Abstract
Background:
Correcting the scoliosis and stabilizing the spine in the corrected position is the basis of treatment for adolescent idiopathic scoliosis (AIS). Spinal instrumentation and derotation are the principle steps of surgery for any type of AIS. A perspicuous understanding needs to be attained regarding derotation maneuvers in practice; therefore, we intend to compare radiological outcomes following concave and convex rod derotation maneuvers to analyze their efficacy to correct selective Lenke's Type-1 scoliosis.
Materials and Methods:
Retrospectively, 88 patients with Lenke's Type-1 scoliosis who were operated with selective thoracic instrumentation were divided into two groups depending on the derotation side. Preoperative radiographs were analyzed for curve angles, thoracic apical vertebral translation, apical vertebral rotation, and coronal/sagittal balance. Postoperative and followup assessment was focused on curve correction. Correction rate of main thoracic (MT) curve and its corresponding loss of correction at final followup are calculated.
Results:
Concave group (n = 40; age 13.8 ± 1.9) and the convex group (n = 48; Age 14.3 ± 2.4) showed similar demographic characteristics. Postoperative and followup parameters showed no significant difference. Correction rate of MT curve between both groups (concave group = 69.2 ± 10.5%; convex group = 66 ± 12.8%; P = 0.20) was similar. There was minimal loss of correction at final followup among both groups (concave group = 2.2° ±5.4°; Convex group = 1.5° ± 4.8°; P = 0.52).
Conclusion:
The study results showed similar sustained satisfactory correction of flexible Lenke's type 1 scoliotic curves irrespective of the derotation maneuver used. Adequate correction, thereby restoring balance was predominantly perceived among the entire sample. Hence, convex derotation can be considered equally effective as that of concave derotation for achieving adequate correction of selective Lenke's Type-1 scoliosis.
Keywords: Adolescent idiopathic scoliosis, curve correction, derotation, posterior instrumentation
MeSH terms: Scoliosis, vertebral column, spinal curvatures, spinal cord compression, spinal manipulation
Introduction
At present, the surgery for correction of scoliosis involves bilateral multi-segmental pedicle screw constructs and derotation maneuvers that have evolved over a long period.1 Derotation maneuver implies rotating the prebent rod that is fixed to strategically placed pedicle screws along the curve that persuades the spine back to the normal plane. Maneuvers of derotation include concave rod derotation, convex rod derotation, and simultaneous double rod derotation techniques.2,3,4 These techniques are invariably used based on individual expertise and operative circumstances. Use of concave side derotation maneuver dates long back when hooks and wires were commonly used as a part of scoliosis correction, but their principles are still followed.5,6,7
However, recent advancements in implant biomechanics have led to modifications and development in technique that can be an effective alternative that provides better results.8 With the advent of pedicle screws, the drawbacks of using pedicle or laminar hooks for scoliosis correction are completely overcome.9,10 The concept of convex rod derotation became a possibility as applying pedicle screws on the convex side is easier, secure, and safer; thus, convex derotation does not put much load on the pedicle.3 Yet, this remains a debated issue. We intend to compare the radiological outcomes following concave and convex rod derotation maneuvers to analyze the efficacy of these techniques to bring adequate sustained correction of curves.
Materials and Methods
Patients from our integrated information system database with the diagnosis of Lenke's Type 1 adolescent idiopathic scoliosis who were operated for deformity correction with selective thoracic instrumentation, during the years 2008 – 2015 were included in this retrospective study. The selection was strictly restricted to Lenke's Type 1 curves (major thoracic) where unilateral rod derotation maneuver was used as a critical step to reduce the curve. Only those patients who were followed for a minimum duration of 3 years were included in study. This selection was automated and patients with curve types other than Type 1, those in whom other modalities of reduction or special instrumentation were used, and those without adequate followup were excluded, and their data were not reviewed.
All selected patients were operated by a single surgeon (PLL) with similar implants and technique. Appropriate exposure, followed by facetectomy before insertion of screws was the standard protocol. Pedicle screws were strategically placed on both sides using free hand technique with two screws in most segments and at least one screw in selected segments. Whether concave or convex derotation would be done was not predetermined but rather decided intraoperatively. As a general rule, derotation was performed from the side with more number of satisfactorily secure screws. Our procedure involved connecting a prebent rod to the screws of a selected side (concave or convex) followed by the derotation maneuver, after which a more appropriate rod would be fixed on the opposite side to complete the construct. Following reduction, thoracoplasty, by partial resection of three or more ribs at the convex side apex was done as a routine in all patients. Depending on the side from which derotation maneuver was performed, the sample was divided into Group 1 (concave group) and Group 2 (convex group).
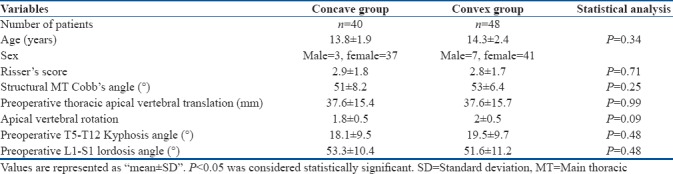
Demographic characteristics of both the groups were tabulated [Table 1]. All measurements were carried out digitally at the workstation of our picture archiving and communication system. Parameters such as preoperative proximal thoracic (PT), main thoracic (MT), and thoracolumbar/lumbar (TL/L) Cobb's angles were calculated from standing whole spine anteroposterior (AP) radiographs. Bending AP views were assessed to differentiate structural and nonstructural curves to confirm selection and classification based on Lenke's criteria.11,12 Modifiers as described in Lenke's classification, the L spine modifier and thoracic sagittal profile (T5–T12) were calculated form AP and lateral view radiographs, respectively, to determine the classification subtypes.
Table 1.
Demographic characteristics and preoperative measurements
Thoracic apical vertebral translation (TAVT) was calculated as the distance from the central sacrovertebral line (CSVL) to the center of the MT apical vertebra. Apical vertebral rotation (AVR) was classified according to “Nash-Moe” method which calculates the displacement percentage of the apical convex pedicle using AP radiographs.13,14 Sagittal T5-T12 and L1–S1 Cobb's angle were also measured using lateral radiographs. The preoperative coronal balance was measured as the distance between the CSVL and C7 plumb line in an AP view radiograph. The preoperative sagittal balance was measured as the distance between the posterosuperior part of S1 body and C7 plumb line in a lateral view radiograph. Statistical comparisons of all available preoperative parameters were carried out between the groups to check if they were significantly matched.
Immediate postoperative radiographs were assessed, and the number of screws on both concave and convex sides was noted. Anchor density of each patient was calculated by dividing the total number of screws by the total number of fixed levels. Postoperative assessment was mainly focused on curve correction using parameters, including coronal, sagittal curve angles, correction rate of MT curve, TAVT, and AVR [Figures 1 and 2]. Correction rate of the curve was measured using the formula, (preoperative Cobb's angle– postoperative Cobb's angle)/preoperative Cobb's angle ×100%. Postoperative coronal and sagittal balance were also measured. Subsequently, we measured all followup parameters that correspond to postoperative measurements to analyze if both maneuvers offered sustained correction of curves. In addition, loss of correction of MT curve was calculated as the difference between postoperative MT Cobb's angle and final followup MT cobb's angle. All available parameters were compared among both the groups to analyze if one group had better-sustained correction than the other.
Figure 1.
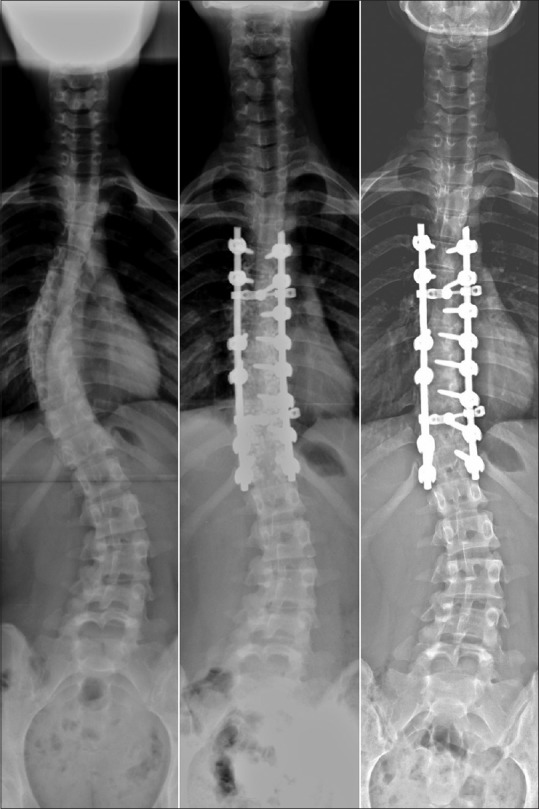
Preoperative, postoperative and followup anteroposterior view radiographs of a 15-year-old female patient from the concave group, showing portraying adequate sustained correction of curves
Figure 2.

Preoperative, postoperative and followup anteroposterior view radiographs of a 16-year-old patient from the convex group, showing equally effective outcomes as that of concave group
Statistical analysis was performed using GraphPad Prism 5 (GraphPad Software Inc., San Diego CA). We used the Student's t-test for continuous variables and Chi-square test for categorical variables. The values of P < 0.05 were considered statistically significant. This study was reviewed and approved by the Institutional Review Board of Chang Gung Memorial Hospital with IRB No – 201601846B0, and was performed in accordance with the ethical standards laid down in the most recent version of the 1964 declaration of Helsinki.
Results
The study sample consisted of 88 patients with a mean age of 14.1 ± 2.2 (10 – 20) years. There were 10 male and 78 female patients in the selected sample. Their average Risser's score was 2.9 ± 1.8. Division of our selected sample according to the derotation maneuver used intraoperatively, ensued 2 comparable groups that were termed as the concave group (n = 40, age 13.8 ± 1.9 years) and the convex group (n = 48, age 14.3 ± 2.4 years). Statistical comparison of age and Risser's score of both the groups showed no significant difference.
Preoperative mean structural MT coronal Cobb's angle was 51° ± 8.2° in the concave group and 53° ± 6.4° in the convex group. Using the supine bending AP view radiographs, we calculated the mean flexibility percentage of the MT curve which was found to be 33.6° ± 18.2° and 32.4° ± 16.2° in the concave and convex group, respectively. Concomitant presence of compensatory PT or TL/L curves were confirmed to be nonstructural, evincing the previously documented classification based on Lenke's criteria. Subtypes based on Lenke's classification, L spine modifier type A, B, and C were noticed in 44, 33, and 11 patients, respectively; sagittal thoracic profile (T5-T12) was hypo, normal, and hyper in 16, 70, and 2 patients, respectively. Parameters including MT coronal Cobb's angle, TAVT, AVR, T5-T12 Kyphosis angle and L1–S1 lordosis angle showed no statistically significant difference between the groups and hence were considered to be matched [Table 1]. Preoperative coronal balance (concave group = 10.3 ± 15.8; convex group = 7 ± 15.1) and sagittal balance (concave group = −24.7 ± 35.2; convex group = −25 ± 28.4) were also calculated to be compared with postoperative measurements.
Operative parameters including the number of fused segments and the number of pedicle screws used varied according to individual requirements. There were totally 355 fused segments in the concave group averaging 8.9 ± 1.1 segments per person; and 456 fused segments in the convex group averaging 9.5 ± 1 segments per person. There were 554 screws in the concave group, averaging 13.8 ± 2.1 screws per person; and 636 screws in the convex group averaging 13.2 ± 1.6 screws per person. Mean anchor density was found to be 1.6 ± 0.2 in the concave group and 1.4 ± 0.2 in the convex group. This difference was statistically in favor of the concave group having more anchor density (P = 0.0005).
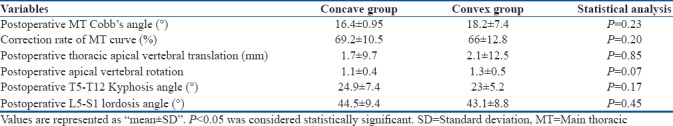
Postoperative parameters corresponding to all preoperative measurements, in addition including postoperative correction rate of MT curve were tabulated for comparison [Table 2]. Correction rate of MT curve between both the groups (concave group = 69.2 ± 10.5%; convex group = 66 ± 12.8%) revealed no significant difference (P = 0.20). This signifies that, both the derotation maneuvers achieved similar coronal curve reduction, irrespective of the concave group having more anchor density. Both techniques were impeccable in bringing TAVT toward normal. The TAVT correction achieved using both maneuvers were statistically similar between the groups (P = 0.85). Similarly, AVR also showed no significant difference between the groups postoperatively (P = 0.07). Mean T5-T12 kyphosis angle among those in the concave group (24.9° ± 7.4°) and the convex group (23° ±5.2°) had very minimal difference which was statistically insignificant (P = 0.17). Other postoperative parameters including L5-S1 lordosis angle (concave group = 44.5 ± 9.4; convex group = 43.1 ± 8.8; P = 0.45), coronal balance (concave group = 15.6 ± 16.5; convex group = 14.2 ± 15.7; P = 0.70) and sagittal balance (concave group = -23 ± 37.4; convex group = -22 ± 34.2; P = 0.88) were also found to be similar in both the groups with no significant difference.
Table 2.
Postoperative measurements
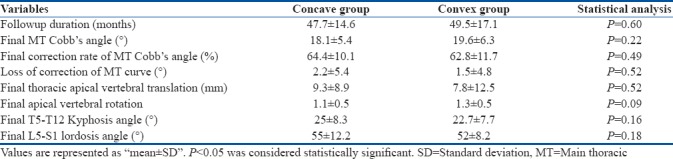
Both groups were followed up for similar durations (Concave group = 47.7 ± 14.6 months; convex group = 49.5 ± 17.1 months; P = 0.60) at least for a minimum of 36 months. There were no complications that required intervention in majority of cases belonging to both the groups. A few patients developed intercostal neuralgia which was conservatively managed. Final followup measurement of the MT coronal Cobb's angle, was similar between both the groups (P = 0.22), yet there was minimal loss of correction among patients of both the groups (concave group = 2.2° ± 5.4°; convex group = 1.5° ± 4.8°; P = 0.52) [Table 3]. Final TAVT seemed to be increased compared to postoperative measurement but remained similar between the groups. T5-T12 kyphosis angle remained the same as that of postoperative measurement even during final followup. Other parameters including L5-S1 lordosis angle, coronal balance, and sagittal balance showed no significant difference between the groups. Betterment of coronal and sagittal balance at final followup was noted among both the groups.
Table 3.
Final followup measurements
Discussion
Derotation of the prebent rod that transforms scoliosis into a kyphosis thereby restoring the sagittal profile is the principle step for deformity correction during scoliosis surgery. However, techniques vary according to individual preference and circumstances. Concave derotation maneuver dates long back to Cotrel-dubousset instrumentation when pedicle hooks were used as an essential part of the construct.2,5,6,7 However today, with the advent of pedicle screws and advancement in implant biomechanics, better correction of curves can be achieved, and potential complications are overcome.9,10,15,16 Yet, concave derotation maneuver is still practiced mainly to avoid worsening of vertebral rotation and rib hump that is said to occur if the convex side is de-rotated initially.7,17 However, among our patients, we did not encounter any worsening of AVR after correction of curves by either of these maneuvers. Moreover, none of our patients had obvious rib hump after surgery mainly because the curve magnitude of our selected patients was relatively low; besides that, we always performed thoracoplasty as a routine by partially resecting three or more ribs from the convex side apex and hence, rib hump was considered inconsequential.
We initially used the concave derotation technique, but randomly did convex side derotation depending on operative circumstances, especially when we felt one or more of the concave side screws were not stable enough. We noticed similar radiological outcomes in either of the maneuvers and hence decided to do a retrospective comparative study with a significant number of patients to analyze if our findings were mere coincidence. Our selection of concave or convex derotation maneuver was entirely based on the surgeon's perception of which side had more number of satisfactorily secure and stable screws. By this way, we made sure that adequate correction is achieved by de-rotating the secure side with the minimal load as safety was our major concern. In this study, concave group patients had more anchor density than convex group patients. This was unintentional and entirely based on intraoperative circumstances. This may have given an advantage to the concave group by means of stability but will definitely underpin the result when the convex group shows equally good outcomes.
Considerations of smaller pedicle width and a higher incidence of cortical penetration on the concave side have led to the deviation toward convex derotation.3,18 It is also considered that even a small amount of medial cortical breach on the concave side causes potential danger to the neural elements as there is a shift of the dural sac toward the concave side of the scoliotic curve.3,19 Considering these parameters, it is understood that a medial pedicle breach on the convex side is safer than the same on the concave side, especially at the apex of the curve.19 As the pedicles are larger and satisfactorily distant from each other on the convex side compared to the concave side, the prebent rod can be easily applied, and manipulation can be done without excess load.3
This reversal of concept is debated to be equally efficient in bringing similar outcomes as of the previous concave derotation maneuvers.17,20 Some authors even consider simultaneous double rod derotation maneuver to be equally effective in reducing the curve, but the superiority of it over other techniques is not satisfactorily proven.4 We only compared the radiological outcomes following concave and convex derotation maneuvers, strictly with relation to coronal and sagittal curve correction by analyzing selective parameters. The study results showed no significant difference in the amount of curve correction achieved by either of these maneuvers; however, it should be noted that the selected patients had curves that were flexible to a certain extent. All measured parameters showed no statistically significant difference between both the groups. This observation clearly makes it known that both these maneuvers are equally efficient in offering sustained correction of selective curves. Even though we only included Lenke's Type 1 curves, our findings can be considered foremost, and further research can be carried out to analyze the efficacy of these maneuvers in other curve types of greater magnitude.
Conclusion
We compared the radiological outcomes following concave and convex derotation maneuvers for reduction of selective Lenke's type 1 scoliosis, to analyze the efficacy of these maneuvers to achieve adequate, sustained correction of curves. Our results showed similar sustained satisfactory correction of Lenke's type 1 scoliotic curves that were flexible to a certain extent, irrespective of the derotation maneuver used. Adequate correction, thereby restoring balance was predominantly perceived among the entire sample. Hence, we feel both these maneuvers can be used in appropriate circumstances and such decision can be made intraoperatively, based on the screw-rod construct strength. We feel, our study is preeminent in unraveling a factual understanding toward correction biomechanics of selective scoliosis, yet being a retrospective study, limitations need to be considered.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patients have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Hasler CC. A brief overview of 100 years of history of surgical treatment for adolescent idiopathic scoliosis. J Child Orthop. 2013;7:57–62. doi: 10.1007/s11832-012-0466-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim JY, Song K, Kim KH, Rim DC, Yoon SH. Usefulness of simple rod rotation to correct curve of adolescent idiopathic scoliosis. J Korean Neurosurg Soc. 2015;58:534–8. doi: 10.3340/jkns.2015.58.6.534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anekstein Y, Mirovsky Y, Arnabitsky V, Gelfer Y, Zaltz I, Smorgick Y, et al. Reversing the concept: Correction of adolescent idiopathic scoliosis using the convex rod de-rotation maneuver. Eur Spine J. 2012;21:1942–9. doi: 10.1007/s00586-012-2355-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ito M, Abumi K, Kotani Y, Takahata M, Sudo H, Hojo Y, et al. Simultaneous double-rod rotation technique in posterior instrumentation surgery for correction of adolescent idiopathic scoliosis. J Neurosurg Spine. 2010;12:293–300. doi: 10.3171/2009.9.SPINE09377. [DOI] [PubMed] [Google Scholar]
- 5.Remes V, Helenius I, Schlenzka D, Yrjönen T, Ylikoski M, Poussa M, et al. Cotrel-dubousset (CD) or universal spine system (USS) instrumentation in adolescent idiopathic scoliosis (AIS): Comparison of midterm clinical, functional, and radiologic outcomes. Spine (Phila Pa 1976) 2004;29:2024–30. doi: 10.1097/01.brs.0000138408.64907.dc. [DOI] [PubMed] [Google Scholar]
- 6.Shah SA. Derotation of the spine. Neurosurg Clin N Am. 2007;18:339–45. doi: 10.1016/j.nec.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 7.Suk SI. Pedicle screw instrumentation for adolescent idiopathic scoliosis: The insertion technique, the fusion levels and direct vertebral rotation. Clin Orthop Surg. 2011;3:89–100. doi: 10.4055/cios.2011.3.2.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sud A, Tsirikos AI. Current concepts and controversies on adolescent idiopathic scoliosis: Part II. Indian J Orthop. 2013;47:219–29. doi: 10.4103/0019-5413.111493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu X, Yang S, Xu W, Yang C, Ye S, Liu X, et al. Comparative intermediate and long term results of pedicle screw and hook instrumentation in posterior correction and fusion of idiopathic thoracic scoliosis. J Spinal Disord Tech. 2010;23:467–73. doi: 10.1097/BSD.0b013e3181bf6797. [DOI] [PubMed] [Google Scholar]
- 10.Yilmaz G, Borkhuu B, Dhawale AA, Oto M, Littleton AG, Mason DE, et al. Comparative analysis of hook, hybrid, and pedicle screw instrumentation in the posterior treatment of adolescent idiopathic scoliosis. J Pediatr Orthop. 2012;32:490–9. doi: 10.1097/BPO.0b013e318250c629. [DOI] [PubMed] [Google Scholar]
- 11.Lenke LG, Betz RR, Clements D, Merola A, Haher T, Lowe T, et al. Curve prevalence of a new classification of operative adolescent idiopathic scoliosis: Does classification correlate with treatment? Spine (Phila Pa 1976) 2002;27:604–11. doi: 10.1097/00007632-200203150-00008. [DOI] [PubMed] [Google Scholar]
- 12.Ogon M, Giesinger K, Behensky H, Wimmer C, Nogler M, Bach CM, et al. Interobserver and intraobserver reliability of lenke's new scoliosis classification system. Spine (Phila Pa 1976) 2002;27:858–62. doi: 10.1097/00007632-200204150-00014. [DOI] [PubMed] [Google Scholar]
- 13.Lam GC, Hill DL, Le LH, Raso JV, Lou EH. Vertebral rotation measurement: A summary and comparison of common radiographic and CT methods. Scoliosis. 2008;3:16. doi: 10.1186/1748-7161-3-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nash CL, Jr, Moe JH. A study of vertebral rotation. J Bone Joint Surg Am. 1969;51:223–9. [PubMed] [Google Scholar]
- 15.Kim YJ, Lenke LG, Cho SK, Bridwell KH, Sides B, Blanke K, et al. Comparative analysis of pedicle screw versus hook instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2004;29:2040–8. doi: 10.1097/01.brs.0000138268.12324.1a. [DOI] [PubMed] [Google Scholar]
- 16.Liljenqvist U, Hackenberg L, Link T, Halm H. Pullout strength of pedicle screws versus pedicle and laminar hooks in the thoracic spine. Acta Orthop Belg. 2001;67:157–63. [PubMed] [Google Scholar]
- 17.Terai H, Toyoda H, Suzuki A, Dozono S, Yasuda H, Tamai K, et al. A new corrective technique for adolescent idiopathic scoliosis: Convex manipulation using 635 mm diameter pure titanium rod followed by concave fixation using 635 mm diameter titanium alloy. Scoliosis. 2015;10:S14. doi: 10.1186/1748-7161-10-S2-S14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smorgick Y, Millgram MA, Anekstein Y, Floman Y, Mirovsky Y. Accuracy and safety of thoracic pedicle screw placement in spinal deformities. J Spinal Disord Tech. 2005;18:522–6. doi: 10.1097/01.bsd.0000154448.90707.a8. [DOI] [PubMed] [Google Scholar]
- 19.Wang S, Qiu Y, Liu W, Shi B, Wang B, Yu Y, et al. The potential risk of spinal cord injury from pedicle screw at the apex of adolescent idiopathic thoracic scoliosis: Magnetic resonance imaging evaluation. BMC Musculoskelet Disord. 2015;16:310. doi: 10.1186/s12891-015-0766-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Uçar BY. A new corrective technique for adolescent idiopathic scoliosis (Ucar's convex rod rotation) J Craniovertebr Junction Spine. 2014;5:114–7. doi: 10.4103/0974-8237.142304. [DOI] [PMC free article] [PubMed] [Google Scholar]


