Abstract
Background:
For Grade I degenerative lumbar spondylolisthesis (DLS), both decompression alone and decompression with fusion are effective surgical treatments. Which of the two techniques is superior is still under debate. The purpose of this study was to compare clinical outcomes after decompression alone versus decompression with fusion for Grade I DLS.
Materials and Methods:
139 patients who underwent surgery for Grade I DLS at L4-L5 were prospectively enrolled. Decompression alone was used to treat 74 patients, and decompression with fusion was used to treat 65 patients. Six patients in the first group and four patients in the second group were lost during the 2-year followup. Demographic data were recorded. Operation time, perioperative blood loss, total blood transfusion volume, and length of hospital stay were compared between the two groups. Back pain and functional outcomes were evaluated using the visual analog scale (VAS) and the Oswestry Disability Index (ODI), respectively.
Results:
Baseline demographic data were not different between the two groups. Operation time, blood loss, total blood transfusion volume, and length of hospital stay were all significantly greater in the fusion group than in the decompression group. This would be expected because fusion is the more invasive procedure. VAS scores were not different up until 6 months postoperatively. Twelve months after surgery, however, VAS scores were significantly lower in the fusion group. The same results were shown in terms of ODI. Although ODI decreased in both groups over time, the fusion group showed better functional outcomes than did the decompression group.
Conclusions:
Although both decompression alone and decompression with fusion improved functional outcomes for Grade I DLS, fusion surgery resulted in better results compared to decompression alone. Therefore, fusion should be considered as the treatment of choice for Grade I DLS.
Keywords: Comparative, decompression, degenerative lumbar spondylolisthesis, fusion, Grade I
MeSH terms: Lumbar vertebrae, spondylolisthesis, degenerative processes in disease, decompression, spinal fusion
Introduction
Degenerative lumbar spondylolisthesis (DLS) is a condition in which one lumbar vertebra slips forward onto the adjacent vertebra without any defect or dysplasia of the neural arch. This typically develops after the age of 50 years, is disproportionately more common in women than in men, and most commonly affects the L4-L5 level.1 Iguchi et al. found an incidence of 8.7% in an Asian population.2 There have been few studies about the natural course of DLS. A 10-18-year followup study of 145 nonsurgical cases by Matsunaga et al. reported that 49 cases (34%) showed the progression of the slip.3 The slip, however, rarely exceed 30% of the anteroposterior length of the adjacent vertebra.
Patients with DLS usually present with three symptoms, mechanical back pain, radicular pain, and neurogenic claudication. Low back pain and buttock pain may also be experienced, because of instability produced by the degeneration of disc and facet joints. Radicular pain including sensory or motor deficits in the affected nerve root may be generated by direct compression or inflammation of the nerve root.4 Neurogenic claudication results from concomitant stenotic conditions such as hypertrophy of the ligamentum flavum, disc protrusion, and osteophytes.
In symptomatic patients, which treatment is the best remains an open question. Conservative treatment consists of various medications, physiotherapy, and injections.5 Surgical treatment is considered when conservative treatment fails unless the initial symptoms consisted of serious neurological deficits. The mainstay of surgical treatment is decompression for the alleviation of neurological symptoms. The additional fusion surgery is optional and is generally performed for back pain caused by instability. However, there has long been a debate about whether fusion is necessary, especially for low-grade DLS.6,7,8,9,10
This prospective study analyzes the surgical results between decompression alone and decompression with fusion in Grade I DLS and compare their clinical outcomes during a 2 years followup.
Materials and Methods
From January 2009 to December 2012, patients who were scheduled to undergo surgical treatments in our institute for symptomatic Grade I DLS at L4-L5 and had no previous history of surgery at this level were enrolled after providing informed consent. This study was approved by our Institutional Review Board. Preoperative radiographic evaluating including lumbar spine plain radiographs with dynamic radiographs and magnetic resonance imaging was performed routinely. Patients with definite angular instability (>15°) or translational instability (>3 mm) at the index level were excluded before the enrollment. Before surgery, all patients were counselled of the procedure, advantages, and disadvantages of the two surgical methods (decompression and decompression with fusion), and then chose their surgical method by themselves. One hundred thirty-nine patients underwent decompressive laminectomy alone (n = 74) or decompressive laminectomy with fusion (n = 65) for symptomatic Grade 1, DLS at L4L5. We included patients in which conservative treatment failed for more than 3 months. Patients who were lost to followup before 2 years postoperatively were excluded from the data analysis; this consisted of 6 patients in the decompression group and 4 patients in the fusion group. Finally, 61 patients in the fusion group (Group A) and 68 patients in the decompression group (Group B) were analyzed.
When performing a decompressive laminectomy, partial facetectomy, <50% of the inferior articular processes in the transverse dimension, and foraminotomy according to the extent of radiculopathy were performed, and both facet joints were preserved. Circumferential fusion was used, as a combination of instrumentation using pedicle screws, posterolateral fusion with an autologous iliac bone graft, and posterior lumbar interbody fusion using a titanium cage filled with a local bone graft. All surgeries were carried out in the same manner by one experienced spinal surgeon. Several surgical factors, including operation time, blood loss, total blood transfusion volume, and hospital stay were recorded. The incidence rates of intra/postoperative complications, such as nerve root injury, dural tearing, infection, re-operation, and re-admission were compared between the two groups. Postoperative back pain and functional outcomes were quantified by the visual analog scale (VAS) and Oswestry Disability Index (ODI), respectively, at 1, 3, 6, 12, 18, and 24 months postoperatively.
Statistical analysis
Statistical analysis was performed using SPSS 21.0 (SPSS Inc., Chicago, IL, USA). Results are expressed as mean ± standard deviation. The data were analyzed by Student's t-test and P < 0.05 was considered significantly significant.
Results
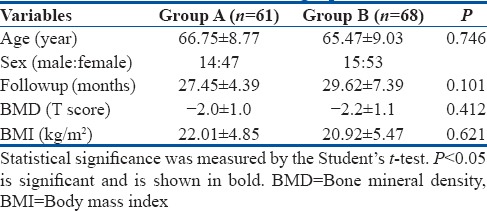
Baseline demographic data of the patients in the two groups were not significantly different [Table 1].
Table 1.
Patient demographics
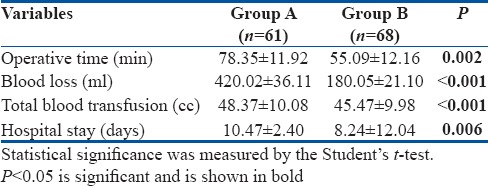
All operative data, including mean operative time, volume of blood loss, total blood transfusion volume, and hospital stay were statistically significantly greater in Group A than in Group B [Table 2]. This result was expected because fusion is a more invasive procedure than laminectomy alone and thus, increased operation time, bleeding, and length of hospital stay are inevitable.
Table 2.
Operative data
Operative complications
In Group A, one patient experienced an unintentional durotomy, which was repaired easily. Two cases of postoperative superficial infection occurred during the hospital stay in each group. Two patients who underwent fusion presented no radiologic evidence of union until 1 year postoperatively.
Postoperative back pain and functional outcomes
VAS scores for back pain were not significantly different between the two groups at postoperative 1, 3, and 6 months. However, at the 12 months followup, group A had lower VAS scores than did Group B, and statistical differences were noted at postoperative 12 and 24 months (but not 18 months) [Table 3 and Figure 1]. ODI showed a similar pattern to VAS, demonstrating better outcomes in Group A from postoperative 12 months onward [Table 4 and Figure 2].
Table 3.
Comparison of average visual analog scale for back pain at the given postoperative time points
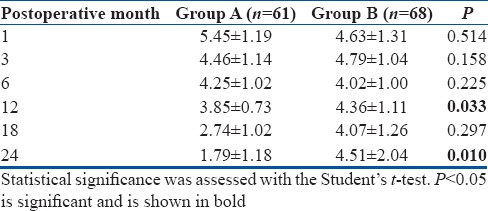
Figure 1.
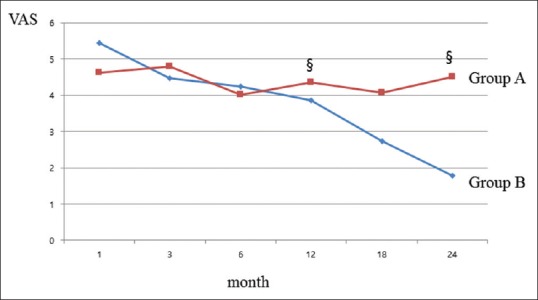
A graph showing that the pain levels during 2 years after surgery are shown by Visual Analog Scale. While no difference is observed until 6 months, significant between-group difference appears after postoperative 12 months. § Means statistical significance (P < 0.05)
Table 4.
Comparison of average Oswestry Disability Index at the given postoperative time points
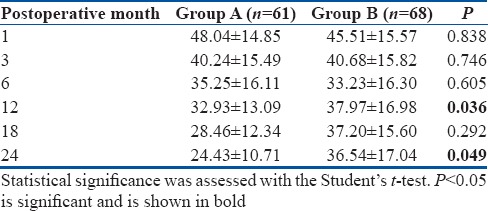
Figure 2.
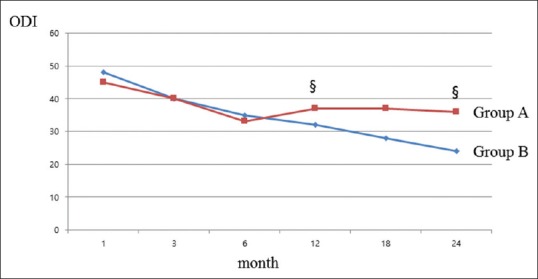
A graph showing that the functional outcomes during 2 years after surgery are shown by Oswestry Disability Index. While no difference is observed until 6 months, significant between-group difference appears after postoperative 12 months. § Means statistical significance (P < 0.05)
Discussion
The etiology of DLS has been investigated but remains unclear. The degenerative cascade proposed by Kirkaldy-Willis et al. in 1978 is believed to be involved in the pathophysiology of spinal degenerative diseases, including DLS.11 Disc degeneration leads to segmental instability in both the coronal and sagittal planes. Then, anterolisthesis, retrolisthesis, or lateral listhesis may occur. Various biomechanical studies on slippage have been done.12,13,14 Studies attempting to identify physiological causes have also been conducted. Ha et al. found higher estrogen receptor expression in the facet joints of patients with DLS.15 An association of DLS with collagen IX tryptophan alleles was also reported.16
The optimal management of DLS remains controversial. If neurologic impairments are absent, conservative treatment is recommended at first. In general, patients with degenerative lumbar diseases including DLS respond partly to conservative treatment. A long term followup study (10-18-year followup) of patients with DLS treated conservatively, conducted by Matsunaga et al.3 showed that 76% of the patients with low back pain did not experience a worsening of their condition over time because of re-stabilization of the vertebrae involved. On the other hand, most of the patients who initially presented with neurological symptoms, including intermittent claudication or vesicorectal disorders, experienced deterioration of their symptoms.
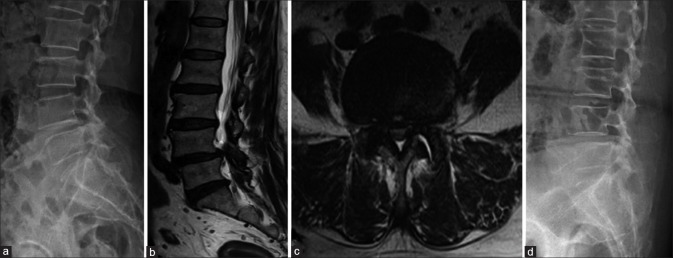
Weinstein et al. demonstrated quite convincingly that patients with DLS treated surgically showed substantially greater improvement in terms of pain and functional outcomes than did patients treated nonsurgically13,17 Several surgical options for DLS have been introduced: decompression alone, decompression with fusion, dynamic stabilization, and distraction using lumbar interspinous spacers.18 There is a consensus that decompression is the mainstay of surgical treatment for DLS, as for other degenerative lumbar diseases, but a debate about the benefits of additional instrumented fusion in cases of low grade (Meyerding I) DLS is still underway. The opinion of advocates for fusion is that spondylolisthesis inherently involves instability. The theoretical basis of this opinion is the pathologic cascade from disc degeneration to spinal stenosis proposed by Kirkaldy-Willis.11,19 Two randomized controlled trials supported that fusion produces superior outcomes to decompression alone.6,7 Other reports also demonstrated that fusion is associated with better outcomes.8,10,20,21 Recent biomechanical studies, on the other hand, have shown that cases of DLS do not always involve instability.22,23 Several studies have reported that decompressive laminectomy alone produced good to excellent results in select subjects, like in elderly patients without dynamic instability.9,24 However, delayed instability and increased reoperation rate have been reported after decompression alone for Grade 1 DLS,25 and one patient who underwent decompression showed postoperative slip progression [Figure 3]. Most spinal surgeons increasingly prefer to perform decompression and fusion together for DLS.26,27
Figure 3.
(a) Lateral standing radiograph of lumbosacral spine of a 64-year-old woman who had undergone an L4-L5 laminectomy surgery. Patient presented with Grade I degenerative spondylolisthesis (L4-L5). (b and c) Magnetic resonance imaging T2W sagittal and axial views showing that diffuse posterior bulging disc, with both facet hypertrophy, resulting in spinal stenosis at L4-L5. (d) Lateral standing radiograph of lumbosacral spine at 6 months post-surgery (Patient's symptoms were aggravated) showing further progression of slip at L4-L5 level
Clinical outcomes of this study support the notion that fusion surgery is superior to decompression alone. VAS for back pain and ODI were similar between groups until 6 months postoperatively, but the fusion group had better functional outcomes than the decompression group beginning 1 year postoperatively. We believe that our results stem from the natural fusion process. Solid fusion of the spine is known to begin 6 months to 1 year postoperatively.28,29 In this study, the patients who underwent fusion showed a dramatic decline in VAS and ODI after 1 year, whereas the others did not. However, it should be noted that operation time, blood loss, transfusion volume, and hospital stay were all significantly greater in Group A than in Group B. With an increase in operation time, there is a potentially greater risk of infection. In addition, fusion may have nonunion as a complication, whereas that is not possible with decompression alone. Although the fusion group did undergo protracted and more complicated surgeries, they did not have greater rates of severe complications.
This study had some limitations. First, this was not a randomized trial. Second, radiological parameters which could have affected the outcomes were not investigated. Third, the followup period was relatively short. Prospective randomized controlled trials with long term followup periods are necessary to make the evidence stronger.
Conclusion
Although both decompression alone and decompression with fusion improved functional outcomes for Grade I DLS, fusion showed better results than decompression alone after 1 year postoperatively. Surgery-related complications, including increased blood loss, longer hospital stay, and nonunion were associated with fusion, but no serious complications occurred in either group. Decompression with fusion may thus be considered as the first option for Grade I DLS.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Jacobsen S, Sonne-Holm S, Rovsing H, Monrad H, Gebuhr P. Degenerative lumbar spondylolisthesis: An epidemiological perspective: The copenhagen osteoarthritis study. Spine (Phila Pa 1976) 2007;32:120–5. doi: 10.1097/01.brs.0000250979.12398.96. [DOI] [PubMed] [Google Scholar]
- 2.Iguchi T, Wakami T, Kurihara A, Kasahara K, Yoshiya S, Nishida K. Lumbar multilevel degenerative spondylolisthesis: Radiological evaluation and factors related to anterolisthesis and retrolisthesis. J Spinal Disord Tech. 2002;15:93–9. doi: 10.1097/00024720-200204000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Matsunaga S, Ijiri K, Hayashi K. Nonsurgically managed patients with degenerative spondylolisthesis: A 10- to 18-year followup study. J Neurosurg. 2000;93(2 Suppl):194–8. doi: 10.3171/spi.2000.93.2.0194. [DOI] [PubMed] [Google Scholar]
- 4.Brisby H. Nerve root injuries in patients with chronic low back pain. Orthop Clin North Am. 2003;34:221–30. doi: 10.1016/s0030-5898(03)00002-6. [DOI] [PubMed] [Google Scholar]
- 5.Kalichman L, Hunter DJ. Diagnosis and conservative management of degenerative lumbar spondylolisthesis. Eur Spine J. 2008;17:327–35. doi: 10.1007/s00586-007-0543-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Herkowitz HN, Kurz LT. Degenerative lumbar spondylolisthesis with spinal stenosis. A prospective study comparing decompression with decompression and intertransverse process arthrodesis. J Bone Joint Surg Am. 1991;73:802–8. [PubMed] [Google Scholar]
- 7.Bridwell KH, Sedgewick TA, O'Brien MF, Lenke LG, Baldus C. The role of fusion and instrumentation in the treatment of degenerative spondylolisthesis with spinal stenosis. J Spinal Disord. 1993;6:461–72. doi: 10.1097/00002517-199306060-00001. [DOI] [PubMed] [Google Scholar]
- 8.Sigmundsson FG, Jönsson B, Strömqvist B. Outcome of decompression with and without fusion in spinal stenosis with degenerative spondylolisthesis in relation to preoperative pain pattern: A register study of 1,624 patients. Spine J. 2015;15:638–46. doi: 10.1016/j.spinee.2014.11.020. [DOI] [PubMed] [Google Scholar]
- 9.Jang JW, Park JH, Hyun SJ, Rhim SC. Clinical outcomes and radiologic changes after microsurgical bilateral decompression by a unilateral approach in patients with lumbar spinal stenosis and grade I degenerative spondylolisthesis with a minimum 3-year followup. Clin Spine Surg. 2016;29:268–71. doi: 10.1097/BSD.0b013e31827566a8. [DOI] [PubMed] [Google Scholar]
- 10.Ghogawala Z, Benzel EC, Amin-Hanjani S, Barker FG nd, Harrington JF, Magge SN, et al. Prospective outcomes evaluation after decompression with or without instrumented fusion for lumbar stenosis and degenerative grade I spondylolisthesis. J Neurosurg Spine. 2004;1:267–72. doi: 10.3171/spi.2004.1.3.0267. [DOI] [PubMed] [Google Scholar]
- 11.Kirkaldy-Willis WH, Wedge JH, Yong-Hing K, Reilly J. Pathology and pathogenesis of lumbar spondylosis and stenosis. Spine (Phila Pa 1976) 1978;3:319–28. doi: 10.1097/00007632-197812000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Berlemann U, Jeszenszky DJ, Bühler DW, Harms J. The role of lumbar lordosis, vertebral end-plate inclination, disc height, and facet orientation in degenerative spondylolisthesis. J Spinal Disord. 1999;12:68–73. [PubMed] [Google Scholar]
- 13.Weinstein JN, Lurie JD, Tosteson TD, Zhao W, Blood EA, Tosteson AN, et al. Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis.four-year results in the Spine patient outcomes research trial (SPORT) randomized and observational cohorts. J Bone Joint Surg Am. 2009;91:1295–304. doi: 10.2106/JBJS.H.00913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim HJ, Chun HJ, Lee HM, Kang KT, Lee CK, Chang BS, et al. The biomechanical influence of the facet joint orientation and the facet tropism in the lumbar spine. Spine J. 2013;13:1301–8. doi: 10.1016/j.spinee.2013.06.025. [DOI] [PubMed] [Google Scholar]
- 15.Ha KY, Chang CH, Kim KW, Kim YS, Na KH, Lee JS. Expression of estrogen receptor of the facet joints in degenerative spondylolisthesis. Spine (Phila Pa 1976) 2005;30:562–6. doi: 10.1097/01.brs.0000154674.16708.af. [DOI] [PubMed] [Google Scholar]
- 16.Matsui Y, Mirza SK, Wu JJ, Carter B, Bellabarba C, Shaffrey CI, et al. The association of lumbar spondylolisthesis with collagen IX tryptophan alleles. J Bone Joint Surg Br. 2004;86:1021–6. doi: 10.1302/0301-620x.86b7.14994. [DOI] [PubMed] [Google Scholar]
- 17.Weinstein JN, Lurie JD, Tosteson TD, Hanscom B, Tosteson AN, Blood EA, et al. Surgical versus nonsurgical treatment for lumbar degenerative spondylolisthesis. N Engl J Med. 2007;356:2257–70. doi: 10.1056/NEJMoa070302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Eismont FJ, Norton RP, Hirsch BP. Surgical management of lumbar degenerative spondylolisthesis. J Am Acad Orthop Surg. 2014;22:203–13. doi: 10.5435/JAAOS-22-04-203. [DOI] [PubMed] [Google Scholar]
- 19.Simmonds AM, Rampersaud YR, Dvorak MF, Dea N, Melnyk AD, Fisher CG. Defining the inherent stability of degenerative spondylolisthesis: A systematic review. J Neurosurg Spine. 2015;23:178–89. doi: 10.3171/2014.11.SPINE1426. [DOI] [PubMed] [Google Scholar]
- 20.Resnick DK, Watters WC, 3rd, Sharan A, Mummaneni PV, Dailey AT, Wang JC, et al. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 9: Lumbar fusion for stenosis with spondylolisthesis. J Neurosurg Spine. 2014;21:54–61. doi: 10.3171/2014.4.SPINE14274. [DOI] [PubMed] [Google Scholar]
- 21.Park JH, Hyun SJ, Roh SW, Rhim SC. A comparison of unilateral laminectomy with bilateral decompression and fusion surgery in the treatment of grade I lumbar degenerative spondylolisthesis. Acta Neurochir (Wien) 2012;154:1205–12. doi: 10.1007/s00701-012-1394-1. [DOI] [PubMed] [Google Scholar]
- 22.Hasegawa K, Kitahara K, Shimoda H, Ishii K, Ono M, Homma T, et al. Lumbar degenerative spondylolisthesis is not always unstable: Clinicobiomechanical evidence. Spine (Phila Pa 1976) 2014;39:2127–35. doi: 10.1097/BRS.0000000000000621. [DOI] [PubMed] [Google Scholar]
- 23.Phan KH, Daubs MD, Kupperman AI, Scott TP, Wang JC. Kinematic analysis of diseased and adjacent segments in degenerative lumbar spondylolisthesis. Spine J. 2015;15:230–7. doi: 10.1016/j.spinee.2014.08.453. [DOI] [PubMed] [Google Scholar]
- 24.Kristof RA, Aliashkevich AF, Schuster M, Meyer B, Urbach H, Schramm J. Degenerative lumbar spondylolisthesis-induced radicular compression: Nonfusion-related decompression in selected patients without hypermobility on flexion extension radiographs. J Neurosurg. 2002;97(3 Suppl):281–6. doi: 10.3171/spi.2002.97.3.0281. [DOI] [PubMed] [Google Scholar]
- 25.Sato S, Yagi M, Machida M, Yasuda A, Konomi T, Miyake A, et al. Reoperation rate and risk factors of elective spinal surgery for degenerative spondylolisthesis: Minimum 5-year followup. Spine J. 2015;15:1536–44. doi: 10.1016/j.spinee.2015.02.009. [DOI] [PubMed] [Google Scholar]
- 26.Schroeder GD, Kepler CK, Kurd MF, Vaccaro AR, Hsu WK, Patel AA, et al. Rationale for the surgical treatment of lumbar degenerative spondylolisthesis. Spine (Phila Pa 1976) 2015;40:E1161–6. doi: 10.1097/BRS.0000000000001116. [DOI] [PubMed] [Google Scholar]
- 27.Kepler CK, Vaccaro AR, Hilibrand AS, Anderson DG, Rihn JA, Albert TJ, et al. National trends in the use of fusion techniques to treat degenerative spondylolisthesis. Spine (Phila Pa 1976) 2014;39:1584–9. doi: 10.1097/BRS.0000000000000486. [DOI] [PubMed] [Google Scholar]
- 28.Boden SD. Overview of the biology of lumbar spine fusion and principles for selecting a bone graft substitute. Spine (Phila Pa 1976) 2002;27(16 Suppl 1):S26–31. doi: 10.1097/00007632-200208151-00007. [DOI] [PubMed] [Google Scholar]
- 29.Ha KY, Lee JS, Kim KW. Bone graft volumetric changes and clinical outcomes after instrumented lumbar or lumbosacral fusion: A prospective cohort study with a five-year followup. Spine (Phila Pa 1976) 2009;34:1663–8. doi: 10.1097/BRS.0b013e3181aacab5. [DOI] [PubMed] [Google Scholar]