Abstract
Background:
Gustilo Anderson III B/C open tibial fractures are more difficult to manage than I, II, and III A fractures. These open tibial fractures are often associated with wound infection, soft tissue necrosis, bone nonunion, osteomyelitis or amputation. Staged treatment for this severe trauma is very necessary.
Materials and Methods:
25 cases of Gustilo Anderson IIIB/C open tibial fractures with serious soft-tissue defects treated between January 2010 and January 2015 were included in this study. The treatment was administered in three stages. The first stage included emergency debridement, external fixation, repair of damaged main blood vessels and nerves, covering of the wound, and infection control. The second stage involved skin flap or skin graft placement to repair wounds. The third stage involved replacement of the external fixator with an internal fixator and the placement of bone grafts.
Results:
All the skin flaps or skin grafts survived, and a small necrotic area in the distal flap was observed in only two cases (which resolved spontaneously after the dressing was changed). Bone union occurred at the predicted time in 23 cases, while it was delayed in 2 cases. The rate of excellent and good was 88%.
Conclusion:
Staged treatment was safe and effective for Gustilo Anderson IIIB/C tibial fractures. The timing for the placement of internal and external fixators and choosing the appropriate skin flap repair technique are important.
Keywords: External fixator, open fractures, skin flap
MeSH terms: Tibial fractures, open fractures, soft tissue injuries, surgical flaps
Introduction
Open tibial fractures are very common in the clinical setting, especially Gustilo Anderson IIIB/C open fractures, which are mostly high-energy injuries. It is very difficult to treat patients who have serious fractures with crushing of surrounding soft tissue. In addition, open tibial fractures are often associated with wound infection, soft tissue necrosis, bone nonunion, and osteomyelitis, and in extreme cases, even amputation is required. Research shows that severely contaminated wounds need to be temporarily closed in the case of patients who need to be hospitalized for a long period. Soft tissue injuries have been managed by different methods. The list includes fasciocutaneous flaps, sural flaps, propeller flaps, adipofascial flaps, pedicled muscle flaps, free perforator, and free muscle flaps. However, the outcome of treatment of these fractures is often unsatisfactory. Repeated debridement, bone handling, bone grafting, and replacement of external fixators are often necessary for the treatment of this type of tibial fracture. Thus, considering the complications and wide array of treatment requirements and options, the management of these fractures poses a great challenge for orthopedic surgeons, microscopic surgeons, and plastic surgeons.1 Between January 2010 and January 2015, 25 cases of Gustilo Anderson IIIB/C open complex tibial fractures with serious soft-tissue defects were managed at our hospital. Based on our experience, we have proposed the management of staged treatment for this severe trauma. This paper describes the treatment and its outcomes, which were found to be satisfactory.
Materials and Methods
Staged therapeutic method
(i) First stage: on admission, the patients were resuscitated by Advanced Trauma Life Support protocol. Intravenous antibiotics were administered within 3 h of admission. The neurovascular assessment was carefully made and recorded along with the description of the fracture and the other injuries. Limb salvage surgery was performed, after ensuring that the patients were stable. The wound was washed repeatedly with about 1 liter of hydrogen peroxide solution, 1 liter of dilute dynamic iodized salt water, and 5 liters of physiological saline until the raw surface was clean. Next, inactivate soft tissue, and small pieces of bone were removed, and large pieces of the fracture with soft tissue were reserved. The fracture was then fixed with a combination of external fixators to maintain the body length and fracture lines of force. In patients with Gustilo III C open tibial fractures, we repaired the damaged main blood vessels and nerves, including the anterior and posterior tibial vessels, tibial nerves, and peroneal nerves as far as possible. Soft-tissue defects of the skin wound were covered with vacuum-closed drainage until they were treated again in the second stage.
(ii) Second stage: the patient's condition usually stabilized within 7–10 days, after which skin flaps or free skin grafts were used to repair the wound. In 25 cases, the defective area of the soft tissue was 8 cm × 6 cm to 38 cm × 26 cm in size. The tendons and bones were not exposed in eight cases, in which thick free skin grafts were used to cover the wound. Free flap grafts were used to cover the wound in 12 cases: free anterolateral thigh flaps were used in eight cases, free umbilical thoracic flaps were used in three cases, and free latissimus dorsi muscle skin flaps were used in one case. Transplantation of pedicled skin flaps was performed in five cases: perforator flaps were used on the medial malleolus in three cases, and sural nerve nutrient vessel flaps were used in two cases.
(iii) Third stage: when the skin flap or skin graft had completely survived, the wound healed well and no obvious infection appeared on the external fixator needle after 3–4 weeks. In such cases, the external fixator was dismantled and replaced with the internal fixator, and the bone defect was treated with iliac bone grafts at the same time if necessary.
Patients
The study population included 25 patients (19 males and 6 females; age range 18–61 years) with Gustilo Anderson IIIB/C open tibial fractures with serious soft-tissue defects. Of these, there were four cases with Gustilo III C open tibial fractures. The defective area of soft tissues after debridement was 8 cm × 6 cm to 38 cm × 26 cm in size, and the average area was 20.6 cm × 13.1 cm. In the third stage plates were used in 9 cases; and intramedullary nail was used in 7 cases. In 12 cases, the bone defects were fixed with bone grafts; the defects were 1 cm to 4 cm in size. The bone graft was taken from the iliac bone. Internal fixation could not be done in 9 cases, in which bone transport was performed with an external fixator. The Ilizarov circular external fixator was used in six of these nine cases, and the Orthfix unilateral external fixator was used in the remaining three cases. The defects were 4 cm to 12 cm in size.
Postoperative management
The limb was elevated to reduce swelling for symptomatic treatment after surgery. The patients were also asked to perform functional exercises for their knee and ankle as early as possible and regularly take radiographs to observe healing of the fracture. The exercises with a cane were also encouraged. The period after which the internal and external fixators could be removed was decided according to the rate at which the healing progressed, and function was estimated using lower limb evaluation at the last followup. The function of the lower extremities was estimated using the Johner-Wruhs scoring system.2
Results
The patients were followed up for 14–26 months. All skin flaps or skin grafts survived. A small necrotic area in the distal flap was observed in only two cases, and it spontaneously resolved when the dressing was changed. The fracture healed within the expected time in 23 cases, and the union was delayed in 2 cases. The bone grafts used resulted in healing in all the cases. The average healing time was 9.2 months. Infection at the site of the pin was observed in two cases, but it was easily managed by the patients themselves through symptomatic treatment and adjustment of the bone pins. There was only one case of chronic osteomyelitis in which the wound was not healed, and the patient still requires regular wound dressing. All the limbs were survived, and there was no amputee. The details of all the cases are shown in Table 1. According to the Johner-Wruhs scoring system,2 the result was excellent in 16 cases, good in 6 cases, and poor in 3 cases. The rate of excellent and good was 88%. The most common complications that led to the poor results were chronic osteomyelitis and nerve injury. Figure 1 and 2 illustrate two representative cases.
Table 1.
Patient demographics and reconstruction outcomes
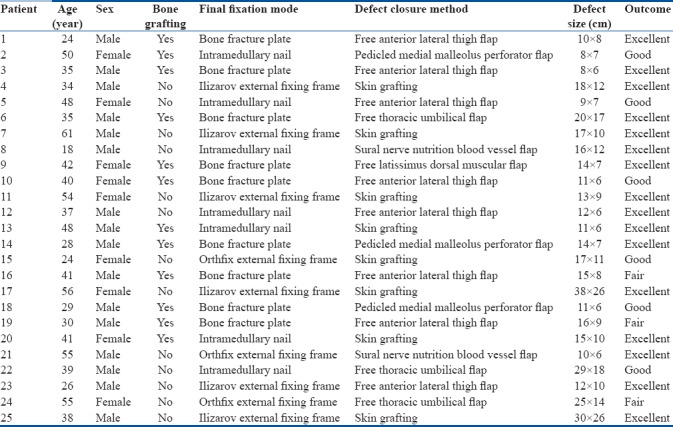
Figure 1.
(a) Clinical photograph of a patient (male, 48-year-old) who was injured in a car accident. Seven days after the emergency debridement surgery, the wound showing obvious infection (b) Clinical photograph of same patient showing that after repeated debridement, soft tissue damage and bone defect, were obvious (c and d) X-ray anteroposterior and lateral views of both bones leg showing that the external fixator was used to fix the fractures in emergency (e) Clinical photograph showing that after the wound infection was controlled, we covered the wound with a free skin graft (f) Clinical photograph showing that wound infection was in control, and the skin graft survived (g) X-ray anteroposterior view of leg bones showing that the Ilizarov circular external fixation frame was used in bone transport to treat bone defects (h) X-ray anteroposterior view of leg bones showing that the defect of the bone was about 8 cm in size, and nonunion of the bone was observed (i) The Ilizarov circular external fixation frame was removed after the bone transport was completed (j) We fixed the fracture with an intramedullary nail and the iliac bone graft was done (k) The bone callus showed obvious growth at 3 months after the internal fixation surgery (l) The fracture healed well 8 months after the internal fixation surgery (m) The internal fixation was removed 1 year after the internal fixation surgery (n) The appearance of the limb was satisfactory, and the patient resumed normal life within 14 months after the procedures (o) Clinical photograph showing that limb function was good and satisfactory
Figure 2.
(a) Clinical photograph showing that the patient (male, 26-year-old) was injured in a car accident. Seven days after the emergency debridement surgery, the wound shows obvious infection with a considerable amount of purulent secretion (b) X-ray leg bones anteroposterior view showing that the external fixator was used to fix the fractures in emergency cases, and the tibia was crushed severely. (c) Clinical photograph showing that after several rounds of debridement, wound was covered using vacuum-closed drainage. (d) After repeated debridement, we removed a lot of necrotic bone and infected soft tissue. (e) Clinical photograph showing that after repeated debridement, the infection was eliminated. (f) Clinical photograph showing that after we designed a free anterolateral thigh composite tissue flap to cover the wound. (g) Clinical photograph showing that the composite tissue flap was prepared. (h) Clinical photograph showing that after flap crossed the subcutaneous tunnel to cover the multiple irregular wounds. (i) Clinical photograph showing that the infection was controlled, and the tissue flap and skin graft survived. (j) X-ray anteroposterior view of leg bones showing that the tibial defect was about 8 cm in size. (k) Clinical photograph showing that the Ilizarov circular external fixation frame was used for bone transport to treat the bone defect. (l) X-ray anteroposterior view of leg bones showing that the Ilizarov circular external fixation frame (m) X-ray lateral view of leg bones showing the callus at 3 months after the bone transport procedure (n) Clinical photograph showing the lower limb appeared well at 1 year after the procedures. (o) X-ray of leg bones anteroposterior view at 1 year followup showing that fracture healed well
Discussion
Emergency treatment of Gustilo Anderson IIIB/C open fracture of the lower limbs
Gustilo Anderson IIIB/C open lower limb fractures are high-energy injuries that are characterized by extensive and serious injury to soft tissue and serious contamination of the wounds. In 1984, Gustilo et al. studied 75 cases of Type III open fractures reported between 1976 and 1979. The infection rates for Type IIIB and Type IIIC open fractures were 52% and 42%, respectively, while the amputation rates were 16% and 42%, respectively.3 Delayed union or nonunion occurred in 12 cases, while the patients died in 5 cases. In recent decades, with the development of internal and external fixation techniques as well as microsurgical techniques and the establishment of minimally invasive methods and breakthrough antibiotic drugs, the approach to fracture management has changed. Therefore, the treatment outcomes of this type of trauma have improved considerably. At present, Gustilo Type III open fractures are generally treated by debridement, reliable means of fracture fixation, wound coverage, and infection control. The ideal time for treatment is 6–8 h after the injury. In the case of wounds that are only slightly contaminated, one-stage fixing of Gustilo I/II and some Gustilo IIIA open fractures is usually beneficial. Many surgeons are still inclined to fix the fractures and cover the wound emergently in the case of some Gustilo IIIB open fractures in which the soft tissue is not obviously damaged, and this strategy is usually beneficial. However, in the case of serious Gustilo IIIB fractures with large bone defects and serious soft tissue injury, the ideal treatment strategy is still unclear. Many surgeons are of the opinion that it is risky to perform emergency internal fixation and flap closure of the wound, so staged surgery seems like a viable option for reducing complications in such cases. However, along with the placement of external fixators, it is also important to use small implants to fix fractures to reduce complications in later stages.4,5,6 In addition, it is very important to prevent infections in seriously contaminated wounds when the preoperative time is long. It is very difficult to remove all the polluted tissue and control for potential infections in the case of these wounds. Therefore, closing the wound emergently may not be the best option; instead, vacuum-closed drainage, and wound irrigation have been shown to have good results in the clinic. This approach has been reported to reduce the incidence of clostridial infections and gas gangrene. A study by Zalavras et al. analyzed Gustilo III open fractures in a large clinical sample and recommended that the closing of seriously contaminated wounds is delayed to within 72 h after the injury and that debridement is performed repeatedly as necessary.7,8,9
Optimal time for replacing external fixators with internal fixators for Gustilo Anderson IIIB/C open fractures of the lower limbs
Liu et al. were of the opinion that the ideal management of Gustilo IIIB or more serious open tibial fractures involves fixing the fracture with an external fixator after early debridement and repair of tissue defects with tissue flaps in the second stage.10 At present, the use of an external fixator for serious Gustilo Anderson IIIB/C open tibial fractures as the first immobilization technique is generally agreed on. However, once the infection is under control and the skin condition stabilizes, the need for strong internal fixators such as a plate or intramedullary nail in the second stage is not clear. Wani et al. used the Ilizarov circular external fixator to treat 60 cases of Gustilo II, Gustilo IIIA and Gustilo IIIB open tibial fractures and achieved satisfactory results.11 We believe that Gustilo Anderson IIIB/C tibial fractures require longer healing time. The external fixator affects the patients’ daily life activities as well as social life. Given the possibility of complications such as infection at the pin site and loosening of the pin, it is necessary to use a strong internal fixator such as the steel plate early on, as long as the patients’ condition is conducive for the placement of the fixator. Further, bone grafts should be used as supplementary methods to treat circumscribed bone defects and delayed union, to promote early healing of the fractures. Blauth et al. discovered that the infection rate increased when the indwelling time of external fixators was >28 days, so the indwelling time should ideally be <28 days. Premature conversion of internal fixator would aggravate injuries to the local soft tissue, while delayed conversion would lead to a high infection rate. On the other hand, the growth of callus of fractures also affects the resetting of internal immobilization and the placement of the fixator.12 In this study, the internal fixator was replaced 3 weeks later. Once it is confirmed that the soft tissue is not obviously contaminated and there is no necrosis, the internal fixator should be replaced early, so as not to increase the risk of pin site infection from the external fixator and to overcome the difficulties associated with placing the internal fixator. There is still some debate about the use of preventive bone grafts early on in Gustilo III open tibial fractures. The incidence of bone nonunion has been reported to be 5% in Gustilo I open tibial fractures and 8%–18% in Gustilo IIIA open fractures within 9 months after the operation in large clinical samples. Therefore, an increasing number of clinicians are considering the use of preventive bone grafts early on or bone morphogenetic protein (BMP) administration.13,14,15,16,17,18
Advantages and limitations of staged treatment for Gustilo Anderson IIIB/C open fractures of the lower limbs
In the case of severe trauma, such as Gustilo Anderson IIIB/C open tibial fractures, the fracture needs to be fixed temporarily in a simple, rapid, and effective way at its early stage. The second stage should be commenced only once the patients’ condition is conducive for a second surgery.19 Proceeding to fracture fixation and tissue repair without considering these factors would lead to severe complications.20,21 Kamath et al. summarized 151 cases of Gustilo Anderson IIIB/C open fractures: amputation was performed in 10 cases; skin flap surgery to cover the wound was performed after 10 days in 38 cases; different degrees of wound infection were observed in 44 cases; surgical intervention for delayed union was performed in 43 cases; and Ilizarov bone transport was performed in 15 cases to treat bone nonunion or bone defect.22 Thus, there is a wide range of treatments for these fractures, and the optimal method should be determined based on each patients’ condition and degree of injury. The occurrence of late complications and treatment outcomes also depend on the physicians’ skill and experience. In different stages of treatment, the injuries and prognosis should be evaluated, based on which the next steps should be decided; thus, individualized treatment and adopting the concept of staged treatment are recommended for the management of Gustilo Anderson IIIB/C fractures. At present, most surgeons perform external fixation, repair major nerve and blood vessels, and cover wounds using vacuum-closed drainage, skin flaps or myocutaneous flaps, as required. Moreover, complications such as skin and soft-tissue defects, necrosis, wound infection, bone defect, and bone nonunion are treated in the late phase.23,24
Based on all our findings, we think that it is important to correctly assess the patients’ condition and accordingly select the approach to cover the wound. When the patients’ general condition and wound infection are controlled, different kinds of skin flaps and myocutaneous flaps should be used, as appropriate, to repair the wounds and close them in the second stage. If the wound is healed in the later phase, internal fixation or other comprehensive treatments for late complications should be performed as required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) have given their consent for their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Johner R, Wruhs O. Classification of tibial shaft fractures and correlation with results after rigid internal fixation. Clin Orthop Relat Res. 1983;9:7–25. [PubMed] [Google Scholar]
- 2.Pape HC, Tornetta P, 3rd, Tarkin I, Tzioupis C, Sabeson V, Olson SA, et al. Timing of fracture fixation in multitrauma patients: The role of early total care and damage control surgery. J Am Acad Orthop Surg. 2009;17:541–9. doi: 10.5435/00124635-200909000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: A new classification of type III open fractures. J Trauma. 1984;24:742–6. doi: 10.1097/00005373-198408000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Kim JW, Oh CW, Jung WJ, Kim JS. Minimally invasive plate osteosynthesis for open fractures of the proximal tibia. Clin Orthop Surg. 2012;4:313–20. doi: 10.4055/cios.2012.4.4.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tong D, Ji F, Zhang H, Ding W, Wang Y, Cheng P, et al. Two-stage procedure protocol for minimally invasive plate osteosynthesis technique in the treatment of the complex pilon fracture. Int Orthop. 2012;36:833–7. doi: 10.1007/s00264-011-1434-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ma CH, Yu SW, Tu YK, Yen CY, Yeh JJ, Wu CH, et al. Staged external and internal locked plating for open distal tibial fractures. Acta Orthop. 2010;81:382–6. doi: 10.3109/17453674.2010.487244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zalavras CG, Marcus RE, Levin LS, Patzakis MJ. Management of open fractures and subsequent complications. J Bone Joint Surg Am. 2007;89:884–95. doi: 10.2106/00004623-200704000-00027. [DOI] [PubMed] [Google Scholar]
- 8.Giannoudis PV, Papakostidis C, Roberts C. A review of the management of open fractures of the tibia and femur. J Bone Joint Surg Br. 2006;88:281–9. doi: 10.1302/0301-620X.88B3.16465. [DOI] [PubMed] [Google Scholar]
- 9.Hoogendoorn JM, van der Werken C. Grade III open tibial fractures: Functional outcome and quality of life in amputees versus patients with successful reconstruction. Injury. 2001;32:329–34. doi: 10.1016/s0020-1383(00)00250-3. [DOI] [PubMed] [Google Scholar]
- 10.Liu FG, Chen BJ, Li HY, Cao SF, Chen JM, Fan AM. Treatment of severe open fractures with soft tissue defect of crus. Chin J Orthop Trauma. 2009;11:940–2. [Google Scholar]
- 11.Wani N, Baba A, Kangoo K, Mir M. Role of early ilizarov ring fixator in the definitive management of type II, IIIA and IIIB open tibial shaft fractures. Int Orthop. 2011;35:915–23. doi: 10.1007/s00264-010-1023-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Blauth M, Bastian L, Krettek C, Knop C, Evans S. Surgical options for the treatment of severe tibial pilon fractures: A study of three techniques. J Orthop Trauma. 2001;15:153–60. doi: 10.1097/00005131-200103000-00002. [DOI] [PubMed] [Google Scholar]
- 13.DeLong WG, Jr, Born CT, Wei SY, Petrik ME, Ponzio R, Schwab CW. Aggressive treatment of 119 open fracture wounds. J Trauma. 1999;46:1049–54. doi: 10.1097/00005373-199906000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Hope PG, Cole WG. Open fractures of the tibia in children. J Bone Joint Surg Br. 1992;74:546–53. doi: 10.1302/0301-620X.74B4.1624514. [DOI] [PubMed] [Google Scholar]
- 15.Whorton AM, Henley MB. The role of fixation of the fibula in open fractures of the tibial shaft with fractures of the ipsilateral fibula: Indications and outcomes. Orthopedics. 1998;21:1101–5. doi: 10.3928/0147-7447-19981001-09. [DOI] [PubMed] [Google Scholar]
- 16.Stegemann P, Lorio M, Soriano R, Bone L. Management protocol for unreamed interlocking tibial nails for open tibial fractures. J Orthop Trauma. 1995;9:117–20. doi: 10.1097/00005131-199504000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Bhandari M, Guyatt GH, Swiontkowski MF, Schemitsch EH. Treatment of open fractures of the shaft of the tibia. J Bone Joint Surg Br. 2001;83:62–8. doi: 10.1302/0301-620x.83b1.10986. [DOI] [PubMed] [Google Scholar]
- 18.Court-Brown CM, Keating JF, Christie J, McQueen MM. Exchange intramedullary nailing. Its use in aseptic tibial nonunion. J Bone Joint Surg Br. 1995;77:407–11. [PubMed] [Google Scholar]
- 19.Xu YQ, Lin YQ, Li J. Flap combined with external fixation for treatment of tibial fractures with crus soft tissue defect. Chin J Microsurg. 2004;27:164–5. [Google Scholar]
- 20.Farouk O, Krettek C, Miclau T, Schandelmaier P, Guy P, Tscherne H, et al. Minimally invasive plate osteosynthesis: Does percutaneous plating disrupt femoral blood supply less than the traditional technique? J Orthop Trauma. 1999;13:401–6. doi: 10.1097/00005131-199908000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Ramasamy PR. Management of gustilo anderson III B open tibial fractures by primary fascio-septo-cutaneous local flap and primary fixation: The ‘fix and shift’ technique. Indian J Orthop. 2017;51:55–68. doi: 10.4103/0019-5413.197532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kamath JB, Shetty MS, Joshua TV, Kumar A, Harshvardhan, Naik DM. Soft tissue coverage in open fractures of tibia. Indian J Orthop. 2012;46:462–9. doi: 10.4103/0019-5413.97265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leininger BE, Rasmussen TE, Smith DL, Jenkins DH, Coppola C. Experience with wound VAC and delayed primary closure of contaminated soft tissue injuries in Iraq. J Trauma. 2006;61:1207–11. doi: 10.1097/01.ta.0000241150.15342.da. [DOI] [PubMed] [Google Scholar]
- 24.Herscovici D, Jr, Sanders RW, Scaduto JM, Infante A, DiPasquale T. Vacuum-assisted wound closure (VAC therapy) for the management of patients with high-energy soft tissue injuries. J Orthop Trauma. 2003;17:683–8. doi: 10.1097/00005131-200311000-00004. [DOI] [PubMed] [Google Scholar]




