Abstract
Background:
Anterior knee pain following total knee arthroplasty (TKA) remains one of the important reasons for patient dissatisfaction. The management of patellofemoral joint is controversial and a decision whether to resurface the patella or not, is important. The present study compares the clinical and radiological outcomes between patellar resurfacing and nonresurfacing in patients undergoing bilateral TKA.
Materials and Methods:
This is a prospective comparative study with 60 patients undergoing bilateral simultaneous TKA (120 knees) with posterior stabilized Hi flex fixed bearing knee (Zimmer, Warsaw, Indiana), by two surgeons. The patients were allocated to the two groups of resurfacing versus nonresurfacing of patella. In nonresurfacing group, patellaplasty was done. Patients with clinicoradiological signs of tricompartmental arthritis were included in the study. Exclusion criteria included unilateral TKA, rheumatoid arthritis, postseptic arthritis, previous high tibial osteotomy, or unicondylar knee arthroplasty cases. Patients were assessed using Knee Society Score (KSS), Modified Samsung Medical Centre Score (MSMCS), Feller patellar score. Radiological evaluation was performed at 1 year using congruence angle and patellar tilt angle.
Results:
Mean followup was 19 months (range 12–25 months). Mean KSS, MSMCS, Feller patellar scores in resurfacing group were 82.67, 10.68, and 25.97, respectively and in nonresurfacing group were 82.93, 10.48, and 24.90, respectively. Mean congruence angle in resurfacing group was −12.83° and in nonresurfacing group was −12.383° (P = 0.917) and mean patellar tilt angle in resurfacing is 8.07 and nonresurfacing group is 7.97 (P = 0.873).
Conclusion:
There was no statistically significant difference in short-term clinical, functional, and radiological outcomes in the two groups and therefore, routine patellar resurfacing for patient undergoing TKA is not advantageous.
Keywords: Feller patellar score, Knee Society Score, patellar resurfacing, total knee arthroplasty
MeSH terms: Arthroplasty, replacement, knee, patella, patellar dislocation, patellofemoral pain syndrome
Introduction
Total knee arthroplasty (TKA) is the recommended treatment to correct deformity, relieve pain, and restore normal biomechanics in osteoarthritis of the knee joint.1 There is still controversy about the ideal treatment for patellofemoral joint arthritis, i.e., whether to resurface patella or not. Anterior knee pain (AKP) is a common reason for patient dissatisfaction, reportedly seen in up to 5%–47% of cases postprimary TKR.2,3,4 Early designs of total knee arthoplasties retained the patella. AKP being a predominant symptom prompted many surgeons to resurface the patella. Patellar resurfacing have their own complications, namely, subluxation, dislocation, loosening, patellar fracture, rupture of quadriceps tendon or patellar tendon, and patellar clunk.5,6,7 One of the controversial topics among arthroplasty surgeons is resurfacing of the patella. Three basic strategies have evolved as follows: (i) always resurface patella, (ii) never resurface, and (iii) selectively resurface patella.8 Proponents of selective resurfacing patella base their decisions on patient-related and prosthesis-related factors of preoperative weight, AKP, deformity, radiographic changes, quality of the remaining patellofemoral cartilage, intraoperative tracking, and the feasibility of patellar resurfacing.9,10,11
A metaanalysis of 1223 knees showed 14% reduction in AKP following patellar resurfacing in primary TKA.12 A randomized controlled trial (RCT) of 1715 patients showed no significant difference in functional outcomes between patellar resurfacing or nonresurfacing, using the Oxford knee score.13 Four meta-analyses of RCT comparing patellar resurfacing versus nonresurfacing14,15,16,17 have concluded that patellar resurfacing reduces the risk of reoperation, however, a reduction in AKP and improvement in knee function was not proven.
The present study compares the clinical and functional outcomes of patella resurfacing and nonresurfacing, in 120 TKA operated by two surgeons using identical implants applying Knee Society scoring system,18 Modified Samsung Medical Centre Score (MSMCS),19 and Feller patellar score.20 Radiological assessment was made using congruence angle and patellar tilt angle.
Materials and Methods
60 patients (120 knees) undergoing bilateral simultaneous TKR were allocated to two arthroplasty surgeons. One of the senior authors who believed in resurfacing performed 60 TKA with patellar resurfacing and the other senior author performed the same number without patellar resurfacing. This prospective comparative study comparing resurfacing versus nonresurfacing in TKA was undertaken after the approval of institutional review board in 2012. Patients were included in the study after obtaining informed written consent. All cases underwent simultaneous bilateral TKA between August 2012 and June 2014 using identical surgical protocol, implants, and rehabilitation care. Patients who decided to get operated by the surgeon who believed in patellar resurfacing underwent resurfacing, and patients who underwent surgery under other surgeon who believed in nonresurfacing underwent patellar nonresurfacing with patelloplasty.21 Other than the two different methods of managing patella, all other factors were kept constant in between two groups such as same surgical protocol, similar implants, and rehabilitation care. Patients with clinical and radiological signs of femorotibial and patellofemoral arthritis in both the knees were enrolled into the study, patient to medical fitness exclusion criteria included patients with rheumatoid arthritis, postseptic arthritis, previous operated high tibial osteotomy or unicondylar knee arthroplasty cases. All cases who underwent unilateral TKA were also not included in the study, as the nonoperative side pain and deformity will affect the outcome scores.
All patients underwent single-stage bilateral TKA using subvastus approach and were implanted with posterior stabilized/posterior cruciate substituting Zimmer Hi flex fixed bearing knee (Nexgen, Zimmer, Warsaw, Indiana). Patellar denervation and osteophyte resection were done in both groups, thus excluding the effect of denervation reflecting on the outcome scores. In patellar nonresurfacing group, patellaplasty was also done as described by Agarwala et al.21 In patellar resurfacing group, the patellar thickness was measured first and an appropriate thickness of the patella was resected and cemented with polyethylene dome-shaped patellar component (Nexgen, Zimmer, Warsaw, Indiana, USA) to recreate the original thickness.
Postoperative protocol
All patients received three doses of first-generation cephalosporin perioperatively with one dose preoperatively and two doses postoperatively. Patient-controlled analgesia for pain management and low-molecular-weight heparin with venous foot pumps for DVT prophylaxis was given. All patients were subjected to same rehabilitation protocol with an active range of motion exercises and mobilization with walker started on the first postoperative day. Patients were assessed clinically at 2 weeks, 6 weeks, 3 months, 6 months, 1 year, and yearly thereafter, with respect to the improvement of function and range of motion, AKP and ability to climb stairs. Any problems related to patellofemoral articulation and complications of patellar replacement such as the loosening of patellar component, patellar fracture, dislocation, subluxation, rupture of patellar tendon, or quadriceps were noted. Knee function was assessed using Knee Society Score (KSS), MSMCS, Feller patellar score. Radiological assessment was made at 1 year using congruence angle and patellar tilt angle.
Statistical method used
Statistical analysis was performed using GraphPad software version 6.0 by a statistical consultant with the level of significance being 0.05. Comparison of means was performed using the independent-samples t-test for continuous variables and the Mann–Whitney U-test for skewed variables. Fisher's exact test was used for categorical variables, and Chi-square test was used for dichotomous variables.
Results
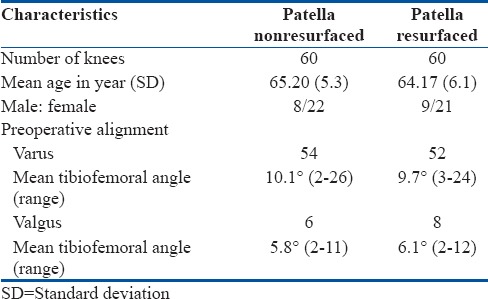
Both the groups were similar in baseline characteristics such as age, preoperative mechanical alignment indices, and male/female ratio [Table 1]. All patients were followed up for a minimum of 1 year with an average followup of 19 months (range 12–25 months) and no patient lost to followup. Mean followup in resurfacing group was 18.8 months (range 12–24 months) and in nonresurfacing group was 19.2 months (range 12–25 months). No postoperative or intraoperative complications were seen in both the groups.
Table 1.
Baseline characteristics of patella resurfacing and nonresurfacing group
Pain
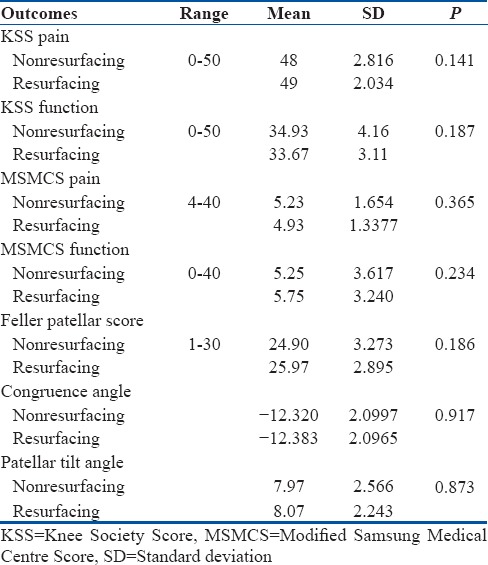
The pain was measured using Knee Society pain score, Modified Samsung Medical center score, and Feller patellar score [Table 2]. Mean knee society pain score in resurfacing group was 49 and in nonresurfacing group was 48 (P = 0.141). Modified Samsung Medical center pain score in resurfacing group was 4.93 and in nonresurfacing group was 5.23 (P = 0.365). Feller patellar score in resurfacing group was 25.97 and in nonresurfacing group was 24.90 (P = 0.186), which is statistically insignificant. AKP on stair climbing was present in 7 knees in 5 patients in patellar resurfacing group and in 9 knees in 6 patients in nonresurfacing group which was statistically not significant (P > 0.05). All the patients with AKP were managed conservatively and did not require any surgical intervention.
Table 2.
Clinical and radiological outcomes (at mean followup of 19 months)
Functional outcome
Mean Knee Society functional score in resurfacing group was 33.67 and in nonresurfacing group was 34.93 (P = 0.187). No statistically significant difference (P = 0.234) was observed in the two groups using Modified Samsung Medical center functional score (resurfacing group −5.75 and in nonresurfacing group −5.25).
Radiological outcome
Mean congruence angle in resurfacing group was −12.83° and in nonresurfacing group was −12.383° (P = 0.917). There is no significant difference (P = 0.873) in mean patellar tilt angle in resurfacing (8.07) and nonresurfacing group (7.97).
Discussion
Total knee replacement has revolutionized the treatment of arthritis of knee joint by providing significant pain relief, improving function, and walking ability, thus restoring a good quality of life. Earliest designs of total knee arthroplasties focused on tibiofemoral replacements but increased patellofemoral and extensor mechanism complications led to change in femoral component designs with the addition of a trochlear flange to allow normal patellar tracking.22,23 Despite these improvements in implant design, the problem of AKP persisted which encouraged many surgeons in the 80s to resurface patella.24 Overtime, patellar resurfacing surgeries started having their complications specific to patellofemoral articulation, despite improvements in design and surgical techniques.5,6,7 Subsequent modifications in implant design allowed the surgeon to opt for nonresurfacing. Increased awareness of component orientation and rotation have also improved the results with regard to patellofemoral articulation after TKA.25
Numerous systematic reviews,26,27 meta analysis,10,12 and randomized controlled trials11,28,29,30,31,32 done until date comparing resurfacing with nonresurfacing have reached no consensus regarding which technique is better. Despite advances in design and surgical techniques, the reported rates of AKP in the patellar resurfacing group is 0%–47%4,9,29,32 and in the nonresurfacing group is 0%–43%.4,9,11 Studies have concluded that irrespective of the management of patella approximately 10% of the patients will still have AKP after TKA.33,34 Another complication seen with patellar resurfacing is patellar clunk syndrome.35 There are various etiologies for patellar clunk syndrome, including the high position of the patellar component, inadequate synovial tissue debridement at the upper pole of patella, abnormal patellar tilt and tracking, joint line alteration of 8 mm or more, etc.36,37,38 One of the senior authors has concluded that implant design also plays an important role in the occurrence of this syndrome.39 In his retrospective study of 208 TKA, a high rate (15%) of patellar clunk was seen in knees receiving mobile bearing prosthesis as compared to none in the fixed bearing prosthesis group.
Various different techniques have been described in the literature for the management of patella when the patella is not resurfaced, including the use of electrocautery, drills, facetectomy, bone nibblers, etc., alone or in combination.40,41 Agarwala et al.21 have described a technique of patellaplasty in which electrocautery was used to demarcate the patellar rim, then power saw was used to excise osteophytes, hypertrophied lateral facet and smoothens the articular surface. This technique of patellaplasty was used for all the 60 TKA in the nonresurfacing group in the present study. Hwang et al.41 conducted a retrospective comparative study using low contact stress mobile bearing prosthesis with patellar retention and patellaplasty in 132 knees and patellar resurfacing in 143 knees. At a minimum followup of 7 years, none of the patients in retention group required secondary resurfacing. The authors have concluded that patellar retention with patellaplasty provide superior results even in severe patellofemoral arthritis if the soft tissues are properly balanced, and a patella friendly prosthetic design is chosen.
Swedish Knee Replacement Register42 in a report of 27,372 TKA operated between 1981–1995, concluded that patient satisfaction was more in resurfacing group, but the benefit of patellar resurfacing diminished over time. Various other studies have also reported no significant difference in terms of AKP or patient satisfaction between the two groups.9,30,43,44 The study also had similar findings, i.e. no significant difference in the two groups as measured using KSS, Modified Samsung Medical center score and Feller patellar score.
Feller et al.,20 in a prospective randomized trial of 40 patients reported that 22% cases of resurfaced patella were tilted with lateral retinacular release required in 12 (24%) in resurfacing group as compared to 5 (10%) of the nonresurfaced knees. Schroeder-Boersch et al.44 reported less postoperative patellar tilt (mean 3.8°) in the resurfaced group as compared to nonresurfaced group (mean 6.4°). In the present study, we found no statistically significant difference in patellar tilt angle and congruence angle in the two groups.
Five randomized, double-blind, prospective clinical trials which included 471 knees with a followup of 2–6.3 years concluded no difference in the two groups.20,31,44,45,46 The rate of revision for patellofemoral symptoms was lower in the resurfaced group, but the reluctance to revise a resurfaced patella was found as a confounding factor due to the high complication rates reported after isolated revision of a patellar component of a total knee prosthesis.47 In a retrospective study by Seo et al.,48 the authors have found no association between the severity of the patellar articular defect and resurfacing in terms of clinical and functional outcomes. Meantime between primary arthroplasty and secondary patellar resurfacing varied from 30.9–112 months.49,50 The study has a short-term followup. Thus, there were no cases of secondary resurfacing reported. This paper agrees with other papers stating that secondary resurfacing of the patella may be required in a long term followup. A long term evaluation of this group will be required for making a conclusive argument for resurfacing or nonresurfacing in terms of knee pain requiring secondary resurfacing.
The limitation of the present study is that the followup period was short (mean = 19 months). However, there are many studies which state that the results at 1–2 years after primary or revision surgery stays the same at 5 or 10 years postoperatively.51,52 We do agree that this study evaluated the short-term outcomes between the two groups. A longer followup is required to assess the long term complications. Another shortcoming of this study is that the patients in the two groups were operated by two different surgeons leading to surgeon based bias.
Conclusion
We conclude that clinical outcomes, patient satisfaction, revision rates and complication rates were similar in the resurfacing and nonresurfacing groups in a short-term followup. On reviewing the literature and analyzing our results, we concluded that there is no evidence to resurface the patella in knees with osteoarthritis and routine resurfacing of the patella in primary TKA for osteoarthritis is not advantageous.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We are thankful to the residents and colleagues at the Department of Orthopaedics P.D. Hinduja National Hospital and Research Centre Mumbai for helping in this study. No benefits or funds were received in support of this study.
References
- 1.Scott WN, Rubinstein M, Scuderi G. Results after knee replacement with a posterior cruciate-substituting prosthesis. J Bone Joint Surg Am. 1988;70:1163–73. [PubMed] [Google Scholar]
- 2.Badhe N, Dewnany G, Livesley PJ. Should the patella be replaced in total knee replacement? Int Orthop. 2001;25:97–9. doi: 10.1007/s002640100225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barrack RL, Wolfe MW. Patellar resurfacing in total knee arthroplasty. J Am Acad Orthop Surg. 2000;8:75–82. doi: 10.5435/00124635-200003000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Patel K, Raut V. Patella in total knee arthroplasty: To resurface or not to – A cohort study of staged bilateral total knee arthroplasty. Int Orthop. 2011;35:349–53. doi: 10.1007/s00264-010-1063-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gomes LS, Bechtold JE, Gustilo RB. Patellar prosthesis positioning in total knee arthroplasty. A roentgenographic study. Clin Orthop Relat Res. 1988 Nov;236:72–81. [PubMed] [Google Scholar]
- 6.Rosenberg AG. Management of the failed metal-backed patella. Orthopedics. 1996;19:813–5. doi: 10.3928/0147-7447-19960901-32. [DOI] [PubMed] [Google Scholar]
- 7.Rand JA. Extensor mechanism complications following total knee arthroplasty. J Bone Jt Surg. 2004;86-A:2062–72. [PubMed] [Google Scholar]
- 8.Calvisi V, Camillieri G, Lupparelli S. Resurfacing versus nonresurfacing the patella in total knee arthroplasty: A critical appraisal of the available evidence. Arch Orthop Trauma Surg. 2009;129:1261–70. doi: 10.1007/s00402-008-0801-9. [DOI] [PubMed] [Google Scholar]
- 9.Burnett RS, Haydon CM, Rorabeck CH, Bourne RB. Patella resurfacing versus nonresurfacing in total knee arthroplasty: Results of a randomized controlled clinical trial at a minimum of 10 years’ followup. Clin Orthop Relat Res. 2004;428:12–25. [PubMed] [Google Scholar]
- 10.Nizard RS, Biau D, Porcher R, Ravaud P, Bizot P, Hannouche D, et al. A meta-analysis of patellar replacement in total knee arthroplasty. Clin Orthop Relat Res. 2005;432:196–203. doi: 10.1097/01.blo.0000150348.17123.7f. [DOI] [PubMed] [Google Scholar]
- 11.Kim BS, Reitman RD, Schai PA, Scott RD. Selective patellar nonresurfacing in total knee arthroplasty. 10 year results. Clin Orthop Relat Res. 1999;367:81–8. [PubMed] [Google Scholar]
- 12.Pakos EE, Ntzani EE, Trikalinos TA. Patellar resurfacing in total knee arthroplasty. A meta-analysis. J Bone Joint Surg Am. 2005;87:1438–45. doi: 10.2106/JBJS.D.02422. [DOI] [PubMed] [Google Scholar]
- 13.Breeman S, Campbell M, Dakin H, Fiddian N, Fitzpatrick R, Grant A, et al. Patellar resurfacing in total knee replacement: Five-year clinical and economic results of a large randomized controlled trial. J Bone Joint Surg Am. 2011;93:1473–81. doi: 10.2106/JBJS.J.00725. [DOI] [PubMed] [Google Scholar]
- 14.Fu Y, Wang G, Fu Q. Patellar resurfacing in total knee arthroplasty for osteoarthritis: A meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2011;19:1460–6. doi: 10.1007/s00167-010-1365-0. [DOI] [PubMed] [Google Scholar]
- 15.He JY, Jiang LS, Dai LY. Is patellar resurfacing superior than nonresurfacing in total knee arthroplasty? A meta-analysis of randomized trials. Knee. 2011;18:137–44. doi: 10.1016/j.knee.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 16.Pavlou G, Meyer C, Leonidou A, As-Sultany M, West R, Tsiridis E, et al. Patellar resurfacing in total knee arthroplasty: Does design matter? A meta-analysis of 7075 cases. J Bone Joint Surg Am. 2011;93:1301–9. doi: 10.2106/JBJS.J.00594. [DOI] [PubMed] [Google Scholar]
- 17.Chen K, Li G, Fu D, Yuan C, Zhang Q, Cai Z, et al. Patellar resurfacing versus nonresurfacing in total knee arthroplasty: A meta-analysis of randomised controlled trials. Int Orthop. 2013;37:1075–83. doi: 10.1007/s00264-013-1866-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the knee society clinical rating system. Clin Orthop Relat Res. 1989;248:13–4. [PubMed] [Google Scholar]
- 19.Lee CH, Ha CW, Kim S, Kim M, Song YJ. A novel patellofemoral scoring system for patellofemoral joint status. J Bone Joint Surg Am. 2013;95:620–6. doi: 10.2106/JBJS.K.01606. [DOI] [PubMed] [Google Scholar]
- 20.Feller JA, Bartlett RJ, Lang DM. Patellar resurfacing versus retention in total knee arthroplasty. J Bone Joint Surg Br. 1996;78:226–8. [PubMed] [Google Scholar]
- 21.Agarwala S, Sobti A, Naik S. Patellaplasty, as an alternative to replacing patella in total knee arthroplasty. Open J Orthop. 2015;5:277–82. [Google Scholar]
- 22.Insall JN, Ranawat CS, Aglietti P, Shine J. A comparison of four models of total knee-replacement prostheses. J Bone Joint Surg Am. 1976;58:754–65. [PubMed] [Google Scholar]
- 23.Ranawat CS, Insall J, Shine J. Duo-condylar knee arthroplasty: Hospital for special surgery design. Clin Orthop Relat Res. 1976;120:76–82. [PubMed] [Google Scholar]
- 24.Insall JN, Lachiewicz PF, Burstein AH. The posterior stabilized condylar prosthesis: A modification of the total condylar design. Two to four-year clinical experience. J Bone Joint Surg Am. 1982;64:1317–23. [PubMed] [Google Scholar]
- 25.Barrack RL, Schrader T, Bertot AJ, Wolfe MW, Myers L. Component rotation and anterior knee pain after total knee arthroplasty. Clin Orthop Relat Res. 2001;392:46–55. doi: 10.1097/00003086-200111000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Forster MC. Patellar resurfacing in total knee arthroplasty for osteoarthritis: A systematic review. Knee. 2004;11:427–30. doi: 10.1016/j.knee.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 27.Li S, Chen Y, Su W, Zhao J, He S, Luo X, et al. Systematic review of patellar resurfacing in total knee arthroplasty. Int Orthop. 2011;35:305–16. doi: 10.1007/s00264-010-1109-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Burnett RS, Boone JL, McCarthy KP, Rosenzweig S, Barrack RL. A prospective randomized clinical trial of patellar resurfacing and nonresurfacing in bilateral TKA. Clin Orthop Relat Res. 2007;464:65–72. doi: 10.1097/BLO.0b013e31812f783b. [DOI] [PubMed] [Google Scholar]
- 29.Campbell DG, Duncan WW, Ashworth M, Mintz A, Stirling J, Wakefield L, et al. Patellar resurfacing in total knee replacement: A ten-year randomised prospective trial. J Bone Joint Surg Br. 2006;88:734–9. doi: 10.1302/0301-620X.88B6.16822. [DOI] [PubMed] [Google Scholar]
- 30.Keblish PA, Varma AK, Greenwald AS. Patellar resurfacing or retention in total knee arthroplasty. A prospective study of patients with bilateral replacements. J Bone Joint Surg Br. 1994;76:930–7. [PubMed] [Google Scholar]
- 31.Wood DJ, Smith AJ, Collopy D, White B, Brankov B, Bulsara MK, et al. Patellar resurfacing in total knee arthroplasty: A prospective, randomized trial. J Bone Joint Surg Am. 2002;84-A:187–93. doi: 10.2106/00004623-200202000-00004. [DOI] [PubMed] [Google Scholar]
- 32.Waters TS, Bentley G. Patellar resurfacing in total knee arthroplasty. A prospective, randomized study. J Bone Joint Surg Am. 2003;85-A:212–7. doi: 10.2106/00004623-200302000-00005. [DOI] [PubMed] [Google Scholar]
- 33.Brander VA, Stulberg SD, Adams AD, Harden RN, Bruehl S, Stanos SP, et al. Predicting total knee replacement pain: A prospective, observational study. Clin Orthop Relat Res. 2003;416:27–36. doi: 10.1097/01.blo.0000092983.12414.e9. [DOI] [PubMed] [Google Scholar]
- 34.Elson DW, Brenkel IJ. Predicting pain after total knee arthroplasty. J Arthroplasty. 2006;21:1047–53. doi: 10.1016/j.arth.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 35.Hozack WJ, Rothman RH, Booth RE, Jr, Balderston RA. The patellar clunk syndrome A complication of posterior stabilized total knee arthroplasty. Clin Orthop Relat Res. 1989 Apr;241:203–8. [PubMed] [Google Scholar]
- 36.Yau WP, Wong JW, Chiu KY, Ng TP, Tang WM. Patellar clunk syndrome after posterior stabilized total knee arthroplasty. J Arthroplasty. 2003;18:1023–8. doi: 10.1016/s0883-5403(03)00447-9. [DOI] [PubMed] [Google Scholar]
- 37.Fukunaga K, Kobayashi A, Minoda Y, Iwaki H, Hashimoto Y, Takaoka K, et al. The incidence of the patellar clunk syndrome in a recently designed mobile-bearing posteriorly stabilised total knee replacement. J Bone Joint Surg Br. 2009;91:463–8. doi: 10.1302/0301-620X.91B4.21494. [DOI] [PubMed] [Google Scholar]
- 38.Ip D, Wu WC, Tsang WL. Comparison of two total knee prostheses on the incidence of patella clunk syndrome. Int Orthop. 2002;26:48–51. doi: 10.1007/s00264-001-0316-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Agarwala SR, Mohrir GS, Patel AG. Patellar clunk syndrome in a current high flexion total knee design. J Arthroplasty. 2013;28:1846–50. doi: 10.1016/j.arth.2013.03.019. [DOI] [PubMed] [Google Scholar]
- 40.Ertürk C, Altay MA, Işikan UE. Patelloplasty with patellar decompression to relieve anterior knee pain in total knee arthroplasty. Acta Orthop Traumatol Turc. 2011;45:425–30. doi: 10.3944/AOTT.2011.2590. [DOI] [PubMed] [Google Scholar]
- 41.Hwang BH, Yang IH, Han CD. Comparison of patellar retention versus resurfacing in LCS mobile-bearing total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2012;20:524–31. doi: 10.1007/s00167-011-1593-y. [DOI] [PubMed] [Google Scholar]
- 42.Robertsson O, Dunbar M, Pehrsson T, Knutson K, Lidgren L. Patient satisfaction after knee arthroplasty: A report on 27,372 knees operated on between 1981 and 1995 in Sweden. Acta Orthop Scand. 2000;71:262–7. doi: 10.1080/000164700317411852. [DOI] [PubMed] [Google Scholar]
- 43.Shoji H, Yoshino S, Kajino A. Patellar replacement in bilateral total knee arthroplasty. A study of patients who had rheumatoid arthritis and no gross deformity of the patella. J Bone Joint Surg Am. 1989;71:853–6. [PubMed] [Google Scholar]
- 44.Schroeder-Boersch H, Scheller G, Fischer J, Jani L. Advantages of patellar resurfacing in total knee arthroplasty. Two-year results of a prospective randomized study. Arch Orthop Trauma Surg. 1998;117:73–8. doi: 10.1007/BF00703446. [DOI] [PubMed] [Google Scholar]
- 45.Bourne RB, Rorabeck CH, Vaz M, Kramer J, Hardie R, Robertson D, et al. Resurfacing versus not resurfacing the patella during total knee replacement. Clin Orthop Relat Res. 1995;321:156–61. [PubMed] [Google Scholar]
- 46.Barrack RL, Bertot AJ, Wolfe MW, Waldman DA, Milicic M, Myers L, et al. Patellar resurfacing in total knee arthroplasty. A prospective, randomized, double-blind study with five to seven years of followup. J Bone Joint Surg Am. 2001;83-A:1376–81. [PubMed] [Google Scholar]
- 47.Berry DJ, Rand JA. Isolated patellar component revision of total knee arthroplasty. Clin Orthop Relat Res. 1993;286:110–5. [PubMed] [Google Scholar]
- 48.Seo SS, Kim CW, Moon SW. A comparison of patella retention versus resurfacing for moderate or severe patellar articular defects in total knee arthroplasty: Minimum 5-year followup results. Knee Surg Relat Res. 2011;23:142–8. doi: 10.5792/ksrr.2011.23.3.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Muoneke HE, Khan AM, Giannikas KA, Hägglund E, Dunningham TH. Secondary resurfacing of the patella for persistent anterior knee pain after primary knee arthroplasty. J Bone Joint Surg Br. 2003;85:675–8. [PubMed] [Google Scholar]
- 50.Khatod M, Codsi M, Bierbaum B. Results of resurfacing a native patella in patients with a painful total knee arthroplasty. J Knee Surg. 2004;17:151–5. doi: 10.1055/s-0030-1248214. [DOI] [PubMed] [Google Scholar]
- 51.Ryd L, Albrektsson BE, Carlsson L, Dansgård F, Herberts P, Lindstrand A, et al. Roentgen stereophotogrammetric analysis as a predictor of mechanical loosening of knee prostheses. J Bone Joint Surg Br. 1995;77:377–83. [PubMed] [Google Scholar]
- 52.Grewal R, Rimmer MG, Freeman MA. Early migration of prostheses related to long term survivorship. Comparison of tibial components in knee replacement. J Bone Joint Surg Br. 1992;74:239–42. doi: 10.1302/0301-620X.74B2.1544960. [DOI] [PubMed] [Google Scholar]


