Abstract
Pregnancy is associated with changes in normal physiology, including changes to the normal parameters for blood tests. Abnormal liver function tests are a common reason for referral to gastroenterology. However, in the pregnant patient, there are unique potential causes. It is of prime importance to be aware of pregnancy-specific liver diseases as they can be serious and progress rapidly affecting outcomes for both the mother and fetus. Here, we provide an overview of the manifestations of pregnancy-related liver diseases and discuss their potential consequences.
Keywords: liver disease in pregnancy, acute fatty liver
Introduction
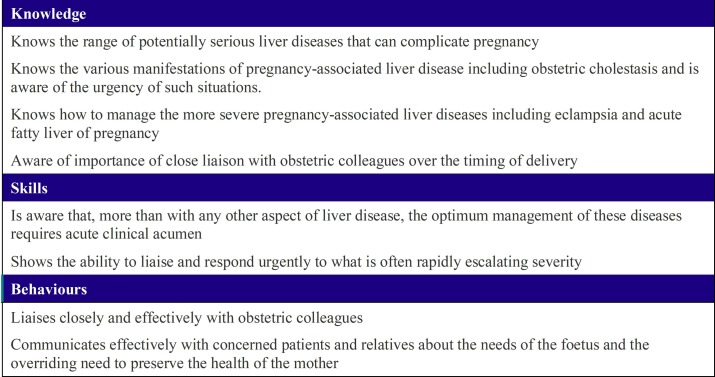
Pregnancy-associated liver disorders—though uncommon—will require the expert review of a gastroenterologist/hepatologist. Liver disorders may present inconspicuously during gestation. What is probably the most challenging factor is establishing the diagnosis in the context of the expected physiological changes of pregnancy. Prognostic models utilising existing hepatological scores (model end-stage liver disease) have been suggested to promote early recognition of those who are potentially at higher risk.1 In this curriculum-mapped review (see figure 1), we discuss the most common pregnancy-related liver diseases encountered during gastroenterology training. An overview is provided in table 1.
Figure 1.
Curriculum item 3a: pregnancy-associated liver disease.
Table 1.
Summary of pegnancy-related liver conditions
| Trimester | Features | Alanine aminotransferase | Bilirubin | Platelets | Recur | Comments | |
| Hyperemesis gravidarum | First | Vomiting, dehydration, weight loss, ketosis | 1–2× in 50% of patients | Normal | Normal | +++ | Twin pregnancies |
| Intrahepatic cholestasis of pregnancy | Second and third | Bile acids↑ pruritus | 1–4× | Normal in 75% | Normal | +++ | Treat with ursodeoxycholic acid Deliver at 37 weeks (risk of late intrauterine death) |
| Acute fatty liver disease of pregnancy | Third | Creatinine↑ Uric Acid↑ |
1–10× | Can be elevated | Can be low but usually normal | Rarely | Maternal body mass index<20 Biopsy: microvesicular steatosis, foamy hepatocytes, hepatic necrosis 50% will have evidence of pre-eclampsia |
| Haemolysis, elevated liver enzyme levels and low platelet levels (HELLP) | Third May occur postpartum |
Lactate dehydrogenase↑ Prothrombin and fibrinogen normal Uric acid↑ |
1–100× | Normal | Low | ++ | 25% of cases will happen in postpartum period Associated with pre-eclampsia |
| Pre-eclampsia | >20 weeks | Hypertension Proteinuria±end organ damage |
20%–30% will have abnormal liver function tests | Can be low in severe disease | ++ | Usually due to uteroplacental ischaemia Urgent delivery to avoid eclampsia, liver rupture and necrosis Up to 10%–20% will show features of HELLP17 |
|
Hyperemesis gravidarum
Hyperemesis gravidarum is a condition of early pregnancy occurring in 1 in 200 pregnancies,2 with symptoms mainly resolving by mid-pregnancy. It is the extreme form of nausea and vomiting of pregnancy leading to dehydration, ketosis and weight loss of >5% of body weight. Women often need hospitalisation, and in this situation, biochemical abnormalities include renal and electrolyte disturbance due to dehydration. In the cohort who are hopsitalised, a mild elevated aminotransferases occurs in 50%.2 Abnormal liver function tests (LFTs) resolve on cessation of vomiting symptoms. The aetiology remains unclear, but we know that hyperemesis often recurs in future pregnancies.
Acute fatty liver disease of pregnancy (AFLP)
AFLP is a rare but life-threatening illness for both the mother and fetus. It is characterised by microvesicular fatty infiltration of the liver and usually occurs in the third trimester (median presentation 36 weeks), although can occur postnatally.3 Risk factors for its development include nulliparity, twin pregnancy and low maternal body mass index (BMI).3
Early recognition, prompt delivery and supportive care are essential to optimise maternal and fetal prognosis, as the postpartum clinical course is dependent on the interval between symptoms and termination of the pregnancy.4
Presenting symptoms are often non-specific including nausea, vomiting and abdominal pain. The hallmarks of liver failure (encephalopathy, coagulopathy and hypoglycaemia) may be present.
The diagnosis of AFLP is usually clinical. The Swansea criteria, validated in a large UK cohort (box 1), combine symptoms and laboratory results5 and offers an 85% positive predictive value and 100% negative predictive value for biopsy proven hepatic microvesicular steatosis. Practically, liver biopsy is rarely performed due to the need to stabilise and deliver affected women.
Box 1. Swansea criteria for diagnosis of acute fatty liver of pregnancy.
Six or more criteria required in the absence of another cause
Vomiting.
Abdominal pain.
Polydipsia/polyuria.
Encephalopathy.
Elevated bilirubin >14 μmol/L
Hypoglycaemia <4 mmol/L.
Elevated uric acid >340 μmol/L.
Leucocytosis >11×106 cells/L.
Ascites or bright liver on ultrasound scan.
Elevated transaminases (aspartate transaminase or alanine transaminase) >42 IU/L.
Elevated ammonia >47 μmol/L.
Renal impairment; creatinine >150 μmol/L.
Coagulopathy; prothrombin time >14 s or activated partial thromboplastin time >34 s.
Microvesicular steatosis on liver biopsy.
There is a link between fetal deficiency of long-chain 3-hydroxyacyl CoA dehydrogenase (LCHAD) and AFLP.6 Homozygous-deficient offspring spill unmetabolised long-chain fatty acids into the maternal circulation, accumulation can lead to hepatoxicity.
Mortality has improved recently due to early recognition and rapid fetal delivery followed by maternal supportive care. A recent meta-analysis by Wang et al showed that caesarean section is the safest method of delivery and is associated with better pregnancy outcomes.7 Although treatment, in the main, is supportive, there have been reports of liver transplantation and plasma exchange postdelivery.4
Intrahepatic cholestasis of pregnancy (ICP)
ICP is the most common liver disease in pregnancy, often presenting in the second and third trimesters. It has a variable incidence, ranging from 3% to 5% of pregnant women in Chile to 0.7% in the UK; it is rarely reported in African countries.8 It is likely that elevated oestrogen and progesterone metabolites in pregnancy unmask the disease in genetically susceptible women.9 It is a reversible cholestasis characterised by pruritus and elevated serum bile acids with spontaneous relief of signs and symptoms within 6 weeks of delivery. ICP has a high recurrence rate. Jaundice occurs in <25% of patients with ICP and always after the onset of pruritus. If jaundice is the presenting symptom, further evaluation is necessary.
Risk factors include advanced maternal age, a history of cholestasis secondary to oral contraceptives, a personal or family history of ICP, multiple pregnancy and fertility treatment. Some studies suggest a higher prevalence in patients with hepatitis C, cholelithiasis and non-alcohol fatty liver disease.10
In ICP, bile acid concentrations are typically >10μmol/L, with most complications occurring with levels >40μmol/L.11 12 Aminotransferase levels may also be elevated. Ultrasonography should be performed to exclude cholelithiasis. Maternal outcomes are excellent; however, there is a risk of fetal distress, preterm labour, prematurity and intrauterine death.12
Delivery at 37 weeks should be considered because intrauterine death is more common in the last month of pregnancy, with few deaths before 37 weeks.13 Decisions should be tailored to the individual pregnancy.14 First-line therapy is ursodeoxycholic acid (UDCA) at 10–15 mg/kg maternal body weight which results in improved maternal symptoms and biochemistry in approximately 75% of cases.15 UDCA increases expression of bile salt export pumps and increases placental bile transporters. UDCA is more effective than cholestyramine or dexamethasone in controlling pruritus. Fat malabsorption can result in fat-soluble vitamin deficiencies. Some women do not respond to UDCA, and combining with rifampicin can improve the symptoms and biochemical results.16
Affected women also have an increased risk of hepatobiliary disease later in life, most commonly gallstones, hepatobiliary malignancies and immune mediated and cardiovascular diseases. If women have ongoing symptoms or biochemical hepatic impairment for more than 3 months postpartum an alternative/additional diagnosis should be sought.
Pre-eclampsia
Pre-eclampsia is defined as new onset gestational hypertension (in a previously normotensive woman) with significant proteinuria and can be complicated by end-organ dysfunction, eclampsia and death. Proteinuria is defined as:
≥ +1 (30 mg/dL) on urine dipstick;
random Protein: Creatinine ratio ≥0.3 mg protein/mg creatinine;
≥0.3 mg protein/24 hours.
Hypertension in pregnancy (gestational hypertension) is defined as systolic blood pressure ≥140 mm Hg and diastolic blood pressure ≥90 mm Hg without proteinuria±end organ damage. Pre-eclampsia could occur in women with pre-existing chronic hypertension and diagnosis should be dictated by the new-onset proteinuria±end organ damage. It typically occurs after 20 weeks of gestation. Several risk factors have been identified and these are listed in table 2.
Table 2.
Risk factors associated with gestational hypertension and pre-eclampsia
| Moderate risk | High risk |
| Primigravida | Hypertension in previous pregnancy |
| Maternal age >40 years or <18 years | Systemic lupus erythematosus |
| Pregnancy interval >10 years | Antiphospholipid syndrome |
| Body mass index ≥35 kg/m2 | Autoimmunity |
| Family history of pre-eclampsia | Diabetes mellitus |
| Chronic kidney disease | Hypertension |
| Mutifetal gestations | |
| Black race | |
| Hydrops fetalis | |
| In vitro fertilisation | |
| Partner related (new partner, limited sperm exposure) |
The pathophysiology of pre-eclampsia involves placental and maternal vascular dysfunction characterised by abnormal trophoblast invasion of spiral arteries. The symptoms of pre-eclampsia include severe headache, visual disturbances, emesis, oedema (peripheral and/or pulmonary), abdominal and epigastric pain, dyspnoea, chest pain, oliguria (in severe disease) and reduced mental status. Serum and urine investigations may reveal acute kidney injury, hyperuricaemia, hyperlipidaemia, neutrophilia, urinary sediment and raised haematocrit. Serious forms of the disease may be characterised by thrombocytopenia, haemolysis and elevated aminotransferases. It is believed that abnormalities to LFTs are secondary to reduced hepatic flow leading to hepatic ischaemia or periportal haemorrhage. Typically, clotting studies are normal unless there is progression to liver failure or placental abruption.
Patients with gestational hypertension including pre-eclampsia may have long-term health complications, and these need to be emphasised to patients. These are shown in box 2.
Box 2. Long-term health risks for people with pre-eclampsia.
Non-gestational hypertensive disease.
Gestational hypertension in future pregnancies (1 in 2–8 pregnancies).
Increased pre-eclampsia risk in future pregnancies.
End-stage renal disease.
Cardiovascular disease including ischaemic heart disease and stroke.
It should be noted that pre-eclampsia can develop postpartum. Generally, a conservative approach should be considered until week 34. Oral labetalol should be offered as first line for patients with blood pressure ≥150/100 mm Hg. LFTs, renal function tests and full blood count should be performed at least twice weekly. The timing of birth for patients with pre-eclampsia should be reviewed carefully by an obstetric consultant. Successful conservative management could delay elective delivery until after 34 weeks, even for patients with severe hypertension (blood pressure ≥160/110 mm Hg) if their blood pressure has been adequately controlled. Delivery before 34 weeks should be considered in patients who are refractory to antihypertensive therapy or if there are any other identified risk factors for the mother and/or fetus.
HELLP
The acronym HELLP was first described in 1982 and stands for haemolysis (with a micoangiopathic blood smear), elevated liver enzymes (LFTs) and low platelet count. There is debate as to whether HELLP is a severe form of pre-eclampsia. The incidence of HELLP is 0.1%–0.8% of all pregnancies and risk factors include family history and HELLP in previous pregnancies as well as pre-eclampsia (10%–20% of patients).17 The pathogenesis of HELLP involves abnormal or aberrant placentation and more rarely fetal LCHAD deficiency.6
Patients with HELLP may present with a plethora of symptoms both in variety and severity, most usually between 28 and 36 weeks of gestation. The condition can also present postpartum. Commonly patients will demonstrate gastrointestinal symptoms including abdominal pain (especially right-upper-quadrant), nausea, vomiting and malaise. About 85% of patients are hypertensive (blood pressure ≥140/90 mm Hg) and proteinuric. Apart from the deranged LFTs, other severe hepatic manifestations have been described with HELLP including hepatic infarction, haemorrhage and rupture. Other serious complications include acute kidney injury, retinal detachment, pulmonary oedema, abruption placentae and disseminated intravascular coagulation.
All three elements of the HELLP acronym need to be satisfied in a pregnant patient before the diagnosis is made. When the diagnosis is considered, LFTs, blood film, full blood count, renal function tests and urine protein:creatinine ratio should be obtained especially in women presenting between 28 and 36 weeks of gestation and within 1–2 weeks postpartum. The Tennessee classification is the most widely used system, the parameters of which are outlined in table 3).18
Table 3.
The Tennessee classification of HELLP syndrome (adapted from Sibai et al 18)
| 1 | Platelet count ≤100 x 10^9/L |
| 2 | AST ≥70 IU/L and LDH ≥600 IU/L |
| 3 | Haemolysis on peripheral smear |
Two out of three criteria=partial HELLP.
All criteria=full HELLP.
AST, aspartate aminotransferase; LDH, lactate dehydrogenase; HELLP, haemolysis, elevated liver enzyme levels and low platelet levels.
SCE style questions
- Which of the following is the most accurate regarding the frequency of HELPP cases that occur in the postpartum period?
- Less than 10%
- 10%–20%
- 25%–35%
- 40%–50%
- More than 50%
Answer: A
- Which one of the following conditions has the highest risk of recurrence in subsequent pregnancies?
- Acute fatty liver disease of pregnancy
- Intrahepatic cholestasis of pregnancy
- Pre-eclampsia
- HELLP syndrome
Answer: B
- Acute fatty liver of pregnancy is associated with which of the following?
- Low maternal BMI
- High maternal BMI
- Singleton pregnancy
- Underlying liver disease
- Advanced maternal age
Answer: A
Footnotes
Contributors: Both authors were involved in the conceptualisation of the work and designed the manuscript, carried out the literature review, drafted the work and revised it critically for important intellectual content. Both authors provided final approval of the version to be published and agreed to be accountable for the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Murali AR, Devarbhavi H, Venkatachala PR, et al. . Factors that predict 1-month mortality in patients with pregnancy-specific liver disease. Clin Gastroenterol Hepatol 2014;12:109–13. 10.1016/j.cgh.2013.06.018 [DOI] [PubMed] [Google Scholar]
- 2. Quinla JD, Hill DA. Nausea and vomiting of pregnancy. Am Fam Physician 2003;68:121–8. [PubMed] [Google Scholar]
- 3. Knight M, Nelson-Piercy C, Kurinczuk JJ, et al. . A prospective national study of acute fatty liver of pregnancy in the UK. Gut 2008;57:951–6. 10.1136/gut.2008.148676 [DOI] [PubMed] [Google Scholar]
- 4. Ringers J, Bloemenkamp K, Francisco N, et al. . Auxiliary or orthotopic liver transplantation for acute fatty liver of pregnancy: case series and review of the literature. BJOG 2016;123:1394–8. 10.1111/1471-0528.13707 [DOI] [PubMed] [Google Scholar]
- 5. Goel A, Ramakrishna B, Zachariah U, et al. . How accurate are the Swansea criteria to diagnose acute fatty liver of pregnancy in predicting hepatic microvesicular steatosis? Gut 2011;60 138–9. 10.1136/gut.2009.198465 [DOI] [PubMed] [Google Scholar]
- 6. Ibdah JA, Bennett MJ, Rinaldo P, et al. . A fetal fatty-acid oxidation disorder as a cause of liver disease in pregnant women. N Engl J Med 1999;340:1723–31. 10.1056/NEJM199906033402204 [DOI] [PubMed] [Google Scholar]
- 7. Wang HY, Jiang Q, Shi H, et al. . Effect of caesarean section on maternal and foetal outcomes in acute fatty liver of pregnancy: a systematic review and meta-analysis. Sci Rep 2016;6:28826 10.1038/srep28826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Geenes V, Williamson C. Intrahepatic cholestasis of pregnancy. World J Gastroenterol 2009;15:2049–66. 10.3748/wjg.15.2049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Abu-Hayyeh S, Ovadia C, Lieu T, et al. . Prognostic and mechanistic potential of progesterone sulfates in intrahepatic cholestasis of pregnancy and pruritus gravidarum. Hepatology 2016;63:1287–98. 10.1002/hep.28265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Marschall HU, Wikström Shemer E, Ludvigsson JF, et al. . Intrahepatic cholestasis of pregnancy and associated hepatobiliary disease: a population-based cohort study. Hepatology 2013;58:1385–91. 10.1002/hep.26444 [DOI] [PubMed] [Google Scholar]
- 11. Garcia-Flores J, Cañamares M, Cruceyra M, et al. . Clinical value of maternal bile Acid quantification in intrahepatic cholestasis of pregnancy as an adverse perinatal outcome predictor. Gynecol Obstet Invest 2015;79:222–8. 10.1159/000370003 [DOI] [PubMed] [Google Scholar]
- 12. Geenes V, Chappell LC, Seed PT, et al. . Association of severe intrahepatic cholestasis of pregnancy with adverse pregnancy outcomes: a prospective population-based case-control study. Hepatology 2014;59:1482–91. 10.1002/hep.26617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Williamson C, Hems LM, Goulis DG, et al. . Clinical outcome in a series of cases of obstetric cholestasis identified via a patient support group. BJOG 2004;111:676–81. 10.1111/j.1471-0528.2004.00167.x [DOI] [PubMed] [Google Scholar]
- 14. Henderson CE, Shah RR, Gottimukkala S, et al. . Primum non nocere: how active management became modus operandi for intrahepatic cholestasis of pregnancy. Am J Obstet Gynecol 2014;211:189–96. 10.1016/j.ajog.2014.03.058 [DOI] [PubMed] [Google Scholar]
- 15. European Association for the Study of the Liver. EASL clinical practice guidelines: management of cholestatic liver diseases. J Hepatol 2009;51:237–67. 10.1016/j.jhep.2009.04.009 [DOI] [PubMed] [Google Scholar]
- 16. Geenes V, Chambers J, Khurana R, et al. . Rifampicin in the treatment of severe intrahepatic cholestasis of pregnancy. Eur J Obstet Gynecol Reprod Biol 2015;189:59–63. 10.1016/j.ejogrb.2015.03.020 [DOI] [PubMed] [Google Scholar]
- 17. Gibbs RS, Danforth DN. Danforth’s obstetrics and gynecology. 10th edn Philadelphia, PA; London: Lippincott Williams & Wilkins, 2008. [Google Scholar]
- 18. Sibai BM, Ramadan MK, Usta I, et al. . Maternal morbidity and mortality in 442 pregnancies with hemolysis, elevated liver enzymes, and low platelets (HELLP syndrome). Am J Obstet Gynecol 1993;169:1000–6. 10.1016/0002-9378(93)90043-I [DOI] [PubMed] [Google Scholar]