Abstract
The objective of the current study was to characterize the association between dating violence victimization and dispositional aggression in predicting nonsuicidal self-injury (NSSI) among psychiatrically hospitalized male and female adolescents. One hundred fifty-five adolescents (ages 13–17) and their parents completed the Schedule for Affective Disorders and Schizophrenia for School-Age Children clinical interview to assess NSSI and child abuse; adolescents completed self-report measures of aggression and dating violence victimization (verbal, physical, and sexual). Dating violence victimization and NSSI were found to be highly prevalent among both males and females in this psychiatric inpatient sample. Two moderational models were supported, wherein dating violence was associated with NSSI in the context of elevated trait anger in males and indirect aggression in females. Findings suggest that helping victims of dating violence acquire skills to address certain forms of dispositional aggression may attenuate NSSI.
Nonsuicidal self-injurious (NSSI) behavior is quite common among teenagers. A recent study of ninth and tenth graders found that 46% engaged in at least one self-injurious behavior within the past year, including 14% who had cut or carved skin and 12% who had burned skin (Lloyd-Richardson, Perrine, Dierker, & Kelley, 2007). Rates in adolescent inpatient settings are even higher, with approximately 40% to 77% of youth reporting NSSI (Conterio, Lader, & Bloom, 1998; Darche, 1990; DiClemente, Ponton, & Hartley, 1991; Nock & Prinstein, 2004). Numerous clinical and non-clinical studies suggest that early traumas (e.g., sexual assault, childhood abuse) are highly correlated with NSSI in adolescents (Dube et al., 2001; Glassman, Weierich, Hooley, Deliberto, & Nock, 2007; Weismoore & Esposito-Smythers, 2010). One trauma not yet explored in relation to adolescent NSSI is dating violence (DV).
DV includes psychological or emotional violence, such as controlling behaviors or jealousy; physical violence, such as hitting or punching; and sexual violence, such as nonconsensual sexual activity and rape. Although DV prevalence can vary, with certain subpopulations of youth disproportionately burdened, DV remains a widespread public health issue. It occurs in heterosexual and same-sex relationships and cuts across racial/ethnic and socioeconomic lines (Halpern, Young, Waller, Martin, & Kupper, 2004; Spriggs, Halpern, Herring, & Schoenback, 2009). Up to 45% of adolescent girls and 43% of adolescent boys in a community sample report having been victims of violence by a dating partner (O’Keefe & Treister, 1998). Rates may be even higher in clinical samples (e.g., youth with conduct/oppositional defiant disorders), as these adolescents may select aggressive dating partners (Kim & Capaldi, 2004). Indeed, as shown in our previous work with this sample of psychiatrically hospitalized adolescents, 77% of teens who had initiated dating reported psychological, physical, or sexual abuse by a dating partner over the past year (Rizzo, Esposito-Smythers, Spirito, & Thompson, 2010).
DV is not only a prevalent public health problem, but is linked to a myriad of negative outcomes. Our team has found that psychiatrically hospitalized adolescents with a history of any DV report elevated rates of major depressive disorder. Victims of severe DV (physical/sexual victimization) have a more pernicious clinical picture, including relatively high rates of posttraumatic stress disorder, alcohol use disorder, comorbid externalizing and internalizing disorders, and elevated cognitive distortions (Rizzo et al., 2010). Given the relevance of DV to mental health problems, an important next step is to examine the relationship between DV and NSSI, a frequent mental health problem reported among psychiatrically hospitalized adolescents.
A small number of studies have examined the link between partner violence and NSSI with adults. Levesque, Lafontaine, Bureau, Cloutier, and Dandurand (2010) examined intimate partner violence and NSSI in a sample of university students (ages 18–25). In their study, a history of intimate partner violence emerged as a significant predictor of recent NSSI behaviors in both men and women. Sansone, Chu, and Wiederman (2007) examined this same relationship in a clinical sample of psychiatrically hospitalized females (ages 18–57). They found that women with histories of intimate partner violence were more likely to engage in NSSI behaviors, even after controlling for age and a history of being married. These studies provide preliminary evidence of an association between violence among dating or romantic partners and NSSI.
Although a relation between adolescent DV victimization and NSSI is probable based on theory, not all youth who report DV will engage in NSSI. Dispositional aggression may influence the nature of this relationship. Dispositional aggression includes a propensity to engage in behavioral forms of aggression, such as physical fighting, verbal attacks, and indirect actions such as spreading rumors. It can also include a propensity to experience psychological forms of aggression such as elevated anger (affective component) and hostility (cognitive component; Ramírez & Andreu, 2006). A fair amount of research suggests that DV victimization may be linked to dispositional aggression, as physical fighting, gun-carrying behavior (Kim-Godwin, Clements, McCuiston, & Fox, 2009), and anger (Follingstad, Wright, Lloyd, & Sebastian, 1991; Swan, Gambone, Fields, Sullivan, & Snow, 2005) frequently co-occur with DV. Indeed, anger problems are associated with an increased risk of being both the victim and perpetrator of intimate partner violence (Korman et al., 2008; Leadbeater, Banister, Ellis, & Yeung, 2008; Whitaker, Haileyesus, Swahn, & Saltzman, 2007). Although it is not known whether there is a causal relationship between DV and dispositional aggression, the data do suggest that DV and aggression are interrelated.
The link between DV victimization and dispositional aggression is relevant to studies of NSSI for a number of reasons. According to several theoretical models of NSSI, adolescents use NSSI for affect regulation purposes (see Messer & Fremouw, 2008, for a review). For example, Chapman, Gratz, and Brown (2006) propose an experiential avoidance model, which suggests that NSSI is used as a means to escape from and/or reduce strong aversive emotions resulting from negative events, such as interpersonal traumas. Similarly, a primary component in the functional model of NSSI proposed by Nock and Prinstein (2004) is that NSSI is initiated and maintained via automatic negative reinforcement (i.e., reduction of negative mood states). Based on these theories, adolescent victims of DV who are predisposed to anger and hostility may engage in NSSI as a means to manage these strong aversive internalized emotions. Indeed, rates of NSSI have been found to be elevated among adolescents who report anger problems (Laye-Gindhu & Schonert-Reichl, 2005). Darche (1990) also found greater anger and hostility among adolescents who do versus do not self-injure. However, NSSI may be less likely among teens predisposed to engaging in aggressive behavior (physical, verbal, and indirect) because acting on aggressive impulses may serve as an externalized outlet for negative emotions.
In summary, DV victimization is a salient interpersonal trauma for adolescents and thus a likely risk factor for NSSI. Although studied cursorily in adults, to our knowledge, research has not been conducted to examine the association between DV victimization and NSSI in adolescent clinical samples. Dispositional aggression, both psychological and physical forms, has been found to co-occur with DV. This co-occurrence is relevant to NSSI for two important reasons. First, psychological forms of aggression may promote NSSI behaviors and amplify the relationship between DV and NSSI, as anger and hostility are strong aversive emotions that adolescents may wish to escape from through self-injury. Second, behavioral forms of aggression may reduce NSSI and attenuate the relationship between DV and NSSI, as physical, verbal, and indirect acts of aggression may serve as outlets for stressors such as DV. The purpose of the present study was to examine this association between DV and NSSI in a clinical sample of adolescents as well as to examine whether psychological and behavioral aspects of dispositional aggression moderate this relationship.
Given that there are known gender differences in the consequences of adolescent DV, with adolescent girls reporting more severe physical and emotional reactions to the violence (Molidor & Tolman, 1998), we tested our hypotheses for males and females separately to establish whether or not our findings would be stable across gender. Furthermore, we provide a conservative test of our hypotheses by controlling for a history of childhood abuse. Controlling for abuse history is particularly important as numerous studies have shown that childhood abuse can predispose adolescents to both NSSI (Boudewyn & Liem, 1995; Herpertz, 1995; Lehrer, Buka, Gortmaker, & Shrier, 2006; Romans, Martin, Anderson, Herbison, & Mullen, 1995; Van der Kolk, Perry, & Herman, 1991; Winchel & Stanley, 1991; Yeo & Yeo, 1993; Zuckerbrot & Jenson, 2006) and DV victimization (Coffey, Leitenberg, Henning, Bennett, & Jankowski, 1996; Lehrer et al., 2006; O’Keefe, 1998; Wolfe, Scott, Wekerle, & Pittman, 2001).
METHOD
Participants
Two hundred sixty-three adolescents psychiatrically hospitalized on an inpatient unit of a regional children’s psychiatric hospital in southern New England were invited to participate in a larger parent research study examining cognitive influences on psychopathology and suicidality. This hospital serves all patients regardless of insurance status. According to state census tract data, socioeconomic status (SES) for the population served at this facility includes 16% high SES, 39% middle SES, 15% low SES, and 12% poverty conditions. Adolescents were eligible for participation if they (1) were 13 to 17 years old, (2) lived with their parents/primary caregivers (who legally had custody) for the past 3 months, (3) were not actively psychotic, and (4) spoke English. Adolescents with a developmental disability or an IQ < 70 were excluded.
Parental consent and assent were obtained for 201 adolescents (76%). Of these, a subsample of 155 participants (mean age = 15.1, SD = 1.3; 76% female), who had initiated dating by the time of the assessment and thus completed the dating related assessments, were retained for the current analyses. The median family income of study participants was $50,001–60,000; 21% of participant’s families reported an annual income of $20,000 or below. Self-reported race of the sample was 81% Caucasian/European American, 11% Hispanic, 3% Asian American, 3% African American, and 2% mixed ethnicity-other. There were no significant age, gender, race, or ethnic differences between the 46 youths who were enrolled in the study, but not included in analyses, and 155 youths who were included in analyses.
Measures
Nonsuicidal Self-Injury.
NSSI was assessed using the depression module of the Schedule for Affective Disorders and Schizophrenia for School-Age Children—Present Episode (K-SADS-P; Chambers et al., 1985). The K-SADS-P is a semi-structured diagnostic interview that provides a reliable and valid measurement of DSM–IV diagnoses in children and adolescents as well as suicidal and nonsuicidal self-injurious behaviors. NSSI as defined in the K-SADS-P refers to self-mutilation or other physical acts performed without the intent of killing oneself. Participants were asked to indicate whether they tried to hurt themselves, such as burned self with matches or candles, scratched self with needles or knife or nails, put hot pennies on the skin, or another method of self-injury. They were then asked when and how often they engaged in this type of behavior in the past year. Interviewers were trained to distinguish responses that involved deliberate, self-inflicted destruction of body tissue without suicidal intent from responses involving unintentional injury and suicidality. The K-SADS-P NSSI rating scales measures a continuum of NSSI experiences including no NSSI, thoughts of NSSI, NSSI behaviors of increasing frequency, and medically severe NSSI. The rating scale intentionally conflates NSSI presence, frequency, and medical severity to reflect the range of experiences observed in clinical settings in order of increasing “clinical severity.” The adolescent and parent consensus rating was used in analyses (1 = not present, 2 = only thoughts of self-harm, 3 = 1–2 times per year, 4 = 4–11 times per year, 5 = 12+ times per year, 6 = at least one nonaccidental act which left permanent substantial functional deficit).
Childhood Caregiver Abuse.
Childhood physical and sexual abuse perpetrated by a caregiver was assessed using the Schedule for Affective Disorders and Schizophrenia for School-Age Children—Present and Lifetime Version (K-SADS-PL; Kaufman et al., 1997). Participants were coded for whether they were ever a victim of physical abuse or sexual abuse as defined in the K-SADS-PL Posttraumatic Stress Disorder screen. Adolescents were asked to indicate whether they had been physically abused, defined as bruises sustained on more than one occasion or one or more serious injuries perpetrated by a caretaker, or sexually abused, defined as isolated or repeated incidents of genital fondling, oral sex, or vaginal or anal penetration, perpetrated by a caretaker. Adolescent participants and their parent/guardian were asked to recount whether, at what age, and by whom, the adolescent had experienced any of these traumatic events.
Dating Violence.
DV victimization over the past year was assessed using the Conflict in Adolescent Dating Relationships Inventory (CADRI; Wolfe et al., 2001). The CADRI is a 35-item measure completed by teens in reference to actual conflict or disagreement with a current or recent dating partner. It assesses abuse perpetration and victimization. Sample items include “I slapped him or pulled his hair” and “I deliberately tried to frighten her.” For the purposes of this study, only victimization was assessed. Response choices (0–3) are never, seldom (this has happened only 1–2 times), sometimes (this has happened about 3–5 times), and often (this has happened six times or more). Adolescents were considered to have experienced emotional, physical, or sexual abuse if they reported at least one indicator of that type of violence as measured by the CADRI. The CADRI has strong internal consistency (total α = .83) and 2-week test-retest reliability, r = .68, p < .01 (Wolfe et al., 2001), as well as acceptable partner agreement (r = .64, p < .01; Wolfe, Crooks, Lee, McIntyre-Smith, & Jaffe, 2003). Internal consistency for our sample was good, α = .91.
Dispositional Aggression.
The Aggression Questionnaire (AQ; Buss & Warren, 2000) is a widely used self-report measure of trait aggression. This 34-item instrument consists of the five dispositional subtraits of aggression, including psychological (anger, hostility) and behavioral (physical, verbal, indirect) aggression. Participants rated all items on a 5-point scale anchored at 1 (extremely uncharacteristic of me) and 5 (extremely characteristic of me). Buss and Warren (2000) report good to moderate reliability. Internal consistency for our sample was acceptable: physical aggression (α = .90), verbal aggression (α = .82), anger (α = .74), hostility (α = .88), indirect aggression (α = .77), and the total scale (α = .95).
Procedures
Eligible adolescents and their parents/guardians were approached for recruitment by a research assistant after family meetings or during family visits on the adolescent inpatient unit. After parent/guardian consent and adolescent assent was obtained, adolescents and their parent/guardian were separately administered the assessments, while the adolescent was hospitalized on the inpatient unit. With the exception of the diagnostic interview that was conducted by trained masters and doctoral-level clinicians, a bachelor-level research assistant administered the battery. As compensation for participation, parents were given $50 and adolescents were given four movie tickets. This research was approved by both the university and hospital internal review boards.
RESULTS
Preliminary Analyses
The NSSI variable was examined for skewness and acceptable normality was found (skew = ‒.179, SE = .177). Table 1 presents participant characteristics, by gender, including the prevalence of DV victimization, NSSI, and childhood caregiver abuse; 77% of psychiatrically hospitalized adolescents reported a history of DV victimization in the past year, 67% reported engaging in NSSI (frequency score of 3 or more) over the past year.
TABLE 1.
Participant Characteristics (n = 155)
| M (SD) or n (%) | |||
|---|---|---|---|
| Variable | Males | Females | Total |
| Mean age in years Race/Ethnicity |
15.6 (1.1) | 14.5 (1.3) | 15.1 (1.3) |
| Race/Ethnicity | |||
| Caucasian | 28 (88) | 80 (80) | 108 (81) |
| African American | 0 (0) | 4 (3) | 4 (3) |
| Latino/Hispanic | 2 (6) | 12 (12) | 14 (11) |
| Asian | 1 (3) | 3 (3) | 4 (3) |
| Other | 3 (9) | 14 (12) | 3 (2) |
| Dating violence victimizationa | 26 (70) | 94 (80) | 120 (77) |
| Childhood caregiver abuseb | 6 (16) | 43 (57) | 49 (32) |
| Nonsuicidal self-injury (NSSI)b | 16 (43) | 88 (75) | 104 (67) |
Dating violence and NSSI are measured for the past year.
Females reported higher levels of NSSI and abuse than males.
A series of zero-order correlations, one-way analyses of variance (ANOVA), chi-square, and two-tailed t tests were conducted to examine associations between study variables. The main study constructs did not differ by age, race, or ethnicity. However, female participants were more likely than male participants to report trait hostility, t(155) = 2.31, p < .05, a history of childhood caregiver abuse, χ2 = 5.33, p < .05, and frequent NSSI, t(155) = 3.07, p < .01. Given these findings and the gender differences in the consequences of DV reported in the literature, we conducted our analyses for males and females separately.
The correlations between predictor and criterion variables by gender are presented in Table 2. Results of correlational analyses revealed that trait physical aggression was positively correlated with NSSI for males, whereas the propensity for anger, hostility, and verbal aggression were positively correlated with NSSI for girls. DV victimization was positively associated with trait hostility and verbal aggression among males and propensity for physical aggression among females.
TABLE 2.
Pearson and Point-Biserial Correlations between Predictor and Criterion Variables for Males and Females
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | Mean (Range) or n (%) | SD | |
|---|---|---|---|---|---|---|---|---|---|
| Males (n = 37) | |||||||||
| 1. Nonsuicidal self-injury | – | 2.5 (1–5) | 1.8 | ||||||
| 2. Anger | .16 | – | 51.8 (27–73 | 10.8 | |||||
| 3. Hostility | .22 | .65** | – | 47.8 (26–72) | 13.14 | ||||
| 4. Indirect aggression | .21 | .75** | .75** | – | 50.7 (30–74) | 11.5 | |||
| 5. Physical aggression | .31* | .66** | .42** | .49** | – | 51.1 (29–76) | 11.5 | ||
| 6. Verbal aggression | .19 | .60** | .76** | .63** | .48** | – | 53.6 (30–72) | 10.1 | |
| 7. Childhood caregiver abuse | .18 | .07 | .17 | .02 | −.03 | −.02 | – | – | – |
| 8. Dating violence victimization | .14 | .20 | .33* | .19 | −.05 | .35** | .27 | – | – |
| Females (n = 118) | |||||||||
| 1. Nonsuicidal self-injury | – | 3.5 (1–5) | 1.6 | ||||||
| 2. Anger | .26** | – | 53.6 (32–79) | 11.9 | |||||
| 3. Hostility | .29** | .67** | – | 53.4 (26–80) | 12.9 | ||||
| 4. Indirect aggression | .14 | .70** | .63** | – | 50.6 (25–76) | 11.2 | |||
| 5. Physical aggression | .10 | .68** | .48** | .73** | – | 50.8 (32–80) | 11.2 | ||
| 6. Verbal aggression | .22* | .74** | .58** | .67** | .64** | – | 54.4 (24–75) | 11.4 | |
| 7. Childhood caregiverabuse | .10 | .11 | .07 | .13 | .22** | .16 | – | – | – |
| 8. Dating violence victimization | .15 | .10 | .11 | .13 | .25** | .17 | −.01 | – | – |
p < .05;
p < .01.
DV Victimization and NSSI
In the full sample, DV victimization was positively associated with NSSI, M = 3.38 vs. 2.73, t(155) = −1.98, p < .05. When males and females were examined separately, findings were nonsignificant, females: M = 3.60 vs. 3.00, t(118) = −1.62, p = .09; males: M = 2.67 vs. 2.10, t(37) = −0.85, ns. Given that the NSSI variable measures a continuum of NSSI experiences that include no NSSI, thoughts of NSSI, NSSI behaviors of increasing frequency, and medically severe NSSI, along with the fact that predictors of NSSI presence may vary from predictors of frequency and medical severity, we decided to further explore the relationship between DV victimization and NSSI frequency alone. To do this, the NSSI variable was re-coded to compare frequent NSSI (12 or more times per year) from no to infrequent NSSI. In these analyses, a notable relationship emerged between DV victimization and NSSI for females; 12.5% of females without DV reported engaging in NSSI more than 12 times in the past year, whereas 45.7% of DV victims reported this frequency of NSSI behaviors, χ2(2, n = 118) = 8.88, p < .01. For males, 20% of non-DV victims engaged in frequent NSSI compared with 33% of victims, χ2(2, n = 37) = 0.62, ns.
Hierarchical Regression: Dispositional Aggression, DV Victimization, and NSSI
Hierarchical regression models were computed to determine whether psychological and behavioral forms of trait aggression moderated the association between DV victimization and the continuum of NSSI experiences. Models were run separately for males and females. The main effects of the five aggression variables and their interactions with DV were all examined in one model which allowed us to test the contribution of each aggression variable (psychological vs. behavioral subtraits) and their interaction with DV, while other relevant terms are accounted for in the models. In the first round of analyses, relationships were examined without caregiver abuse in the model. In the second round of analyses, caregiver abuse was added as a covariate. In all cases, the addition of caregiver abuse did not change the outcomes. Given the theoretical importance of accounting for the abuse variable in our analyses, findings reported here are from the second set of analysis that accounted for abuse. Predictor and interaction terms were centered as recommended by Aiken and West (1991).
Dispositional Aggression: Psychological.
In males, trait anger was found positively associated with NSSI frequency, while accounting for DV victimization, childhood caregiver abuse, and other forms of aggression. Trait anger was also found to significantly interact with DV victimization to predict NSSI frequency. The significant interaction predicting NSSI frequency was interpreted using a nonparametric graph. We chose to represent the data with nonparametric graphing techniques because they make fewer assumptions about the relationships between variables (e.g., linear, quadratic, etc.). As shown in Figure 1, males with histories of DV victimization who reported a tendency to experience elevated levels of anger were more likely to report engaging in NSSI. In contrast, trait hostility was not positivity related to NSSI frequency. The interaction effect with DV was also nonsignificant. In females, the main effects for trait anger and hostility on NSSI frequency were all nonsignificant, as were the interactions effects (Table 3).
Figure 1.
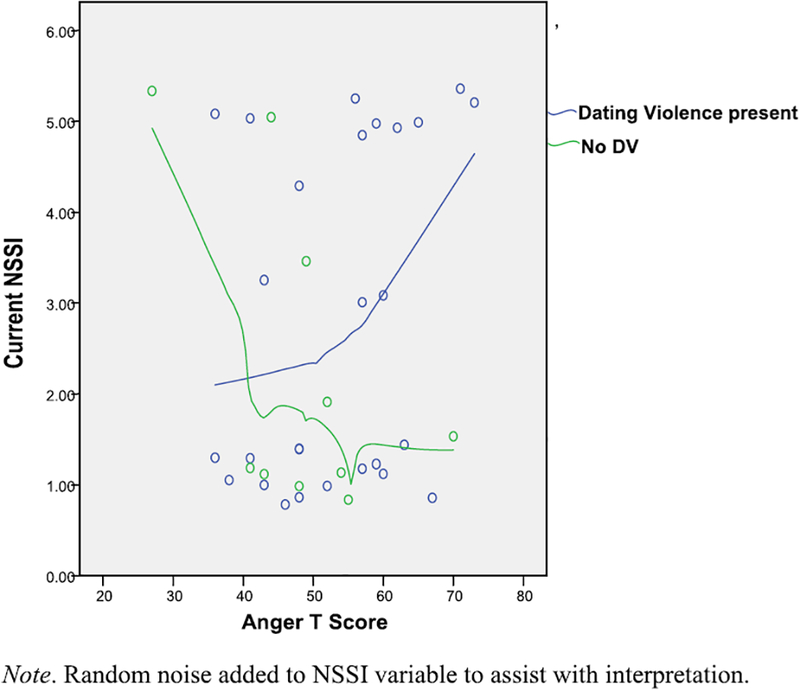
Nonparametric graph exploring the relationship between dating violence status, trait anger, and nonsuicidal self-injury (NSSI) among males.
TABLE 3.
Linear Regression Analyses Predicting Nonsuicidal Self-Injury as a Function of Dispositional Aggression Subtraits and Their Interaction with Dating Violence Victimization (n = 155)
| Step | Variable | β | t | ΔR2 for step | ΔF for step |
|---|---|---|---|---|---|
| Males | |||||
| 1 | Childhood caregiver abuse | .29 | 1.45 | .16 | 0.80 |
| Dating violence victimization | .49 | 2.13 | |||
| Hostility | .47 | 0.90 | |||
| Anger | −1.28 | −2.76* | |||
| Indirect aggression | −.29 | −0.43 | |||
| Physical aggression | .98 | 1.01 | |||
| Verbal aggression | .28 | 0.52 | |||
| 2 | Hostility × DV | −.77 | −1.43 | .18 | 1.32 |
| Anger × DV | 1.30 | 2.59* | |||
| Indirect aggression × DV | .67 | 1.10 | |||
| Physical aggression × DV | −.87 | −0.89 | |||
| Verbal aggression × DV | −.15 | −0.14 | |||
| Females | |||||
| 1 | Childhood caregiver abuse | .02 | 0.16 | .10 | 1.79 |
| Dating violence victimization | .04 | 0.37 | |||
| Hostility | .17 | 0.70 | |||
| Anger | .05 | 0.13 | |||
| Indirect aggression | −.99 | −2.64* | |||
| Physical aggression | .65 | 1.73 | |||
| Verbal aggression | .06 | 0.15 | |||
| 2 | Hostility × DV | .01 | 0.03 | .06 | 1.42 |
| Anger × DV | .10 | 0.29 | |||
| Indirect aggression × DV | .88 | 2.38* | |||
| Physical aggression × DV | −.66 | −1.87 | |||
| Verbal aggression × DV | .02 | 0.05 |
DV, dating violence victimization.
p < .05; **p < .01.
Dispositional Aggression: Behavioral.
In males, there were no main effects for indirect aggression, physical aggression, or verbal aggression on NSSI frequency. Similarly, none of the interaction terms were significant. In females, there were also no main effects for indirect aggression, physical aggression, or verbal aggression on NSSI frequency. However, trait indirect aggression interacted with DV victimization to predict NSSI frequency. The significant interaction predicting NSSI frequency was interpreted using a nonparametric graph. As shown in Figure 2, females with histories of DV victimization who reported a propensity for elevated levels of indirect aggression were more likely to report engaging in NSSI (Table 3).
Figure 2.
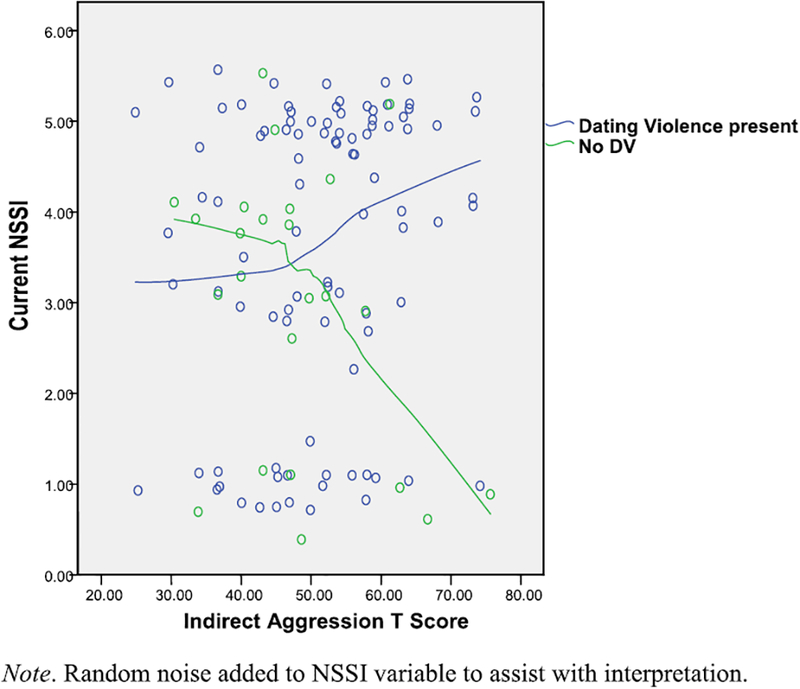
Nonparametric graph exploring the relationship between dating violence status, propensity for indirect aggression, and nonsuicidal self-injury (NSSI) among females.
DISCUSSION
In the present study we examined the association between DV victimization and NSSI, as well as behavioral and psychological forms of dispositional aggression as moderators of this association in a sample of psychiatrically hospitalized adolescents. A stringent test of these associations was conducted by examining the relationships for males and females separately and by controlling for a history of childhood caregiver abuse in study analyses. Notable was the high prevalence rate of DV victimization (77%) and NSSI (67%) reported by adolescents over the course of the last year. These rates are substantially higher than those reported in adolescent community samples (Lloyd-Richardson et al., 2007; O’Keefe & Treister, 1998) and reinforce the importance of this area of study, particularly in clinical samples of adolescents. Consistent with the literature (Andover, Primack, Gibb, & Pepper, 2010), in this psychiatrically hospitalized sample, females reported more NSSI than males. Additionally, there were no gender differences in rates of DV victimization. Aside from our own work, there are no studies of DV in psychiatrically hospitalized youth; however, the lack of gender differences is consistent with findings from nationally representative samples of adolescents (Halpern, Oslak, Young, Martin, & Kupper, 2001).
Contrary to the study hypotheses, DV victimization did not significantly predict the continuum of NSSI experiences for males (e.g., thoughts, behaviors, medical impairment) nor did it differentiate between males who engaged in frequent NSSI versus infrequent/no NSSI. These results are contrary to that found in the adult literature, which suggests that intimate partner violence predicts NSSI across males and females (Levesque et al., 2010; Sansone et al., 2007). It is possible that developmental differences in the qualities of adult romantic relationships may partly explain these findings. For example, adult males may have more intense and emotionally intimate relationships than adolescent males (Madsen & Collins, 2011; Meier & Allen, 2009); this increased intensity may cause DV to have a greater impact on psychiatric processes such as NSSI. For females, a relationship between DV and NSSI did emerge when frequent NSSI was compared to infrequent/no NSSI. These findings are consistent with other studies conducted by our group, which have concluded that DV victimization is often linked to the most serious clinical course of mental illness in psychiatrically hospitalized youth (Rizzo et al., 2010).
In addition to the finding that female DV victims engage in frequent NSSI, two subgroups of adolescents were found to report more NSSI. Specifically, adolescent males with a history of DV victimization who reported higher levels of trait anger reported a greater intensity NSSI experiences than those who reported lower levels. Similarly, adolescent females with a history of DV victimization who reported higher propensity for engaging in indirect aggression reported a greater intensity of NSSI experiences than those who reported a lower propensity. The finding that trait anger moderated the association between DV victimization among males is consistent with study hypotheses as well as research which suggests that adolescents with NSSI report significant anger problems (Laye-Gindhu & Schonert-Reichl, 2005). It is also consistent with theory which suggests that adolescents may use NSSI to reduce affective arousal associated with negative interpersonal events (Chapman et al., 2006; Messer & Fremouw, 2008; Nock & Prinstein, 2004). Interestingly and contrary to study hypotheses, the trait hostility did not moderate the relation between DV victimization and NSSI for males or females. It is possible that lack of consistency in study results may reflect differences in levels of physiological arousal and cognitive reactivity associated with trait anger versus hostility.
Also contrary to study hypotheses was the interaction found between DV victimization and the propensity for indirect aggression in females. Although these results were unexpected, prior research has suggested that girls are more distressed by negative interpersonal events and tend to struggle with interpersonal difficulties (Leadbeater, Blatt, & Quinlan, 1995; Rose & Rudolph, 2006). It may be that indirect aggression (i.e., spread gossip, give silent treatment, slam doors, mess up others work) simply creates more interpersonal conflict for adolescent females which, in synergy with the stress of DV, increases the need to use NSSI as a stress-management strategy. A future study could examine interpersonal stress as a mechanism in this relationship.
The finding that psychological forms of dispositional aggression (anger and hostility) did not directly relate to NSSI or moderate the relation with DV in females suggests that NSSI may function slightly differently for them. Specifically, NSSI may be utilized to alleviate other forms of negative affect (e.g., sadness, anxiety) or to accomplish other goals (e.g., to try to get a reaction from someone or gain control of a situation; Nock & Prinstein, 2004). There is a small body of research on gender differences in NSSI that suggest that the method and frequency of NSSI behaviors may be slightly different in males than in females (Andover et al., 2010). Furthermore, in a community sample of adolescents, males were more likely to report that they engaged in NSSI to “make others angry,” whereas females were more likely to report that their NSSI was “to punish yourself” (Lloyd-Richardson et al., 2007). More research is needed on these important gender differences.
Although study findings are novel and build uniquely upon existing literature, several limitations of this research should be noted. First, although DV and NSSI were measured over the past year, data were cross-sectional in nature and thus directionality cannot be determined. Indeed, we conducted exploratory follow-up analyses to examine specificity of study findings (i.e., tested NSSI as the moderator) and found that an association between DV and anger (in males) or indirect aggression (in females) was present among those with more but not less frequent (or no) NSSI. Thus, although theory would suggest that DV victims may use NSSI as a means to manage negative affect or manipulate a social situation (Chapman et al., 2006; Nock & Prinstein, 2004), it is equally plausible that NSSI may trigger anger or perceived need for indirect aggression among victims of DV. Second, as mentioned above, there was significant multicollinearity between the individual subscales of the AQ. As such, it was difficult to establish that any one subtrait of aggression was accounting for change in NSSI, above and beyond other forms. Third, DV victimization is highly correlated with DV perpetration with most adolescent relationships characterized by mutual violence (Molidor & Tolman, 1998). As a result, DV perpetration could more closely linked with NSSI and dispositional aggression; unfortunately, we did not measure perpetration in this study. A future study should examine both victimization and perpetration to disentangle these relationships. Fourth, our participants included primarily White adolescents who were psychiatrically hospitalized. Our findings may not generalize to more racially and ethnically diverse samples or those from less intensive clinical or community populations. Finally, limited statistical power due to the modest sample size in the present study (n = 155) may have limited some of the statistical comparisons conducted. A post hoc power analysis conducted on the full model presented in Table 3 with the program G*Power 3.1 revealed that an n of approximately 86 would be needed to detect a large effect f2 = .35), an n of approximately 184 would be needed to detect a medium effect f2 = .15), and an n of approximately 1,304 would be needed to detect a small effect f2 = .02). Thus, we cannot completely rule out that there were small- or medium-sized effects in the models conducted separately for boys and for girls.
Despite its limitations, the current work suggests that DV victimization is a common interpersonal trauma among both male and female psychiatrically hospitalized adolescents. Although others have demonstrated links with substance use (Ackard, Neumark-Sztainer, & Hannan, 2003; Coker, Smith, McKeown, & King, 2000; Kreiter et al., 1999), cigarette smoking (Ackard et al., 2003), disordered eating (Ackard & Neumark-Sztainer, 2002; Silverman, Raj, Mucci, & Hathaway, 2001; Thompson, Wonderlich, Crosby, & Mitchell, 2001), depression and anxiety (Howard & Wang, 2003a,b), sexual health risks (Coker et al., 2000; Howard & Wang, 2003a,b; Kreiter et al., 1999), and suicidality (Ackard et al., 2003; Howard & Wang, 2003a,b; Kreiter et al., 1999; Silverman et al., 2001), our data suggest that DV victimization also has significant associations with NSSI between various subgroups of youth. DV was linked to frequent NSSI only among females, yet not directly linked to NSSI among males. Furthermore, male DV victims with elevated trait anger and female DV victims with a propensity for indirect aggression engaged in behaviors further along the NSSI continuum of clinical seriousness. These findings add to a growing body of literature demonstrating the importance of considering gender-specific effects of adolescent DV on youth emotional and behavioral health outcomes.
Clinically, our results may help improve interventions so they more effectively meet the needs of adolescents with distinct risk profiles. For example, as male DV victims with elevated trait anger were found to engage in NSSI, effective NSSI interventions may need to incorporate adaptive strategies to effectively process and manage anger in adolescent males. Similarly, female DV victims may benefit from adaptive strategies to manage their propensity for indirect aggression. By focusing intervention strategies on these intertwining issues, it may be possible to reduce self-harm behavior in an already vulnerable group of teens.
REFERENCES
- Ackard DM, & Neumark-Sztainer D (2002). Date violence and date rape among adolescents: Associations with disordered eating behaviors and psychological health. Child Abuse and Neglect, 26, 455–473. [DOI] [PubMed] [Google Scholar]
- Ackard DM, Neumark-Sztainer D, & Hannan P (2003). Dating violence among a nationally representative sample of adolescent girls and boys: Associations with behavioral and mental health outcomes. The Journal of Gender Specific Medicine, 6, 39–48. [PubMed] [Google Scholar]
- Aiken LS, & West SG (1991). Multiple regression: Testing and interpreting interactions. Newbury Park, CA: Sage. [Google Scholar]
- Andover MS, Primack JM, Gibb BE, & Pepper CM (2010). An examination of non-suicidal self-injury in men: Do men differ from women in basic NSSI characteristics? Archives of Suicide Research, 14, 79–88. [DOI] [PubMed] [Google Scholar]
- Boudewyn AC, & Liem JH (1995). childhood sexual abuse as a precursor to depression and self-destructive behavior in adulthood. Journal of Traumatic Stress, 8, 445–459. [DOI] [PubMed] [Google Scholar]
- Buss AH, & Warren WL (2000). The aggression questionnaire manual. Los Angeles, CA: Western Psychological Service. [Google Scholar]
- Chambers WJ, Puig-Antich J, Hirsch M, Paez P, Ambrosini PJ, Tabrizi MA, et al. (1985). The assessment of affective disorders in children and adolescents by semi-structured interview: Test–retest reliability of the Schedule for Affective Disorders and Schizophrenia for School-Age Children, Present Episode version. Archives of General Psychiatry, 42, 696–702. [DOI] [PubMed] [Google Scholar]
- Chapman AL, Gratz KL, & Brown MZ (2006). Solving the puzzle of deliberate self-harm: The experiential avoidance model. Behaviour Research and Therapy, 44, 371–394. [DOI] [PubMed] [Google Scholar]
- Coffey P, Leitenberg H, Henning K, Bennett R, & Jankowski M (1996). Dating violence: The association between methods of coping and women’s psychological adjustment. Violence and Victims, 11, 227–238. [PubMed] [Google Scholar]
- Coker AL, Smith PH, McKeown RE, & King MJ (2000). Frequency and correlates of intimate partner violence by type: Physical, sexual, and psychological battering. American Journal of Public Health, 90, 553–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conterio K, Lader W, & Bloom JK (1998). Bodily harm: The breakthrough healing program for self-injurers. New York: Hyperion. [Google Scholar]
- Darche MA (1990). Psychological factors differentiating self-mutilating and non-self-mutilating adolescent inpatient females. Psychiatric Hospital, 21, 31–35. [Google Scholar]
- DiClemente RJ, Ponton LE, & Hartley D (1991). Prevalence and correlates of cutting behavior: Risk for HIV transmission. Journal of the American Academy of Child and Adolescent Psychiatry, 30, 735–739. [PubMed] [Google Scholar]
- Dube SR, Anda RF, Felitti VJ, Chapman DP, Williamson DF, & Giles WH (2001). Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: Findings from the Adverse Childhood Experiences Study. Journal of the American Medical Association, 286, 3089–3096. [DOI] [PubMed] [Google Scholar]
- Follingstad DR, Wright S, Lloyd S, & Sebastian JA (1991). Sex differences in motivations and effects in dating violence. Family Relations, 40, 51–57. [Google Scholar]
- Glassman LH, Weierich MR, Hooley JM, Deliberto TL, & Nock MK (2007). Child maltreatment, non-suicidal self-injury, and the mediating role of self-criticism. Behaviour Research and Therapy, 45, 2483–2490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halpern CT, Oslak SG, Young ML, Martin SL, & Kupper LL (2001). Partner violence among adolescents in opposite-sex romantic relationships: Findings from the National Longitudinal Study of Adolescent Health. American Journal of Public Health, 91, 1679–1685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halpern CT, Young ML, Waller MW, Martin SL, & Kupper LL (2004). prevalence of partner violence in same-sex romantic and sexual relationships in a national sample of adolescents. Journal of Adolescent Health, 35, 124–131. [DOI] [PubMed] [Google Scholar]
- Herpertz S (1995). Self-injurious behaviour: psychopathological and nosological characteristics in subtypes of self-injurers. Acta Psychiatrica Scandinavica, 91, 57–68. [DOI] [PubMed] [Google Scholar]
- Howard DE, & Wang MQ (2003a). Risk profiles of adolescent girls who were victims of dating violence. Adolescence, 38, 1–14. [PubMed] [Google Scholar]
- Howard DE, & Wang MQ (2003b). Psychosocial factors associated with adolescent boys’ reports of dating violence. Adolescence, 38, 519–533. [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. (1997). Schedule for Affective Disorders and Schizophrenia for School-Age Children—Present and Lifetime Version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry, 36, 980–988. [DOI] [PubMed] [Google Scholar]
- Kim ΗK, & Capaldi DM (2004). The association of antisocial behavior and depressive symptoms between partners and risk for aggression in romantic relationships. Journal of Family Psychology, 18, 82–96. [DOI] [PubMed] [Google Scholar]
- Kim-Godwin YS, Clements C, McCuiston AM, & Fox JA (2009). Dating violence among high school students in Southeastern North Carolina. The Journal of School Nursing, 25, 141–151. [DOI] [PubMed] [Google Scholar]
- Korman LM, Collins J, Dutton D, Dhayanathan B, Littman-Sharp N, & Skinner W (2008). Problem gambling and intimate partner violence. Journal of Gambling Studies, 24, 13–23. [DOI] [PubMed] [Google Scholar]
- Kreiter SR, Krowchuk DP, Woods CR, Sinal SΗ, Lawless MR, & DuRant RΗ (1999). Gender differences in risk behaviors among adolescents who experience date fighting. Pediatrics, 104, 1286–1292. [DOI] [PubMed] [Google Scholar]
- Laye-Gindhu A, & Schonert-Reichl KA (2005). Nonsuicidal self-harm among community adolescents: Understanding the “whats” and “whys” of self-harm. Journal of Youth and Adolescence, 34, 447–457. [Google Scholar]
- Leadbeater B, Banister E, Ellis W, & Yeung R (2008). Victimization and relational aggression in adolescent romantic relationships: The influence of parental and peer behaviors, and individual adjustment. Journal of Youth and Adolescence, 37, 359–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leadbeater BJ, Blatt SJ, & Quinlan DM (1995). Gender-linked vulnerabilities to depressive symptoms, stress, and problem behaviors in adolescents. Journal of Research on Adolescence, 5, 1–29. [Google Scholar]
- Lehrer JA, Buka S, Gortmaker S, & Shrier LA (2006). Depressive symptomatology as a predictor of exposure to intimate partner violence among US female adolescents and young adults. Archives of Pediatrics & Adolescent Medicine, 160, 270–276. [DOI] [PubMed] [Google Scholar]
- Levesque C, Lafontaine M, Bureau J, Cloutier P, & Dandurand C (2010). The influence of romantic attachment and intimate partner violence on non-suicidal self-injury in young adults. Journal of Youth and Adolescence, 39, 474–483. [DOI] [PubMed] [Google Scholar]
- Lloyd-Richardson E, Perrine N, Dierker L, & Kelley ML (2007). Characteristics and functions of non-suicidal self-injury in a community sample of adolescents. Psychological Medicine, 37, 1183–1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madsen SD, & Collins WA (2011). The salience of adolescent romantic experiences for romantic relationship qualities in young adulthood. Journal of Research on Adolescence, 21, 789–801. [Google Scholar]
- Meier A, & Allen G (2009). Romantic relationships from adolescence to young adulthood: Evidence from the National Longitudinal Study of Adolescent Health. The Sociological Quarterly, 50, 308–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messer J, & Fremouw W (2008). A critical review of explanatory models for self-mutilating behaviors in adolescents. Clinical Psychology Review, 28, 162–178. [DOI] [PubMed] [Google Scholar]
- Molidor C, & Tolman RM (1998). Gender and contextual factors in adolescent dating violence. Violence Against Women, 4, 180–194. [DOI] [PubMed] [Google Scholar]
- Nock MK, & Prinstein MJ (2004). A functional approach to the assessment of self-mutilative behavior. Journal of Consulting and Clinical Psychology, 72, 885–890. [DOI] [PubMed] [Google Scholar]
- O’Keefe M (1998). Posttraumatic stress disorder among incarcerated battered women: A comparison of battered women who killed their abusers and those incarcerated for other offenses. Journal of Traumatic Stress, 11, 71–85. [DOI] [PubMed] [Google Scholar]
- O’Keefe M, & Treister L (1998). Victims of dating violence among high school students. Violence Against Women, 4, 195–223. [DOI] [PubMed] [Google Scholar]
- Ramírez JM, & Andreu JM (2006). Aggression, and some related psychological constructs (anger, hostility, and impulsivity): Some comments from a research project. Neuroscience and Biobehavioral Reviews, 30, 276–291. [DOI] [PubMed] [Google Scholar]
- Rizzo CJ, Esposito-Smythers C, Spirito A, & Thompson A (2010). Psychiatric and cognitive functioning in adolescent inpatients with histories of dating violence victimization. Journal of Aggression, Maltreatment, and Trauma, 19, 565–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romans SE, Martin JL, Anderson JC, Herbison GP, & Mullen PE (1995). Sexual abuse in childhood and deliberate self-harm. American Journal of Psychiatry, 152, 1336–1342. [DOI] [PubMed] [Google Scholar]
- Rose AJ, & Rudolph KD (2006). A review of sex differences in peer relationship processes: Potential trade-offs for the emotional and behavioral development of girls and boys. Psychological Bulletin, 132, 98–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sansone RA, Chu J, & Wiederman MW (2007). Self-inflicted bodily harm among victims of intimate-partner violence. Clinical Psychology and Psychotherapy, 14, 352–357. [Google Scholar]
- Silverman JG, Raj A, Mucci LA, & Hathaway JE (2001). Dating violence against adolescent girls and associated substance use, unhealthy weight control, sexual risk behavior, pregnancy, and suicidality. Journal of the American Medical Association, 286, 572–579. [DOI] [PubMed] [Google Scholar]
- Spriggs AL, Halpern CT, Herring AH, & Schoenback VJ (2009). Family and school socioeconomic disadvantage: interactive influences on adolescent dating violence victimization. Social Science & Medicine, 68, 1956–1965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swan SC, Gambone LJ, Fields AM, Sullivan TP, & Snow DL (2005). Women who use violence in intimate relationships: The role of anger, victimization, and symptoms of posttraumatic stress and depression. Violence Victims, 20, 267–285. [DOI] [PubMed] [Google Scholar]
- Thompson KM, Wonderlich SA, Crosby RD, & Mitchell JE (2001). Sexual victimization and adolescent weight regulation practices: A test across three community-based samples. Child Abuse and Neglect, 25, 291–305. [DOI] [PubMed] [Google Scholar]
- Van der Kolk BA, Perry JC, & Herman JL (1991). Childhood origins of self-destructive behavior. American Journal of Psychiatry, 149, 1280–1281. [DOI] [PubMed] [Google Scholar]
- Weismoore J, & Esposito-Smythers C (2010). The role of cognitive distortion in the relationship between abuse, assault, and non-suicidal self-injury. Journal of Youth and Adolescence, 39, 281–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitaker DJ, Haileyesus T, Swahn M, & Saltzman LS (2007). Differences in frequency of violence and reported injury between relationships with reciprocal and nonreciprocal intimate partner violence. American Journal of Public Health, 97, 941–947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winchel RM, & Stanley M (1991). Self-injurious behavior: A review of the behavior and biology of self-mutilation. American Journal of Psychiatry, 148, 306–317. [DOI] [PubMed] [Google Scholar]
- Wolfe DA, Crooks CV, Lee V, McIntyre-Smith A, & Jaffe PG (2003). The effects of children’s exposure to domestic violence: A meta-analysis and critique. Clinical Child and Family Psychology Review, 6, 171–187. [DOI] [PubMed] [Google Scholar]
- Wolfe DA, Scott K, Wekerle C, & Pittman AL (2001). Child maltreatment: Risk of adjustment problems and dating violence in adolescence. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 282–289. [DOI] [PubMed] [Google Scholar]
- Yeo ΗM, & Yeo WW (1993). Repeat deliberate self-harm: A link with childhood sexual abuse? Archives of Emergency Medicine, 10, 161–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuckerbrot RA, & Jenson PS (2006). Improving recognition of adolescent depression in primary care. Archives of Pediatrics & Adolescent Medicine, 160, 694–704. [DOI] [PubMed] [Google Scholar]


