Abstract
Objective
The purpose of this systematic review and meta-analysis was to examine the impact of pragmatic versus prescriptive study designs on the outcomes of low back and neck pain when using mobilization or manipulation techniques.
Methods
This study design was a systematic review and meta-analysis, which was performed according to the PRISMA guidelines. A search of MEDLINE and CINAHL complete databases was performed. Article titles and abstracts were reviewed to identify studies comparing mobilization and manipulation in low back or neck pain that met eligibility criteria. Validity of studies was examined using the Cochrane Risk of Bias tool. Data analysis was performed using RevMan 5.3. Forest plots were constructed after data were analyzed to determine effect sizes.
Results
Thirteen studies with a total of 1313 participants were included in the systematic review, and 12 studies with 977 participants in the meta-analysis. For most time-points prescriptive studies found manipulation to be superior to mobilization for both pain and disability. At no time-point did pragmatic designs find a difference between mobilization and manipulation for either pain or disability.
Discussion
When a pragmatic design was used, representing actual clinical practice, patients improved with both techniques with no difference between mobilization and manipulation. When clinicians were prescribed techniques, not representing true clinical practice, manipulation showed better outcomes than mobilization for pain and disability.
Level of Evidence
1a
Keywords: Manipulation, mobilization, prescriptive, pragmatic, manual therapy, pain, disability, spine
Introduction
Physical therapists often treat individuals with a variety of musculoskeletal conditions including mechanical low back pain (LBP) and/or cervical pain (CP) [1–3]. It has been reported that approximately 28.8% of the population 18 years and older will experience some form of low back pain within the last 3 months [4]. Additionally, 15.8% of the population will have experienced some form of neck pain within the last 3 months [4]. The 1-year incidence of neck pain has been reported to be between 10.4 and 21.3%, with higher incidence noted in office and computer workers [5]. In fact a recent systematic analysis found low back and neck pain to be one of the leading causes of disability in numerous countries around the world [6].
The cost of LBP continues to rise, ranking as the most expensive musculoskeletal ailment to manage. As of 2006, it is estimated that in the United States the total costs of low back pain exceeds 100 billion dollars yearly [7]. Approximately two-thirds of this is indirect costs, resulting from lost wages and productivity [7]. There is an estimated 149.1 million lost workdays due to low back pain [8]. In terms of neck pain, between 11 and 14.1% of workers each year will be limited in their activity due to their symptoms [9]. One study from the Netherlands determined the total cost to treat cervical pain to be €485 million, which currently equates to about 520 million US dollars [10]. As the prevalence and costs of LBP and neck pain management continue to rise, debate remains among the medical community on the most effective way to reduce pain and disability as well as the societal burden associated with these disorders.
There are many conservative treatment approaches used to manage mechanical spine pain. Among those, interventions including manual therapy, therapeutic exercise, and modalities are most common [11]. Manual therapy, including manipulation and mobilization, appears to be one of the most common treatment choices applied by physical therapists for the management of these conditions. Research has shown that manual therapy and exercise is effective in treating non-specific spinal pain [1,12,13]. However, evidence from studies has been conflicting [14,15] so it is unclear whether spinal manipulation or mobilization is superior to the other in the management of these conditions.
In addition to the controversies surrounding which technique is superior [16], it is also unclear if clinician decision-making impacts outcomes [17]. Two studies have explored the therapist equipoise and have found associations between the clinician’s preferred technique and the patient reported outcomes. Interestingly, a recent trial compared two different forms of mobilization (one therapist selected and one in which the mobilization was standardized) and the results showed similar outcomes for pain and disability between groups, but at a 6-month follow-up, the group receiving therapist selected mobilization reported greater perceived well-being [18]. Further complicating issues is a meta-analysis by Kent et al. [19] that investigated if clinician treatment choice improves the outcomes of manual therapy for nonspecific LBP. Although few quality studies existed, Kent et al. found that roughly two-thirds of the included RCTs had clinician choice of treatment, and that there was no significant difference favoring the studies that allowed for clinician choice as opposed to those that did not [19].
Study designs that allow for clinician choice are often referred to as pragmatic while study designs that prescribe exactly which technique to use and levels to target are known as prescriptive. Pragmatic study designs attempt to examine the effectiveness of interventions as they would be applied in a typical clinical setting [20,21]. This often involves broader inclusion criteria with less focus on internal validity, and often comparing effectiveness of two competing treatments. Pragmatic trials involve a population that closely mirrors what a clinician would typically see in practice and frequently allows for clinical decision-making in the plan of care. Prescriptive study designs typically have narrow inclusion criteria, stronger internal validity, and specifically dosed interventions [21–23]. This design is optimal in maximizing ideal controlled circumstances rather than clinical reality. Prescriptive designs are focused on determining the specific effects of isolated treatments. It is plausible that the two study designs could find opposing results when directly comparing two interventions. To the best of our knowledge, to date there have been no systematic reviews or meta-analysis comparing the effects of manipulation and mobilization between prescriptive and pragmatic designs. Therefore, the purpose of this systematic review and meta-analysis is to examine the impact of pragmatic versus prescriptive study designs on the outcomes of low back and neck pain when using mobilization or manipulation techniques.
Methods
We performed this systematic review and meta-analysis according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [24].
Literature search
An electronic literature search was conducted between 1 December 2016 and 20 December 2016 in MEDLINE and CINAHL complete databases from their dates of inception to December of 2016. A combination of search terms was used to identify possible relevant articles. Search terms included mobilization, manipulation, low back pain, cervical pain, clinician choice, disability, and pain. Nine different combinations of these terms were used to complete the literature search which included: mobilization, low back pain; mobilization, manipulation; mobilization, manipulation, low back pain; mobilization, manipulation, low back pain, clinician choice; mobilization, manipulation, low back pain, clinician choice, disability; mobilization, manipulation, low back pain, clinician choice, disability, pain; mobilization, manipulation, cervical pain, clinician choice, disability; mobilization, manipulation, cervical pain, clinician choice, disability, pain; mobilization, manipulation, and cervical pain. Reference lists from identified articles were hand searched for any other potentially eligible studies. Additionally, corresponding authors of relevant articles were contacted by email and asked if they could identify any additional articles that had not been identified through the database searches (Figure 1).
Figure 1.
Flowchart of included articles.
Study selection
Six researchers completed the database searches independently and reviewed all article titles and abstracts to identify potentially relevant articles. All reviewers needed to reach a consensus for a study to be included in the systematic review and meta-analysis. Articles also needed to satisfy all of the following inclusion criteria: written in English; randomized clinical trials; compared mobilization versus manipulation in isolation; included patients with low back pain or neck pain; and used an outcome measure of pain and/or disability (Figure 1). Mobilization was defined as low-velocity spinal mobilization and manipulation was defined as high-velocity, low amplitude, thrust manipulation (HVLAT).
Eligible studies were classified as prescriptive or pragmatic based on the criteria used by Kent et al. To be classified as pragmatic, clinicians needed to be able to choose the technique and spinal levels to be treated. If both of these criteria were not met, the study was classified as prescriptive [19].
Data extraction
Data extraction was compiled using a standard form modified from a previous systematic review and meta-analysis [25]. Data included consisted of participants, sample size, interventions, follow-up period, outcome measure, adverse events, and main results.
Risk of bias assessment tool
The methodological quality of each study was determined using the Cochrane risk of bias tool [26]. This tool uses five different items (selection bias, performance bias, detection bias, attrition bias, and reporting bias) to examine the validity of studies. The items are rated on a three-point scale to assess risk of bias (0 = high risk, 1 = unclear risk, 2 = low risk) with a maximum score of 16 points and lower scores indicating a higher risk of bias.
Similar to a previously published systematic review and meta-analysis we calculated a percentage score for each study [25]. For example, if a study scored 11/16 points that would receive a risk of bias score of 68.8%. We also used a cut off of 69% for indicating high and low risk of bias [25].
Data analysis
The primary outcomes for this systematic review were pain and disability. We performed the meta-analyses using RevMan 5.3 (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, Denmark) for different follow-up periods similar to a recent systematic review; immediate (within 5 min of the application of the intervention), 1–6 days, 4 weeks, 5–11 weeks, and 3–6 months. For analysis of continuous data we selected to use the standardized mean differences (SMD) with the 95% confidence interval (95% CI) since it is more generalizable [27] and allows for the assessment of outcomes that used different scales. The random effects model was used to account for variability between studies and its effect on the intervention. The I2 statistic was used to measure the heterogeneity between trials [28]. According to Higgins and colleagues, an I2 value of 25% represents a small, 50% moderate, and 75% large, degree of heterogeneity [29]. Effect size was interpreted using Cohen’s criteria for pooled estimates. Cohen described 0.2 as small, 0.5 as moderate, and 0.8 as large effect sizes [30].
Results
Of the 29,384 potential studies identified during the original search, 13 studies were deemed relevant after screening titles, abstracts, and full article reviews. No additional articles were provided by any of the corresponding authors who were emailed asking if they were aware of any other articles that could potentially fit out eligibility criteria. Figure 1 shows the PRISMA flow diagram of the search strategy and results in addition to reasons for exclusion. No additional studies were identified through hand searching reference lists or contacting the corresponding author on each study. A total of 13 studies with a combined total of 1313 participants were included in the systematic review with 12 studies and 977 participants included in the meta-analysis. Of the three authors we contacted requesting additional data to complete the analysis, one author [31] did not provide adequate data to develop forest plots as the corresponding author was unable to identify the original data-set.
Study characteristics
Data included consisted of participants, sample size, interventions, follow-up period, outcome measure, adverse events, and main results can be found in Table 1.
Table 1.
Characteristics of the included studies using prescriptive and pragmatic intervention.
| Study | Participants | Intervention | Follow-up Period | Outcome Measure | Results Between Groups |
|---|---|---|---|---|---|
| PRESCRIPTIVE STUDIES | |||||
| Cassidy et al. [36] | n = 100 subjects with report of unilateral neck pain with referral into trapezius muscle (16 < 1 week, 34.1 weeks-6 months, 50 > 6 months) | Group 1 (n = 52): Manipulated (rotational cervical to symptomatic level) | Within 5 min following intervention | Pain Intensity (NPS) | Difference in pain intensity between groups: 6.8, P = 0.05 |
| Group 1 (n = 52): mean ± SD age, 34.5 ± 13 years | Group 2 (n = 48): Mobilized (muscle energy technique with stretching to hypertonic cervical musculature) | ||||
| Group 2 (n = 48): 37.7 ± 12.5 years | |||||
| Cleland et al. [27] | n = 112 subjects with report of low back pain with or without symptoms into the lower extremity; median length of symptoms, (interquartile range), 45 (27, 60); 57 male, 55 female; mean ± SD age, 40.4 ± 11.5 years | Group 1 (n = 37): Supine thrust manipulation (non-specific lumbar) and spinal ROM exercise (2 sessions week 1), exercise regime (one session weekly for 3 weeks) | 1 week, 4 week, 6 months | Subjective Disability Report (ODQ) | Difference in disability between groups 1&3: 1 week, 11.45, P < 0.001; 4 weeks, 14.23, P < 0.001; 6 months, 5.97, P < 0.027 |
| Group 1 (n = 37): 43.7 ± 10.4 years | Group 2 (n = 38): Side-lying thrust manipulation (non-specific lumbar) and spinal ROM exercise (2 sessions week 1), exercise regime (one session weekly for 3 weeks) | Pain Intensity (NPS) | Difference in disability between groups 2&3: 1 week, 7.94, P = 0.003; 4 weeks, 12.73, P < 0.001; 6 months, 6.81, P = 0.004 | ||
| Group 2 (n = 38): 37.1 ± 11.5 years | Group 2 (n = 38): Side-lying thrust manipulation (non-specific lumbar) and spinal ROM exercise (2 sessions week 1), exercise regime (one session weekly for 3 weeks) | No statistically significant difference in disability between groups 1&2 reported | |||
| Group 3 (n = 37): 40.1 ± 12 years | Group 3: (n = 37): Non-thrust technique (2 Hz oscillatory P-A mobilization L4&L5) and spinal ROM exercise (2 sessions week 1), exercise regime (one session weekly for 3 weeks) | Difference in pain intensity between groups 1&3: 1 week, 2.07, P < 0.001; 4 weeks, 1.79, P = 0.002; 6 months, 0.58, P = 0.018 | |||
| Difference in pain intensity between groups 2&3: 1 week, 1.46, P < 0.001; 4 weeks, 1.32, P = 0.002; 6 months, 0.39, P = 0.29 | |||||
| No statistically significant difference in pain intensity between groups 1&2 reported | |||||
| Cleland et al. [28] | n = 60 subjects with mechanical neck pain with or without upper extremity symptoms between the ages of 18 and 60; 27 male, 33 female; mean ± SD age, 43.3 ± 12.7 years | Group 1 (n = 30): Non-thrust mobilization/manipulation (30 sec grade III/IV central P-A mob each, T3-T6 ) | 2–4 days following intervention | Subjective Disability Report (NDI) | Difference in disability between groups: 10.03 (95% CI: 5.3, 14.7), P < 0.001 |
| Group 1 (n = 30): 42.7 ± 13.9 years | Group 2 (n = 30): Thrust mobilization/manipulation (supine upper thoracic (T1-T4) and middle thoracic (T5-T8)) | Pain Intensity (NPS) | Difference in pain intensity between groups: 2.03 (95% CI: 1.4, 2.7), P < 0.001 | ||
| Group 2 (n = 30): 43.8 ± 11.5 years | |||||
| Dunning et al. [29] | n = 107 ; 34 males, 73 females with mechanical neck pain between the superior nuchal line and first thoracic spinal process | Group 1 (n = 56): HVLA thrust manipulation (R and L supine C1-C2, supine T1-T2) | 48 h following intervention | Subjective Disability Report (NDI) | Difference in disability between groups: 8 (95% CI: 5.9, 10.2), P < 0.001 |
| Group 1 (n = 56): mean ± SD age, 41.5 ± 11.9 years | Group 2 (n = 51): Non-thrust mobilization (prone grade IV P-A unilateral oscillatory mobilization 30 sec R&L, 30 sec prone grade IV P-A central oscillatory mobilization T1-T2) | Pain Intensity (NPS) | Difference in pain intensity between groups: 2.0 (95% CI: 1.5, 2.5), P < 0.001 | ||
| Group 2 (n = 51): 42.7 ± 13.9 years | |||||
| Lopez-Lopez et al. [32] | n = 48 subjects 18–65 years of age with history of neck pain within the superior nuchal line and first thoracic spinous process with more than 12 weeks of evolution without radicular symptoms; 6 male, 42 female | Group 1 (n = 15) HVLA technique (supine HVLAT manipulation to hypomobile cervical zygapophyseal joints until cavitation noted, max of 2 attempts | Immediately following intervention | Pain intensity (VAS) | A statistically significant difference in pain intensity between groups was reported, P = 0.04 |
| Group 1 (n = 15): mean ± SD age, 35.4 ± 8.0 years | Group 2 (n = 16) Mobilization (prone grade III P-A unilateral oscillatory mobilization over hypomobile cervical segments, 3 periods of 2 min) | ||||
| Group 2 (n = 16); 36.0 ± 9.9 years | |||||
| Group 3 (n = 17): 37.8 ± 8.6 years | |||||
| Pérez et al. [33] | n = 61 subjects 20–65 years of age with pain in the posterior cervical spine persisting at least 12 weeks without radicular symptoms to head, trunk, or arms; 35 male, 26 female | Group 1 (n = 19) HVLAT technique (supine HVLAT manipulation to hypomobile cervical segments in hypomobile planes of motion, max of 2 thrusts) | Immediately following treatment, 1 month, month, 3 month | Subjective Disability Report (NDI) | No statistically significant difference in disability between groups reported |
| Group 1 (n = 19): mean ± SD age, 36.2 ± 8.9 years | Group 2 (n = 21) Mobilization (prone P-A unilateral oscillatory mobilization to hypomobile cervical segments, 2 min, 3 times | Pain Intensity (VAS) | No statistically significant difference in pain intensity between groups reported | ||
| Group 2 (n = 21): 35.6 ± 10.3 years | |||||
| Group 3 (n = 21): 37.8 ± 9.1 years | |||||
| Salom-Moreno et al. [34] | n = 52 subjects 18–60 years of age with idiopathic mechanical neck pain persisting for at least 6 months with no radicular symptoms; 30 male, 22 female | Group 1 (n = 27) Thrust manipulation (supine, HVLAT manipulation to T3-T6 until cavitation noted, max of 2 attempts) | 10 min following intervention | Pain intensity (NPS) | Difference in pain intensity between groups: 1.4 (95% CI: 0.8–2.1), P < 0.001 |
| Group 1 (n = 27): mean ± SD age 32 ± 7 years | Group 2 (n = 25) Non-thrust mobilization (prone grade III-IV P-A central oscillatory mobilization to T3-T6 segments, 20 second bouts, 2 min total) | ||||
| Group 2 (n = 25): 34 ± 9 years | |||||
| Suvarnnato et al. [35] | n = 39 subjects with either unilateral or bilateral chronic mechanical pain in the posterior neck and/or shoulder region; 10 male, 29 female | Group 1 (n = 13): Manipulation (prone ‘screw thrust’ high velocity thrust technique to zygapophyseal joints T6-T7) | Immediately following intervention, 24 h | Pain Intensity (VAS) | Difference in pain intensity between groups: immediately following intervention, .85 (CI:7.84–9.54), P < 0.05; 24 h, 1.94 (CI: 7.84–11.72), P < 0.05 |
| Group 1 (n = 13): mean ± SD age, 35.33 ± 10.96 years | Group 2 (n = 13): Mobilization (grade III unilateral P-A mobilization on both sides of zygapophyseal joints of T6-T7 R&L, 1 min each) | ||||
| Group 2 (n = 13): 37 ±12.59 years | |||||
| Group 3 (n = 13): 39.91 ± 11.52 years | |||||
| PRAGMATIC STUDIES | |||||
| Cook et al. [26] | n = 149 subjects 18 years of age or older with mechanically producible LBP; 70 males, 79 females | Group 1 (n = 76): Thrust manipulation (technique to affected lumbar segment, including sidelying rotational and/or supine ASIS thrust) | Following treatment #2, at discharge (group 1: mean ± SD days in care, 33.8 ± 26.2 days; group 2: mean ± SD days in care, 37.6 ± 33.4 days) | Subjective Disability Report (ODI) | No statistically significant difference in disability between groups reported |
| Group 1 (n = 76): mean age ± SD, 46.1 ± 14.5 years | Group 2 (n = 73): Non-thrust manipulation (technique to affected lumbar segment, including central P-A, unilateral P-A, and sidelying rotational mobilization) | Pain Intensity (NPS) | No statistically significant difference in pain intensity between groups reported | ||
| Group 2 (n = 73): 50.3 ± 15.1 years | |||||
| Gemmell et al. [38] | n = 47 subjects 18–64 years of age with neck pain persisting between 4 and 12 weeks; 10 males, 37 females | Group 1 (n = 16): Manipulated (HVLAT techniques to restricted cervical and upper thoracic segments) 2x/week for 3 weeks or until symptom free | Immediately following final treatment, 3 month, months, 12 months | Subjective Disability Report (NBQ) | No statistically significant difference in disability between groups reported |
| Group 1 (n = 16): mean ± SD age, 46.9 ± 9.1 years | Group 2 (n = 15): Mobilized (supine grade III P-A and transverse oscillatory low grade passive movement to articular pillar and and spinous process of one or more restricted upper thoracic or cervical segments) 2x/week for 3 weeks) | Pain Intensity (NPS) | No statistically significant difference in pain intensity between groups reported | ||
| Group 2 (n = 15): 43.8 ± 13.0 years | |||||
| Group 3 (n = 16): 46.8 ± 11.8 years | |||||
| Griswold et al. [30] | n = 20 subjects 18–70 years of age with primary complaint of reproducible non-specific neck pain between the superior nuchal line and first thoracic spinous process; 9 males, 11 females | Group 1 (n = 7): Manipulated (HVLA thrust to the most symptomatic segment of both the cervical and upper thoracic spine) | Following second treatment (3–4 days), at discharge (36–41 days) | Subjective Disability Report (NDI) | No statistically significant difference in disability between groups reported |
| Group 1 (n = 7): mean ± SD age, 37.4 ± 15.7 years | Group 2 (n = 13): Mobilized (applied to the most symptomatic cervical and thoracic segments | Pain Intensity (NPS) | No statistically significant difference in pain intensity between groups reported | ||
| Group 2 (n = 13): 41.2 ± 14.6 years | |||||
| Hurwitz et al. [31] | n = 336 subjects with report of neck pain from upper thoracic spine to occiput and the surrounding musculature; 105 male, 231 female | Group 1 (n = 171): Manipulation: with and without heat and with and without NMES. Subjects assigned to one of the spinal mobilization groups received at least 1 controlled dynamic thrust, applied with high-velocity and low-amplitude with minimal extension and rotation directed at one or more restricted upper thoracic and/or cervical spine joint segment within patient tolerance | 2 week, 6 week, 3 month, 6 months | Subjective Disability Report (NDI) | Difference in disability intensity between groups: 2 week, 1.03 (95% CI: –0.002–2.08); 6 week, .92 (95% CI: –0.032–2.17); 3 month, .05 (95% CI: –1.33–1.44); 6 months, 0.46 (95% CI: –0.089–1.82) |
| Group 1 (n = 171): mean ± SD age, 45.7 ± 11.8 years | Group 2 (n = 165): Mobilization: with and without heat and with and without NMES. Subjects assigned to one of the spinal mobilization groups received one or more movements of low velocity and variable amplitude directed to one or more restricted upper thoracic and/or cervical spine joint segments | Pain Intensity (NPS) | Difference in pain intensity between groups: 2 week, .14 (95% CI: –0.055–0.26); 6 week, .23 (95%CI: –0.26–0.72); 3 month, 0.05 (95% CI: –0.46–0.56); 6 months, 0.01 (95% CI: –0.52–0.54) | ||
| Group 2 (n = 165): 45.7 ± 12.2 years | |||||
| Leaver et al. [37] | n = 182 subjects 18–70 years of age with neck pain between the superior nuchal line and first thoracic spinous process persisting less than 3 months; 64 male, 118 female | Group 1 (n = 91) Manipulated (HVLAT manipulation technique applied to the upper cervical spine) | Pain: 2 week, 12 weeks | Subjective Disability Report (NDI) | No statistically significant difference disability between groups reported |
| Group 1 (n = 91): mean ± SD age , 38 ± 10.3 years | Group 2 (n = 91) Mobilized (low velocity oscillatory passive movement applied to the upper cervical spine) | Disability: 4 week, 12 weeks | Pain intensity (NPS) | No statistically significant difference in pain between groups reported | |
| Group 2 (n = 91): 39.7 ± 11.1 years | |||||
Notes: NPS = Numeric Pain Rating Scale, ODQ = Oswestry Disability Questionnaire, NDI = Neck Disability Index; NBQ = Neck Bournemouth Questionnaire: VAS = Visual Analog Scale.
Outcome measures
All 13 studies used a Visual Analog Scale (VAS) or Numeric Pain Rating Scale (NPRS) to measure pain-related outcomes. A total of seven studies reported outcome measures on disability [14,15,31–35] including the Neck Disability Index (NDI), Neck Bournemouth Questionnaire (NBQ), and the Oswestry Disability Index (ODI).
Prescriptive approach
Of the 13 total studies, 8 (61.5%) examined the effects of mobilization versus manipulation in a prescriptive treatment design where the clinician did not have choice or clinical decision-making and included a total of 579 subjects. 7 prescriptive studies (467 subjects) examined mobilization versus manipulation when treating mechanical neck pain [ 32–33,37–39]. One study (112 subjects) examined mobilization versus manipulation when treating mechanical lower back pain [15].
Pragmatic approach
Of the 13 total studies, 5 (38.5%) examined the effects of mobilization versus manipulation in a pragmatic treatment design where the clinician had choice and clinical decision-making and included a total of 734 subjects. A total of 4 studies (585 subjects) examined mobilization versus manipulation when treating mechanical neck pain [31,34,40,41]. Additionally, 1 study (149 subjects) examined mobilization versus manipulation when treating mechanical lower back pain [14].
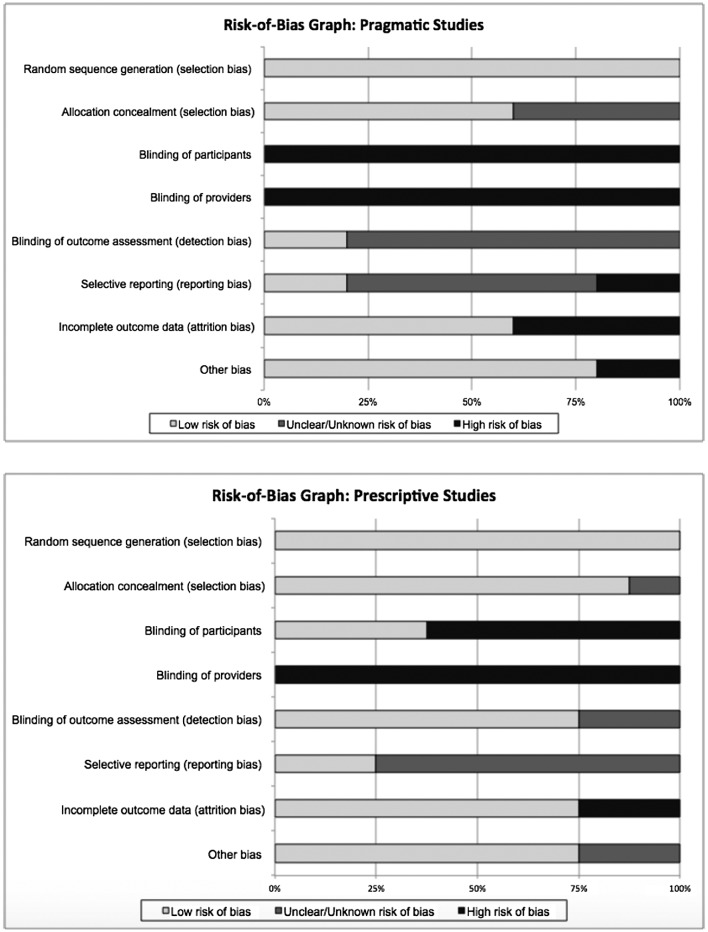
Risk-of-bias appraisal
The mean risk of bias scores of prescriptive studies was greater than pragmatic studies. The mean ± SD score on the Cochrane risk of bias tool across all eight prescriptive studies was 67.97% ± 8.48%. Six studies [15,33,35–38] had a score of at least 69% (11/16), indicating a moderate to low risk of bias. The other two studies [32,39] scored less than 69%, indicating high risk of bias (Figure 2).
Figure 2.
Risk of bias mean scores across pragmatic and prescriptive studies.
The mean ± SD score on the Cochrane risk of bias tool across all five pragmatic studies was 53.75% ± 16.30%. Two studies [32,41] had a score of at least 69% (11/16), indicating a moderate to low risk of bias. The other three studies [31,34,41] scored less than 69%, indicating high risk of bias (Figure 2).
None of the studies had low risk of bias for all eight categories due to the impossibility to blind the providers to type of manual therapy provided. Only three studies [35–37] were able to blind the participant due to the intervention characteristics. In 7 of the 13 studies [15,31,33,36–40], blinding of the assessor was successfully reported. Selective reporting bias (incomplete outcome data) was present in 10 of the 13 studies [15,31–35,37,39–41]. Figure 3 represents bias and risk of bias across studies for each individual prescriptive and pragmatic study.
Figure 3.

Risk of bias across pragmatic and prescriptive studies
Note: + low risk of bias, - high risk of bias, ? unclear risk of bias.
Primary analyses
Prescriptive outcomes for pain and disability
A total of 8 studies out of 13 (61.5%) compared pain outcomes in those treated with manipulations or mobilizations using a prescriptive approach. In studies reporting immediate outcomes, the SMD (0.45, 95% CI; 0.16, 0.74) demonstrates that manipulation was superior to mobilization in regards to an improvement in pain. Studies that reported findings within 1–6 days (SMD; 1.14, 95% CI; 0.83, 1.45), and 1–4 weeks (SMD; 1.02, 95% CI; 0.77, 1.27) also presented data that favored manipulations over mobilizations. However, data reported during 5–11 weeks showed no statistically significant difference between the two methods (SMD; 0.16, 95% CI; −0.48, 0.81). At longer term follow-up (3–6 month range), manipulations again proved to be more effective (SMD; 0.41, 95% CI; 0.06, 0.77) than mobilizations for reducing pain. Forest plots for pain when mobilization and manipulation were prescriptive can be found in Figure 4.
Figure 4.
Prescriptive mobilization vs. manipulation pain outcomes.
A total of four studies included in this meta-analysis reported disability scores when clinician’s treatment was standardized. The results suggest that there was no difference between prescriptive manipulation and mobilization at the immediate (SMD; −0.19, 95% CI; −0.81, 0.43), and 5–11-week follow-up (SMD; −0.21, 95% CI; −0.83, 0.41). However manipulation had a significant effect on decreasing disability scores compared to prescriptive mobilizations at 1–6 days (SMD; 1.31, 95% CI; 0.97, 1.64), 1–4 weeks (SMD; 0.85, 95% CI; 0.58, 1.11), and 3–6 months (SMD; 0.46, 95% CI; 0.11, 0.80) (Figure 5).
Figure 5.
Prescriptive mobilization vs. manipulation disability outcomes.
Pragmatic outcomes of pain and disability
A total of 5 studies out of 13 (38.5%) compared outcomes for pain when individuals with neck or low back pain were treated with manipulation or mobilization using a pragmatic approach. Overall, there was no statistically significant difference between mobilizations or manipulations at any of the designated time frames. The SMDs were 0.26 (95% CI; −0.66, 1.18), −0.05 (95% CI; −0.34, 0.25), 0.01 (95%CI; −0.29, 0.32), 0.11 (95% CI; −0.19, 0.40) 0.38 (95% CI; −0.33, 1.09) at 1–6 days, 1–4 weeks, 5–11 weeks, 3–6 months, and 7–12 months, respectively, as shown by Figure 6.
Figure 6.
Pragmatic mobilization vs. manipulation pain outcomes.
Of the 13 studies reviewed, only 3 (23.1%) pragmatic studies reported disability scores. Figure 7 demonstrates that there was no statistically significant difference between mobilizations or manipulations at, 1–6 days (SMD; 0.43, 95% CI; −0.50, 1.36), 1–4 weeks (SMD; −0.06, 95% CI; −0.35, 0.24), 5–11 weeks (SMD; −0.04, 95% CI; −0.34, 0.26), or 3–6 months (SMD; −0.03, 95% CI; −0.33, 0.26).
Figure 7.
Pragmatic mobilization vs. manipulation disability outcomes.
The one pragmatic study by Hurwitz et al. [31] that was not included in the meta-analysis found no difference between manipulation and mobilization for pain or disability.
Discussion
This systematic review and meta-analysis was performed to investigate the difference in disability and pain outcomes within individuals with back and neck pain when mobilization and manipulation techniques were performed in either a prescriptive or pragmatic fashion in both the short and long terms. Thirteen CT’s were identified including 8 which used a prescriptive design [15,32,33,35–39], and 5 which used a pragmatic approach [14,31,34,40,41]. The results of this meta-analysis suggest that when using a prescriptive approach comparing mobilization to manipulation to treat pain and disability, the outcomes favored manipulation. However, when a pragmatic approach to using manual therapy was performed in the respective studies, mobilization and manipulation were found to be equivalent. Additionally, when considering the 95% CIs around the point estimate for effect size at each time point, we noticed no overlap for pain at 1–6 days (95% CI; 0.83, 1.45 vs. 95% CI; −0.34, 0.25), 1–4 weeks (95% CI; 0.77, 1.27 vs. 95%CI; −0.29, 0.32), and disability at the 1–4 week follow-up (95% CI; 0.58, 1.11 vs. 95% CI; −0.35, 0.24). This further suggests that when applied in a prescriptive fashion manipulation has a superior outcome in reducing pain and disability compared to when both are applied in a pragmatic fashion for both pain and disability at 1–4 weeks and pain 1–6 days. However, the overlap in the 95% CI for pain and disability in the 3–6-month follow-up suggests there may be no actual difference between the outcomes of pragmatic and prescriptive study designs.
A number of reasons can explain the findings of the systematic review and meta-analysis. A number of differences exist between prescriptive and pragmatic studies such as inclusion criteria, different levels of focus on internal and external validity including the method of treatment delivery. The pragmatic approach is more representative of actual clinical care and demonstrates that when clinicians are allowed to use their decision-making and expertise, manipulation and mobilization have similar outcomes. In contrast, when clinician choice is removed, as in the prescriptive approach, which is not a true representation of actual clinical practice, a moderate effect size was observed in favor of manipulation. However, this type of study design is not actually representative of the method in which clinicians currently practice and in such the results may not be generalizable to actual clinical practice.
The included prescriptive studies had less risk of bias than the pragmatic approaches suggesting higher levels of internal validity. This may be reflective of the design nuances associated with pragmatic trials, which are Phase III in orientation, are designed to reflect a true clinical practice setting, and devote greater attention to external validity. Mechanistically, under controlled situations, it does appear that manipulation has greater benefit than mobilization for pain reduction. Indeed, one could argue that under less control (in pragmatic studies) some of the effect of manipulation may be lost through the interactions germane to a normal clinical setting (e.g. attrition of patients, compliance, technique dosage and response) resulting in no difference between treatment techniques. It is worth noting that the prescriptive study results may also be reflective of sampling bias. For example, Cleland et al. [15] only selected subjects for inclusion criteria if they satisfied a clinical prediction rule [43]. We view these findings as two of the most interesting results of the systematic review, which require further investigation.
Strengths and limitations of the review
Strengths of this review include contacting corresponding authors on studies we included in this review to determine if we had missed any potentially relevant studies. We also used the previously validated Cochrane Risk of Bias Tool in assessing internal validity of the included research and statistical pooling of all but one of the identified relevant studies. However, due to the nature of our question, this review does carry some limitations. First, we only searched two databases. It is possible that other databases might have revealed other studies relevant to the current systematic review. Also, a limited number (13) of available RCT’s comparing manipulation to mobilization techniques with a low risk of bias score were available as it is impossible to blind the provider of the specific technique performed. We also were unable to include the Hurwitz et al. [31] study in the forest plots as adequate data were not provided in the article. Additionally, we included studies from various manual practitioners (e.g. physical therapy, chiropractors) and the literature search criteria included only English articles, which means we may not have captured additional studies in differing languages.
Conclusion
The results of this systematic review and meta-analysis suggest studies that used a prescriptive approach found manipulation to be superior to mobilization at most time points for individuals with neck and mechanical back pain. However, this design type is not entirely representative of actual clinical practice and removes any clinical decision-making which potentially could impact the effectiveness of either mobilization or manipulation. When clinicians had a choice in the segment targeted and technique used there was no significant difference in pain and disability outcome scores between patients treated with manipulation and mobilization. This suggests that when mobilization is performed in the exact same fashion as it would be in actual clinical practice it may be just as useful a technique as manipulation.
Disclosure statement
No potential conflict of interest was reported by the authors.
Notes on contributors
Daniel Roenz is a third-year doctor of physical therapy student at Franklin Pierce University. Upon graduation in March of 2018, he will begin his career as a physical therapist and plans to specialize in orthopedics and manual therapy.
Jake Broccolo is a third-year doctor of physical therapy student at Franklin Pierce University. Upon graduation in March of 2018, he will begin his career as a physical therapist and plans to specialize in orthopedics.
Steven Brust is a third-year doctor of physical therapy student at Franklin Pierce University. Upon graduation in March of 2018, he will begin his career as a physical therapist and plans to specialize in orthopedics.
Jordan Billings is a third-year doctor of physical therapy student at Franklin Pierce University. Upon graduation in March of 2018, she will begin her career as a physical therapist and plans to specialize in acute inpatient therapy.
Alexander Perrott is a third-year doctor of physical therapy student at Franklin Pierce University. Upon graduation in March of 2018, he will begin his career as a physical therapist and plans to specialize in orthopedics and geriatrics.
Jeremy Hagadorn is a third-year doctor of physical therapy student at Franklin Pierce University. Upon graduation in March of 2018, he will begin his career as a physical therapist and plans to specialize in orthopedics.
Chad Cook is the director of the Doctor of Physical Therapy program at Duke University. He is a clinical researcher, physical therapist, and author. He has co-authored three textbooks and has over 200 publications with specific interest focused on orthopedic examination and treatment.
Joshua Cleland is a professor in the Doctor of Physical Therapy program at Franklin Pierce University. He is a clinical researcher, author, and practicing clinician who has co-authored four textbooks and has over 200 publications with specific interest focused on the efficacy of manual therapy and exercise for disorders affecting the spine and extremities.
Supplementary data
The supplementary material for this article is available online at https://doi.org/10.1080/10669817.2017.1398923
Supplementary Material
References
- [1].Hidalgo B, Detrembleur C, Hall T, et al. The efficacy of manual therapy and exercise for different stages of non-specific low back pain: an update of systematic reviews. J Man Manip Ther. 2013;22:59–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Petersen T, Christensen R, Juhl C. Predicting a clinically important outcome in patients with low back pain following McKenzie therapy or spinal manipulation: a stratified analysis in a randomized controlled trial. BMC Musculoskelet Disord. 2015;16:74. 10.1186/s12891-015-0526-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Garcia JD, Arnold S, Tetley K, et al. Mobilization and manipulation of the cervical spine in patients with cervicogenic headache: any scientific evidence? Front Neurol. 2016;7:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].National Center for Health Statistics Health, United States, 2011: with special feature on socioeconomic status and health. Hyattsville, MD; 2012. [PubMed] [Google Scholar]
- [5].Hoy DG, Protani M, De R, et al. The epidemiology of neck pain. Best Prac Res Clin Rheumatol. 2010;24(6):783–792. 10.1016/j.berh.2011.01.019 [DOI] [PubMed] [Google Scholar]
- [6].GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1545–1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Katz JN. Lumbar disc disorders and low-back pain: socioeconomic factors and consequences [review]. J Bone Joint Surg Am. 2006;88(Suppl 2):21–24. [DOI] [PubMed] [Google Scholar]
- [8].Guo HR, Tanaka S, Halperin WE, et al. Back pain prevalence in US industry and estimates of lost workdays. Am J Public Health. 1999;89(7):1029–1035. 10.2105/AJPH.89.7.1029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Côté P, Velde GVD, Cassidy JD, et al. The burden and determinants of neck pain in workers. Spine. 2008:S33–S38. [DOI] [PubMed] [Google Scholar]
- [10].Borghouts JA, Koes BW, Vondeling H, et al. Cost-of-illness of neck pain in The Netherlands in 1996. Pain. 1999;80:629–636. 10.1016/S0304-3959(98)00268-1 [DOI] [PubMed] [Google Scholar]
- [11].Page P. Cervicogenic Headaches: an evidence-led approach to clinical management. Int J Sports Phys Ther. 2011;6:254–266. [PMC free article] [PubMed] [Google Scholar]
- [12].Paige N, Miake-Lye I, Booth M, et al. Association of spinal manipulative therapy with clinical benefit and harm for acute low back pain: systematic review and meta-analysis. JAMA. 2017;317:1451–1460. 10.1001/jama.2017.3086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].National Institute for Health and Care Excellence [Internet] Low back pain and sciatica in over 16s: assessment and management. 2016. Available from: www.nice.org.uk/guidance/ng59 [PubMed]
- [14].Cook C, Learman K, Showalter C, et al. O’halloran B. Early use of thrust manipulation versus non-thrust manipulation: a randomized clinical trial. Man Ther. 2013;18:191–198. 10.1016/j.math.2012.08.005 [DOI] [PubMed] [Google Scholar]
- [15].Cleland JA, Fritz JM, Kulig K, et al. Comparison of the effectiveness of three manual physical therapy techniques in a subgroup of patients with low back pain who satisfy a clinical prediction rule. Spine. 2009;34:2720–2729. 10.1097/BRS.0b013e3181b48809 [DOI] [PubMed] [Google Scholar]
- [16].Cook C. How about a little love for non-thrust manipulation? J Man Manip Ther. 2012;20:1–2. 10.1179/106698112X13243937084444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Bishop MD, Bialosky JE, Penza CW, et al. The influence of clinical equipoise and patient preferences on outcomes of conservative manual interventions for spinal pain: an experimental study. J Pain Res. 2017;10:965–972. 10.2147/JPR [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Donaldson M, Petersen S, Cook C, et al. A prescriptively selected nonthrust manipulation versus a therapist-selected nonthrust manipulation for treatment of individuals with low back pain: A randomized clinical trial. J Orthop Sports Phys Ther. 2016;46:243–250. 10.2519/jospt.2016.6318 [DOI] [PubMed] [Google Scholar]
- [19].Kent P, Marks D, Pearson W, et al. Does clinician treatment choice improve the outcomes of manual therapy for nonspecific low back pain? A Metaanalysis J Man Manip Ther. 2005;28:312–322. [DOI] [PubMed] [Google Scholar]
- [20].Treweek S, Zwarenstein M. Making trials matter: pragmatic and explanatory trials and the problem of applicability. Trials. 2009;10:37. 10.1186/1745-6215-10-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Schwartz D, Lellouch J. Explanatory and pragmatic attitudes in therapeutical trials. J Clin Epidemiol. 2009;62:499–505. 10.1016/j.jclinepi.2009.01.012 [DOI] [PubMed] [Google Scholar]
- [22].Maclure M. Explaining pragmatic trials to pragmatic policymakers. J Clin Epidemiol. 2009;62:476–478. 10.1016/j.jclinepi.2008.06.021 [DOI] [PubMed] [Google Scholar]
- [23].Rowbotham MC, Gilron I, Glazer C, et al. Can pragmatic trials help us better understand chronic pain and improve treatment? Pain. 2013;154:643–646. 10.1016/j.pain.2013.02.034 [DOI] [PubMed] [Google Scholar]
- [24].Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Desjardins-Charbonneau A, Roy JS, Dionne CE, et al. The efficacy of manual therapy for rotator cuff tendinopathy: A systematic review and meta-analysis. J Orthop Sports Phys Ther. 2015;45:330–350. 10.2519/jospt.2015.5455 [DOI] [PubMed] [Google Scholar]
- [26].Furlan AD, Malmivaara A, Chou R, Maher CG, Deyo RA, Schoene M, et al. 2015 updated method guideline for systematic reviews in the cochrane back and neck group. Spine. 2015;40:1660–1673. 10.1097/BRS.0000000000001061 [DOI] [PubMed] [Google Scholar]
- [27].Takeshima N, Sozu T, Tajika A, et al. Which is more generalizable, powerful and interpretable in meta-analyses, mean difference or standardized mean difference? BMC Med Res Methodol. 2014;14:30. 10.1186/1471-2288-14-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions [Internet] Version 5.1.0 [updated March 2011]. The Cochrane Collaboration; 2011. Available from http://handbook.cochrane.org [Google Scholar]
- [29].Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed Hillsdale (NJ): L. Erlbaum Associates; 1988. [Google Scholar]
- [31].Hurwitz EL, Morgenstern H, Harber P, et al. A randomized trial of chiropractic manipulation and mobilization for patients with neck pain: clinical outcomes from the UCLA neck-pain Study. Am J Public Health. 2002;92:1634–1641. 10.2105/AJPH.92.10.1634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Cleland JA, Glynn P, Whitman JM, et al. Short-term effects of thrust versus nonthrust mobilization/manipulation directed at the thoracic spine in patients with neck pain: a randomized clinical trial. Phys Ther. 2007;87:431–440. 10.2522/ptj.20060217 [DOI] [PubMed] [Google Scholar]
- [33].Dunning JR, Cleland JA, Waldrop MA, et al. Upper cervical and upper thoracic thrust manipulation versus nonthrust mobilization in patients with mechanical neck pain: a multicenter randomized clinical trial. J Orthop Sports Phys Ther. 2012;42:5–18. 10.2519/jospt.2012.3894 [DOI] [PubMed] [Google Scholar]
- [34].Griswold D, Learman K, O’halloran B, et al. A preliminary study comparing the use of cervical/upper thoracic mobilization and manipulation for individuals with mechanical neck pain. J Man Manip Ther. 2014;23:75–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Lopez-Lopez A, Alonso Perez JL, Gonzalez Gutierez JL, et al. Mobilization versus manipulations versus sustain apophyseal natural glide techniques and interaction with psychological factors for patients with chronic neck pain: randomized controlled trial. Eur J Phys Rehabil Med. 2015;51:121–132. [PubMed] [Google Scholar]
- [36].Pérez HI, Perez JLA, Martinez AG, et al. Is one better than another?: A randomized clinical trial of manual therapy for patients with chronic neck pain. Man Ther. 2014;19:215–221. [DOI] [PubMed] [Google Scholar]
- [37].Salom-Moreno J, Ortega-Santiago R, Cleland JA, et al. Immediate changes in neck pain intensity and widespread pressure pain sensitivity in patients with bilateral chronic mechanical neck pain: a randomized controlled trial of thoracic thrust manipulation vs non–thrust mobilization. J Manipulative Physiol Ther. 2014;37:312–319. 10.1016/j.jmpt.2014.03.003 [DOI] [PubMed] [Google Scholar]
- [38].Suvarnnato T, Puntumetakul R, Kaber D, et al. The effects of thoracic manipulation versus mobilization for chronic neck pain: a randomized controlled trial pilot study. J Phys Ther Sci. 2013;25:865–871. 10.1589/jpts.25.865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Cassidy JD, Lopes AA, Yong-Hing K. The immediate effect of manipulation versus mobilization on pain and range of motion in the cervical spine: a randomized controlled trial. J Manipulative Physiol Ther. 1992;15:570–575. [PubMed] [Google Scholar]
- [40].Leaver AM, Maher CG, Herbert RD, et al. A randomized controlled trial comparing manipulation with mobilization for recent onset neck pain. Arch Phys Med Rehabil. 2010;91:1313–1318. 10.1016/j.apmr.2010.06.006 [DOI] [PubMed] [Google Scholar]
- [41].Gemmell H, Miller P. Relative effectiveness and adverse effects of cervical manipulation, mobilisation and the activator instrument in patients with sub-acute non-specific neck pain: results from a stopped randomised trial. Chiropr & Osteopat. 2010;18:20. 10.1186/1746-1340-18-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Bishop MD, Torres-Cueco R, Gay CW, et al. What effect can manual therapy have on a patient’s pain experience? Pain Manage. 2015;5:455–464. 10.2217/pmt.15.39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Childs JD, Fritz J, Flynn T, et al. A clinical prediction rule to identify patients with low back pain most likely to benefit from spinal manipulation: a validation study. Ann Intern Med. 2004;141:920–928. 10.7326/0003-4819-141-12-200412210-00008 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.