Abstract
Aim
This study aimed to evaluate the optimal combination of parameters for the management of pain during surgical abortion using transcutaneous acupoint electrical stimulation (TEAS).
Methods
This study recruited patients scheduled for surgical abortion between October 2014 and August 2015. The treatment protocol was created using three levels for each factor (stimulating time, acupoints, age, and parity). The primary outcomes were intraoperative visual analog scale (VAS), postoperative VAS, cervical relaxation degree and intraoperative blood loss. The secondary outcomes were the vital signs.
Results
Stimulation time was associated with intraoperative VAS scores (P < 0.001), acupoints were associated with postoperative VAS scores (P = 0.037), and age was associated with postoperative VAS scores (P < 0.043). Parity (P = 0.025) was associated with heart rate. A comprehensive analysis of the parameters revealed the best levels for each (stimulation time: from 15 min before operation to immediate postoperative; acupoints: SP 6 and LR 3; patient age 25.1–30.0 years; and parity: G≥2P0A≥1). Seven patients did not complete follow‐up. The remaining 135 subjects did not show continuous vaginal bleeding, abdominal pain, fever or any other adverse effect.
Conclusion
During surgical abortion, TEAS stimulation from 15 min before operation to immediate postoperative, SP 6 and LR 3, age 25.1–30.0 years and G≥2P0A≥1 were associated with the best analgesic effect.
Keywords: orthogonal design, pain, surgical abortion, transcutaneous electrical acupoint stimulation
Introduction
Unintended pregnancy accounts for more than 40% of all pregnancies worldwide and induced abortion is one of the ways to manage unintended pregnancies.1 Induced abortion includes medical and surgical abortions. Mifepristone combined with misoprostol is widely used for medical abortion.2 Although medical abortion is associated with less anxiety and pain than surgical abortion,3 there are potential risks of incomplete abortion, excessive bleeding and still ongoing pregnancy.4 On the other hand, surgical abortion is associated with high rates of complete abortion and short postoperative vaginal bleeding. Therefore, it is widely used in China. Nevertheless, expanding the cervix and scraping the endometrium can induce pain and discomfort and even cause increases of heart rate, changes of blood pressure and abortion syndrome.
Recently, acupuncture anesthesia and transcutaneous acupoint electrical stimulation (TEAS) has been suggested as an alternative to drug therapy for the management of pain. Indeed, TEAS is a new type of acupuncture with analgesic effect. TEAS integrates transcutaneous electrical nerve stimulation therapy and traditional acupuncture therapy.5 A study showed that TEAS can reduce postoperative pain, nausea and vomiting.6 TEAS is widely used for analgesia,7, 8, 9, 10, 11 especially for gynecological surgery and labor.12 A previous study by our group showed that TEAS may play a supporting role during surgical abortion,13 but there is no available study about the TEAS parameters associated with the most appropriate management of pain during surgical abortion.
Therefore, this study used an orthogonal design to evaluate the best combination of TEAS parameters for the management of pain during surgical abortion. The tested parameters were stimulation time, acupoint compatibility, age and condition of the patients. Hence, each of these four parameters was studied at three levels in order to determine the best combination of parameters for the management of pain during surgical abortion.
Methods
Study design
This was a cohort orthogonal design study of patients scheduled for surgical abortion between October 2014 and August 2015 at the outpatient operating room of the Obstetrics and Gynecology department of the First Affiliated Hospital of WenZhou Medical University. The study was approved by the ethics committee of the First Affiliated Hospital of WenZhou Medical University. All study procedures involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Each patient signed a written informed consent form. This study was registered (Chinese Clinical Trial Registry #ChiCTR‐IPR‐15007145).
Patients
The indications for surgical abortion were: (i) unwilling to continue pregnancy, the woman was suffering from a disease preventing the continuation of the pregnancy or the fetus had congenital malformations or genetic disease; (ii) pregnancy of less than 10 weeks; and (iii) no contraindication to surgery.3
The inclusion criteria were: (i) 18–40 years of age; (ii) gestational age (GA) of 42–70 days; and (iii) confirmed pregnancy by ultrasonography and urinary human chorionic gonadotropin (hCG). The exclusion criteria were: (i) known cardiovascular dysfunction; (ii) renal impairment; (iii) allergy to acupuncture needles or any contraindication to TEAS; (iv) opioid medications within a month; (v) operation expected to last >10 min; or (vi) inflammatory disease or psychiatric illness.
Out of the 184 patients evaluated for eligibility, 42 were excluded because they did not meet the eligibility criteria, and 11 declined participation (Figure 1); 142 patients were included, and 135 completed the trial.
Figure 1.
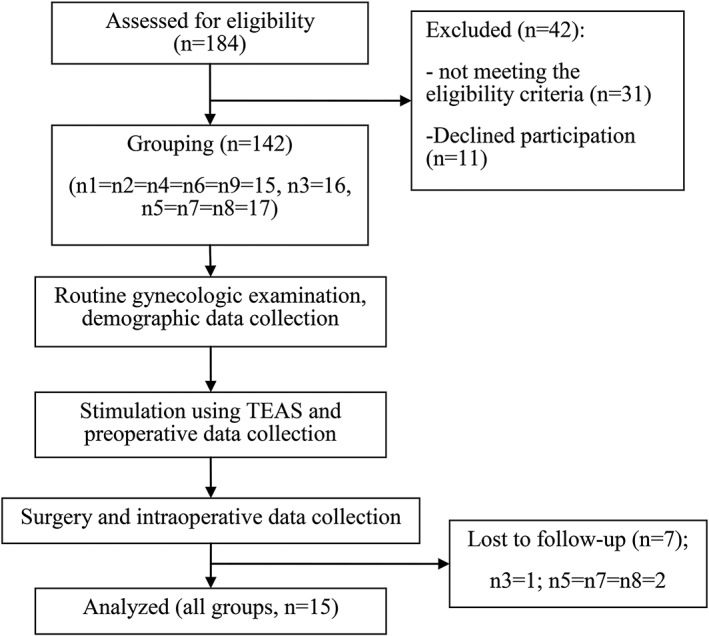
Patient flowchart.
Grouping
An L9 (34) orthogonal design was used in this study (Table 1).14, 15 Therefore, the patients were assigned to one of nine TEAS protocols. The subjects, an independent outcome assessor and the statistician were blinded to the implementation of TEAS. As previous studies7, 8, 9 have shown that TEAS has a significant analgesic effect, the present study did not include a control group.
Table 1.
The L9 (34) orthogonal design
| Test number | Column number | |||
|---|---|---|---|---|
| A | B | C | D | |
| T1 | 1 | 1 | 1 | 1 |
| T2 | 1 | 2 | 2 | 2 |
| T3 | 1 | 3 | 3 | 3 |
| T4 | 2 | 1 | 2 | 3 |
| T5 | 2 | 2 | 3 | 1 |
| T6 | 2 | 3 | 1 | 2 |
| T7 | 3 | 1 | 3 | 2 |
| T8 | 3 | 2 | 1 | 3 |
| T9 | 3 | 3 | 2 | 1 |
In Table 1, A, B, C and D denote the different treatment parameters, and 1, 2 and 3 indicate the three different levels for each parameter. The details of parameters and levels are shown in Table 2.
Table 2.
Parameters and levels used in the orthogonal design
| Parameters | Levels |
|---|---|
| A: Stimulating time | 1: 15 min before operation to immediate postoperative |
| 2: 20 min before operation to immediate postoperative | |
| 3: 25 min before operation to immediate postoperative | |
| B: Acupoints | 1: Sanyinjiao27 (SP 6) (anode) + Zusanli28 (ST 36) (cathode) |
| 2: Sanyinjiao (SP 6) (anode) + Taichong29 (LR 3) (cathode) | |
| 3: Sanyinjiao (SP 6) (anode) + Diji30 (SP 8) (cathode) | |
| C: Age | 1: ≤25 years |
| 2: ≥25 years and ≤ 30 years | |
| 3: >30 years | |
| D: Parity | 1: G1P0A0 |
| 2: G≥2P0A≥1 | |
| 3: GxP≥1Ax |
Fifteen patients were recruited in each group in order to fit the criteria for parameters C and D. Because of the orthogonal design, all groups had to be equal in size. Therefore, if a subject had to be excluded for any reason, new patients were screened until the group was complete.
Transcutaneous electroacupuncture
A portable battery‐operated electroacupuncture device (HANS‐100A, 100100410547, Ji Sheng Company, Beijing, China), which provides electrical current with an intensity of 0–30 mA, was used in this study. A frequency of 100 Hz, burst frequency of 2 Hz (dense‐dispersed waveform) and pulse duration of 0.5 ms were used.
The acupuncture points Sanyinjiao (SP 6), Zusanli (ST 36), Taichong (LR 3) and Diji (SP 8) were identified by the investigators, who were Chinese‐trained and licensed acupuncturists with a median of 10 years of experience. SP 6 is located on the medial side of the shank, 3 “cun” directly above the tip of the medial malleolus, on the posterior border of the medial aspect of the tibia. ST 36 is located on the anterior aspect of the leg, at 3 “cun” below the knee cap and one finger breadth from the anterior crest of the tibia. LR 3 is located on the dorsum of the foot, in the depression distal to the junction of the first and second metatarsal bones. SP 8 is located on the medial side of the shank, on the line joining the tip of the medial malleolus and Yinlingquan (SP 9) and 3 “cun” below SP 9 ([Link], [Link], [Link], Supporting information). For clarification, the “cun” is a measurement unit for the positioning of acupuncture points. Its full name in English could be “proportional measurement”. It is a standard method that uses the sclerotome as the main marker for positioning. By measuring their size, the length of all body parts can be converted to “cun” according to the proportions. For example, the distance from the wrist to the cubital fossa is traditionally defined as 12 “cun,” meaning that the distance from the wrist to the cubital fossa is divided into 12 equal segments.
All of the selected acupuncture points were swabbed with alcohol following a standard antiseptic process before the TEAS electrodes were applied. Four gel pads were cut to 20 × 20 mm and placed over the acupuncture points (bilaterally). Based on the parameters of Table 2, the anode was attached to SP 6 and the cathode attached to ST 36, LR 3 or SP 8. Each cleaned electrode was placed over the small gel pad; this allowed electrical stimulation to be focused mainly over the acupuncture points. The electrodes were then attached to the device. The strength of stimulation was increased until the woman felt a comfortable tingling in the area supplied by the nerve being stimulated. This stimulation protocol has been shown to be effective in inducing endorphin production.16
Before surgery, all subjects underwent a gynecological examination, ultrasound, blood routine and serology for HIV, HCV and HBsAg. All patients were monitored using a multifunctional monitor (BeneView T5, Mindray medical international Co., Ltd, Shenzhen, China) for blood pressure (BP), mean arterial pressure (MAP), heart rate (HR) and arterial oxygen saturation (SPO2) during surgery.
The abortion procedure was carried out according to standard clinical practice with a vacuum curette and suction. In the bladder lithotomy position, the vulva, vagina and cervix were disinfected conventionally. The cervix was expanded when the prescribed intervention time with TEAS was reached, as designed in Table 2. According to the size of the gestational sac, a suction tube of suitable size was introduced into the uterine cavity. A thorough vacuum suction was proceed with each stroke in either a clockwise or a counterclockwise manner to ensure that the entire uterine cavity has been covered. Intraoperative blood loss (BL) was measured. All abortions were performed by the same doctor, who is an associate chief physician of obstetrics and gynecology with more than 20 years of experience. After surgery, the participants were transferred to a ward when considered stable with regard to respiration and circulation, according to standard clinical criteria.
Evaluation indexes
After enrolment in the study, the participants were interviewed; the study purpose and the use of the visual analog scale (VAS) were explained. All data were recorded by an independent outcome assessor.
In order to assess the effect of TEAS on surgical abortion, the primary outcomes were intraoperative VAS, postoperative VAS, cervical relaxation degree (CRD) and intraoperative BL.
Pain intensity was evaluated with a VAS, which is a 10‐cm nongraduated line, with “no discomfort at all” indicated to the “0” end and “discomfort cannot be tolerated” indicated to the “10” end. All patients were asked to evaluate their pain using the VAS during suction in the operating room (worst pain during the procedure) and at 30 min after surgery in the ward. The patient was handed a clipboard with the VAS and was supervised by an independent outcome assessor. Two different forms were used for the two assessments.
Intraoperative BL was measured after filtration of the tissues using a measuring cup.17 The operative time was recorded as the time from the start of cervical dilatation until the end of suction. CRD was directly recorded as the number of cervical dilators that were entered into the intracervical mouth smoothly.18 The secondary outcomes were the range of BP (systolic/diastolic), MAP, SPO2 and HR, recorded at the beginning of the operation (T 0), at the time of suction (T 1) and 30 min after the operation (T 2).
Follow‐up
All participants were followed up by telephone. Follow‐up included whether there was continuous vaginal bleeding, abdominal pain or fever.
Sample size estimation
Sample size estimation was based on the comparison of two groups from an independent sample. The estimation was based on the assumption that TEAS could decrease the mean VAS by at least 2 points, assuming a standard deviation of 1.5. To yield a power of 90% with α = 0.05, a sample size of at least 12 subjects in each group was required. The analysis was performed using spss 18.0 for Windows (IBM, Armonk, NY, USA). Because of eventual technique failure or loss to follow‐up, a decision was made to recruit 15 patients in each group.
Statistical analysis
Normally distributed data were presented as mean ± standard deviation. Nonnormally distributed data were converted to ranks and presented as mean ± standard deviation. All data were analyzed by the orthogonal experiment design analysis of variance. Comparison between two groups was performed using the Bonferroni test. spss 18.0 for Windows (IBM, Armonk, NY, USA) was used for data analysis. Two‐sided P‐values <0.05 were considered statistically significant.
Results
Table 3 presents the characteristics of the patients. There were no differences among all groups in terms of preoperative BMI, GA, SP, DP, MAP, HR and SPO2 (all P > 0.05).
Table 3.
Characteristics of the patients (n = 15/group)
| Protocols | BMI (kg/m2) | GA (days) | SP | DP | MAP | HR | SPO2 |
|---|---|---|---|---|---|---|---|
| T1 | 23.1 ± 2.9 | 54.0 ± 7.9 | 115.7 ± 13.6 | 68.4 ± 8.5 | 81.9 ± 10.5 | 89.8 ± 16.3 | 99.5 ± 0.6 |
| T2 | 22.7 ± 2.9 | 54.4 ± 6.5 | 116.6 ± 13.6 | 68.5 ± 9.3 | 85.7 ± 11.4 | 86.5 ± 12.9 | 99.6 ± 0.5 |
| T3 | 22.5 ± 3.3 | 55.4 ± 6.5 | 120.9 ± 13.2 | 74.2 ± 8.6 | 91.0 ± 5.9 | 86.9 ± 15.2 | 99.3 ± 1.0 |
| T4 | 22.7 ± 3.1 | 56.1 ± 5.8 | 122.3 ± 15.0 | 75.3 ± 10.0 | 90.5 ± 13.9 | 88.8 ± 12.0 | 99.3 ± 0.6 |
| T5 | 22.7 ± 2.7 | 54.0 ± 5.7 | 126.3 ± 17.7 | 73.5 ± 10.6 | 94.8 ± 16.7 | 80.8 ± 13.9 | 99.3 ± 0.9 |
| T6 | 22.1 ± 2.6 | 56.3 ± 6.5 | 121.4 ± 13.7 | 74.8 ± 10.0 | 89.1 ± 10.1 | 90.8 ± 15.9 | 99.6 ± 0.5 |
| T7 | 22.3 ± 2.5 | 56.3 ± 6.8 | 123.0 ± 12.9 | 75.9 ± 9.5 | 93.8 ± 10.0 | 86.6 ± 14.2 | 99.2 ± 1.2 |
| T8 | 21.9 ± 2.6 | 54.6 ± 6.7 | 118.9 ± 12.1 | 72.5 ± 5.9 | 86.8 ± 6.2 | 87.2 ± 9.9 | 99.5 ± 0.6 |
| T9 | 21.6 ± 2.5 | 55.0 ± 6.3 | 127.5 ± 12.3 | 75.7 ± 9.1 | 91.8 ± 8.5 | 94.5 ± 14.6 | 99.5 ± 0.6 |
BMI, body mass index; DP, diastolic blood pressure; HR, heart rate; GA, gestational age; MAP, mean arterial pressure; SP, systolic blood pressure; SPO2, oxygen saturation.
Primary outcomes
Table 4 presents intraoperative VAS, postoperative VAS, CRD and intraoperative BL. The postoperative VAS data were not normally distributed and were converted to the rank of postoperative VAS for analysis of variance of the orthogonal test design. P A, P B, P C, and P D are the P‐values of the four parameters.
Table 4.
Comparisons of intraoperative VAS, postoperative VAS, CRD and intraoperative blood loss (n = 15/group)
| Protocols | Intra‐op VAS | Post‐op VAS | Rank of post‐op VAS | CRD | Intra‐op BL |
|---|---|---|---|---|---|
| T1 | 6.8 ± 1.1 | 2.5 ± 1.1 | 86.3 ± 30.8 | 5.93 ± 0.68 | 41.3 ± 27.7 |
| T2 | 5.9 ± 2.3 | 2.2 ± 2.3 | 65.4 ± 42.9 | 6.33 ± 0.65 | 64.0 ± 38.1 |
| T3 | 4.3 ± 1.8 | 0.9 ± 0.9 | 38.1 ± 22.8 | 6.43 ± 0.56 | 53.0 ± 34.8 |
| T4 | 4.8 ± 2.1 | 2.2 ± 2.2 | 67.2 ± 46.0 | 6.30 ± 0.88 | 67.3 ± 49.8 |
| T5 | 5.9 ± 1.4 | 1.7 ± 1.5 | 63.2 ± 40.8 | 6.07 ± 0.86 | 42.3 ± 34.5 |
| T6 | 7.0 ± 1.8 | 2.3 ± 1.1 | 79.6 ± 32.3 | 6.43 ± 0.73 | 39.7 ± 33.9 |
| T7 | 5.5 ± 1.4 | 1.5 ± 1.2 | 58.2 ± 35.3 | 6.15 ± 0.66 | 53.7 ± 50.6 |
| T8 | 6.0 ± 1.5 | 2.1 ± 1.1 | 71.9 ± 31.5 | 6.32 ± 0.75 | 53.0 ± 28.5 |
| T9 | 5.8 ± 1.5 | 2.7 ± 1.8 | 82.2 ± 39.2 | 6.30 ± 0.82 | 51.3 ± 30.7 |
| P A | 0.853 | 0.737 | 0.560 | 0.976 | 0.911 |
| P B | 0.059 | 0.037 | 0.058 | 0.353 | 0.839 |
| P C | <0.001 | 0.286 | 0.043 | 0.579 | 0.268 |
| P D | 0.198 | 0.066 | 0.056 | 0.243 | 0.096 |
P A, P B, P C and P D are the P‐values of the four parameters. BL, blood loss; CRD, cervix relaxation degree; VAS, visual analog scale.
Parameters A and D factors influenced intraoperative VAS. Parameter A did not influence postoperative VAS. Parameter B factor influenced intraoperative VAS (P = 0.059), where B 1 = 5.7, B 2 = 5.4 and B 3 = 6.2; two‐group comparisons showed that the difference between B 2 and B 3 was significant (P = 0.056). Parameter B influenced postoperative VAS (P = 0.058), where B 1 = 70.6, B 2 = 57.7 and B 3 = 75.7; two‐group comparisons showed that the difference between B 2 and B 3 was significant (P = 0.062). Parameter C influenced intraoperative VAS (P < 0.001), where C 1 = 6.6, C 2 = 5.0 and C 3 = 5.8; two‐group comparisons showed that the differences between any two‐group combinations of C 1, C 2 and C 3 were significant (P = 0.080). Parameter C influenced postoperative VAS (P = 0.043), where C 1 = 79.3, C 2 = 62.5 and C 3 = 62.3; two‐group comparisons showed that the differences between C 1 and C 2 (P = 0.091) and between C 1 and C 3 (P = 0.085) were significant. Parameter D influenced postoperative VAS (P = 0.056), where D 1 = 77.2, D 2 = 58.6 and D 3 = 68.2; two‐group comparisons showed that the difference between D 1 and D 2 was significant (P = 0.050). No parameter significantly influenced CRD. Parameter D influenced intraoperative BL (P = 0.096), where D 1 = 45.0, D 2 = 48.8 and D 3 = 61.4; two‐group comparisons showed that there was no difference among the three levels (P > 0.116). Parameters A, B and C did not influence intraoperative BL.
Secondary outcomes
Table 5 presents the secondary outcomes. Parameters A, B, C and D did not influence BP (SP/DP), MAP and rank of SPO2. Parameters A and C did not influence HR. Parameter B influenced HR (P = 0.082), where B 1 = 20.8, B 2 = 15.8 and B 3 = 20.7; two‐group comparisons showed that there was no difference among B 1, B 2 and B 3 (P = 0.15). Parameter D influenced HR (P = 0.025), where D 1 = 18.9, D 2 = 22.7 and D 3 = 15.7; two‐group comparisons showed that the difference between D 2 and D 3 was significant (P = 0.020).
Table 5.
Secondary outcomes among the different groups (n = 15/group)
| Protocols | SP | DP | MAP | HR | Rank of SPO2 |
|---|---|---|---|---|---|
| T1 | 19.1 ± 18.7 | 19.5 ± 15.9 | 21.1 ± 16.1 | 23.3 ± 20.0 | 81.2 ± 36.5 |
| T2 | 16.7 ± 6.5 | 12.0 ± 6.0 | 14.9 ± 9.5 | 16.6 ± 7.8 | 71.3 ± 34.4 |
| T3 | 19.3 ± 11.1 | 13.7 ± 10.0 | 17.2 ± 11.3 | 18.7 ± 10.9 | 64.3 ± 38.0 |
| T4 | 17.8 ± 11.6 | 15.3 ± 10.9 | 16.8 ± 14.8 | 18.1 ± 10.3 | 65.6 ± 40.1 |
| T5 | 20.1 ± 15.4 | 13.4 ± 7.7 | 17.9 ± 10.3 | 16.3 ± 8.6 | 54.6 ± 31.3 |
| T6 | 21.4 ± 12.3 | 17.5 ± 8.2 | 20.1 ± 10.1 | 28.5 ± 14.9 | 73.0 ± 34.9 |
| T7 | 18.3 ± 10.2 | 14.9 ± 9.0 | 17.3 ± 9.9 | 21.0 ± 12.7 | 67.8 ± 41.5 |
| T8 | 18.5 ± 12.3 | 12.8 ± 8.6 | 16.3 ± 10.4 | 12.4 ± 9.6 | 70.7 ± 38.9 |
| T9 | 20.1 ± 12.9 | 15.7 ± 9.4 | 15.4 ± 11.7 | 17.1 ± 9.3 | 63.4 ± 36.5 |
| P A | 0.876 | 0.906 | 0.730 | 0.260 | 0.596 |
| P B | 0.915 | 0.304 | 0.798 | 0.082 | 0.546 |
| P C | 0.888 | 0.319 | 0.484 | 0.300 | 0.304 |
| P D | 0.680 | 0.376 | 0.609 | 0.025 | 0.936 |
P A, P B, P C and P D are the P‐values of the four parameters. DP, diastolic blood pressure; HR, heart rate; MAP, mean arterial pressure; SP, systolic blood pressure; SPO2, oxygen saturation.
Combinations of parameters for the best effect
Comprehensive analysis of the parameters revealed that stimulation from 15 min before operation to immediate postoperative, SP 6 and LR 3, age 25.1–30.0 years19 and G≥2P0A≥1 showed the best analgesic effects.
Adverse effects
Seven patients did not complete the follow‐up. The remaining 135 subjects did not show continuous vaginal bleeding, abdominal pain, fever or any other adverse effect.
Discussion
Pain during surgical abortion may be managed using a number of drug protocols. TEAS can be used to manage pain in surgical patients,6, 7, 8, 9, 10, 11 for gynecological surgery and labor12 and for surgical abortion,13 but the optimal parameters for pain management during surgical abortion are unknown. Therefore, this study used an orthogonal design to compare the effectiveness of three different levels of four intervention parameters of TEAS for the management of pain during surgical abortion. In order to eliminate the influence of other factors, drugs, including narcotics, were not allowed. No control group is allowed in the orthogonal design. The results showed that during surgical abortion, TEAS stimulation from 15 min before operation to immediate postoperative, SP 6 and LR 3, age 25.1–30.0 years and G≥2P0A≥1 were associated with the best analgesic effects.
To the best of the authors’ knowledge, this is the first report on the use of TEAS alone during surgical abortion using an orthogonal design. Because of the short time of artificial abortion, 15, 20 and 25 min were selected as the three stimulation durations to study. According to the meridian theory of Chinese medicine, the acupoints of Sanyinjiao (SP 6), Zusanli (ST 36), Taichong (LR 3) and Diji (SP 8) were selected. A previous study showed that age and pain threshold are associated20 and that the highest abortion rate is among women of 21–35 years of age in China.21, 22 Therefore, ≤25, between 25 and 30 years and >30 years were selected as age parameters. At present, TEAS intervention during surgical abortion pain management included only studies in nulliparous women.13 Considered together, the results showed that the best analgesic effect of TEAS during surgical abortion was achieved in women aged between 25 and 30 years; nulliparous women but at least at their second pregnancy (G≥2P0A≥1); using the Sanyinjiao (SP 6) and Taichong (LR 3) acupoints; and using a stimulation time of 15 min.
In order to reflect the stability and fluctuation of the vital signs, BP, MAP, SPO2 and HR were monitored, and there were no significant fluctuations during surgical abortion under TEAS. On the other hand, a study showed that under propofol anesthesia, the SPO2 and MAP of pregnant women dropped significantly.23 The present study suggests that TEAS intervention could be safer than anesthesia for surgical abortion, but this will have to be compared in a trial.
Considered together, the results of the present study are supported by a number of studies that showed that TEAS can be successfully used to manage pain.24, 25, 26 In addition, it refined the results of one of our previous studies13 in determining which patients could benefit the most from TEAS and under which conditions.
Nevertheless, this study has some limitations. The sample size was small, and all subjects were from the same area. This study did not consider the effect of the four factors on the primary and secondary outcomes and was therefore unable to determine which factor played the most important role. The interval time points of the VAS score after operation were limited, and it was impossible to determine the effect of this method on long‐term pain after abortion. TEAS was not compared to other pain management methods used during surgical abortion. Finally, the present study identified TEAS parameters and categories of women that were associated with the best effects of TEAS. As no control group was included in the present study, we cannot conclude from that TEAS decreased pain in all patients as there was no comparator. It has to be inferred from our previous study.13
In conclusion, during surgical abortion, TEAS stimulation from 15 min before operation to immediate postoperative, SP 6 and LR 3, age 25.1–30.0 years and G≥2P0A≥1 were associated with the best analgesic effects.
Disclosure
None declared.
Supporting information
Figure S1 Electrodes at Sanyinjiao (SP6) and Zusanli (ST36).
Figure S2 Electrodes at Sanyinjiao (SP 6) and Taichong (LR 3).
Figure S3 Electrodes at Sanyinjiao (SP 6) and Diji (SP 8).
Acknowledgments
None.
Contributor Information
Linchai Zeng, Email: happyzlc@163.com.
Wenxia Xie, Email: xiewenxia@wmu.edu.cn.
References
- 1. Dutta M, Shekhar C, Prashad L. Level, trend and correlates of mistimed and unwanted pregnancies among currently pregnant ever married women in India. PLoS One 2015; 10: e0144400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Creinin M, Blumenthal P, Shulman L. Mortality associated with mifepristone‐misoprostol medical abortion. MedGenMed 2006; 8: 26. [PMC free article] [PubMed] [Google Scholar]
- 3. Cao ZY. The Obstetrics and Gynecology, 2nd edn. Beijing: People's Medical Publishing House, 2005. [Google Scholar]
- 4. Murray S, Wooltorton E. Septic shock after medical abortions with mifepristone (Mifeprex, RU 486) and misoprostol. CMAJ 2005; 173: 485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fang JQ, Chen YF, Liu YL. Under the effect of analgesia cutaneous nerve electrical stimulation therapy approaches. J Zhejing Inst Tradit Chin Med 1999; 23: 52–54. [Google Scholar]
- 6. Han JS. Acupuncture analgesia: Consensus and query. Chin J Pain Med 2011; 17: 9–14. [Google Scholar]
- 7. Yeh TY, Lin JC, Liu CF. Effect of transcutaneous electrical nerve stimulation through acupoints of Pucan (BL 61) and Shenmai (BL 62) on intraocular pressure in patients with glaucoma: A randomized controlled trial. J Tradit Chin Med 2016; 36: 51–56. [DOI] [PubMed] [Google Scholar]
- 8. Yang XY, Xiao J, Chen YH et al Dexamethasone alone vs in combination with transcutaneous electrical acupoint stimulation or tropisetron for prevention of postoperative nausea and vomiting in gynaecological patients undergoing laparoscopic surgery. Br J Anaesth 2015; 115: 883–889. [DOI] [PubMed] [Google Scholar]
- 9. Zhao W, Wang C, Li Z et al Efficacy and safety of transcutaneous electrical acupoint stimulation to treat muscle spasticity following brain injury: A double‐blinded, multicenter, randomized controlled trial. PLoS One 2015; 10: e0116976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wu HX, Wang K, Li GX. Effects of transcutaneous acupoint electrical stimulation onthe imbalance of Th1, Th2, Th17 and Treg cells following thoracotomy of patients with lung cancer. Exp Ther Med 2016; 11: 495–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Liu X, Wang J, Wang B et al Effect of transcutaneous acupoint electrical stimulation on propofol sedation: An electroencephalogram analysis of patients undergoing pituitary adenomas resection. BMC Complement Altern Med 2016; 16: 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chen CB, Jiao ZQ, Zhao YM. The application of the HANS in clinical anesthesia. World J Integr Tradit Western Med 2010; 5: 437–438. [Google Scholar]
- 13. Feng X, Ye T, Wang Z et al Transcutaneous acupoint electrical stimulation pain management after surgical abortion: A cohort study. Int J Surg 2016; 30: 104–108. [DOI] [PubMed] [Google Scholar]
- 14. Bolboaca SD, Jantschi L. Design of Experiments: Useful orthogonal arrays for number of experiments from 4 to 16. Entropy 2007; 9: 198–232. [Google Scholar]
- 15. Collins LM, Dziak JJ, Li R. Design of experiments with multiple independent variables: A resource management perspective on complete and reduced factorial designs. Psychol Methods 2009; 14: 202–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lau KS, Jones AY. A single session of Acu‐TENS increases FEV1 and reduces dyspnoea in patients with chronic obstructive pulmonary disease: A randomised, placebo‐controlled trial. Aust J Physiother 2008; 54: 179–184. [DOI] [PubMed] [Google Scholar]
- 17. Mathur M, Rani J, Vijayshree. Role of sublingual misoprostol for cervical priming in first trimester medical termination of pregnancy. J Clin Diagn Res 2014; 8: OC01–OC03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Huang J, Geng LL, Meng L. The optimal time interval between oral misoprostol and artificial abortion for cervical priming: A random prospective trial. Chin J Clin Obstet Gynecol 2004; 5: 109–112. [Google Scholar]
- 19. Motaghi Z, Poorolajal J, Keramat A, Shariati M, Yunesian M, Masoumi SZ. Induced abortion rate in Iran: A meta‐analysis. Arch Iran Med 2013; 16: 594–598. [PubMed] [Google Scholar]
- 20. Zhang W, Lu H, Kan QC. Comparison of age‐related experiment pain in women. Med Philos 2008; 29: 46–48. [Google Scholar]
- 21. Hu XH, Shao H, Wu LP. Investigation on the current situation and analysis on the related factor of abortion in women of childbearing age from factories in Shenzhen city. Maternal Child Health Care Chin 2013; 28: 3648–3649. [Google Scholar]
- 22. Jin LJ, Sun MY, Zhu XF. Survey and analysis on sociological characteristics of people undergoing artificial abortion and causes of abortion. J Nurs Rehabil 2010; 9: 750–752. [Google Scholar]
- 23. Wu J, Yao S, Wu Z et al A comparison of anesthetic regimens using etomidate and propofol in patients undergoing first‐trimester abortions: Double‐blind, randomized clinical trial of safety and efficacy. Contraception 2013; 87: 55–62. [DOI] [PubMed] [Google Scholar]
- 24. Chao AS, Chao A, Wang TH et al Pain relief by applying transcutaneous electrical nerve stimulation (TENS) on acupuncture points during the first stage of labor: A randomized double‐blind placebo‐controlled trial. Pain 2007; 127: 214–220. [DOI] [PubMed] [Google Scholar]
- 25. Yeh ML, Chung YC, Chen KM, Tsou MY, Chen HH. Acupoint electrical stimulation reduces acute postoperative pain in surgical patients with patient‐controlled analgesia: A randomized controlled study. Altern Ther Health Med 2010; 16: 10–18. [PubMed] [Google Scholar]
- 26. Walsh DM, Howe TE, Johnson MI, Sluka KA. Transcutaneous electrical nerve stimulation for acute pain. Cochrane Database Syst Rev 2009; 15: CD006142. [DOI] [PubMed] [Google Scholar]
- 27. Wu YY, Jiang YL, He XF et al Effects of Electroacupuncture with dominant frequency at SP 6 and ST 36 based on meridian theory on pain‐depression dyad in rats. Evid Based Complement Alternat Med 2015; 2015: 732845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Chen Y, Zhang H, Tang Y, Shu J. Impact of bilateral ST36 and PC6 electroacupuncture on the depth of sedation in general anaesthesia. Acupunct Med 2015; 33: 103–109. [DOI] [PubMed] [Google Scholar]
- 29. Chen T, Wang K, Xu J, Ma W, Zhou J. Electroacupuncture reduces postoperative pain and analgesic consumption in patients undergoing thoracic surgery: A randomized study. Evid Based Complement Alternat Med 2016; 2016: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Chen S, Miao Y, Nan Y et al The study of dynamic characteristic of Acupoints based on the primary dysmenorrhea patients with the tenderness reflection on Diji (SP 8). Evid Based Complement Alternat Med 2015; 2015: 158012. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1 Electrodes at Sanyinjiao (SP6) and Zusanli (ST36).
Figure S2 Electrodes at Sanyinjiao (SP 6) and Taichong (LR 3).
Figure S3 Electrodes at Sanyinjiao (SP 6) and Diji (SP 8).


