Abstract
This study aimed to evaluate the impact of peer counselling on early initiation of breastfeeding (EIBF) and exclusive breastfeeding (EBF) rates for mother–infant pairs living in urban slums, Dhaka, Bangladesh. This randomized controlled trial enrolled 350 mother–infant pairs from selected slums between September 2014 and July 2016. The women assigned to intervention group received peer counselling from locally recruited, trained community female volunteers starting in third trimester of pregnancy until 6 months after delivery; control group received no intervention. EIBF, any liquids given after birth, and EBF were compared between groups. Follow‐up was scheduled at enrolment, following childbirth, and every 2 months up to 6 months after delivery. Multiple logistic regressions were used to assess the effect peer counselling and other associated factors on EIBF and EBF practices. EIBF rate was higher in the intervention group than in the control group (89.1% vs. 77.4%, p = .005). More mothers in intervention group were exclusively breastfeeding at 5 months than mothers in the control group (73% vs. 27%, p < .005). Control mothers were twice as likely to not practice EIBF compared with intervention mothers (adjusted odds risk [aOR]: 2.53, CI [1.29, 4.97], p = .007). Overall, caesarean section was associated with an 8.9‐fold higher risk of not achieving EIBF (aOR: 8.90, CI [4.05, 19.55], p < .001). Intervention mothers were 5.10‐fold more likely to practice EBF compared with control mothers (aOR: 5.10, CI [2.89, 9.01], p < .001) at 5 months. This study demonstrates peer counselling can positively influence both EIBF and EBF among mothers living in urban area.
Keywords: early initiation of breastfeeding, exclusive breastfeeding, intervention, peer counselling, randomized controlled trial
Key messages.
Peer counselling has a positive effect on initiation of breastfeeding within 1 hr of birth and exclusive breastfeeding practices.
Emphasis on encouraging EIBF and discouraging prelacteal feeding should be focused on mothers living who delivered by caesarean section.
1. INTRODUCTION
Worldwide, approximately four million neonatal deaths occur annually within the first 4 weeks of life. The majority of these neonatal deaths are among infants in the developing world, mainly from preventable causes, and approximately half occur in the home. The benefits of breastfeeding for reducing neonatal and infant mortality are well documented (Victora & Barros, 2000). Therefore, promotion of early and exclusive breastfeeding (EBF) is a key intervention. Early initiation of breastfeeding (EIBF) is defined as putting the infant to the breast within 1 hr of birth. EBF is recommended by the World Health Organization (WHO), which states that infants should be breastfed exclusively from birth until 6 months of age, followed by continued breastfeeding alongside gradual introduction of solid foods (World Health Organization and UNICEF, 2003). Several beneficial effects of breastfeeding have been reported, including reductions in the incidence and severity of infectious diseases such as diarrhoea, respiratory tract infections, otitis media, and urinary tract infections, as well as reductions in the incidence of Types 1 and 2 diabetes mellitus, being overweight, obesity, and asthma (Gartner et al., 2005). Conversely, early introduction of breast milk substitutes or semi‐solid foods and delayed introduction of appropriate semi‐solid complementary foods are risk factors associated with the rapid increase in the prevalence of undernutrition among children between 6 and 24 months old (Ramachandran, 2004).
The beneficial effects of EIBF and EBF in the first month of life on mortality have recently been established. A large cohort study conducted in rural Ghana showed that EIBF (within 1 hr) was associated with a 22% reduction in neonatal deaths (Population Attributable Fraction [PAF] adjusted odds ratio [aOR], 41.3%; Edmond et al., 2006). Additionally, the risk of neonatal mortality was higher among infants without EBF practices compared with those with EBF. Improved breastfeeding during the neonatal period helps to reduce mortality and benefits the health, growth, and development of the child in the first year and beyond (Huffman, Zehner, & Victora, 2001). Establishment of good breastfeeding practices in the first days after birth is critical for successful breastfeeding practice and infant health. Initiation of breastfeeding is easiest and most successful when a mother is physically and psychologically prepared for birth and is informed, supported, and confident in her ability to breastfeed and care for the newborn (Development., A.f.E., 2003).
The importance of community support for EIBF was noted in a recent neonatal survival review published in The Lancet covering a range of potential interventions (including EIBF; Darmstadt et al., 2005). Community support via outreach and health education is important for the prevention of neonatal deaths in settings with high mortality and weak health systems to improve home‐care practices and increase the demand for skilled care and care seeking (Darmstadt et al., 2005). Community‐based interventions such as one‐to‐one or group counselling to promote and support infant and young child feeding, along with policy measures and improvements in facility‐based services, are strongly emphasized in the global strategy developed jointly by the WHO and United Nations Children's Fund (UNICEF). A recent meta‐analysis revealed delivery of individual peer counselling to mothers significantly increased the rates of EBF in both the neonatal period (15 studies; odds ratio [OR] = 3.45, 95% CI [2.20, 5.42], p < .0001) and at 6 months of age (nine studies; 1.93, [1.18, 3.15], p < .0001; Edmond et al., 2006). Studies conducted in various developing countries have shown the extent of malnutrition is more severe among children living in slums compared with children living in developed city areas and, sometimes, even compared with children living in rural regions (Fakir & Khan, 2015; Glewwe, Koch, & Nguyen, 2002). An increased risk of inappropriate child feeding practices has been reported among the rapidly growing slum populations in urban areas (Kumar, Nath, & Reddaiah, 1989), as many of these families lack the traditional support of the joint family system. Urban slums are a continually increasing phenomenon in South Asian countries and are underserved by medical facilities (Parvin, Ahsan, & Shaw, 2013). Therefore, we undertook a randomized controlled trial (RCT) to examine whether peer counselling can improve EIBF and EBF practices in an urban slum in Dhaka, Bangladesh.
2. RESEARCH DESIGN AND METHODS
2.1. Trial design
This prospective, RCT to examine the impact of peer counselling—starting in the third trimester of pregnancy and continuing until 6 months after delivery—on infant feeding practices was approved by the local ethics committee and registered at http://clinicaltrial.gov/ as NCT03040375 (last updated: January 31, 2017). Study participants were randomized into two groups: peer counselling (intervention) and no peer counselling (control).
2.2. Setting
The study area was Mirpur, a district of Dhaka with a total population of 5,580,000. The major source of income in Mirpur is wage labour (49.9%), and 53.0% of household heads have no education. The most common improved source of drinking water is a piped water connection inside the user's dwelling, plot or yard (62.8%), and 37.5% of the population of Mirpur have access to sanitary means of waste disposal. Antenatal check‐ups are most commonly performed by Non Government Organization (NGO) facilities (approximately 40%), followed by public sector health facilities (approximately 20%) and private clinics (approximately 10%). Local pharmacies are the most widely known health care facilities in Mirpur (Abul Barkat, Mahiyuddin, Poddar, Hossain, & Ahmed, 2015).
2.3. Study participants
Pregnant women aged between 16 and 49 years old with no more than three living children or a parity of five and who intended to reside in the area for at least 6 months after delivery were identified for the study from a house‐to‐house survey. Women with documented heart disease, insulin‐dependent diabetes mellitus, or pre‐eclampsia in a previous pregnancy were not included. Mother–infant pairs were excluded in cases with congenital anomalies, admission to intensive care, or a birthweight below 1.5 kg (Haider, Ashworth, Kabir, & Huttly, 2000).
2.4. Ethics approval and consent to participate
This study (PR‐14091) was approved by the Research Review Committee and Ethical Review Committee, the two compulsory components of the institutional review board of International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b). Written consent was provided by all study participants. The field research assistants informed the participants about the purpose of the study at the beginning of each interview by reading a consent form. Written consent was also taken from the parent/guardian for anthropometric measurement of the study infants. The respondents were informed of the important point that their participation was voluntary and they were allowed to withdraw themselves at any point of time during the interview/study. The respondents were also informed that the information obtained from this survey would be anonymous and have a broader impact, guide the development of policies and programs related to child nutrition, growth, and development, and would contribute to improve the child health services in Bangladesh and elsewhere.
2.5. Intervention
2.5.1. Selection and training of peer counsellors
Women with personal breastfeeding experience, who had at least 8 years of schooling, who were motivated to help other mothers breastfeed, and who resided in the intervention area were selected to become peer counsellors. Peer counsellors were recruited by the International Centre for Diarrhoeal Disease Research, Bangladesh (icddr,b) and paid a monthly salary. The WHO/UNICEF Breastfeeding Counselling Course, which was validated in a previous study (Haider, Ashworth, Kabir, & Huttly, 2000), was adapted to the local language and culture and used to train peer counsellors. Training was provided over 40 hr (4 hr daily for 10 days). Counselling skills were taught by demonstration and role play, including listening to mothers, learning about their difficulties, assessing the position and attachment of the baby during breastfeeding, building mothers' confidence, giving support, and providing relevant information and practical help when required. One peer counsellor was recruited from each intervention cluster and was responsible for delivering the intervention to 30–35 mothers residing in the same area. Their performance was monitored at least three times over the study period by one breastfeeding supervisor based at the icddr,b field office.
2.5.2. Counselling
The intervention group received at least 10 scheduled visits between the third trimester and 6 months after delivery: three in the last trimester of pregnancy, three in the first month after delivery (one within 48 hr of delivery, one 10–14 days after, and one 24–28 days after), and four visits in the second to sixth months. Counsellors were free to make and receive additional contact with the intervention group if the mothers required additional support. Counselling was given at home, and other family members were included. The duration of each visit was typically 20–40 min. During the two antenatal contacts, the peer counsellors emphasized to the mothers and other members of the family who would support her during delivery the importance of the mother holding the baby within a few minutes of delivery and gave instructions on how to initiate breastfeeding within 1 hr of delivery. They discouraged prelacteal feeds and the use of other fluids and foods after lactation was initiated. The peer counsellors encouraged the mothers to eat more of their usual foods to support lactation and to rest appropriately during the third trimester. These meetings also covered problems with breastfeeding that the mother may encounter and how best to address them.
Fathers and other household members were briefed on the importance of keeping the mother happy and joyful and not subjecting her to violence or harsh treatment. Fortnightly group meetings were organized with the participation of pregnant women, lactating mothers, and their family members. In these meetings, mothers and family members were encouraged to take extra care of the pregnant woman to ensure proper nutrition, attendance of antenatal check‐ups, proper intake of iron tablets, safe delivery, delivery at health facilities, colostrum feeding, and EIBF and continuation of EBF. The peer counsellors emphasized the negative effects of prelacteal feeding, breast milk substitutes, and early introduction of complementary feeding. The peer counsellors provided frequent home visits to support the mothers with EBF.12
2.6. Sample size
The number of mother–infant pairs required was calculated based on achieving a difference of least 20 percentage points in the prevalence of EBF between the intervention and control groups, with a 5% significance level, 80% power, and design effect of 1.5 in a two‐tailed test. The expected prevalence of EBF in the control group was 27% (from unpublished data from another RCT in Mirpur area, personal communication with M. J. Dibley et al.). A sample size of 156 mother–infant pairs was calculated; due to the nature of community‐level interventions, expected migration rate of 12%, and potential loss to follow‐up, the estimated sample size was increased to 175 mother–infant pairs for each group.
2.6.1. Randomization
The trial was conducted in two wards of Mirpur municipality. The average population of a ward is 350,000. There are approximately five wards, each with an average population of 70,000. The interviewer visited door‐to‐door to identify pregnant women in their third trimester at every 2 months interval. Women who fulfilled the inclusion criteria and provided informed consent were randomly allocated to either the intervention or control group.
2.7. Collection of data
Four female field research assistants were recruited and trained over 2 weeks. Each mother was visited by an interviewer four times. Structured questionnaires with precoded closed questions were used during the home interviews. Data on socio‐economic and demographic variables, maternal and pregnancy factors, and previous infant feeding were obtained at enrolment. Details of delivery and early feeding were obtained within 72 hr of birth (60–80 hr). Data on feeding practices were collected every 2 months. To ensure the quality of the data, 10% of the interviews were observed by the field research supervisor. The data were separately recorded, entered, and analysed to ensure consistency with the data collected by the field research assistants. If any inconsistencies were observed, the principal investigator revisited and re‐interviewed the same subjects using the same questionnaire. Unscheduled field visits and spot checks by the principal investigator and research physician were also performed to monitor the quality of data collection.
2.7.1. Data analysis
Data were entered into STATA v13 (StataCorp; College Station, TX, USA). The primary analyses compared the prevalence of EIBF and EBF in children at 0–6 months of age using Pearson's chi square test to calculate 95% confidence intervals for the group difference. Secondary outcome variables included the proportion of mothers who fed colostrum or prelacteals after delivery. For the primary trial outcome, the results of two‐sided 5% tests are reported.
Bivariate and multivariable logistic regressions were used to identify predictive variables, and ORs with 95% confidence intervals and value were used to measure the strength of the associations. Variables with significant associations (aOR, 95% confidence intervals [CI], p value < .05) were included in the final regression model; variables with a p value < .05 were defined as predictor variables.
3. RESULTS
3.1. Baseline comparison
Of 700 pregnant women contacted, 378 were enrolled in the study. Of the 322 (46%) women excluded, the main reasons were that it was too early in the pregnancy, the mother did not live in the cluster, or the mother intended to deliver her child outside of the study area (Figure 1 ). At recruitment, participants did not know if they would be receiving the services of an infant feeding counsellor. The households in the intervention and control groups were similar: Over 80% of mothers in both groups used piped water as their source of drinking water (97.7% and 81.8% in intervention and control groups, respectively; p = .000). Over three fourths of mothers lived in one‐room houses (82.3% and 75.3% in intervention and control groups, respectively; p = 0.332). The majority of households in both groups used water‐sealed sanitary latrines. Most of the mothers in both groups were housewives (Table 1).
Figure 1.
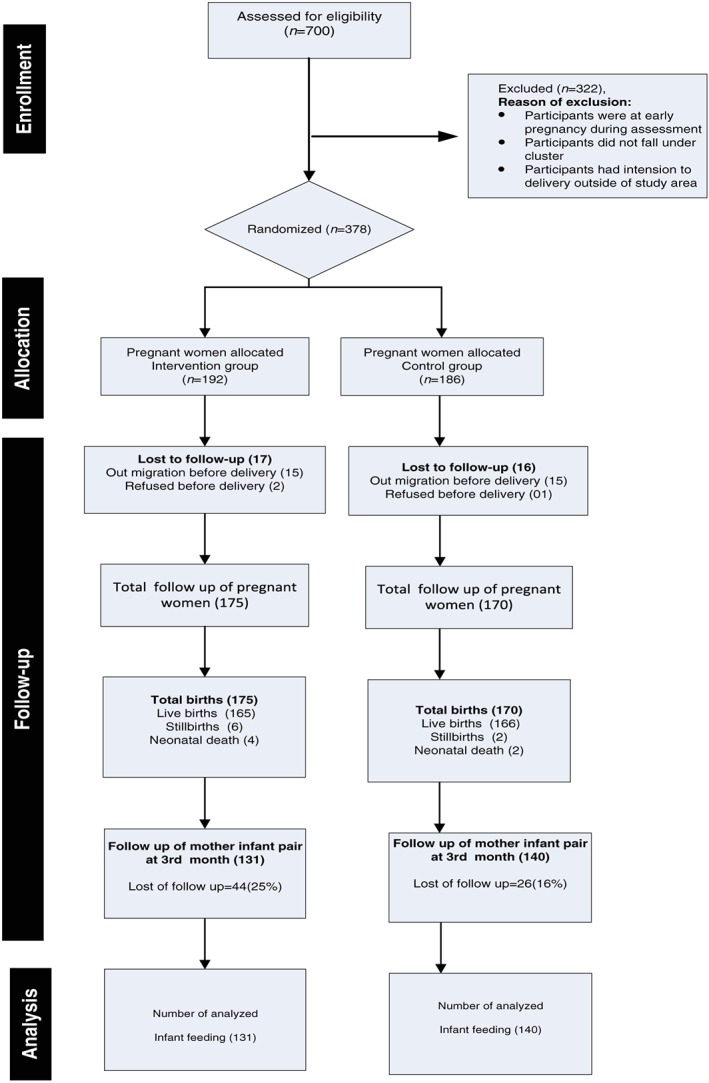
Trial profile
Table 1.
Sociodemographic characteristics of the mothers by study group
| Intervention (175) | Control (170) | p value | |
|---|---|---|---|
| n (%) | n (%) | ||
| Main source of drinking water | |||
| Tube well | 4 (2.3) | 31 (18.2) | |
| Supply (piped) | 171 (97.7) | 139 (81.8) | .000 |
| Number of sleeping rooms in the household | |||
| One | 144 (82.3) | 128 (75.3) | |
| Two | 20 (11.4) | 29 (17.1) | .332 |
| Three | 7 (4.0) | 6 (3.5) | |
| Four or more | 4 (2.3) | 7 (4.1) | |
| Type of toilet | |||
| Sanitary latrine with flush | 3 (1.7) | 3 (1.8) | |
| Sanitary latrine without flush | 163 (93.1) | 160 (94.1) | .806 |
| Pucca/pit (without water seal) | 8 (4.6) | 5 (2.9) | |
| Kutcha/hanging (fixed place) | 1 (0.6) | 2 (1.2) | |
| Religion | |||
| Muslim | 173 (98.9) | 168 (98.8) | |
| Hindu | 2 (1.1) | 2 (1.2) | .977 |
| Employment status | |||
| Unemployed | 165 (94.3) | 161 (94.7) | .864 |
| Employed | 10 (5.7) | 9 (5.3) | |
3.2. Maternal characteristics
Mean maternal age was comparable between groups. A higher proportion of mothers in the control group (58.2%) had not completed secondary education compared with the intervention group (42.9%; p = .029), and 26.9% and 17.1% of control and intervention mothers, respectively, had never attended school. Mean body mass index was similar between groups. Approximately three fourths of the mothers in both groups reported that they had previously discussed child feeding during pregnancy. Concerning antenatal care visits, a higher proportion of mothers in the control group (64.7%) had received four or more visits compared with the intervention group (53.7%, p < .001). Almost 70% of mothers reported they planned to put their babies to the breast within 1 hr of delivery, and only a few (4.6% of intervention mother and 9.5% of the control mother) reported an intention to give prelacteal feeds to their babies (Table 2).
Table 2.
Maternal characteristics and antenatal check‐ups during enrolment
| Indicator | Intervention (n = 175) | Control (n = 170) | p value |
|---|---|---|---|
| n (%) | n (%) | ||
| Mother's age (mean ± SD) | 23.38 ± 4.0 | 23.54 ± 4.3 | .639 |
| Mother's education | |||
| No schooling | 29 (17.1) | 47 (26.9) | |
| Primary incomplete | 20 (11.8) | 28 (16.0) | .029 |
| Secondary incomplete | 99 (58.2) | 75 (42.9) | |
| Secondary complete or higher | 22 (12.9) | 25 (14.3) | |
| Parity | |||
| One | 62 (75.6) | 60 (75.0) | .367 |
| Two | 17 (20.7) | 16 (20.0) | |
| Three | 3 (3.7) | 3 (3.7) | |
| More than three | 0 (0.0) | 1 (1.3) | |
| Mother's anthropometry | |||
| Weight (kg) | 55.41 ± 9.8 | 54.63 ± 9.0 | .778 |
| Height (cm) | 151.19 ± 6.2 | 150.24 ± 5.4 | .951 |
| Body mass index (kg/m2) | 24.21 ± 3.9 | 24.19 ± 3.8 | .389 |
| Antenatal visits | |||
| None | |||
| One to three | 81 (46.3) | 60 (35.3) | .038 |
| Four or more | 94 (53.7) | 110 (64.7) | |
| Discussion about infant feeding during pregnancy | 121 (75.6) | 114 (73.5) | .672 |
| Pregnant mother's intention to breastfed | 173 (98.9) | 166 (97.6) | .585 |
| Intention to initiate breastfeeding | |||
| Within 1 hr | 121 (69.1) | 111 (65.3) | .446 |
| After 1 hr | 54 (30.9) | 59 (34.7) | |
| Intention for prelacteal feeding | 8 (4.6) | 16 (9.5) | .315 |
3.3. Characteristics of delivery
The characteristics of delivery were similar in both groups. One half of mothers in both groups delivered their babies in health facilities (intervention 52.6% vs. control 51.8%; p = .985), whereas approximately one fourth of the mothers in both groups had home deliveries. More than half of the mothers had normal vaginal deliveries, and approximately 31% of both groups had caesarean sections (p = .346). Forty‐eight percent of the mothers in the intervention group and 43.7% in the control group were assisted by qualified doctors during delivery (p = .695), and over 20% of mothers in both groups were assisted by trained birth attendants (p = .681; Table 3).
Table 3.
Characteristics of deliveries by study group
| Indicator | Intervention (n = 175) | Control (n = 170) | p value |
|---|---|---|---|
| n (%) | n (%) | ||
| Reported gestational age (mean ± SD) | 38.76 ± 2.4 | 38.68 ± 2.3 | .379 |
| Birthweight, kg (mean ± SD) | 2.90 ± 0.5 | 2.94 ± 0.5 | .207 |
| Birth length, cm (mean ± SD) | 48.58 ± 2.1 | 48.8 ± 1.7 | .177 |
| Low birthweight | 21 (12.0) | 25 (14.7) | .460 |
| Place of delivery | |||
| Home delivery | 47 (26.9) | 47 (27.6) | |
| Facility delivery | 92 (52.6) | 88 (51.8) | .985 |
| NGO | 36 (20.6) | 35 (20.6) | |
| Type of delivery | |||
| Normal | 101 (58.7) | 9 (53.9) | |
| Caesarian | 54 (31.4) | 52 (31.1) | .346 |
| Assisted vaginal delivery | 17 (9.9) | 25 (15.0) | |
| Delivery assisted by | |||
| Qualified doctor | 83 (48.3) | 73 (43.7) | .695 |
| Nurse/midwife/paramedic | 16 (9.3) | 31 (18.6) | .172 |
| Trained birth attendant | 40 (23.3) | 37 (22.2) | .681 |
| Untrained birth attendant | 33 (19.2) | 26 (15.6) | .147 |
| Delivery complications | |||
| Excessive bleeding | 1 (0.6) | 0 (0.0) | .379 |
| Convulsion | 0 (0.0) | 1 (0.6) | .596 |
| Prolonged labour | 12 (7.0) | 6 (3.6) | .381 |
| Ruptured uterus | 2 (1.2) | 0 (0.0) | .377 |
| High blood pressure | 2 (1.2) | 5 (3.0) | .429 |
| Infant medical check after delivery | |||
| Yes | 91 (55.1) | 107 (65.2) | .062 |
| No | 74 (44.9) | 57 (34.8) | |
3.4. Effects of the intervention on EIBF and EBF
The infant feeding practices of the mothers in both the intervention and control groups are shown in Table 4. A significantly higher proportion of mothers in the intervention group reported EIBF compared with the control group (89.1% vs. 77.4%, p = .005). More than 95% of mothers in both groups gave colostrum to their babies as their first feed. A higher proportion of neonates in the control group (20/164, 12.2%) received prelacteal feeds compared with the neonates in the intervention group (7/165, 4.2%; p = .018). The most common prelacteal feeds given to the babies were water (1/20 in control and 1/7 in intervention area), honey/honey in water (6/20 in control and 2/7 in intervention area), and infant formula (6/20 in control and 3/7 in intervention area). The median duration of EBF for 5 months was 98 days in the intervention group and 56 days in the control group (p = .000). The median duration of any breastfeeding in the first year of life was 275 days in the intervention group and 218 days in the control group (p = .050). Over 80% of mothers in the intervention group reported peer counsellor was the main person who had advised them to initiate breastfeeding immediately after birth, whereas 48% of the control mothers had received such advice from NGO workers (p < .001). Seventy‐six percent of mothers in the intervention group reported the peer counsellor helped them put the child to the breast to initiate breastfeeding, whereas nurses and trained birth attendants helped initiate breastfeeding in the control group (p < .001). The proportion of infants exclusively breastfeeding in the intervention group decreased from 86% at 1 month, 81% at 3 months, and 73% at 5 months, whereas the corresponding rates in the control group were 71%, 49%, and 27%. The differences in the EBF practices between the intervention and control group at 5 months were significantly different (p < .001; Figure 2).
Table 4.
Infant feeding patterns among the study participants
| Indicator | Intervention (n = 165) | Control (n = 164) | p valuea |
|---|---|---|---|
| n (%) | n (%) | ||
| Initiation breastfeeding | |||
| Initiated BF | 147 (89.1) | 127 (77.4) | .005 |
| Received colostrum | |||
| Yes | 163 (98.8) | 159 (96.9) | .248 |
| Prelacteal food given | |||
| Yes | 7 (4.2) | 20 (12.2) | .018 |
| Type of prelacteal food given | Intervention (n = 7) | Control (n = 20) | |
| Honey/sugar water | 2/7 (28.6) | 6/20 (30.0) | .943 |
| Plain water | 1/7 (14.23) | 1/20 (5.0) | .419 |
| Commercial infant formula | 3/7 (42.9) | 6/20 (30.0) | .535 |
| Median duration of EBF (days) | 98 (1–150) | 56 (1–150) | .000b |
| Median duration of any breastfeeding (days) | 275 (1–365) | 218 (1–365) | .050b |
| Main person advising about breastfeeding | |||
| Mother of the child | 5 (3.0) | 16 (9.8) | |
| Mother | 4 (2.4) | 12 (7.4) | |
| Mother in law | 0 (0.0) | 5 (3.1) | |
| Other relatives | 1 (0.6) | 12 (7.4) | <.001 |
| Neighbour | 2 (1.2) | 1 (0.6) | |
| Doctor | 2 (1.2) | 15 (9.2) | |
| Nurse | 8 (4.8) | 11 (6.7) | |
| Trained traditional birth attendant | 3 (1.8) | 7 (4.3) | |
| Friends | 0 (0.0) | 1 (0.6) | |
| NGO worker | 4 (2.4) | 78 (47.9) | |
| Peer counsellor | 137 (83.0) | 4 (2.4) | |
| Main person who helped practically with breastfeeding practice | |||
| Mother of the child | 6 (3.6) | 26 (15.8) | |
| Mother | 10 (6.1) | 16 (9.8) | |
| Husband | 0 (0.0) | 1 (0.6) | |
| Mother in law | 1 (0.6) | 6 (3.7) | |
| Other relatives | 7 (4.2) | 14 (8.5) | <.001 |
| Neighbour | 0 (0.0) | 1 (0.6) | |
| Doctor | 2 (1.2) | 2 (1.2) | |
| Nurse | 10 (6.06) | 53 (32.3) | |
| Trained traditional birth attendant | 1 (0.6) | 27 (16.5) | |
| Untrained birth attendant | 2 (1.2) | 10 (6.1) | |
| NGO worker | 0 (0.0) | 4 (2.4) | |
| Peer counsellor | 126 (76.4) | 4 (2.4) | |
Note. BF = breastfeeding; EBF = exclusive breastfeeding.
p values calculated using Pearson chi square (χ 2) test or if indicated.
Mann–Whitney test.
Figure 2.
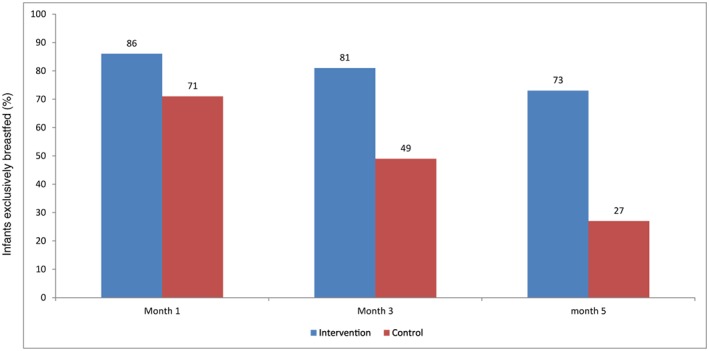
Proportions of infants exclusively breastfed during the first 5 months in the intervention and control areas
3.5. Association of EIBF and EBF with background characteristics
In the adjusted multivariable model, the most significant determinants of a lack of EIBF across the two groups were the mother's education, caesarean section, and low birthweight. The mothers in the control group had a 2.53‐fold higher OR of not initiating breastfeeding immediately compared with the intervention mothers (aOR = 2.53, CI [1.29, 4.97], p = .007). Not completing primary education was associated with an increased risk of late initiation of breastfeeding (aOR = 3.74, CI [1.06, 13.14], p = .040) compared with mothers with no education. The odds of not receiving early breastfeeding were approximately nine times higher for infants born by caesarean section (aOR: 8.90, CI [4.05, 19.55], p < .001) compared with infants who were delivered vaginally. The odds of women practicing EBF for up to 5 months were fivefold higher in the intervention group than the control group (aOR: 5.10, CI [2.89, 9.01], p < .001). No other background variables were associated with EBF practices (Tables 5 and 6).
Table 5.
Factors associated with early initiation of breastfeeding in multivariate analysis
| Variable | Crude OR (95% CI) | p value | aOR (95% CI) | p value |
|---|---|---|---|---|
| Group | ||||
| Intervention | 1 | 1 | ||
| Control | 2.53 (1.25, 5.14) | .010 | 2.53 (1.29, 4.97) | .007 |
| Mother's age (years) | ||||
| Less than 20 | 1 | |||
| 20–29 | 0.66 (0.38, 1.14) | .119 | ||
| 30–39 | 1.61 (0.55, 4.73) | .336 | ||
| Mother's education | ||||
| No education | 1 | 1 | ||
| Primary incomplete | 2.86 (0.75, 10.94) | .125 | 3.74 (1.06, 13.14) | .040 |
| Secondary incomplete | 1.74 (0.57, 5.32) | .329 | 2.02 (0.70, 5.87) | .195 |
| Secondary complete and above | 1.34 (0.36, 4.90) | .662 | 1.66 (0.47, 5.81) | .429 |
| Gestational age | ||||
| Term | 1 | 1 | ||
| Pre‐term | 3.06 (1.39, 6.72) | .005 | 2.47 (1.18, 5.18) | .017 |
| Type of delivery | ||||
| Normal | 1 | 1 | ||
| Caesarian | 8.48 (2.28, 31.47) | .001 | 8.90 (4.05, 19.55) | .000 |
| Assisted vaginal delivery | 2.37 (0.65, 8.57) | .189 | 2.85 (1.10, 8.16) | .051 |
| Place of delivery | ||||
| Home | 1 | |||
| Facility based | 0.59 (0.12, 2.89) | .004 | ||
| NGO based | 0.44 (0.08, 2.32) | .335 | ||
| Birthweight | ||||
| Normal | 1 | |||
| Low birthweight | 2.03 (0.68, 6.26) | .218 | ||
| Antenatal check‐up | ||||
| One to three | 1 | |||
| More than three | 1.38 (0.68, 2.80) | .369 | ||
| Main person who helped with delivery | ||||
| Qualified doctor | 1 | |||
| Nurse/midwife/paramedic | 1.26 (0.31, 5.08) | .748 | ||
| Trained traditional birth attendant | 0.75 (0.14, 3.85) | .727 | ||
| Untrained traditional birth attendant | 0.37 (0.06, 2.54) | .321 | ||
Note. aOR = adjusted odds ratio; OR = odds ratio.
Table 6.
Factors associated with exclusive of breastfeeding in multivariate analysis
| Variable | Crude OR (95% CI) | p value | aOR (95% CI) | p value |
|---|---|---|---|---|
| Group | ||||
| Control | 1 | Ref | ||
| Intervention | 5.11 (2.89, 9.01) | .000 | 5.10 (2.89, 9.01) | .000 |
| Mother's age (years) | ||||
| Less than 20 | 1 | |||
| 20–29 | 1.02 (0.47, 2.19) | .402 | ||
| 30–39 | 0.99 (0.29, 3.41) | .666 | ||
| Mother's education | ||||
| No education | 1 | |||
| Primary incomplete | 1.42 (0.55, 3.71) | .386 | ||
| Secondary incomplete | 1.08 (0.58, 2.02) | .801 | ||
| Secondary complete and above | 1.00 (0.44, 2.27) | .99 | ||
| Gestational age | ||||
| Term | 1 | |||
| Pre‐term | 1.44 (0.80, 2.60) | .221 | ||
| Type of delivery | ||||
| Normal | 1 | |||
| Caesarian | 1.47 (0.85, 2.55) | .402 | ||
| Assisted vaginal delivery | 0.50 (0.22, 1.14) | .666 | ||
| Place of delivery | ||||
| Home | 1 | |||
| Facility based | 1.50 (0.85, 2.64) | .165 | ||
| NGO based | 0.58 (0.27, 1.23) | .158 | ||
| Birthweight | ||||
| Normal | 1 | |||
| Low birthweight | 0.81 (0.40, 1.63) | .559 | ||
| Antenatal check‐ups | ||||
| One to three | 1 | |||
| More than three | 0.85 (0.51, 1.39) | .510 | ||
| Main person who helped with delivery | ||||
| Qualified doctor | 1 | |||
| Nurse/midwife/paramedic | 0.30 (0.12, 0.75) | .010 | ||
| Trained traditional birth attendant | 0.47 (0.25, 0.88) | .018 | ||
| Untrained traditional birth attendant | 1.00 (0.51, 1.98) | .995 | ||
Note. aOR = adjusted odds ratio; OR = odds ratio.
4. DISCUSSION
This study provides evidence that peer counselling positively influences EIBF and EBF practices among mothers living in an urban slum. The low prevalence of EBF in the control group and high prevalence of EBF in the intervention group confirm the need for community‐based peer support to promote breastfeeding in urban slum areas. Peer counselling was found to be an effective strategy and led to much higher rates of EBF in the first 5 months compared with the control group.
In our study, we found that the rate of EIBF in the intervention group was 89.1%, which is higher than the values reported for studies in Pakistan and India, but lower than that in Nepal (Khanal, Scott, Lee, Karkee, & Binns, 2015; Patel et al., 2015; Zafar, Fatmi, & Shafi, 2014). There are multiple factors, including maternal education, multiple births, type of delivery, not putting the baby to the breast after birth, and low birthweight, that are associated with a lack of EIBF (Acharya & Khanal, 2015; Gul, Khalil, Yousafzai, & Shoukat, 2014; Khadduri et al., 2008; Sharma & Byrne, 2016). Our study has also shown that maternal education, low birthweight, and caesarean delivery were associated with late initiation of breastfeeding. Due to cultural and traditional norms, family members frequently introduce prelacteals, and health care staffs sometimes advise prelacteals, which conflicts with the advice provided by the peer counsellors. Despite this, the peer counselling significantly reduced prelacteal and postlacteal feeds in the intervention group, in agreement with the results of previous peer counselling studies conducted in Bangladesh and Mexico (Chapman, Damio, Young, & Pérez‐Escamilla, 2004; Haider, Ashworth, Kabir, & Huttly, 2000).
The rate of EIBF in our control group was surprisingly higher than the national average. The last four consecutive Bangladesh Demographic Health Surveys have revealed a significant positive increase in the rate of EIBF over the last decade (26% in 2004 to 43% in 2007). However, the current national rate, 51%, is insufficient to attain the estimated mortality benefits provided by EIBF (Bangladesh Demographic and Health Survey [BDHS], 2004, 2007, 2014). The high prevalence of EIBF in this study may reflect the fact that these disadvantaged mothers only have one option for infant feeding. Similar findings have been reported in Sri Lanka, Tanzania (Adhikari, Khanal, Karkee, & Gavidia, 2014; Exavery, Kanté, Hingora, & Phillips, 2015; Senarath, Dibley, & Agho, 2006), and Nepal.
Approximately one third of mothers in both groups delivered their babies via caesarean section, and these mothers were nine times less likely to initiate breastfeeding immediately after birth. This could be because the newborn baby is not usually put to the mother's breast until the mother has recovered and been transferred from the post‐operative room. An association between caesarean delivery and late initiation of breastfeeding has been demonstrated in several studies (Rowe‐Murray & Fisher, 2002; Senerath et al., 2000). Caesarean delivery has consistently been identified as a major barrier to initiation of breastfeeding immediately after birth (Cakmak & Kuguoglu, 2007; Pandey et al., 2010; Patel et al., 2010). This finding highlights a target where a major intervention could be provided to improve the rate of EIBF (Joshi et al., 2014). This is particularly important, as the percentage of deliveries by caesarean section in Bangladesh has increased over time, from 4% in 2004 to 9% in 2007, 17% in 2011, and 23% in 2014. Mothers who deliver by caesarean section are usually separated from their babies for more than 1 hr after birth, yet this is the best time for successful initiation of EIBF. Even if the babies are not separated from their mothers after surgery, many mothers still decline breastfeeding as they believe the medication they received during the surgical procedure may exert side effects in their babies (Qiu, Zhao, Binns, Lee, & Xie, 2009a); this belief may discourage EIBF (Duong, Binns, & Lee, 2004; Qiu, Zhao, Binns, Lee, & Xie, 2009b).
More than 60% of deliveries still occur at home in Bangladesh (Sarker et al., 2016), so our finding that approximately one third of women delivered their babies at home in both groups implies the likelihood of delivering in a health facility is higher for urban mothers. Our results indicate that mothers who had facility‐based deliveries were less likely to initiate breastfeeding than mothers who delivered at home. This is in contrast to studies in Nepal and Nigeria, which found mothers who deliver in a health facility were more likely to initiate early breastfeeding compared with mothers who delivered at home (Adhikari, Khanal, Karkee, & Gavidia, 2014b; Berde & Yalcin, 2016). The significantly lower proportion of neonates who were given any type of prelacteal feed in the intervention group implies that peer counsellors had a significant influence on reducing prelacteal feeds. Similar findings were reported in earlier studies from India (Kushwaha et al., 2014), Burkina Faso, Uganda, and South Africa (Tylleskar et al., 2011).
Regarding the rate of EBF in developing countries, global data suggest the prevalence of EBF among infants younger than 6 months increased from 33% in 1995 to 39% in 2010 (Haroon et al., 2013). The rate of EBF increased in most in developing regions, with the highest improvements observed in West and Central Africa where the prevalence of EBF more than doubled from 12% in 1995 to 28% in 2010 (Haroon et al., 2013). More modest improvements were observed in South Asia (from 40% in 1995 to 45% in 2010; Cai, Wardlaw, & Brown, 2012). In Bangladesh, the increase in the prevalence of EBF among infants under 6 months was unsatisfactory until the year 2007 (BDHS, 2007). However, the rate of EBF had significantly improved by the last BDHS (2014); the EBF rate is currently 55% (BDHS, 2014). In this study, the prevalence of EBF at 5 months was 27% in the control group and 73% in the intervention group who received peer counselling (p < .001).
Two previous RCTs have assessed the ability of community‐based peer counselling to promote EBF, but neither followed up the mothers for as long as 5 months. Haider et al. (2010) were the first to explore the impact of peer counselling in Bangladesh and found that 70% of the mothers in the intervention group practiced EBF but only 6% in the control group practiced EBF at 5 months. A similar approach was used in this trial, and we found 73% of mothers in the intervention group and 27% in the control group practiced EBF at 5 months. The overall nationwide improvements in EBF practices, due to social campaigns, media coverage, programs run by national and international NGOs, and so forth, may possibly explain the higher rate of EBF in the control group in this study compared with that of Haider et al. (2010). The participants in this study lived in urban slum communities, and the EBF rate of the control group was similar to the value of 16% reported in the recent study (Akhtar et al., 2012).
Thus, this study demonstrates one‐to‐one peer counselling may be an effective strategy to improve EIBF and EBF practices in urban slum communities, where a high rate of malnutrition exists and inappropriate breastfeeding practices are prominent (Shakya et al., 2017). Our peer counsellors delivered a regular service on a part‐time (half‐day) basis and received a monthly honorarium of approximately US $43. The counsellors also made additional visits if necessary and conducted fortnightly group sessions with the mothers and other family members. In a lower resource setting, fewer visits combined with group counselling may be effective to increase the rates of EIBF and EBF (Haider et al., 2000). Governments and NGOs could even consider training community health volunteers to provide group or peer support on infant and young child feeding practices to the mothers and caregivers.
One strength of this study is its randomized design, which minimized selection bias (Sibbald & Roland, 1998). Moreover, the power of randomization provides excellent internal validity, which is one of the greatest strengths of RCTs. Randomization ensures that the level of exposure to the treatment of interest is the only differentiating factor between the two arms. Strength of this study is that the intervention combined individual counselling with fortnightly group sessions. Including pregnant and lactating mothers and family members in counselling and practical demonstrations has also been proven to be effective (Sibbald & Roland, 1998).
One limitation of this randomized study is that it was not double blinded, and the interviewer knew which clusters were included in the intervention group. To prevent interviewer bias, the questions related to peer counsellor contact were asked to the mothers at the end of each follow‐up interview session. Additionally, the generalizability (external validity) of this study may be limited (Meyer, 2010), as there was a high dropout rate during the trial (25% in the intervention group and 16% in the control group). In most urban slums in Bangladesh, including Mirpur, people often move from one slum to another in search of better employment, cheaper accommodation, or in response to political unrest. Moreover, many working mothers who formerly resided in urban slums often quit their jobs to take care of their children and migrate back to rural areas. This phenomenon could explain the high dropout rate and loss to follow‐up in this study.
In summary, we found that peer counselling was an effective method of promoting EIBF as well as EBF among urban women living in a slum in Dhaka, Bangladesh. This result is very promising, as this slum community has exceedingly low rates of EBF and a strong preference for formula, even if mothers choose to breastfeed their infants (Chapman et al., 2004; Perez‐Escamilla et al., 1998). We have shown the potential of peer counselling to promote EIBF and EBF among women residing in urban slum areas.
5. CONCLUSION
Peer counselling positively influenced the initiation of breastfeeding within 1 hr of birth and the duration of EBF and reduced prelacteal feeding among urban women living in a slum in Dhaka, Bangladesh. This study highlights the need to target the promotion of optimal breastfeeding practices to expectant mothers and mothers who deliver through caesarean section. Furthermore, peer counselling support to support EBF should be continued for at least first months of delivery.
AVAILABILITY OF DATA AND MATERIALS
The dataset has been uploaded as Additional File 1 (EBIF.dta).
CONFLICTS OF INTEREST
The authors declare that they have no conflicts of interest.
CONTRIBUTIONS
GA was responsible for the overall design and implementation of the study, for securing funding, for training and project management, and for data management and analysis. MJD and IK helped design the study and provided technical assistance throughout all stages of the project. BN helped train the interviewers. MK, NP, and Md. AH helped with daily project management, data management, and analysis. All authors are responsible for the final content of this manuscript and have read and approved the final version.
ACKNOWLEDGMENTS
This study was conducted at the icddr,b Centre for Health and Population Research, Bangladesh, with the support of the Stars in Global Health Grand Challenges Canada (GCC). The icddr,b thanks the GCC for its commitment to the centre's research efforts. We also thank the peer counsellors and field staff for their encouragement, support, and dedicated work.
Ara G, Khanam M, Papri N, et al. Peer counselling improves breastfeeding practices: A cluster randomized controlled trial in urban Bangladesh. Matern Child Nutr. 2018;14:e12605 10.1111/mcn.12605
[The copyright line for this article was changed on 24 April 2018 after original online publication]
REFERENCES
- Abul Barkat, M. M. , Mahiyuddin, G. , Poddar, A. , Hossain, K. T. , & Ahmed, F. M. (2015). Report on survey for project areas in urban slums of Mirpur and Karail, Dhaka. United Nations Children Fund (UNICEF) Dhaka, Bangladesh.
- Acharya, P. , & Khanal, V. (2015). The effect of mother's educational status on early initiation of breastfeeding: Further analysis of three consecutive Nepal Demographic and Health Surveys. BMC Public Health, 15, 1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adhikari, M. , Khanal, V. , Karkee, R. , & Gavidia, T. (2014). Factors associated with early initiation of breastfeeding among Nepalese mothers: Further analysis of Nepal Demographic and Health Survey, 2011. International Breastfeeding Journal, 9(1), 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akhtar, K. , Haque, M. E. , Islam, M. Z. , Yusuf, M. A. , Sharif, A. R. , & Ahsan, A. I. (2012). Feeding pattern and nutritional status of under two years slum children. Journal of Shaheed Suhrawardy Medical College, 4(1), 3–6. [Google Scholar]
- Bangladesh Demographic and Health Survey (2007). Dhaka, Bangladesh and Calverton, Maryland, USA: : National Institute of Population Research and Training, Mitra and Associates, and Macro International. [Google Scholar]
- Bangladesh Demographic and Health Survey (2011). Dhaka, Bangladesh and Calverton, Maryland, USA: National Institute of Population Research and Training, Mitra and Associates, and Macro International. [Google Scholar]
- Bangladesh Demographic and Health Survey (2014). Dhaka, Bangladesh and Calverton, Maryland, USA: : National Institute of Population Research and Training, Mitra and Associates, and Macro International. [Google Scholar]
- BDHS (2007). National Institute of Population Research and Training Ministry of Health and Family Welfare Dhaka, Bangladesh. Dhaka, Bangladesh: National Institute of Population Research and Training Ministry of Health and Family Welfare. [Google Scholar]
- BDHS, Bangladesh Demographic and Health Survey (2014). National Institute of Population Research and Training Ministry of Health and Family Welfare; Dhaka, Bangladesh. [Google Scholar]
- BDHS, Bangladesh Demographic and Health Survey (2004). National Institute of Population Research and Training Ministry of Health and Family Welfare Dhaka. Bangladesh: Dhaka, Bangladesh. [Google Scholar]
- Berde, A. S. , & Yalcin, S. S. (2016). Determinants of early initiation of breastfeeding in Nigeria: A population‐based study using the 2013 demograhic and health survey data. BMC Pregnancy and Childbirth, 16(1), 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai, X. , Wardlaw, T. , & Brown, D. W. (2012). Global trends in exclusive breastfeeding. International Breastfeeding Journal, 7(1), 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cakmak, H. , & Kuguoglu, S. (2007). Comparison of the breastfeeding patterns of mothers who delivered their babies per vagina and via cesarean section: An observational study using the LATCH breastfeeding charting system. International Journal of Nursing Studies, 44(7), 1128–1137. [DOI] [PubMed] [Google Scholar]
- Chapman, D. J. , Damio, G. , Young, S. , & Pérez‐Escamilla, R. (2004). Effectiveness of breastfeeding peer counseling in a low‐income, predominantly Latina population: A randomized controlled trial. Archives of Pediatrics & Adolescent Medicine, 158(9), 897–902. [DOI] [PubMed] [Google Scholar]
- Darmstadt, G. L. , Bhutta, Z. A. , Cousens, S. , Adam, T. , Walker, N. , & de Bernis, L. (2005). Evidence‐based, cost‐effective interventions: How many newborn babies can we save? The Lancet, 365(9463), 977–988. [DOI] [PubMed] [Google Scholar]
- Development., A.f.E , & LINKAGES Project (2003). Facts for feeding: Birth, initiation of breastfeeding, and the first seven days after birth. ( p. 8). Washington, DC: LINKAGES Project, Academy for Educational Development. [Google Scholar]
- Duong, D. V. , Binns, C. W. , & Lee, A. H. (2004). Breast‐feeding initiation and exclusive breast‐feeding in rural Vietnam. Public Health Nutrition, 7(6), 795–799. [DOI] [PubMed] [Google Scholar]
- Edmond, K. M. , Zandoh, C. , Quigley, M. A. , Amenga‐Etego, S. , Owusu‐Agyei, S. , & Kirkwood, B. R. (2006). Delayed breastfeeding initiation increases risk of neonatal mortality. Pediatrics, 117(3), e380–e386. [DOI] [PubMed] [Google Scholar]
- Exavery, A. , Kanté, A. M. , Hingora, A. , & Phillips, J. F. (2015). Determinants of early initiation of breastfeeding in rural Tanzania. International Breastfeeding Journal, 10(1), 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fakir, A. M. S. , & Khan, M. W. R. (2015). Determinants of malnutrition among urban slum children in Bangladesh. Health Economics Review, 5, 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowe‐Murray, H. J. , & Fisher, J. R. W. (2002). Baby friendly hospital practices: Cesarean section is a persistent barrier to early initiation of breastfeeding. Birth, 29, 124–131. [DOI] [PubMed] [Google Scholar]
- Gartner, L. M. , Morton, J. , Lawrence, R. A. , Naylor, A. J. , O'Hare, D. , Schanler, R. J. , … American Academy of Pediatrics Section on Breastfeeding (2005). Breastfeeding and the use of human milk. Pediatrics, 115(2), 496–506. [DOI] [PubMed] [Google Scholar]
- Glewwe, P. , Koch, S. , & Nguyen, B. L. (2002). Child nutrition, economic growth, and the provision of health care services in Vietnam in the 1990s. (p. 2776). Washington, DC: World Bank, Development Research Group, Macroeconomics and Growth. [Google Scholar]
- Gul, S. , Khalil, R. , Yousafzai, M. T. , & Shoukat, F. (2014). Newborn care knowledge and practices among mothers attending pediatric outpatient clinic of a hospital in Karachi, Pakistan. International Journal of Health Sciences, 8(2), 167–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haider, R. , Ashworth, A. , Kabir, I. , & Huttly, S. R. A. (2000). Effect of community‐based peer counsellors on exclusive breastfeeding practices in Dhaka, Bangladesh: A randomised controlled trial. The Lancet, 356(9242), 1643–1647. [DOI] [PubMed] [Google Scholar]
- Haroon, S. , Haroon, S. , Das, J. K. , Salam, R. A. , Imdad, A. , & Bhutta, Z. A. (2013). Breastfeeding promotion interventions and breastfeeding practices: A systematic review. BMC Public Health, 13(3), 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huffman, S. L. , Zehner, E. R. , & Victora, C. (2001). Can improvements in breast‐feeding practices reduce neonatal mortality in developing countries? Midwifery, 17(2), 80–92. [DOI] [PubMed] [Google Scholar]
- Joshi, P. C. , Mirak, A. , Sumon, D. , Shahnawaz, A. , Abu, F. , & Tahmeed, A. (2014). Prevalence of exclusive breastfeeding and associated factors among mothers in rural Bangladesh: A cross‐sectional study. International Breastfeeding Journal, 9, 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khadduri, R. , Marsh, D. R. , Rasmussen, B. , Bari, A. , Nazir, R. , & Darmstadt, G. L. (2008). Household knowledge and practices of newborn and maternal health in Haripur district, Pakistan. Journal of Perinatology, 28(3), 182–187. [DOI] [PubMed] [Google Scholar]
- Khanal, V. , Scott, J. , Lee, A. , Karkee, R. , & Binns, C. (2015). Factors associated with early initiation of breastfeeding in Western Nepal. International Journal of Environmental Research and Public Health, 12(8), 9562–9574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar, S. , Nath, L. M. , & Reddaiah, V. P. (1989). Factors influencing prevalence of breastfeeding in a resettlement colony of New Delhi. The Indian Journal of Pediatrics, 56(3), 385–391. [DOI] [PubMed] [Google Scholar]
- Kushwaha, K. , Sankar, J. , Sankar, M. J. , Gupta, A. , Dadhich, J. P. , Gupta, Y. P. , … Sharma, B. (2014). Effect of peer counselling by mother support groups on infant and young child. PLoS One, 9, e109181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer, R. M. (2010). Generalizing the results of cancer clinical trials. Journal of Clinical Oncology, 28(2), 187–189. [DOI] [PubMed] [Google Scholar]
- Pandey, S. , Tiwari, K. , Senarath, U. , Agho, K. E. , Dibley, M. J. , & for the South Asia Infant Feeding Research Network (SAIFRN)* (2010). Determinants of infant and young child feeding practices in Nepal: Secondary data analysis of Demographic and Health Survey 2006. Food and Nutrition Bulletin, 31(2), 334–351. [DOI] [PubMed] [Google Scholar]
- Parvin, G. A. , Ahsan, S. M. R. , & Shaw, R. (2013). Urban risk reduction approaches in Bangladesh In Shaw R., Mallick F., & Islam A. (Eds.), Disaster risk reduction approaches in Bangladesh (pp. 235–257). Tokyo: Springer Japan. [Google Scholar]
- Patel, A. , Badhoniya, N. , Khadse, S. , Senarath, U. , Agho, K. E. , Dibley, M. J. , & for the South Asia Infant Feeding Research Network (SAIFRN)* (2010). Infant and young child feeding indicators and determinants of poor feeding practices in India: Secondary data analysis of National Family Health Survey 2005‐06. Food and Nutrition Bulletin, 31(2), 314–333. [DOI] [PubMed] [Google Scholar]
- Patel, A. , Bucher, S. , Pusdekar, Y. , Esamai, F. , Krebs, N. F. , Goudar, S. S. , … Hibberd, P. L. (2015). Rates and determinants of early initiation of breastfeeding and exclusive breast feeding at 42 days postnatal in six low and middle‐income countries: A prospective cohort study. Reproductive Health, 12(Suppl 2), S10–S10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez‐Escamilla, R. , Himmelgreen, D. , Segura‐Millán, S. , González, A. , Ferris, A. M. , Damio, G. , & Bermúdez‐Vega, A. (1998). Prenatal and perinatal factors associated with breast‐feeding initiation among inner‐city Puerto Rican women. Journal of the American Dietetic Association, 98(6), 657–663. [DOI] [PubMed] [Google Scholar]
- Qiu, L. , Zhao, Y. , Binns, C. W. , Lee, A. H. , & Xie, X. (2009). Initiation of breastfeeding and prevalence of exclusive breastfeeding at hospital discharge in urban, suburban and rural areas of Zhejiang China. International Breastfeeding Journal, 4(1), 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramachandran, P. (2004). Breastfeeding practices in South Asia. The Indian Journal of Medical Research, 119, 13–15. [PubMed] [Google Scholar]
- Sarker, B. K. , Rahman, M. , Rahman, T. , Hossain, J. , Reichenbach, L. , & Mitra, D. K. (2016). Reasons for preference of home delivery with traditional birth attendants (TBAs) in rural Bangladesh: A qualitative exploration. PLoS One, 11(1), e0146161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senarath, U. , Dibley, M. J. , & Agho, K. E. (2006). Breastfeeding practices and associated factors among children under 24 months of age in Timor‐Leste. European Journal of Clinical Nutrition, 61(3), 387–397. [DOI] [PubMed] [Google Scholar]
- Senerath, U. , Dibley, M. , Godakandage, S. , Jayawickrama, H. , Wickramasinghe, A. , & Agho, K. (2000). Determinants of infant and young child feeding practices in Srilanka: Secondary data analysis of Demographic and Health Survey. Food and Nutrition Bulletin, 2010(31), 354–367. [DOI] [PubMed] [Google Scholar]
- Shakya, P. , Kunieda, M. K. , Koyama, M. , Rai, S. S. , Miyaguchi, M. , Dhakal, S. , … Jimba, M. (2017). Effectiveness of community‐based peer support for mothers to improve their breastfeeding practices: A systematic review and meta‐analysis. PLoS One, 12(5), e0177434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharma, I. K. , & Byrne, A. (2016). Early initiation of breastfeeding: a systematic literature review of factors and barriers in South Asia. International Breastfeeding Journal, 11, 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibbald, B. , & Roland, M. (1998). Understanding controlled trials. Why are randomised controlled trials important? BMJ, 316(7126), 201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tylleskar, T. , Jackson, D. , Meda, N. , Engebretsen, I. M. , Chopra, M. , Diallo, A. H. , … PROMISE‐EBF Study Group (2011). Exclusive breastfeeding promotion by peer counsellors in sub‐Saharan Africa (PROMISE‐EBF): A cluster‐randomised trial. Lancet, 378(9789), 420–427. [DOI] [PubMed] [Google Scholar]
- Victora, C. , & Barros, A. (2000). Effect of breastfeeding on infant and child mortality due to infectious diseases in less developed countries. The Lancet, 355(9202), 451–455. [PubMed] [Google Scholar]
- World Health Organization and UNICEF (2003). Global strategy for infant and young child feeding. World Health Organization. [Google Scholar]
- Zafar, M. , Fatmi, Z. , & Shafi, K. (2014). Determinants of child feeding practices in Pakistan; secondary data analysis of demographic and health survey 2006‐07. Journal of Medical Nutrition and Nutraceuticals, 3(2), 78–84. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset has been uploaded as Additional File 1 (EBIF.dta).


