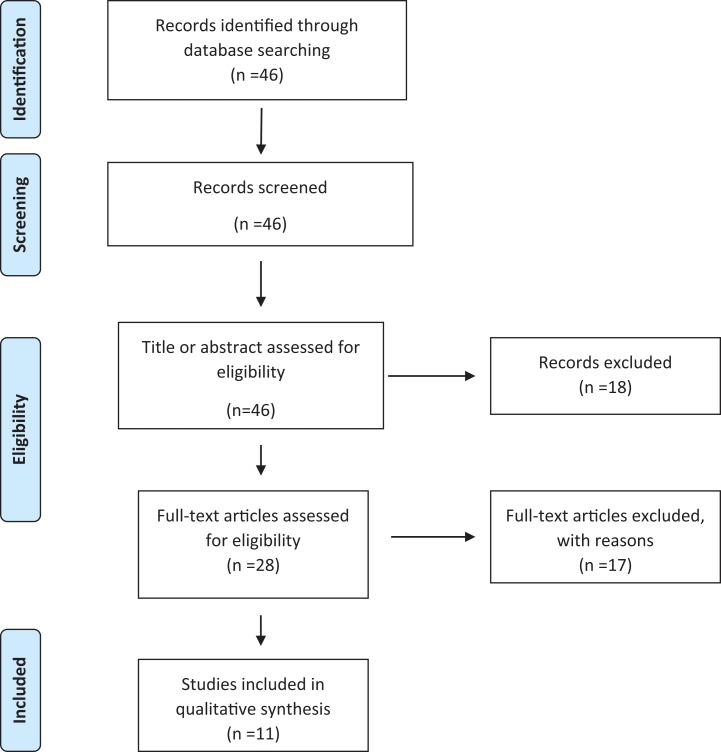
Following the 2 authors’ independent search of the database, a total of 46 citations were identified. This search process is shown in the flow diagram (Figure 1). Following title and abstract assessment, a total of 28 full-text articles were selected for further evaluation. Of these studies, 17 were excluded because they entailed injuries showing no evidence of tearing or avulsions (n = 7 studies), distal biceps femoris injuries with concomitant injuries about the knee (n = 3 studies), injuries sustained during nonsporting activities (n = 3 studies), absence of data regarding sporting activity (n = 3 studies), or absence of data regarding injury management (n = 1 study). Following application of inclusion and exclusion criteria, a total of 11 studies were identified for analysis in the review. To guarantee that all available studies were identified, references within each of the included and excluded articles were cross-referenced for inclusion in case they were overlooked during the initial search. Studies were grouped based on whether injuries were treated operatively or nonoperatively.
Figure 1.
Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) flowchart of study.
Statistical analysis was used to compare mean time to return to sport in athletes based on treatment type (operative vs nonoperative), the tear location (musculotendinous junction vs avulsions), and the extent of tearing (partial vs complete). Because of the small sample size of the included studies, a Fisher exact test was performed, with a P value of less than .05 to determine statistical significance. All statistical analysis was performed with SPSS software (v 23; IBM Corp).
Results
From the 11 studies meeting inclusion criteria, a total of 22 athletes with distal biceps femoris tearing or avulsions sustained during sporting activity were identified (Table 1). The mean (±SD) age of athletes was 30.3 ± 9.1 years, and 96% (n = 21/22) were male. Mean final follow-up time was 8.1 months (range, 2-72 months); follow-up time was not reported in 1 case.25
Table 1.
Overview of Studies Included in Reviewa
| Study | Journal (Year) | LOE | Sex (Age) | Sporting Activity | Injury Mechanism | Tear Location | Complete vs Partial Tear | Treatment | Return to Sport, mo | Complications |
|---|---|---|---|---|---|---|---|---|---|---|
| Lempainen21 | Br J Sports Med (2007) | 4 | M (40) | Ice hockey | NR | Avulsion | Complete | Surgery | 2 | None |
| M (27) | Floorball | NR | MTJ | Complete | Surgery | 3 | None | |||
| M (24) | Track | Sprinting | MTJ | Partial | Surgery | 5 | None | |||
| M (20) | Track | Long jumping | MTJ | Partial | Surgery | 3 | None | |||
| M (24) | Track | Sprinting | MTJ | Partial | Surgery | 4 | None | |||
| M (40) | Marathon | Sprinting | MTJ | Partial | Surgery | 4 | None | |||
| M (24) | Soccer | Kicking, knee hyperextension | Tendinous | Partial | Surgery | 5 | None | |||
| M (18) | Track | Sprinting | MTJ | Partial | Surgery | 2 | None | |||
| M (29) | Triathlon | Sprinting | MTJ | Partial | Surgery | 5 | None | |||
| F (24) | Road cycling | NR | MTJ | Partial | Surgery | 3 | None | |||
| M (18) | Track | Sprinting | MTJ | Partial | Surgery | 2 | None | |||
| Pan26 | Med J Malaysia (2000) | 5 | M (33) | Soccer | Kicking, knee hyperextension | Avulsion | Complete | Surgery | NR | Seroma requiring exploration |
| McGoldrick25 | Arch Orthop Trauma Surg (1990) | 5 | M (36) | Cricket | Running, knee hyperextension | MTJ | Complete | Surgery | NR | None |
| Sebastianelli28 | Clin Orthop Relat Res (1990) | 5 | M (21) | Football | Trauma, knee hyperextension, valgus load | Avulsion | Complete | Surgery | 6 | None |
| Rehm27 | Unfallchirurg (2009) | 5 | M (27) | Soccer | Running, knee hyperextension | Avulsion | Complete | Surgery | 6 | None |
| Kusma19 | Arch Orthop Trauma Surg (2007) | 5 | M (43) | Soccer | Kicking, knee hyperextension | Avulsion | Complete | Surgery | 6 | None |
| Werlich35 | Unfallchirurg (2001) | 5 | M (37) | Soccer | Kicking, knee hyperextension | Avulsion | Complete | Surgery | 12 | None |
| Valente32 | Musculoskelet Surg (2013) | 5 | M (24) | Football | Trauma, knee hyperextension, valgus load | MTJ | Complete | Surgery | 12 | None |
| Verburg33 | Ned Tijdschr Geneeskd (1991) | 5 | M (50) | Water-skiing | Fall over wave, knee hyperextension | MTJ | Complete | Surgery | 3 | None |
| Jensen18 | Scand J Med Sci Sports (1994) | 5 | M (35) | Soccer | Kicking, knee hyperextension | MTJ | Complete | Surgery | 3 | None |
| M (30) | Soccer | Kicking, knee hyperextension | MTJ | NR | Conservativeb | 0.75 | None | |||
| Fortems17 | Injury (1995) | 5 | M (44) | Indoor soccer | Kicking, knee hyperextension | MTJ | Complete | Conservativec | 4 | None |
aF, female athlete; LOE, level of evidence; M, male athlete; MTJ, tears to the musculotendinous junction; NR, not reported.
bAthlete declined surgery at the urging of the team.
cAthlete refused surgery.
Noncontact mechanisms, defined as the athlete sustaining injury without being hit by an opponent or object, accounted for 89% (n = 17/19) of injuries; no clear injury mechanism was reported in 3 athletes.21 Soccer was the most commonly reported sport in athletes sustaining injury, with injury occurring primarily when kicking the ball where the knee was hyperextended with concomitant hip flexion.17–19,21,26,27,35 Sprinting during track and field sports was responsible for the second highest rate of injuries,21 followed by American football, in which the knees of 2 athletes were forced into valgus hyperextension by an opponent.28,32 Injuries were also reported in athletes participating in ice hockey,21 floorball,21 triathlon,21 a marathon race,21 a road cycling race,21 cricket,25 and water-skiing.33
Isolated tears to the distal biceps femoris were reported in 100% of studies. Tear location was identified in all studies by use of either ultrasonography or magnetic resonance imaging (MRI). Sixty-eight percent (n = 15/22) of tears occurred within the musculotendinous junction, with 43% (n = 6/14) of tears at the musculotendinous junction being complete tears; 1 study did not detail the extent of tearing to the musculotendinous junction.18 Complete tendon avulsions from the fibular head accounted for 27% (n = 6/22) of injuries. The remaining tear was localized within the tendon.18
Injuries were treated surgically in 91% (n = 20/22) of athletes. For athletes with tearing located at the musculotendinous junction, repair was performed with suture fixation. In athletes with tendon avulsions, repair was performed with nonabsorbable suture26 or suture anchors19,21,27,28,35 via transosseous fixation accomplished by drilling through the head of the fibula with the knee in varying degrees of flexion. Suture repair was performed in the athlete found to have tearing in the intratendinous aspect of the biceps femoris.21 Postoperatively, the knee was immobilized in 30° of flexion,19 60° of flexion,28 or up to 80° of flexion26 for 1 week,27 4 weeks,28 or 6 weeks,19 followed by progression to full passive and active range of motion by approximately 6 weeks, with gradual advancement to strengthening exercises and running.
Complications were reported in only a single athlete (5%; n = 1/22): At 2 months postoperatively, an athlete had persistent discharge from an open sinus tract at the operative site requiring exploration; no evidence of infection was found, and the condition subsequently healed.26 In athletes treated nonoperatively, either surgery was refused by the athlete17 or the athlete elected for conservative management as, in one case, his return to the team was urgently needed and surgery and rehabilitation were considered to require too long an absence.18 Conservative management consisted of 3 weeks of immobilization at 30° of flexion followed by intensive physical therapy17 or was reported simply as restricted mobility.18 No subsequent injuries or limitations following athletes’ return to sport were reported in any study.
Mean overall time for return to sport was 4.9 ± 3.3 months (range, 0.75-12 months); return to sport was not recorded in 2 athletes.25,26 No significant difference was found in return-to-sport times in athletes treated with surgical management (4.7 ± 3.0 months) versus those treated nonoperatively (2.4 ± 2.3 months) (P = .35). In athletes undergoing operative repair, those with tears to the musculotendinous junction returned to sport more quickly (4.2 ± 2.6 months) compared with athletes sustaining avulsion injuries (6.4 ± 3.2 months); however, this result was not significant (P = .25). Furthermore, athletes had a faster return to play when treated surgically for partial tears at the musculotendinous junction (3.7 ± 1.2 months) compared with athletes who had avulsions or complete tears at the musculotendinous junction (5.9 ± 3.8 months); however, this result was also not significant (P = .13).
Discussion
The purpose of this study was to systematically review the literature to better define the prevalence, mechanism, management, and outcomes of partial tearing, complete tearing, and avulsion injuries to the distal biceps femoris sustained during sporting activities. We identified 22 athletes, in whom noncontact mechanisms were responsible for 84% of injuries, occurring primarily during soccer and track and field sprinting. Injuries were most commonly isolated to the musculotendinous junction. Operative management was performed in 91% of athletes, primarily via suture fixation, with concurrent use of suture anchors in athletes with avulsion injuries. Mean overall time to return to sport was 4.9 ± 3.3 months, and no significant differences were found in return time based on injury location (musculotendinous junction vs avulsion) or extent of tearing (partial vs complete) following operative repair. To our knowledge, this study represents the largest review examining distal biceps femoris tears and avulsions sustained during sporting activities.
Distally, the biceps femoris is a complex structure, arising from 2 separately innervated muscles (long head of biceps femoris and short head of biceps femoris), emerging from different origins proximally with dissimilar force vectors.16,31 The short head component, originating from the linea aspera on the posterior aspect of the femoral diaphysis, converges and coalesces with the tendon of the long head of the biceps femoris (originating from the ischial tuberosity) in the posterolateral aspect of the distal half of the thigh.6,31 In their study of 30 cadaveric knees, Terry and LaPrade31 provided detailed anatomic descriptions of the tendinous insertions of the distal biceps femoris. The authors reported that the tendinous insertion of the long head includes a direct arm inserting on the posterolateral aspect of the proximal fibula and an anterior arm inserting along the lateral edge of the proximal fibula, lateral to the fibular collateral ligament (FCL) and distally along the anterior aponeurosis in the anterior compartment of the leg. Meanwhile, the tendinous component of the short head’s direct arm inserts lateral to the fibular styloid and medial to the FCL, with the anterior arm inserting medial to the FCL and converging anteriorly with the anterior tibiofibular ligament, while also continuing laterally onto the tibia, 1 cm posterior to Gerdy’s tubercle. In a review of 106 MRIs from patients sustaining acute, indirect injuries to the distal biceps femoris, Entwisle et al16 found that the majority of injuries were isolated to the long head of the biceps (51%, n = 54/106) and attributed this to the fact that the long head crosses both the hip and knee joint, while isolated injuries to the short head component were rare (6.6%, n = 7/106).
The most commonly reported mechanism of injury entailed athletes kicking a soccer ball17–19,21,26,27,35 or during track and field sprinting.21,25 Simultaneous contraction of both the hamstrings and knee extensors during quick and forcible hip flexion with knee hyperextension has been shown to place a high tension load on the distal biceps femoris, leaving the tendon susceptible to injury.1,17,19,25 Moreover, multiple investigations have demonstrated that the highest eccentric forces placed across the distal biceps femoris occur at the myotendinous junction,9,11,23 accounting for the high rate of musculotendinous injuries. In American football athletes reporting injuries secondary to contact with an opposing athlete, the knee was forcibly hyperextended with an associated valgus force,28,32 further increasing the eccentric stress placed across the distal biceps tendon. No athlete reported a history of direct trauma to the posterior aspect of the thigh or knee, which has been shown to more commonly result in injuries to the hamstrings muscle belly.3,9
The diagnosis of tears and avulsion injuries to the distal biceps femoris depends on thorough clinical evaluation and appropriate imaging. Most athletes report a sudden, immediate sensation of pain in the posterolateral thigh, often accompanied by an audible or palpable “popping” sensation with inability to return to play.9,28,37 Athletes may report the sensation of being kicked or hit in the posterior knee despite the lack of direct contact.17,19 Subjectively, athletes report pain and stiffness in the distal posterior thigh, with weakness in knee flexion and difficulty bearing weight, while reports of instability about the knee are rare21,28 and are generally associated with multiligamentous injuries.2 Acutely, localized swelling and hematoma formation with associated ecchymosis are appreciated to the lateral aspect of the distal posterior thigh.2,21 On examination, athletes describe tenderness with palpation over the head of the fibula and posterolateral corner of the knee,3,28 with a palpable gap and visual absence of the normal posterolateral skinfold formed by the biceps femoris.13,17–19,25–27,32 A painful lump may be palpated proximal to the fibular head, indicative of hematoma and the retracted muscle.21,25 Athletes generally maintain full range of motion with knee flexion and extension; however, pain may be reported at the extremes of extension.2,26 As the biceps femoris is the strongest hamstring muscle,8 athletes generally demonstrate weakness and report posterolateral pain with resisted knee flexion13 when compared with the contralateral leg.19,28 Further evaluation is essential to determine potential concurrent injuries to the cruciate and collateral ligaments, meniscus, and other posterolateral structures in all athletes.19,29
Ultrasonography or MRI was performed to diagnose the presence of injury to the distal biceps femoris in all cases reviewed. While conventional radiographs of the knee typically fail to demonstrate any abnormalities,13,17,19,25,26,28 radiographs should be obtained to rule out concurrent fibular avulsion fractures, which are best appreciated on external and internal projections.2,14,18,19 Ultrasonography has been shown to provide high-resolution images, allowing for high diagnostic accuracy in determining the location and extent of biceps femoris injury during the acute period.3,13,17,19,23 Ultrasonography has the added benefit of permitting direction correlation with physical examination, allowing for immediate diagnosis.1 MRI remains the most commonly used and preferred imaging technique for the diagnosis of biceps femoris injuries.1 MRI allows for accurate and precise injury localization in multiple planes, enabling assessment of the extent of damage, number of tendons injured, associated soft tissue and bony injury, and the extent of muscle retraction.3,9,11,14,23,30 In chronic cases, delayed soft tissue changes and evidence of fibrosis may be visualized in the injured area on MRI.7,23
Of the 22 cases identified in this review, surgical repair was performed in 91% of athletes, while the remaining athletes were treated conservatively because of refusal to undergo surgery17 or at the preference of the athlete’s sporting organization.18 Although return-to-play times were not provided in 2 cases,25,26 all athletes undergoing surgical repair or conservative management with a stated return-to-play time reported the ability to successfully return to play at preinjury levels without limitations or complications. There was no statistically significant difference in return-to-sport times based on treatment method, but as there were only 2 cases involving conservative management, this review fails to provide any definitive evidence regarding optimal management technique with regard to return to sport timing. However, many authors stress the importance of surgical fixation because of the role of the biceps femoris in knee flexion and dynamic stabilization of the knee, citing restoration of the normal anatomic features as critical in minimizing weakness and instability and preserving function in active patients to allow successful return to sport.13,21,24,28
This study was not without limitations. Because of the strict inclusion and exclusion criteria used, the sample size obtained from our review of the literature was small, primarily limiting analyses between athletes treated surgically versus those treated conservatively. Few studies17,32 reported on the results of isokinetic strength testing to determine peak torque values in knee flexion and extension following injury management, and thus no reliable analysis associating these values with treatment choice could be conducted. Furthermore, the time from injury to treatment and the treatments used prior to operative intervention were infrequently reported, limiting our ability to determine the association between these variables and outcomes. While the majority of injuries to the distal biceps femoris have been reported to occur within the long head component, none of the included studies differentiated injuries based on those isolated to the long head or short head or involving both heads.16
In addition, because of the short follow-up times inherent within the studies included in this review, the prevalence and impact of recurrent injuries were not recorded and could not be evaluated. While additional fixation methods incorporating next-generation suture anchors and screw and washer techniques have evolved and may affect return-to-sport timing in athletes, the studies included in this review were older and did not report the use of any innovative instrumentation or fixation techniques. Due to the inherent limitations of a systematic review, the indications and justification for surgical versus conservative management were not always reported, limiting our ability to define solid criteria validating one treatment method over another. Furthermore, the delineation of a hamstring strain from a partial or complete hamstring injury was dependent on the information reported in the studies included within this review. Moreover, we suspect a selective bias in the reporting of these injuries given the small number of cases17,18 in which conservative treatment was pursued. Finally, the outcomes from this review were limited to case reports and a single case series, limiting our ability to perform additional statistical analyses and limiting the generalizability of the reported outcomes to larger populations of nonathletes.
Conclusion
Isolated tears and ruptures of the distal biceps femoris are uncommon in athletes during sporting activities. Most injuries were localized to the musculotendinous junction of the distal biceps femoris and occurred secondary to noncontact mechanisms, primarily during kicking in soccer and sprinting during track and field. Despite the lack of a significant difference in return to play that we found when comparing athletes treated surgically with those treated conservatively, we are unable to provide definitive criteria with regard to optimizing outcomes based on treatment, as there were a limited number of athletes treated conservatively in the available literature. In athletes presenting with distal posterior thigh pain, a thorough assessment with appropriate imaging is essential to rule out potential disruption of the distal biceps femoris and associated injuries to the knee. Future prospective studies examining patient outcomes based on precise injury location, time from injury to treatment, presence of concurrent injuries, and method of treatment are necessary to better define ideal management for athletes sustaining disruptions of the distal biceps femoris during sporting activities.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: J.E.V. is a paid consultant for Arthrex, Stryker, and Linvatec.
References
- 1. Ahmad CS, Redler LH, Ciccotti MG, Maffulli N, Longo UG, Bradley J. Evaluation and management of hamstring injuries. Am J Sports Med. 2013;41(12):2933–2947. [DOI] [PubMed] [Google Scholar]
- 2. Aldebeyan S, Boily M, Martineau PA. Complete tear of the distal hamstring tendons in a professional football player: a case report and review of the literature. Skeletal Radiol. 2016;45(3):427–430. [DOI] [PubMed] [Google Scholar]
- 3. Ali K, Leland JM. Hamstring strains and tears in the athlete. Clin Sports Med. 2012;31(2):263–272. [DOI] [PubMed] [Google Scholar]
- 4. Alzahrani MM, Aldebeyan S, Abduljabbar F, Martineau PA. Hamstring injuries in athletes: diagnosis and treatment. JBJS Rev. 2015;3(6). [DOI] [PubMed] [Google Scholar]
- 5. Askling C, Karlsson J, Thorstensson A. Hamstring injury occurrence in elite soccer players after preseason strength training with eccentric overload. Scand J Med Sci Sports. 2003;13(4):244–250. [DOI] [PubMed] [Google Scholar]
- 6. Branch EA, Anz AW. Distal insertions of the biceps femoris: a quantitative analysis. Orthop J Sports Med. 2015;3(9):2325967115602255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bresler M, Mar W, Toman J. Diagnostic imaging in the evaluation of leg pain in athletes. Clin Sports Med. 2012;31(2):217–245. [DOI] [PubMed] [Google Scholar]
- 8. Brunet ME, Kester MA, Cook SD, Leinhardt TM, Haddad RJ., Jr Biomechanical evaluation of superficial transfer of the biceps femoris tendon. Am J Sports Med. 1987;15(2):103–110. [DOI] [PubMed] [Google Scholar]
- 9. Clanton TO, Coupe KJ. Hamstring strains in athletes: diagnosis and treatment. J Am Acad Orthop Surg. 1998;6(4):237–248. [DOI] [PubMed] [Google Scholar]
- 10. Cohen S, Bradley J. Acute proximal hamstring rupture. J Am Acad Orthop Surg. 2007;15(6):350–355. [DOI] [PubMed] [Google Scholar]
- 11. Cohen SB, Towers JD, Zoga A, et al. Hamstring injuries in professional football players: magnetic resonance imaging correlation with return to play. Sports Health. 2011;3(5):423–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Croisier JL. Factors associated with recurrent hamstring injuries. Sports Med. 2004;34(10):681–695. [DOI] [PubMed] [Google Scholar]
- 13. David A, Buchholz J, Muhr G. Tear of the biceps femoris tendon. Arch Orthop Trauma Surg. 1994;113(6):351–352. [DOI] [PubMed] [Google Scholar]
- 14. De Smet AA, Best TM. MR imaging of the distribution and location of acute hamstring injuries in athletes. AJR Am J Roentgenol. 2000;174(2):393–399. [DOI] [PubMed] [Google Scholar]
- 15. Elliott MC, Zarins B, Powell JW, Kenyon CD. Hamstring muscle strains in professional football players: a 10-year review. Am J Sports Med. 2011;39(4):843–850. [DOI] [PubMed] [Google Scholar]
- 16. Entwisle T, Ling Y, Splatt A, Brukner P, Connell D. Distal musculotendinous T junction injuries of the biceps femoris: an MRI case review. Orthop J Sports Med. 2017;5(7):2325967117714998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fortems Y, Victor J, Dauwe D, Fabry G. Isolated complete rupture of biceps femoris tendon. Injury. 1995;26(4):275–276. [DOI] [PubMed] [Google Scholar]
- 18. Jensen I, Kramhoft M. Distal rupture of the biceps femoris muscle. Scand J Med Sci Sports. 1994;4(4):259–260. [Google Scholar]
- 19. Kusma M, Seil R, Kohn D. Isolated avulsion of the biceps femoris insertion—injury patterns and treatment options: a case report and literature review. Arch Orthop Trauma Surg. 2007;127(9):777–780. [DOI] [PubMed] [Google Scholar]
- 20. Lempainen L, Banke IJ, Johansson K, et al. Clinical principles in the management of hamstring injuries. Knee Surg Sports Traumatol Arthrosc. 2015;23(8):2449–2456. [DOI] [PubMed] [Google Scholar]
- 21. Lempainen L, Sarimo J, Mattila K, Heikkila J, Orava S, Puddu G. Distal tears of the hamstring muscles: review of the literature and our results of surgical treatment. Br J Sports Med. 2007;41(2):80–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009;62(10):e1–34. [DOI] [PubMed] [Google Scholar]
- 23. Mariani C, Caldera FE, Kim W. Ultrasound versus magnetic resonance imaging in the diagnosis of an acute hamstring tear. PM R. 2012;4(2):154–155. [DOI] [PubMed] [Google Scholar]
- 24. Marshall JL, Girgis FG, Zelko RR. The biceps femoris tendon and its functional significance. J Bone Joint Surg Am. 1972;54(7):1444–1450. [PubMed] [Google Scholar]
- 25. McGoldrick F, Colville J. Spontaneous rupture of the biceps femoris. Arch Orthop Trauma Surg. 1990;109(4):234. [DOI] [PubMed] [Google Scholar]
- 26. Pan KL, Ting F. Delayed repair of rupture of the biceps femoris tendon—a case report. Med J Malaysia. 2000;55(3):368–370. [PubMed] [Google Scholar]
- 27. Rehm O, Linke R, Schweigkofler U, Hoffmann RH, Jager A. Isolated ruptures of the tendon of the biceps femoris muscle. Unfallchirurg. 2009;112(3):332–336. [DOI] [PubMed] [Google Scholar]
- 28. Sebastianelli WJ, Hanks GA, Kalenak A. Isolated avulsion of the biceps femoris insertion: a case report. Clin Orthop Relat Res. 1990;(259):200–203. [PubMed] [Google Scholar]
- 29. Shino K, Horibe S, Ono K. The voluntarily evoked posterolateral drawer sign in the knee with posterolateral instability. Clin Orthop Relat Res. 1987;(215):179–186. [PubMed] [Google Scholar]
- 30. Slavotinek JP, Verrall GM, Fon GT. Hamstring injury in athletes: using MR imaging measurements to compare extent of muscle injury with amount of time lost from competition. AJR Am J Roentgenol. 2002;179(6):1621–1628. [DOI] [PubMed] [Google Scholar]
- 31. Terry GC, LaPrade RF. The biceps femoris muscle complex at the knee: its anatomy and injury patterns associated with acute anterolateral-anteromedial rotatory instability. Am J Sports Med. 1996;24(1):2–8. [DOI] [PubMed] [Google Scholar]
- 32. Valente M, Mancuso F, Alecci V. Isolated rupture of biceps femoris tendon. Musculoskelet Surg. 2013;97(3):263–266. [DOI] [PubMed] [Google Scholar]
- 33. Verburg H, Keeman JN. Complete rupture of the tendon of the biceps muscle of the thigh. Ned Tijdschr Geneeskd. 1991;135(42):1970–1971. [PubMed] [Google Scholar]
- 34. Volpi P, Melegati G, Tornese D, Bandi M. Muscle strains in soccer: a five-year survey of an Italian major league team. Knee Surg Sports Traumatol Arthrosc. 2004;12(5):482–485. [DOI] [PubMed] [Google Scholar]
- 35. Werlich T. Isolated rupture of the biceps tendon of the knee joint. Unfallchirurg. 2001;104(2):187–190. [DOI] [PubMed] [Google Scholar]
- 36. Woods C, Hawkins RD, Maltby S, et al. ; Football Association Medical Research Programme. The Football Association Medical Research Programme: an audit of injuries in professional football—analysis of hamstring injuries. Br J Sports Med. 2004;38(1):36–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Worrell TW. Factors associated with hamstring injuries: an approach to treatment and preventative measures. Sports Med. 1994;17(5):338–345. [DOI] [PubMed] [Google Scholar]