Abstract
Context/Objective
Spinal Cord Injury (SCI) patients face unique identity challenges associated with physical limitations, higher comorbid depression, increased suicidality and reduced subjective well-being. Post-injury identity is often unaddressed in subacute rehabilitation environments where critical physical and functional rehabilitation goals are prioritized. Therapeutic songwriting has demonstrated prior efficacy in promoting healthy adjustment and as a means of expression for post-injury narratives. The current study sought to examine the identity narratives of therapeutic songwriting participants.
Design
Case-series analysis of the individual identity trajectories of eight individuals.
Setting
Subacute rehabilitation facility, Victoria, Australia.
Participants
Eight individuals with an SCI; 7 males and 1 female.
Intervention
Six-week therapeutic songwriting intervention facilitated by a music therapist to promote identity rehabilitation.
Outcome Measures
Identity, subjective well-being and distress, emotional state.
Results
Three participants demonstrated positive trajectories and a further three showed negative trajectories; remaining participants were ambiguous in their response. Injury severity differentiated those with positive trajectories from those with negative trajectories, with greater injury severity apparent for those showing negative trends. Self-concept also improved more in those with positive trajectories. Core demographic variables did not however meaningfully predict the direction of change in core identity or wellbeing indices.
Conclusion
Identity-focused songwriting holds promise as a means of promoting healthy identity reintegration. Further research on benefits for those with less severe spinal injuries is warranted.
Keywords: Spinal cord injuries, Self concept, Rehabilitation, Music therapy, Identity
Introduction
Approximately 10,000–20,000 Australians currently have a traumatic Spinal Cord Injury (SCI). The incidence of SCI is heavily skewed toward men, with estimates suggesting 70–80% of those with a SCI are men.1,2 Spinal injuries are predominantly experienced within the 16–30 year age group, but recent reporting has noted an increase in older age groups. The causes of SCI are varied, but the majority result from motor vehicle accidents or falls.
The effects of SCI depend to a large extent on the level and grade of injury. The level dictates whether the SCI results in tetraplegia (loss of sensation and/or movement of all four limbs) or paraplegia (loss of sensation and/or movement in lower limbs and trunk). The grade is categorized as complete, involving a loss of all movement and sensation in affected areas, or incomplete, involving some retention of movement and/or sensation below the level of SCI. In addition to paralysis and sensation loss, frequent sequelae of SCI include bowel and bladder incontinence, pain, spasticity, and sexual dysfunction.
Research suggests that people with SCI face a number of significant challenges with respect to the psychosocial and emotional impact of their injury, which may go undetected during subacute rehabilitation.3,4 People with SCI face increased risk for psychopathology, including depression and anxiety 5–10; with some authors citing a fivefold increase in suicide rates following SCI.11 Changed family responsibilities and associated carer burden can also lead to relationship breakdowns and loss of friendships, which increases the risk of social isolation and can perpetuate depressive symptomatology.12 Reduced subjective quality of life is frequently reported among SCI populations,3,13,14 and this can perpetuate mood disturbances. Maladaptive coping styles and emotion dysregulation have also been noted to be major influences on wellbeing after SCI.15,16
Identity is a construct which underpins many aspects of post-SCI adjustment.7,17 Identity is both personally and socially constructed and captures a person's unique, individual perceptions as to their nature, life roles, goals, ambitions and achievements. While identity has been long emphasized as a critical component of psychosocial adjustment, the role of identity for those with SCI remains understudied.18 The traumatic nature of SCI means that the injury is internalized as a significant and immediate threat to self.19,20 In this sense, traumatic SCI shares a commonality with the Acquired Brain Injury (ABI) and Traumatic Brain Injury (TBI) literature. Exploration of identity across both SCI and ABI/ TBI studies has identified themes of a shattered or broken self21–23 whereby adjustment difficulties are predicated on the disconnect between perceived current and prior (pre-injury) selves. Maladaptive views of identity post-injury, which can include the desire to return to their former identity and level of functioning, have been associated with maladaptive coping styles and subsequent risk for the development of psychopathology.24 By contrast, healthy perceptions of self appear more aligned with the literature on post-traumatic growth in which people find new meaning and a re-alignment of values and core priorities post-injury.25,26 Reintegration or renegotiation of identity remains a key goal of effective psychosocial adjustment following SCI.27
Therapeutic songwriting is one approach that has been used to promote adjustment to some of the typical losses following TBI, including loss of independence and functioning, loss of life roles and loss of future hopes and dreams.28 Songwriting within a therapeutic context involves assisting individuals to tell their stories through the creation of lyrics and music.29 Therapeutic songwriting enables the person with an acquired injury to use the creative process in a way that allows for reviewing, processing, reframing, and re-authoring his or her life. Songwriting is a culturally acceptable and accessible medium for expression. When used in a therapeutic context, songwriting can reflect a person’s unique experience and personality, and in so doing also capture a representation of their emotions and feelings at that particular point in time.29 Further, the song itself can be a means of communicating with loved ones, reliving positive memories, and affirming progress and recovery. Songwriting provides an alternative vehicle for communication and exploration of pertinent personal concerns and emotional distress and has been found to be an effective way of enhancing growth and self-awareness.30 Further description of the potential underlying mechanisms of therapeutic songwriting are accessible in Baker et al.31
A specific identity-focused therapeutic songwriting intervention has not been previously reported in an inpatient SCI rehabilitation setting. Further, the post-SCI experience and identity perceptions of SCI patients in sub-acute rehabilitation remain underrepresented in the literature. This project aims to characterize the identity narratives of people with SCI in a sub-acute rehabilitation facility that underwent a tailored identity-focused therapeutic songwriting program.
Method
Setting and participants
Participants were individuals with SCI undergoing inpatient rehabilitation at a large rehabilitation hospital in metropolitan Melbourne, Victoria, Australia.
Materials
Identity measures
Identity was evaluated via the Head Injury Semantic Differential Scale (HISDS)32 and the Tennessee Self-Concept Scale – 2 (TSCS-2).33 The HISDS comprises 20 contrasting adjective-pairs (e.g. dependent, independent) rated on a 7-point Likert scale from one descriptor to the opposite descriptor. The HISDS has been shown to have internal reliability (Cronbach’s alpha 0.88), as well as concurrent validity with the Leeds Scale for emotional distress (Tyerman,32 as cited in Ellis-Hill & Horn34). The TSCS-2 comprises 82 items across six self-concept subscales: physical, moral, personal, family, social, and academic, which are rated on a 5-point Likert scale ranging from ‘always false' to ‘always true.' Fitts and Warren33 cite adequate psychometric properties with a median internal consistency score of 0.80 for adults and strong test-retest reliability (0.82).35 Both scales were utilized to determine which measure was most sensitive to identity changes within this population, to inform a future larger scale study.
Subjective wellbeing/ distress
Subjective wellbeing and associated constructs were measured through the Satisfaction with Life Scale,36 a 5-item measure rated on a 7-point Likert scale (Cronbach’s alpha of 0.78; Vassar,37 as cited in Corrigan et al.38), and the Flourishing Scale (FS),39 an 8-item measure assessing thriving or self-perceived success in life on a 7-point Likert scale. The FS was recently supported as a reliable and valid tool for use in a New Zealand population,40 with results comparable to Diener’s original validation.39 Subjective distress was measured through the Generalized Anxiety Disorder 7-item (GAD-7) questionnaire41 and the 9-item Patient Health Questionnaire (PHQ-9).42 The GAD-7 has been validated as a brief screen of anxious symptomatology (α = 0.8943) and uses a 4-point scale to assess the severity of generalized anxiety symptoms. The PHQ-9, a measure of depressive symptomatology, has been found to have adequate sensitivity and specificity in detecting symptoms of depression in TBI populations.44 The Positive and Negative Affect Schedule45 was also incorporated as a 20-item measure of affective state using 5-point Likert scales. The PANAS has been found by Crawford and Henry46 to have adequate convergent validity with the Depression Anxiety and Stress Scales (t (986) = 7.523, P < 0.001) and the Hospital Anxiety and Depression Scale (t (737) = 7.667, P < 0.001).
Procedure
Participants underwent a 6-week tailored music therapy intervention (therapeutic songwriting) during which they worked together with a registered music therapist over 12 sessions to create three songs exploring past, present, and future selves. An individual song was created about each of these perceived selves. Each song was created via a collaborative process between participant and music therapist, following the protocol outlined in Figure 1 below. Sessions one to four focused on the participant’s past, and were dedicated to using the participant’s perception of their life history to shape a song that captured the participant’s view of their pre-injury identity. Sessions five to eight focused on the present, with participants creating a song that reflected on changes resultant from their injury. Sessions nine to twelve focused on the future, and participants created a song that captured their views about their future self. Throughout the songwriting process, participants were encouraged to reflect on their identity perceptions to shape the song lyric content collaboratively with the music therapist, and make choices in terms of the musical elements that shaped each song (genre, melody, key, harmonies, instrumentation, etc.). Participants reported varied histories with regard to prior engagement with music. Two participants indicated a prior history of learning a musical instrument. Music listening behaviors also varied across the sample. Two participants reported listening to music for several hours each day. Remaining participants reported listening to music for varied amounts of time ranging from ‘about an hour a day’ to ‘less than once a year’.
Figure 1.
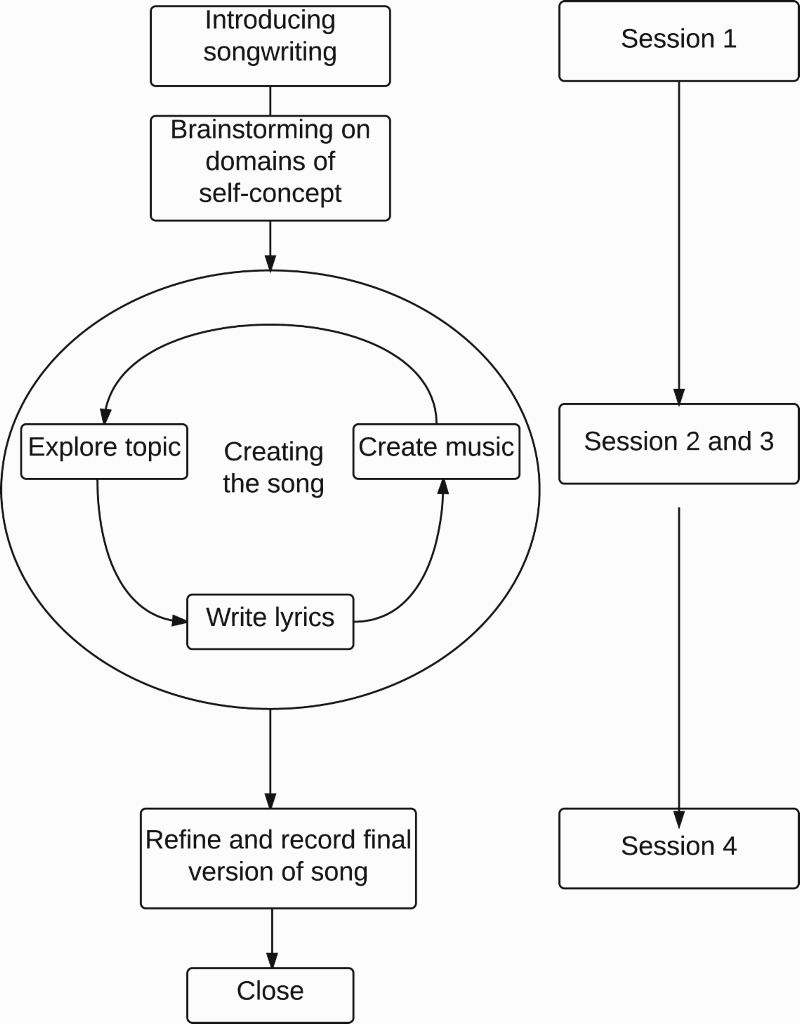
Songwriting for self-concept protocol (Reproduced with permission from Tamplin et al.48).
In order to assess any corresponding changes in identity self-ratings, subjective mood and wellbeing indices, participants utilized an iPad application to complete a questionnaire battery outlined above at three timepoints — prior to the intervention, at the mid-point of the intervention (3 weeks) and at the conclusion of the intervention (6 weeks). Two participants (Participants 3 and 4) were unable to complete mid-intervention measures due to impending discharge timing. Further details about the intervention protocol and songwriting measures are accessible elsewhere (refer31,47,48).
Results
Demographic and clinical characteristics
There were eight participants in this study. The mean age was 30.4 years, (SD = 12.2 years, range = 17–50 years) and only one was female. They were an average of 2.8 months (SD 1.4 months, range = 45–157 days) post-injury. The level and grade of injury were as follows: incomplete paraplegia (Participants 3, 5, 6, and 8), complete paraplegia (Participants 2 and 4) and complete tetraplegia (Participants 1 and 7). Of the eight participants, two (Participants 2 and 5) were prescribed mood-altering medication at the time of the intervention.
Initial classifications
Raw scores and change scores from pre- to post-intervention in all outcome measures were compared for all participants. From this examination, participants were categorized as either those with positive trajectories; those who exhibited the greatest degree of the positive shift relative to other participants on at least three indices, or those with negative trajectories; those who exhibited the greatest degree of negative shift relative to other participants on at least three indices. The change in outcome measures from baseline to post-intervention was highly varied, both across participants and within participants across outcome measures. Nonetheless, Participants 3, 6 and 8 showed the greatest degree of positive change in at least half the outcome measures, and for the purposes of this paper, were classified as those with positive trajectories. Participants 1, 4 and 7 showed the greatest degree of negative changes on at least three of the eight outcome measures, and for the purposes of this paper, were classified as those with negative trajectories. Participants 2 and 5 demonstrated more mixed profiles but with limited change in most indices from pre- to post-intervention and thus were not examined further in this paper.
Identify profiles associated with positive and negative trajectories
Table 3 presents an overview of the core identity scores for all participants on the TSCS-2 and the HISDS respectively. Table 2 shows that those with positive trajectories generally demonstrated an improvement in self-concept over time, with both self-concept indices showing an increase pre to post-intervention for Participants 6 and 8. Participants 3 also showed improvement in the HISDS measure, but conversely showed a decline in TSCS-2 scores. In contrast, all participants with negative trajectories showed a decrease in self-concept scores over time as measured by the TSCS-2. Participants 1 and 7 showed an initial decline in self-concept scores as measured by the HISDS, but demonstrated an improvement by post-intervention. These data indicate that the two measures used to assess self-concept in this study are measuring different constructs and that neither conceptualization clearly predicted whether participants responded to the songwriting intervention over time. Nevertheless, there was a general trend for self-concept scores to improve over time in those with positive trajectories. Tables 4 and 5 present an overview of the accompanying subjective wellbeing and subjective distress measures for both participant groups.
Table 1.
Participant demographic characteristics.
| Participant | Gender | Age | Education | Marital Status | Injury categorisation |
|---|---|---|---|---|---|
| Participant 1 | M | 17 | No higher than Year 10 | Single | C4 ASIA A complete paraplegia |
| Participant 2 | |||||
| M | 19 | Completed high school/ VCE | Single | T5 ASIA A complete paraplegia | |
| Participant 3 | F | 20 | Completed high school/ VCE | Single | T11/12 incomplete paraplegia |
| Participant 4 | M | 27 | Completed Apprenticeship / T.A.F.E. / College Diploma | Single | T3 ASIA A complete paraplegia |
| Participant 5 | |||||
| M | 29 | Completed Apprenticeship/ T.A.F.E./ College Diploma | Single | T12 ASIA D incomplete paraplegia | |
| Participant 6 | M | 37 | Post-graduate university degree | Married/ de facto | T4 incomplete paraplegia (tumour) |
| Participant 7 | M | 44 | Completed high school/ VCE | Married/ de facto | C4 ASIA A complete paraplegia |
| Participant 8 | M | 50 | Post-graduate university degree | Married/ de facto | T8 ASIA B incomplete paraplegia |
Note. All participants reported having been born in Australia.
Table 3.
Identity (Tennessee Self-Concept Scale and Head Injury Semantic Differential Scale) Scores at Pre-, Mid- and Post-intervention for Participants with Positive and Negative Trajectories.
| TSCS-2 | HISDS | |||||
|---|---|---|---|---|---|---|
| Participant | Pre | Mid | Post | Pre | Mid | Post |
| Positive Trajectories | ||||||
| Participant 3 | 33 | - | 52 | 106 | - | 121 |
| Participant 8 | 61 | 60 | 63 | 118 | 113 | 126 |
| Participant 6 | 40 | 49 | 59 | 91 | 94 | 116 |
| Negative Trajectories | ||||||
| Participant 1 | 48 | 35 | 42 | 80 | 69 | 114 |
| Participant 7 | 25 | 26 | 20 | 112 | 111 | 117 |
| Participant 4 | 20 | - | 24 | 113 | - | 61 |
Note. The TSCS-2 Total score is reflective of an individual’s overall self-concept and associated level of self-esteem. High scores (≥ 60T) are suggestive of a largely positive self-view, whereas low scores (≤30T) suggest more long-standing personal difficulties and conflicted self-view. HISDS Total possible scores range from 20 to 140, with higher scores indicative of a more positive self-concept.
Table 2.
Summary of key changes in direction and strength of change in outcome measures.
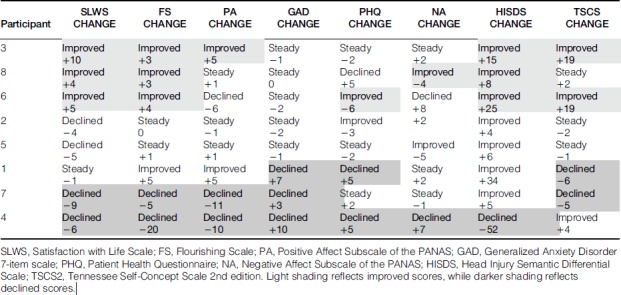 |
Table 4.
Subjective Wellbeing Scores on the Flourishing Scale, Satisfaction with Life Scale and Positive Affect Subscale of the PANAS at Pre-, Mid- and Post-intervention for Participants with Positive and Negative Trajectories.
| Flourishing Scale | Satisfaction with Life Scale | Positive Affect (PANAS) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Participant | Pre | Mid | Post | Pre | Mid | Post | Pre | Mid | Post |
| Positive Trajectories | |||||||||
| Participant 3 | 46 | - | 49 | 10 | - | 20 | 40 | - | 45 |
| Participant 8 | 48 | - | 51 | 20 | - | 24 | 36 | - | 37 |
| Participant 6 | 46 | - | 50 | 21 | 23 | 26 | 36 | 28 | 30 |
| Negative Trajectories | |||||||||
| Participant 1 | 43 | 31 | 48 | 10 | 5 | 9 | 25 | 21 | 30 |
| Participant 7 | 53 | 46 | 48 | 31 | 26 | 22 | 42 | 34 | 31 |
| Participant 4 | 51 | - | 31 | 22 | - | 16 | 42 | 34 | 31 |
Table 5.
Subjective Distress Scores on the Patient Health Questionnaire (PHQ-9), Generalized Anxiety Disorder Scale (GAD-7) and Negative Affect subscale of the PANAS at Pre-, Mid- and Post-intervention for Participants with Positive and Negative Trajectories.
| PHQ-9 | GAD-7 | Negative Affect (PANAS) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Participant | Pre | Mid | Post | Pre | Mid | Post | Pre | Mid | Post |
| Positive Trajectories | |||||||||
| Participant 3 | 6 | - | 4 | 1 | - | 0 | 20 | - | 22 |
| Participant 8 | 2 | 9 | 7 | 1 | 7 | 1 | 16 | 19 | 12 |
| Participant 6 | 9 | 9 | 3 | 6 | 10 | 4 | 22 | 31 | 30 |
| Negative Trajectories | |||||||||
| Participant 1 | 6 | 16 | 11 | 1 | 8 | 8 | 17 | 29 | 19 |
| Participant 7 | 1 | 4 | 3 | 0 | 4 | 3 | 18 | 23 | 17 |
| Participant 4 | 9 | - | 14 | 2 | - | 12 | 21 | - | 28 |
Demographic predictors of classification
Core demographic variables were examined to determine patterns of change in those showing both positive and negative trajectories (see Table 2). Gender could not be assessed in light of the lack of female representation in the sample (n=1). Age did not appear to differ systematically between the two trajectory types. Both groups were of mixed ages ranging from 17–50. Two-thirds of those with positive trajectories had undertaken a postgraduate university degree and were either married or in a defacto relationship, although it is unclear based on these participant numbers whether education or relationship status is reliably able to differentiate positive from negative trajectories.
All three participants showing positive trajectories had a comparatively less severe injury (incomplete paraplegia) than those with negative trajectories (complete paraplegia or tetraplegia). Those with negative trajectories were also on average longer post-injury as compared to those with positive trajectories.
While a content or qualitative analysis of song lyrics was beyond the scope of the current study, a brief inter-rater reliability exercise was undertaken to review the affective content of song lyrics within the past-, current-, and future-focused songs of those with positive and negative trajectories. This process, based on gross coding of positive, neutral or negative themes within the song lyrics, did not identify any reliable differentiation of those with positive and negative trajectories based on affective song content alone. However, visual inspection revealed that those with negative trajectories tended to express themes of grief, loss or regret. This is illustrated through some of the following lyrics:
“I wish I wasn’t here/ So you couldn’t see me in this mess/ I’m sorry for putting you through/ All the worry and stress” (Participant 1)
“I don’t let people see it, but my heart’s breaking/ Grieving for the dreams I’ve lost” (Participant 4)
“I look completely different, lost so much weight/ I feel disconnected from my body in this state” (Participant 7)
Interestingly, all three participants with negative trajectories also appeared to express some optimism about the future in the third, future-focused song:
“No one ever knows how things will be/ Stuff might happen, wait and see/ Take it how it comes, just my fate/ Happiness comes to those who wait” (Participant 1)
“I’ve got a new path to move on/ I have chosen what I want, and I won’t look back again/ Morning sunshine brings me charm” (Participant 4)
“It’s time to fight for a future that I like/ Everything is changing, but it’s gonna be alright” (Participant 7)
Those with positive trajectories also touched on themes of loss or grief in their songs, but additionally included lyrics that touched on gratitude for family and friends, perseverance, re-evaluation of future priorities, and optimism:
“Now I see, the me that I was meant to be” (Participant 3)
“ … I’m grateful for each day that I might never have had” (Participant 3)
“After being somewhere so dark/ I’m moving forward to a future that is full of light” (Participant 3)
“Time is the healer and I know I will survive/ I have lost some things, but gained good things too” (Participant 6)
“I don’t know who I am now, and how I’ll provide/ I’ve lost my motivation, but not my will to survive” (Participant 8)
“I know in time we’ll survive this ordeal” (Participant 8)
The above example lyrics note some of the themes emerging for those with positive and negative trajectories. A more rigorous examination of content across the three songs produced for all participants, alongside the additional measures collected which gauged the experience of ‘flow’ and meaning during the songwriting process, would be of value in future research to provide a stronger empirical basis for any genuine differences between participants with positive and negative trajectories.
Discussion
The current paper presents an analysis of the identity, subjective well-being, and distress measures completed by eight people with SCI undertaking a targeted 6-week therapeutic songwriting program during their inpatient rehabilitation program. Some participants, classified here as those with positive trajectories, demonstrated positive shifts in many of the relevant indices, whereas other participants tended toward negative shifts. No clear patterns in core demographic variables such as age, gender, education or relationship status served to differentiate these classifications as these attributes were mostly evenly distributed between groups (with the exception of the aforementioned gender bias in the sample overall, which hindered closer examination of gender roles).
With regard to the classification of those with positive and negative trajectories, it is of interest that the two participants who were under treatment with mood-altering medications displayed neutral trajectories. It is not within the scope of the current study to determine whether the presence of mood-altering medications may have ‘blunted’ any response to treatment, but the role of such medication in shaping treatment response is an area of note for future control comparison studies.
One key factor that did appear to differentiate the two evident trajectories was injury severity. All participants with positive trajectories were those with less severe injuries. The underlying contributors to this apparently reduced benefit for participants with more severe injuries are unclear. The severity of an injury and associated life role participation restrictions, the significant threat to identity resulting from this injury, and the expectation of longer duration of rehabilitation and reduced mobility may all have played a role in the experience of these participants in the sub-acute rehabilitation environment. These factors would align with prior research which has identified perceived health and mobility4, and the extent to which rehabilitation trajectories/progress matched expectations9 as predictors of post-injury adjustment. Severity of injury has also been found to be positively associated with suicidal ideation and attempts post-SCI.49
It should be noted that one participant with a negative trajectory had a significant pre-morbid history of psychopathology, primarily depression. This participant had extreme difficulty adjusting to the rehabilitation environment, and threatened to self-discharge on multiple occasions. Although prior literature has established that depression is a common comorbidity after a SCI (e.g.50), the role of pre-injury psychopathology as a potential predictor of post-injury adjustment remains less clear. However, it is reasonable to assume that those with pre-existing tendencies toward rumination or anxiety may face a greater challenge in adjusting to their changed circumstances after injury, particularly where this implies a significant threat to physical functioning.
The relationship between injury severity and treatment response warrants further investigation, and holds promise for the applicability of an identity-focused songwriting intervention for those with less severe injuries. Further research into factors such as age, gender, and education in larger samples is also recommended. Although coping style and stress response were outside of the scope of the current study, these have been proposed as predictors of SCI adjustment in prior research51,52 and would also be worthy of future exploration. Significant life events and changes in relationships post-injury were not directly evaluated in the current paper, although the impact of relationship breakdowns on injury adjustment is another area that warrants further investigation.
The current study has a number of limitations. Firstly, the research design precludes any causal inferences being drawn about the effects of the intervention. In the absence of a control condition, it is not possible to attribute any changes in core identity or well-being indices to the music therapy intervention. The small sample size also limits the generalisability of current findings. While recent studies have suggested emerging evidence for identity-focused therapeutic songwriting programs in facilitating post-injury adjustment (e.g.32,49), it is important that future such studies investigate the key causal factors that influence treatment response and in turn, shape post-injury adjustment.
Conclusion
The current paper presents an initial analysis of some of the possible contributors to post-injury adjustment for patients with SCI, and the potential efficacy of an identity-focused therapeutic songwriting program in addressing these. It should be noted that a more extensive comparison with control data is warranted to enable comparisons between those undergoing treatment as usual and those undergoing the songwriting program in the rehabilitation setting. The current study acted as a feasibility study to inform treatment response trends and the sensitivity of the identity and subjective well-being measures for ABI and SCI populations. It is hoped that the preliminary findings from this study can inform the development of future projects.
Identity remains an important driver of the post-injury identity rehabilitation focus, and one which merits attention in a subacute rehabilitation setting. More specifically, therapeutic songwriting holds promise as a means of promoting healthy adjustment and associated positive shifts in mood, well-being and quality of life. Injury severity should be further explored in future studies as a predictor of identity-specific treatment response. The individual narratives and identity trajectories of patients with SCI continue to be an important contributor to the development of effective post-injury therapies to promote healthy, reintegrated self-concept.
Acknowledgement
We would like to thank Young-Eun Claire Lee for assistance in data collection, and Peter New for advice on the draft manuscript.
Funding Statement
This work was supported by the Australian Research Council [grant number DP150100201].
Disclaimer statements
Contributors None.
Declaration of interest: None.
Conflicts of interest None.
Ethics approval The current project was approved by the Austin Health Human Research Ethics Committee (REF H2013/05038).
ORCID
Chantal Roddy http://orcid.org/0000-0001-5220-9226
Nikki Rickard http://orcid.org/0000-0002-4236-8538
Jeanette Tamplin http://orcid.org/0000-0002-3623-033X
Felicity Anne Baker http://orcid.org/0000-0003-2213-4467
References
- 1.Norton L. Spinal Cord Injury, Australia 2007–08. Canberra; 2010.
- 2.New PW, Baxter D, Farry A, Noonan VK.. Estimating the incidence and prevalence of traumatic spinal cord injury in Australia. Arch Phys Med Rehabil [Internet]. 2015;96(1):76–83. Available from: 10.1016/j.apmr.2014.08.013 [DOI] [PubMed] [Google Scholar]
- 3.Hammell KR. Psychosocial outcome following spinal cord injury. Paraplegia. 1994;32(11):771–9. [DOI] [PubMed] [Google Scholar]
- 4.Putzke JD, Richards JS, Hicken BL, DeVivo MJ.. Predictors of life satisfaction: A spinal cord injury cohort study. Arch Phys Med Rehabil. 2002;83(4):555–61. doi: 10.1053/apmr.2002.31173 [DOI] [PubMed] [Google Scholar]
- 5.Salter JE, Smith SD, Ethans KD.. Positive and negative affect in individuals with spinal cord injuries. 2013;(February 2012):252–6. [DOI] [PubMed] [Google Scholar]
- 6.Woolrich R, Kennedy P, Tasiemski T.. A preliminary psychometric evaluation of the Hospital Anxiety and Depression Scale (HADS) in 963 people living with a spinal cord injury. Psychol Health Med. 2006;11(1):80–90. doi: 10.1080/13548500500294211 [DOI] [PubMed] [Google Scholar]
- 7.Crisp R. The long-term adjustment of 60 persons with spinal cord injury. Aust Psychol. 1992;26(1):43–7. doi: 10.1080/00050069208257573 [DOI] [Google Scholar]
- 8.Bombardier CH, Kalpakjian CZ, Graves DE, Dyer JR, Tate DG, Fann JR.. Validity of the patient health questionnaire-9 in assessing major depressive disorder during inpatient spinal cord injury rehabilitation. Arch Phys Med Rehabil [Internet]. 2012;93(10):1838–45. Available from: 10.1016/j.apmr.2012.04.019 [DOI] [PubMed] [Google Scholar]
- 9.Cao Y, Dipiro ND, Xi J, Krause JS.. Unmet Expectations of Adjustment and Depressive Symptoms Among People With Chronic Traumatic Spinal Cord Injury. 2014;59(3):313–20. [DOI] [PubMed] [Google Scholar]
- 10.Migliorini C, Sinclair A, Brown D, Tonge B, New P.. Prevalence of mood disturbance in Australian adults with chronic spinal cord injury. Intern Med J. 2015;45(10):1014–9. doi: 10.1111/imj.12825 [DOI] [PubMed] [Google Scholar]
- 11.Cao Y, Massaro JF, Krause JS, Chen Y, Devivo MJ.. Suicide mortality after spinal cord injury in the United States: Injury cohorts analysis. Arch Phys Med Rehabil [Internet]. 2014;95(2):230–5. Available from: 10.1016/j.apmr.2013.10.007 [DOI] [PubMed] [Google Scholar]
- 12.Webster G, Daisley A, King N.. Relationship and family breakdown following acquired brain injury: the role of the rehabilitation team. Brain Inj. 1999;13(8):593–603. doi: 10.1080/026990599121331 [DOI] [PubMed] [Google Scholar]
- 13.Gerhart KA, Koziol-McLain J, Lowenstein SR, Whiteneck GG.. Quality of Life Following Spinal Cord Injury: Knowledge and Attitudes of Emergency Care Providers. Ann Emerg Med. 1994;23(4):807–12. doi: 10.1016/S0196-0644(94)70318-3 [DOI] [PubMed] [Google Scholar]
- 14.Migliorini CE, New PW, Tonge BJ.. Quality of life in adults with spinal cord injury living in the community. Spinal Cord [Internet]. 2011;49(3):365–70. Available from: http://www.ncbi.nlm.nih.gov/pubmed/20697422 doi: 10.1038/sc.2010.102 [DOI] [PubMed] [Google Scholar]
- 15.Bassett R, Martin Ginis K.. More than looking good: impact on quality of life moderates the relationship between functional body image and physical activity in men with SCI. Spinal Cord. 2009;47(3):252–6. doi: 10.1038/sc.2008.114 [DOI] [PubMed] [Google Scholar]
- 16.Kreuter M, Sullivan M, Dahllöf G, Siösteen A.. Partner relationships, functioning, mood and global quality of life in persons with spinal cord injury and traumatic brain injury. Spinal Cord. 1998;36(4):252–61. doi: 10.1038/sj.sc.3100592 [DOI] [PubMed] [Google Scholar]
- 17.Yoshida KK. Reshaping of self: a pendular reconstruction of self and identity among adults with traumatic spinal cord injury. Sociol Health Illn. 1993;15(2):217–45. doi: 10.1111/1467-9566.ep11346888 [DOI] [Google Scholar]
- 18.Samuel VM, Moses J, Smith H, Thorne K.. Spinal cord injury rehabilitation: the experience of women. Spinal Cord. 2007;45:758–764. doi: 10.1038/sj.sc.3102111 [DOI] [PubMed] [Google Scholar]
- 19.Nolan M. Masculinity lost: a systematic review of qualitative research on men with spinal cord injury. Spinal Cord. 2013;51(8):588–95. doi: 10.1038/sc.2013.22 [DOI] [PubMed] [Google Scholar]
- 20.Schopp LH, Good GE, Mazurek MO, Barker KB, Stucky RC.. Masculine role variables and outcomes among men with spinal cord injury. Disabil Rehabil. 2007;29(8):625–33. doi: 10.1080/09638280600902620 [DOI] [PubMed] [Google Scholar]
- 21.Charmaz K. Loss of self: a fundamental form of suffering in the chronically ill. Sociol Health Illn. 1983;5(2):168–95. doi: 10.1111/1467-9566.ep10491512 [DOI] [PubMed] [Google Scholar]
- 22.Nochi M. Reconstructing self-narratives in coping with traumatic brain injury. Soc Sci Med. 2000;51:1795–804. doi: 10.1016/S0277-9536(00)00111-8 [DOI] [PubMed] [Google Scholar]
- 23.Lennon A, Bramham J, Carroll A, McElligott J, Carton S, Waldron B, et al A qualitative exploration of how individuals reconstruct their sense of self following acquired brain injury in comparison with spinal cord injury. Brain Inj. 2014;28(1):27–37. doi: 10.3109/02699052.2013.848378 [DOI] [PubMed] [Google Scholar]
- 24.Sigurdardottir S, Andelic N, Roe C, Schanke AK.. Identifying longitudinal trajectories of emotional distress symptoms 5 years after traumatic brain injury. Brain Inj [Internet]. 2014;9052(12):1–9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25029224 [DOI] [PubMed] [Google Scholar]
- 25.Rogan C, Fortune DG, Prentice G.. Post-traumatic growth, illness perceptions and coping in people with acquired brain injury. Neuropsychol Rehabil [Internet]. 2013;23(5):639–57. Available from: http://www.ncbi.nlm.nih.gov/pubmed/23701407 doi: 10.1080/09602011.2013.799076 [DOI] [PubMed] [Google Scholar]
- 26.Kalpakjian CZ, Mccullumsmith CB, Fann JR, Richards JS, Stoelb BL, Heinemann AW, et al Post-traumatic growth following spinal cord injury. J Spinal Cord Med. 2014;37(2):218–25. doi: 10.1179/2045772313Y.0000000169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gendreau A, de la Sablonnière R.. The cognitive process of identity reconstruction after the onset of a neurological disability. Disabil Rehabil [Internet]. 2014;36(19):1608–17. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24286233 doi: 10.3109/09638288.2013.859749 [DOI] [PubMed] [Google Scholar]
- 28.Baker FA, Kennelly J, Tamplin J.. Themes in Songs Written by Patients with Traumatic Brain Injury: Differences Across the Lifespan. Aust J Music Ther. 2006;16:25–42. [DOI] [PubMed] [Google Scholar]
- 29.Baker FA. Therapeutic songwriting: Developments in theory, methods, and practice. London: Palgrave McMillan; 2015. [Google Scholar]
- 30.Glassman LR. Music therapy and bibliotherapy in the rehabilitation of traumatic brain injury: A case study. Arts Psychother. 1991;18:149–56. doi: 10.1016/0197-4556(91)90022-3 [DOI] [Google Scholar]
- 31.Baker FA, Rickard N, Tamplin J, Roddy C.. Flow and meaningfulness as mechanisms of change in self-concept and wellbeing following a songwriting intervention for people in the early phase of neurorehabilitation. Front Hum Neurosci. 2015;9:299–399. doi: 10.3389/fnhum.2015.00299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tyerman A, Humphrey M.. Changes in Self-Concept Following Severe Head Injury. Int J Rehabil Res. 1984;7(1):11–23. doi: 10.1097/00004356-198403000-00002 [DOI] [PubMed] [Google Scholar]
- 33.Fitts WH, Warren WL.. Tennessee Self-Concept Scale (2nd ed.). Los Angeles: Western Psychological Services; 1996. [Google Scholar]
- 34.Ellis-Hill CS, Horn S.. Change in identity and self-concept: a new theoretical approach to recovery following a stroke. Clin Rehabil. 2000;14(3):279–87. doi: 10.1191/026921500671231410 [DOI] [PubMed] [Google Scholar]
- 35.Webb MA, Emery LJ.. Self-Identity in an Adolescent a Decade after Spinal Cord Injury. Occup Ther Heal Care. 2009;23(4):267–87. doi: 10.3109/07380570903214796 [DOI] [PubMed] [Google Scholar]
- 36.Diener E, Emmons RA, Larsen RJ, Griffin S.. The Satisfaction with Life Scale. J Pers Assess. 1985;49(1):71–5. doi: 10.1207/s15327752jpa4901_13 [DOI] [PubMed] [Google Scholar]
- 37.Vassar M. A note on the score reliability for the satisfaction with life scale: an RG study. Soc Indic Res. 2008;86(1):47–57. doi: 10.1007/s11205-007-9113-7 [DOI] [Google Scholar]
- 38.Corrigan JD, Kolakowsky-Hayner S, Wright J, Bellon K, Carufel P.. The Satisfaction With Life Scale. J Head Trauma Rehabil [Internet]. 2013;28(6):489–91. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16367493 doi: 10.1097/HTR.0000000000000004 [DOI] [PubMed] [Google Scholar]
- 39.Diener E, Wirtz D, Tov W, Kim-Prieto C, Choi DW, Oishi S, et al New well-being measures: Short scales to assess flourishing and positive and negative feelings. Soc Indic Res. 2010;97(2):143–56. doi: 10.1007/s11205-009-9493-y [DOI] [Google Scholar]
- 40.Hone L, Jarden A, Schofield G.. Psychometric Properties of the Flourishing Scale in a New Zealand Sample. Soc Indic Res. 2014;119:1031–45. doi: 10.1007/s11205-013-0501-x [DOI] [Google Scholar]
- 41.Spitzer RL, Kroenke K, Williams JBW, Löwe B.. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7. doi: 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- 42.Kroenke K, Spitzer RL.. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Ann. 2002;32:509–21. doi: 10.3928/0048-5713-20020901-06 [DOI] [Google Scholar]
- 43.Löwe B, Decker O, Müller S, Brähler E, Schellberg D, Herzog W, et al Validation and standardization of the Generalized Anxiety Disorder Screener (GAD-7) in the general population. Med Care. 2008;46(3):266–74. doi: 10.1097/MLR.0b013e318160d093 [DOI] [PubMed] [Google Scholar]
- 44.Fann JR, Bombardier CH, Dikmen S, Esselman P, Warms CA, Pelzer E, et al Validity of the Patient Health Questionnaire-9 in assessing depression following traumatic brain injury. J Head Trauma Rehabil [Internet]. 2005;20(6):501–11. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16304487 doi: 10.1097/00001199-200511000-00003 [DOI] [PubMed] [Google Scholar]
- 45.Watson D, Clark LA, Tellegen A.. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54(6):1063–70. doi: 10.1037/0022-3514.54.6.1063 [DOI] [PubMed] [Google Scholar]
- 46.Crawford JR, Henry JD.. The Positive and Negative Affect Schedule (PANAS): Construct validity, measurement properties and normative data in a large non-clinical sample Br J Clin Psychol. 2004;43:245–65. doi: 10.1348/0144665031752934 [DOI] [PubMed] [Google Scholar]
- 47.Baker FA, Tamplin J, MacDonald RAR, Ponsford J, Roddy C, Lee C, et al Exploring the Self through Songwriting: An Analysis of Songs Composed by People with Acquired Neurodisability in an Inpatient Rehabilitation Program. J Music Ther [Internet]. 2017;54(1):35–54. Available from: https://academic.oup.com/jmt/article/2918652/Exploring doi: 10.1093/jmt/thw018 [DOI] [PubMed] [Google Scholar]
- 48.Tamplin J, Baker FA, Macdonald RAR, Roddy C, Rickard NS.. A theoretical framework and therapeutic songwriting protocol to promote integration of self-concept in people with acquired neurological injuries. Nord J Music Ther [Internet]. 2015;(March):1–23. Available from: http://www.tandfonline.com/doi/abs/10.1080/08098131.2015.1011208 [Google Scholar]
- 49.McCullumsmith CB, Kalpakjian CZ, Richards JS, Forchheimer M, Heinemann AW, Richardson EJ, et al. Novel Risk Factors Associated With Current Suicidal Ideation and Lifetime Suicide Attempts in Individuals With Spinal Cord Injury. Arch Phys Med Rehabil [Internet]. 2015. [cited 2015 Aug 27];96:799–808. Available from: http://ac.els-cdn.com.ezproxy.lib.monash.edu.au/S0003999315000386/1-s2.0-S0003999315000386-main.pdf?_tid=975c4c44-4c66-11e5-ab51-00000aab0f26&acdnat=1440644101_4c3b9ec74097e2e8b80377820060faaa doi: 10.1016/j.apmr.2014.12.017 [DOI] [PubMed] [Google Scholar]
- 50.Elliott TR, Witty TE, Herrick S, Hoffman JT.. Negotiating reality after physical loss: hope, depression, and disability. J Pers Soc Psychol. 1991;61(4):608–13. doi: 10.1037/0022-3514.61.4.608 [DOI] [PubMed] [Google Scholar]
- 51.Barone SH, Waters K.. Coping and Adaptation in Adults Living with Spinal Cord Injury. J Neurosci Nurs. 2012;44(5):271–83. doi: 10.1097/JNN.0b013e3182666203 [DOI] [PubMed] [Google Scholar]
- 52.Livneh H, Martz E.. Coping Strategies and Resources as Predictors of Psychosocial Adaptation Among People With Spinal Cord Injury. Rehabil Psychol. 2014;59(3):329–39. doi: 10.1037/a0036733 [DOI] [PubMed] [Google Scholar]


