Abstract
Background:
Gustilo IIIB tibial fractures are associated with high rates of infection and nonunion. This study evaluates the impact of factors such as patient demographics, mechanism of injury, time to the first debridement, and time to flap coverage on the union and infection rates.
Materials and Methods:
A retrospective analysis was performed on all patients with open tibial fractures who presented to our tertiary trauma center over 13 years from April 2000 to August 2013. All patients were followed for at least 6 months and continued till radiographic evidence of union (maximum 72 months). Time to fracture union was based on radiological evidence of callus bridging at least three cortices. Information on infection rates and the presence of microbes were evaluated.
Results:
A total of 120 patients were analyzed. The mean time to fracture union was 33.8 weeks. Younger age was associated with a lower risk of nonunion with the mean age being 30.4 years in union group compared to 38.2 in the delayed-union group. Smoking was associated with an increased risk of delayed union with revision surgery being needed in 61.5% of smokers compared to 36.4% in nonsmokers. Rates of infection were high at 30.3%. Smoking was associated with an increased risk of infection (65.4% vs. 24.7%).
Conclusion:
High-energy open tibia fractures required an average of 8.5 months to heal and delayed or nonunion at an earlier juncture cannot be assumed.
Keywords: Infection, nonunion, tibia fracture, trauma, open fracture
MeSH terms: Tibia fractures, open fractures, infection
Introduction
The tibia is reported to be the most commonly fractured long bone in the human body.1 Gustilo-Anderson IIIB injuries are a major challenge requiring aggressive debridement, adequate fixation, and early coverage of soft tissue defect. These fractures occur as a result of high-velocity injuries, such as a fall from height or a crush injury. A small but significant proportion of fracture will occur in patients with multiple injuries.2 These fractures are associated with high infection3 and nonunion rates and may result in limb loss in an otherwise fit and healthy adult.4 An understanding of its epidemiology and pathogenesis allows the surgical team to better plan and allocate resources for fixation and soft tissue coverage so as to ensure the best outcome for the patient. It is also well published that the outcomes of open fractures vary by institution.1,5 The main outcome criteria for assessing open tibial fractures in the literature include infection, nonunion, and amputation. The outcome of open fractures is also a good indicator of the quality of care in any institution.6
The objective of this study was to evaluate the impact of factors, such as patient demographics, mechanism of injury, time to the first debridement, and time to flap coverage on the union and infection rates in patients with Gustilo-Anderson IIIB tibial fractures.
Materials and Methods
The National University Hospital (NUH) serves the Western central part of Singapore and is the primary receiving center for road traffic accidents occurring on three major expressways. It is also a tertiary referral center for complex trauma referred from other hospitals. Western Singapore is mostly industrialized, with a major container port and an oil refinery.
A retrospective analysis was performed on all patients with open tibial fractures who presented to NUH over 13 years from April 2000 to August 2013. The management of all patients comprised: prompt debridement, fixation, and flap coverage as feasible, which is consistent with the British Orthopaedic Association guidelines.7 Patient demographics, mechanism of injury, time to definitive fixation, flap coverage, union, and complications were recorded. The data were obtained from patient records and digital radiographs. Patients who underwent amputation were excluded from the analysis for union rates. Local ethical approval for our research study was obtained through our Institutional Review Board.
The minimum follow up period was 6 months, and follow up was continued till radiographic evidence of union (maximum 72 months). Inclusion criteria were all adults (age ≥18 years) with open diaphyseal tibial fractures who presented during the study. Patients were identified through operative records as well as in-house electronic discharge coding. Patients with delayed presentations (i.e., referrals from other local and overseas centers) were excluded from this study.
Fracture union was based on radiological evidence of callus bridging at least three cortices. Assessment of radiographic union was independently performed using two of the authors. Information on infection rates and the presence of microbes was obtained from clinical notes that documented infection as well as bacteriological cultures from operative samples. Deep infection was defined as infection requiring surgical debridement with positive deep tissue or bone cultures.
Statistical analysis was performed using the Statistical Package for the Social Sciences version 16.0 (SPSS Inc, Chicago, IL, USA). For comparison of means, the t-test or analysis of variance was used for parametric versus. continuous variables. For parametric data comparisons, the Chi-square test was used. Where the data were not normally distributed, analysis was performed on the log10 value.
Results
A total of 385 patients were analyzed, of which 120 patients had Gustilo IIIB fractures. One patient died after external fixation secondary to intracranial hemorrhage and was excluded from the analysis. Sixteen patients were lost to follow up. All patients received intravenous antibiotics and were operatively managed, undergoing at least a thorough wound debridement and temporary fracture stabilization at the initial operation.
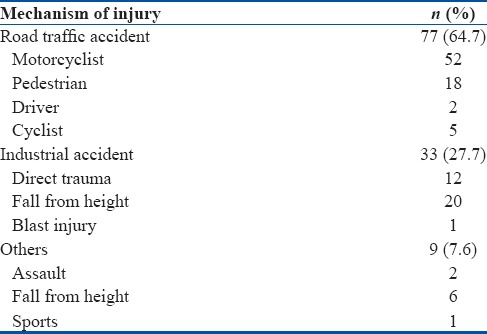
The mean age of the patients was 38.2 years (range 18–70 years). There were 111 males (93.2%) and eight females. Seventy seven cases (64.7%) were the result of motor vehicle accidents, 33 resulted from industrial accidents, and nine resulted from other causes. Sixty five cases involved the right leg, and 54 involved the left leg. The demographics are shown in Table 1 and the mechanisms of injury are shown in Table 2.
Table 1.
Demographic data
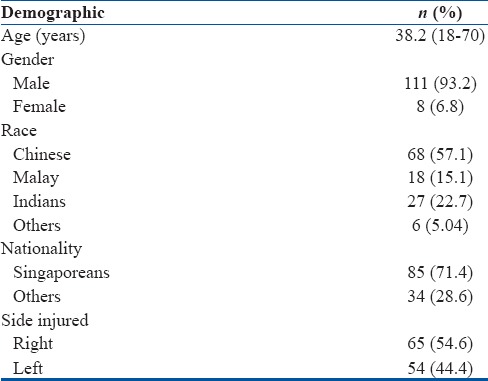
Table 2.
Mechanism of injury
Forty four patients (29.3%) had multiple injuries, whereas the rest had isolated tibia fractures. Mean time to definitive fixation was 9 days with 44 treated with intramedullary nailing, forty with plating and 32 with external fixation. Three patients required amputations due to severe shortening or infection. Two patients ended up with severe shortening and bone loss that were deemed to be not amenable to reconstruction after debridement. One patient developed flap failure with infection but was not keen for further surgeries and opted for amputation. This patient was a foreigner and was not able to stay in Singapore for long and wanted to have a single operation with a prosthesis before going back to his native country.
One patient required further bone procedure but declined surgery and is currently on follow up at 72 months with nil evidence of union. This patient was excluded from the analysis to prevent skewing of results.
Time to union
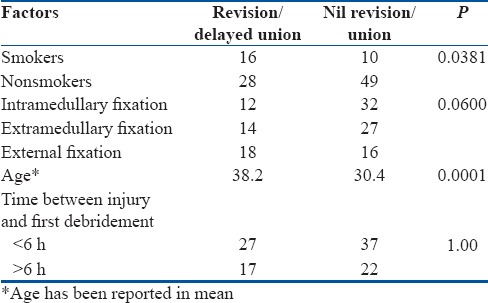
The mean time to fracture union was 33.8 weeks (range 8–84 weeks), and 42 (41.1%) patients needed further procedures due to the delayed union. Twenty two patients required further bone procedures such as bone grafting and twenty patients had dynamization of their intramedullary nails performed. Younger age was associated with a lower risk of delayed union with the mean age being 30.4 years in the union group compared to 38.2 in the nonunion group. Smoking was associated with an increased risk of nonunion with revision surgery being needed in 61.5% of smokers compared 36.4% in nonsmokers. This was statistically significant as well (P < 0.05). Earlier surgical debridement did not affect union rates [Table 3].
Table 3.
Factors related with delayed union following tibia open fractures requiring revision
Types of fixation
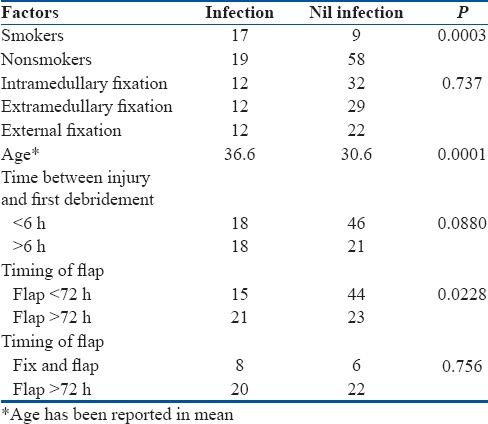
Forty four patients underwent fixation with an intramedullary device, 41 patients had an extramedullary device, and 34 patients had external fixation as their definitive mode of fixation. There were no differences observed with regards to time to union between all these three modalities [Table 3]. There were also no differences observed in terms of infection between the three modes of definitive fixation in the analyses [Table 4].
Table 4.
Factors related with infection following tibia open fractures requiring revision
Flap coverage
All patients required flap coverage. Mean time to definitive flap coverage in those patients that was 7.2 days. Mean number of operations done per patient was 7.8. In terms of flap coverage, early soft tissue coverage within 72 h reduced risks of infection. In cases where definitive fixation and flap coverage was taken at the same time, there was no reduction of risk of infection seen [Table 4].
Infection rates
Rates of infection were also high at 30.3% or affecting 36 of the patients. Smoking was associated with an increased risk of infection and need for revision [Tables 3 and 4]. Infection occurred in 65.4% of the smokers and in 24.7% of the nonsmokers. Both of these values were statistically significant with P < 0.05. Earlier surgical debridement within 6 h did not show any significant reduction in infection rates.
Discussion
This is the largest series of open tibial Gustilo IIIB fractures reported to date. Smaller series on open tibial shaft fractures have been published by Gopal et al. (84 fractures),8 Reuss and Cole (81 fractures)9 and Naique et al. (73 fractures).10 Our results are comparable with those published in other studies.2,11,12,13 It is well known and published that Gustilo IIIB fractures are associated with an increased risk of nonunion, deep infection, osteomyelitis, flap failure, and amputation.14
In our series, a large number of the open tibial fractures have been caused by road traffic accidents with 64.7% of the cases being due to road traffic accidents. Court-Brown et al. reported that road traffic accidents contributed to only 58% of open tibial fractures in Edinburgh, Scotland1 while Ikem et al. noted that 71% of their cases in Nigeria were due to traffic accidents.5
In this series, open tibial fractures occur more commonly in the younger male population who are economically active. Nearly 93.2% of our population was male as compared to other studies in other developed nations that reported 66% of these fractures occurring in the male population.1 In Nigeria, the males accounted for 69% of the open tibial fractures. It is however, interesting to note that in our neighboring country, Malaysia, 84.6% of open tibial fractures occurred in the male population as per their trauma database.15 The study also had a significant number of foreigners making up 28.6% of the patients and these may have thus skewed the percentages. This is also the first series to look at Gustilo IIIB fractures, and it is possible that higher Gustilo grade fractures may be occurring in the male population given the higher energy in these fractures and involvement of this population in construction work. Moreover, our hospital also serves a large western part of Singapore where there is a larger coverage of industrial areas.
In our series, delayed union was seen in 42 patients who required further intervention. Templeman et al. recommended early bone procedures to promote bone healing for severe open fractures.16 A total of 22 patients underwent bone grafting in our series and all of these patients went into the union. Only one patient in the series had nonunion, but this was because this patient refused any further intervention and is still on followup until 72 months.
We also did not find any difference with regards to infection and union rates when comparing between the different modalities of definitive fixation (intramedullary, extramedullary, and external fixation). This has been consistent with the data in the current literature with regards to fixation in Gustilo IIIB fractures without any modality being superior to the other.14
The timing of debridement has been controversial in open tibia fractures. The oft-quoted 6-h rule for operating on open fractures is not evidence-based,17,18 as the 2010 guidelines from the British Orthopaedic Association Standards for Trauma7 have recommended that open lower limb fractures be managed in a tertiary referral center with no mention of a specific time frame for most open fractures. In our series, this was shown as well as earlier surgical debridement did not reduce the risk of infection or nonunion. Naique et al. compared the management of open tibial fractures in local centers with specialist centers and found that local centers experienced a higher rate of revision surgery and complications.10 Our institution, which possesses a full complement of general surgical trauma support with orthopedic, vascular, plastic, and microsurgical expertise, aims to operatively manage all open fractures as soon as possible. Reuss and Cole, however, found that delayed operative management of up to 48 h did not adversely affect nonunion and infection rates in their study of 81 cases of open tibial shaft fractures.9
The timing for soft-tissue coverage in open tibial fractures is controversial. Some advocate early flap coverage,10 whereas others advocate delayed wound closure.19 Our series showed that earlier flap coverage within 72 h reduced infection rates, but a single stage “fix and flap” procedure did not seem to reduce infection rates in patients. In a review by Caudle and Stern, it was reported that for Gustilo IIIB fractures, soft-tissue coverage within (versus after) 1 week resulted in lower rates of infection (8% vs. 59%) and nonunion (23% vs. 77%).20 Infection rates were lower in the early than late flap coverage group (4% vs. 50%).21 In Gustilo IIIB and IIIC open tibial fractures treated with single-stage “fix and flap” procedures, the flap failure rate was 3.5%, and the deep infection rate was 9.5%.8
The infection rate for Grade IIIB open fractures has been reported to be between 8.5% and 52%.8,10,16,22,23,24,25 Our reported infection rate is 34.3% which is well within the reported rates for Gustilo IIIB fractures. Important factors that reduce the rate of infection include adequacy of debridement, younger age, and no history of smoking. Smoking has been a strong predictor with regards to infection and union rates and in our series; this was again seen with an increased risk of delayed union and infection in smokers as compared to nonsmokers. Schmitz et al. reported an increased time of healing of tibial fractures in smokers26 and in a separate systemic review by Patel et al., they concluded that smoking has a negative effect on bone healing, in terms of delayed union, nonunion, and more complications such as infection.27
This study, however, is not without its limitations. First, this was a retrospective single-institution review, where the patient population (from the industrial area) that our hospital serves is unlike the rest of the country. In addition, there was a relatively high number of patients lost to follow up making up 13.3% of the study population due to the significant proportion of injuries occurring in foreign industrial workers who returned to their country of origin once they were fit to travel. Factors affecting the decision to perform early or late flap coverage were not known. The definition of Gustilo IIIB fractures is not as specific as described in newer classifications,28,29 but it remains the most commonly used classification. In addition, functional outcomes, patient preferences, and costs were not compared.
Conclusion
High-energy open tibia fractures required an average of 8.5 months to heal and delayed or nonunion at an earlier juncture cannot be assumed. Despite early fixation and flap coverage, more than one-third of the fractures required further intervention. Early flap coverage within 72 h reduced rates of infection. However, rates of infection and need for revision surgery was also noted to be high in all these fractures with smoking being a significant risk factor. Younger age was associated with reduced risks of infection and delayed union. We recommend that management of these fractures to strictly follow international guidelines and implementation of a multidisciplinary team approach with nil need to rush in for early surgery unnecessarily.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Court-Brown CM, Rimmer S, Prakash U, McQueen MM. The epidemiology of open long bone fractures. Injury. 1998;29:529–34. doi: 10.1016/s0020-1383(98)00125-9. [DOI] [PubMed] [Google Scholar]
- 2.Pollak AN, McCarthy ML, Burgess AR. Short-term wound complications after application of flaps for coverage of traumatic soft-tissue defects about the tibia. The Lower Extremity Assessment Project (LEAP) Study Group. J Bone Joint Surg Am. 2000;82-A:1681–91. [PubMed] [Google Scholar]
- 3.Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: Retrospective and prospective analyses. J Bone Joint Surg Am. 1976;58:453–8. [PubMed] [Google Scholar]
- 4.Giannoudis PV, Papakostidis C, Roberts C. A review of the management of open fractures of the tibia and femur. J Bone Joint Surg Br. 2006;88:281–9. doi: 10.1302/0301-620X.88B3.16465. [DOI] [PubMed] [Google Scholar]
- 5.Ikem IC, Oginni LM, Bamgboye EA. Open fractures of the lower limb in Nigeria. Int Orthop. 2001;25:386–8. doi: 10.1007/s002640100277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Casparie AF. Postoperative wound infections: A useful indicator of quality of care? Ned Tijdschr Geneeskd. 2000;144:460–2. [PubMed] [Google Scholar]
- 7.British Orthopaedic Association Standards for Trauma (BOAST) guideline to lower limb open fractures. [Last accessed 2010 Feb 10]. Available from: wwww.bapras.org.uk/guide.asp?id=355#guide_278 .
- 8.Gopal S, Majumder S, Batchelor AG, Knight SL, De Boer P, Smith RM. Fix and flap: The radical orthopaedic and plastic treatment of severe open fractures of the tibia. J Bone Joint Surg Br. 2000;82:959–66. doi: 10.1302/0301-620x.82b7.10482. [DOI] [PubMed] [Google Scholar]
- 9.Reuss BL, Cole JD. Effect of delayed treatment on open tibial shaft fractures. Am J Orthop (Belle Mead NJ) 2007;36:215–20. [PubMed] [Google Scholar]
- 10.Naique SB, Pearse M, Nanchahal J. Management of severe open tibial fractures: The need for combined orthopaedic and plastic surgical treatment in specialist centres. J Bone Joint Surg Br. 2006;88:351–7. doi: 10.1302/0301-620X.88B3.17120. [DOI] [PubMed] [Google Scholar]
- 11.Papakostidis C, Kanakaris NK, Pretel J, Faour O, Morell DJ, Giannoudis PV. Prevalence of complications of open tibial shaft fractures stratified as per the Gustilo-Anderson classification. Injury. 2011;42:1408–15. doi: 10.1016/j.injury.2011.10.015. [DOI] [PubMed] [Google Scholar]
- 12.Soni A, Tzafetta K, Knight S, Giannoudis PV. Gustilo IIIC fractures in the lower limb: Our 15-year experience. J Bone Joint Surg Br. 2012;94:698–703. doi: 10.1302/0301-620X.94B5.27948. [DOI] [PubMed] [Google Scholar]
- 13.Rohde C, Greives MR, Cetrulo C, Lerman OZ, Levine JP, Hazen A. Gustilo grade IIIB tibial fractures requiring microvascular free flaps: External fixation versus intramedullary rod fixation. Ann Plast Surg. 2007;59:14–7. doi: 10.1097/SAP.0b013e31803403c8. [DOI] [PubMed] [Google Scholar]
- 14.Saddawi-Konefka D, Kim HM, Chung KC. A systematic review of outcomes and complications of reconstruction and amputation for type IIIB and IIIC fractures of the tibia. Plast Reconstr Surg. 2008;122:1796–805. doi: 10.1097/PRS.0b013e31818d69c3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jamaluddin SF, Wahab MA, Mohamed FL, Saiboon IM. National Trauma Database January to December 2007. Second Report Kuala Lumpur, MY: National Trauma Database; 2009. [Google Scholar]
- 16.Templeman DC, Gulli B, Tsukayama DT, Gustilo RB. Update on the management of open fractures of the tibial shaft. Clin Orthop Relat Res. 1998 May;350:18–25. [PubMed] [Google Scholar]
- 17.Sungaran J, Harris I, Mourad M. The effect of time to theatre on infection rate for open tibia fractures. ANZ J Surg. 2007;77:886–8. doi: 10.1111/j.1445-2197.2007.04266.x. [DOI] [PubMed] [Google Scholar]
- 18.Fulkerson EW, Egol KA. Timing issues in fracture management: A review of current concepts. Bull NYU Hosp Jt Dis. 2009;67:58–67. [PubMed] [Google Scholar]
- 19.Russell GG, Henderson R, Arnett G. Primary or delayed closure for open tibial fractures. J Bone Joint Surg Br. 1990;72:125–8. doi: 10.1302/0301-620X.72B1.2298770. [DOI] [PubMed] [Google Scholar]
- 20.Caudle RJ, Stern PJ. Severe open fractures of the tibia. J Bone Joint Surg Am. 1987;69:801–7. [PubMed] [Google Scholar]
- 21.Cierny G, 3rd, Byrd HS, Jones RE. Primary versus delayed soft tissue coverage for severe open tibial fractures. A comparison of results. Clin Orthop Relat Res. 1983;178:54–63. [PubMed] [Google Scholar]
- 22.Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: A new classification of type III open fractures. J Trauma. 1984;24:742–6. doi: 10.1097/00005373-198408000-00009. [DOI] [PubMed] [Google Scholar]
- 23.Singh J, Rambani R, Hashim Z, Raman R, Sharma HK. The relationship between time to surgical debridement and incidence of infection in grade III open fractures. Strategies Trauma Limb Reconstr. 2012;7:33–7. doi: 10.1007/s11751-012-0130-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chua W, Murphy D, Siow W, Kagda F, Thambiah J. Epidemiological analysis of outcomes in 323 open tibial diaphyseal fractures: A nine-year experience. Singapore Med J. 2012;53:385–9. [PubMed] [Google Scholar]
- 25.Okike K, Bhattacharyya T. Trends in the management of open fractures. A critical analysis. J Bone Joint Surg Am. 2006;88:2739–48. doi: 10.2106/JBJS.F.00146. [DOI] [PubMed] [Google Scholar]
- 26.Schmitz MA, Finnegan M, Natarajan R, Champine J. Effect of smoking on tibial shaft fracture healing. Clin Orthop Relat Res. 1999;365:184–200. doi: 10.1097/00003086-199908000-00024. [DOI] [PubMed] [Google Scholar]
- 27.Patel RA, Wilson RF, Patel PA, Palmer RM. The effect of smoking on bone healing: A systematic review. Bone Joint Res. 2013;2:102–11. doi: 10.1302/2046-3758.26.2000142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rajasekaran S, Naresh Babu J, Dheenadhayalan J, Shetty AP, Sundararajan SR, Kumar M, et al. A score for predicting salvage and outcome in Gustilo type-IIIA and type-IIIB open tibial fractures. J Bone Joint Surg Br. 2006;88:1351–60. doi: 10.1302/0301-620X.88B10.17631. [DOI] [PubMed] [Google Scholar]
- 29.Orthopaedic Trauma Association: Open Fracture Study Group. A new classification scheme for open fractures. J Orthop Trauma. 2010;24:457–64. doi: 10.1097/BOT.0b013e3181c7cb6b. [DOI] [PubMed] [Google Scholar]


