Abstract
Purpose
Blue nevus is a melanocytic tumor that has been commonly described in the skin. Extracutaneous presentations including the ocular surface are rare. As such, the purpose of this study was to characterize the clinical features and clinical course of the congenital melanocytic tumor (blue nevus) of the conjunctiva.
Design
Retrospective noncomparative case series
Participants
21 patients with 23 blue nevi of the ocular surface that were surgically excised between 2000–2016.
Methods
A chart review of patients identified from a database search of the Florida Lions Ocular Pathology Laboratory records. Pathological diagnoses were confirmed by two pathologists (SRD and GE). All specimens were bleached and tissue permitting, stained using SOX10 (MilliporeSigma, Darmstadt, Germany) and CD68 (Leica Biosystems, Nussloch, Germany).
Main outcome measures
Clinical characteristics, pathological features, and clinical course.
Results
Mean age of the population was 55±15; 71.4% (n=15) were white and 57.1% (n=12) male. One patient had 3 lesions for a total of 23 lesions examined. Clinically, 13 lesions were on the bulbar conjunctiva, 3 on the tarsal conjunctiva, 3 in the fornix, 2 caruncular, 1 episcleral and 1 at the limbus. Pre-excision, 8 patients were thought to have primary acquired melanosis (PAM), 4 with concern for primary conjunctival melanoma, and 1 thought to have metastatic disease from a plantar melanoma. Five lesions were thought to be benign, and in 8 patients the lesions were identified incidentally after other ocular surgeries, with no pre-excision diagnosis of the lesions. Pathological features were consistent with simple blue nevi in 21 lesions and cellular blue nevus in 2 lesions. No malignant transformations were noted in any patient over the mean 20.2 months follow up period (range 2 weeks to 103 months).
Conclusion
Blue nevus is a rare deeply pigmented congenital melanocytic lesion with a benign clinical course that can appear clinically similar to PAM or melanoma.
Keywords: Blue nevus, nevi, conjunctival nevus
Introduction
Blue nevus is a melanocytic tumor that has been commonly described in the skin. Classically, it is considered a congenital lesion1 however, its full degree of pigmentation and hence its clinical diagnosis may occur later in life, most commonly during childhood and young adulthood.2–4 It has a higher frequency in females.2–4
Histologically, blue nevi are composed of deeply located neural crest-derived, spindled, dendritic and stellate melanocytes that become arrested during the course of their embryonic migration to the epithelium. In normal embryonic development, dermal melanocytes normally disappear everywhere except the presacral area, the head, neck, and the dorsal extremities. The melanocytes then form dense collections of uniformly pigmented cells in the skin dermis.5,6 In contrast, typical nevocellular nevi have histologically bland nests of melanocytes present at the dermal epidermal junction, within the dermis or ina combination of both. The cells migrate from the epithelium downward and may include epithelial inclusion cysts.
Blue nevi are divided into two main histological groups, common blue and cellular blue nevi. Common blue nevi have loosely aggregated spindle shape or dendritiform cells with no mitotic activity.1, 5 In contrast, cellular blue nevi have cells arranged in islands, with a highly cellular nodule in the center containing lightly pigmented spindle or polygonal cells of little mitotic activity. The nodules are surrounded by sclerotic regions with cells resembling common blue nevi.1, 7 Blue nevi may also occur in combination with other nevi to form combined melanocytic nevi.8, 9
Given the deep location of the brown melanin in the dermis, the Tyndall effect gives blue nevi their distinctive color when encountered in the skin. This effect describes the phenomenon where longer wavelengths of light are absorbed by the superficial layers while the shorter wavelengths (blue) are reflected. The net effect of the different wavelengths of light determines the observed color.10
Extracutaneous presentations of blue nevi are infrequent and have only rarely been described on the ocular surface. The frequency of blue nevi in cohorts with melanocytic lesions was found to be 0.6%(2/343),11 2.5% (5/200)10 and 3% (4/148),12 respectively. In all, 11 case reports covering 11 patients have described the presence of a blue nevus on the conjunctiva.1, 7, 13–21 (Table 2). Of these, one case first described the discrepancies between blue nevi of the conjunctiva and the skin, with a focus on differences in apparent color.16 Three reports described multifocal lesions,17, 19, 20 two of which were mostly or completely cellular blue nevi17, 19 and one which transformed into a malignant melanoma.19 Another case report described the presence of a cellular blue nevus in a patient with oculodermal melanocytosis (nevus of Ota) syndrome.13
Table 2.
Literature review: Demographics and clinical characteristics of conjunctival blue nevus:
| Publication | Location of lesions | Age in years | Gender | Race | Size in mm |
|---|---|---|---|---|---|
| Speakman and Phillips 197313 | Conjunctiva near right lower punctum | 61 | M | White | Not mentioned |
| Smith and Brockhurst 197614 | OD sclera under medial rectus | 50 | M | Unknown | 7 × 15 × 2 |
| Boudet, Arnaud et al. 197715 | OD 7 to 8 o’clock limbus | 36 | M | Unknown | 2 × 3.5 |
| Eller and Bernardino 198316 | OD bulbar conjunctiva, near limbus | 30 | F | White | 1.5 × 2.8 |
| Blicker, Rootman et al. 19927 | OD, entire inferior fornix &lower lid, Upper lid palpebral conjunctiva Upper lid margin |
74 | F | White | Not mentioned |
| Holbach, Nagel et al. 199417 | OS plica, caruncle, fornix, mucocutaneous junction | 54 | M | White | Not mentioned |
| Tucker, Linberg et al. 199418 | OS bulbar conjunctiva | 68 | F | White | Not mentioned |
| Demirci, Shields et al. 200019 | OS inferior fornix | 41 | M | White | 25 × 10 |
| Berman, Shields et al. 200820 | OS limbus, bulbar conjunctiva, tarsal conjunctiva, fornix and plica semilunaris | 55 | F | White | Bulbar:0.75 ×0.75 Limbus 7×6, Plica 3×2, Tarsus 3.5×3, Fornix 5×4 & 2×2 |
| Jakobiec, Nguyen et al. 201021 | OD 10 o’clock limbus | 13 | F | Indian descent | 5×2 |
| Kirzhner, Jakobiec et al. 20111 | Mucocutaneous junction of right eyelid margin | 93 | F | White | 3×4 |
M=male; F=female, OD= Right eye, OS= Left eye
Blue nevi cells in the conjunctiva are found in a more superficial location (substantia propria) than can be found in the dermis of the skin.22 Because the color of melanin is not filtered by the thin overlying epithelium,16, 10 the Tyndall effect is absent. Thus conjunctival blue nevi may appear brown, black, slate gray or blue, depending on both depth and thickness.5 In contrast, typical nevocellular nevi are raised or flat, are more superficial, are potentially cystic, and possibly change size and pigmentation with age and hormonal changes. The distinction is not absolute, however, and histologically, combined nevi (composed of blue nevus cells and nevocellular cells) can be seen in the conjuntiva.8, 9
To our knowledge, we present the largest case series of 21 patients with 23 blue nevi of the ocular surface emphasizing their clinical characteristics, pre-operative impressions, histopathologic findings, and clinical course.
Methods
Study Population
This study was conducted with adherence to the tenets of the Declaration of Helsinki and with approval from the University of Miami’s Institutional Review Board to retrospectively review patient charts. All patients with a pathological diagnosis of blue nevus of the ocular surface between the years of 2000 and 2016 were compiled from a search of the database of the Florida Lions Ocular Pathology lab records. After pathology record review, patients with combined nevi (nevi containing elements of blue nevus and nevocellular nevi) were excluded (n=4) and one lesion too necrotic to make an absolute determination, leaving a total of 21 patient charts of pure blue nevi which were reviewed. Pathological diagnoses were confirmed by two pathologists (SRD and GE). All specimens were bleached with potassium permanganate and tissue permitting, immunohistochemical stains, namely SOX10 (MilliporeSigma, Darmstadt, Germany) and CD68 (Leica Biosystems, Nussloch, Germany), were obtained.
Data Collection
Demographic information for each patient was collected, including age, gender, and ethnicity. Recorded medical history included a history of previous cancers, age at the discovery of the lesion, suspected diagnosis pre-lesion excision, the size of the lesion, color, focality, pathologic findings, and clinical course.
Statistical Analysis
All statistical analyses were performed using SPSS Version 22 (SPSS Inc., Chicago, Illinois USA) statistical package. Descriptives and frequencies were calculated for all aforementioned patient data.
Results
Study population
Demographics of our study population (n=23) at time of blue nevus diagnosis included a mean age of 55 years standard deviation 15.1, range 27-82 years; 42.9% (n=9) were female; 71.4% (n=15) self-identified as white and 38.1% (n=8) as Hispanic (Table 1). Two patients had a previous history of cancer; one had a previous history of a plantar melanoma suspicious of metastasis (patient 11, Table 1). She later developed a papillary thyroid carcinoma which was excised. In this patient, the lesion was initially debulked and a year later definitive removal was completed. The lesion has not recurred within the 8.5 years of follow up of the re-excision. The other patient had a history of lymphoma and was undergoing chemotherapy at the time of presentation, (patient 12, Table 1). He was lost to follow up after 8 months.
Table 1.
Demographics and clinical characteristics of conjunctival blue nevus study population.
| Pt | Age (years) | Gender | Location | Pre-excision diagnosis | Race Ethnicity |
Size mm* |
|---|---|---|---|---|---|---|
| 1 | 63 | M | Palpebral | Benign | Black/NH | 2.5×1.5 |
| 2 | 82 | M | Palpebral | PAM | White/NH | 4×2.5 |
| 3 | 56 | M | Palpebral | Melanoma | White/H | 5×1 |
| 4 | 58 | F | Inferior fornix | PAM | – | 2×1 |
| 5 | 32 | M | Bulbar | Incidental with PKP | White/H | 3×1 |
| 6 | 30 | M | Bulbar | Benign | White/NH | 2×3 |
| 7 | 61 | F | Bulbar | Melanoma | White/NH | 10×8 |
| 8 | 43 | F | Bulbar | Melanoma | White/H | 4×2 |
| 9 | 27 | M | Bulbar | Nevus | – | 3×2 |
| 10 | 58 | F | Bulbar | Melanoma | White/NH | 4×3 |
| 11* | 79 | F | Bulbar/episcleral | Metastatic melanoma | White/H | 6.5×5 |
| 12* | 65 | M | Bulbar | Melanocytosis | Black/NH | 3×1 |
| 13 | 58 | F | Bulbar | Incidental with RD repair | – | 3×1 |
| 14 | 65 | F | Bulbar | Incidental with scleral buckle removal | White/NH | 5.5×2.5 |
| 15 | 42 | F | Bulbar | Incidental with pterygium | White/H | 0.5×0.5 |
| 16 | 45 | M | Bulbar | Incidental with PKP | White/NH | 7×4 |
| 17 | 57 | M | Bulbar | Incidental with pterygium | White/H | 6×1 |
| 18 | 52 | F | Bulbar | Incidental with pterygium | White/H | 2.5×2 |
| 19 | 39 | M | Caruncle | Incidental with nasolacrimal duct surgery | White/NH | 2×1 |
| 20 | 63 | M | Caruncle | Nevus vs melanosis | – | 3×2 |
| 21 | 71 | M |
Conjunctiva at limbus OS Inferior Fornix OS Inferior Fornix OD |
PAM | White/H | 1.5×1 3×2.5 3×3 |
Pt=patient; M=male; F=female, H=Hispanic; NH=non-Hispanic; PAM=primary acquired melanosis; PKP=penetrating keratoplasty; RD=retinal detachment
by pathology report; – information not available
Patients with previous or concurrent history of cancer
Clinical characteristics
All individuals but 1 had a solitary blue nevus on the ocular surface (Table 1); one white Hispanic male had 3 blue nevi on his conjunctiva. One patient had a nevus of Ota Of the 23 lesions, 3 were on the palpebral conjunctiva, 3 in the inferior fornix (Figure 1), 13 on the bulbar conjunctiva, 2 on the caruncle, 1 episcleral and 1 at the limbus (Figure 2). Eight patients had color photographs available for review, which demonstrated lesions of various sizes and colors. Seven lesions were flat as demonstrated by Figure 1; 1 was nodular as demonstrated by Figure 3. Two lesions were light brown in color, 3 moderately brown (Figure 1), and 4 deeply brown-black (Figure 3–4).
Figure 1.
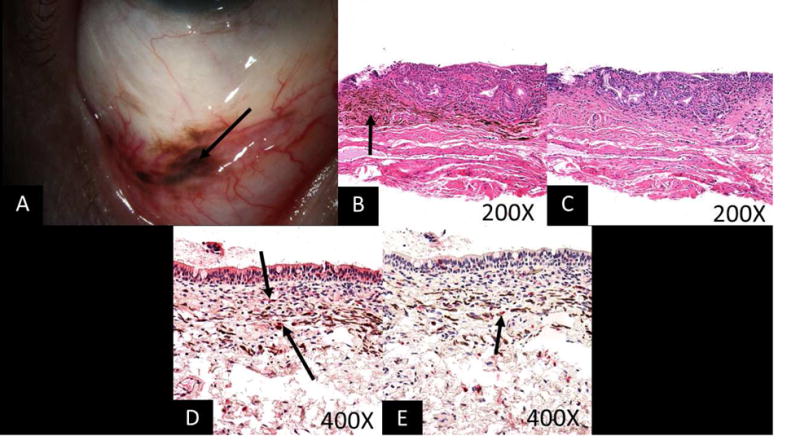
Images from a 71 year old white Hispanic male A. Slit lamp photograph showing moderately pigmented lesions in the forniceal and adjacent palpebral and bulbar conjunctiva (arrow). B. Photomicrograph reveals densely pigmented spindled melanocytes containing copious intracytoplasmic pigment, consistent with blue nevus (arrow) (stain, hematoxylin–eosin; original magnification, ×200). C. Photomicrograph demonstrates removal of melanin pigment with bleach and morphologically benign dendritic cells lacking prominent nucleoli (stain, permanganate bleach; original magnification, ×200). D. Photomicrograph demonstrating SOX10 staining (arrow) within the dendritic pigmented melanocytes (stain, SOX10 immunostain with red chromagen; original magnification, ×400) E. Photomicrograph demonstrating CD68 positive melanophages (arrow) interspersed with the dendritic melanocytes (stain, CD68 immunostain with red chromagen; original magnification, ×400).
Figure 2.
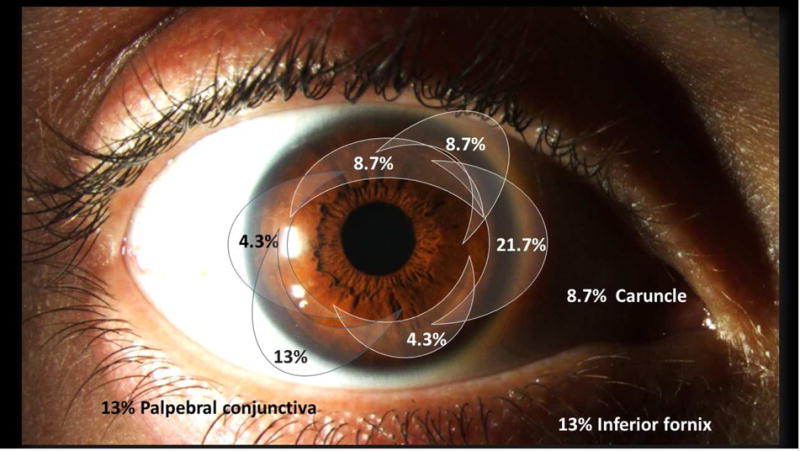
Distribution of the 23 blue nevi on the ocular surface in this series. Of 23 lesions, 5 were nasal (21.7%), 2 supero-nasal (8.7%), 1 infero-nasal (4.3%), 1 temporal (4.3%), 3 infero-temporal (13%) and 2 were superior (8.7%). Other lesion locations including 3 on palpebral conjunctiva (13%), 2 on the caruncle (8.7%), and 3 in the inferior fornix (13%). One lesion (4.3%) was in an unknown quadrant, found incidentally in a specimen taken during retinal detachment surgery.
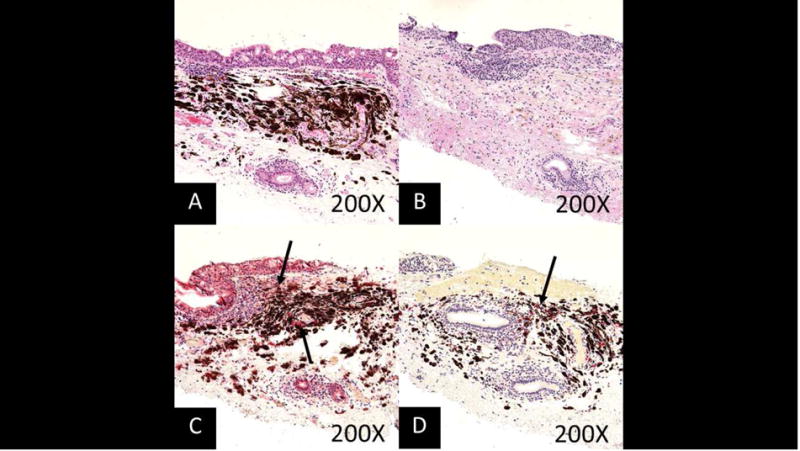
Figure 3.
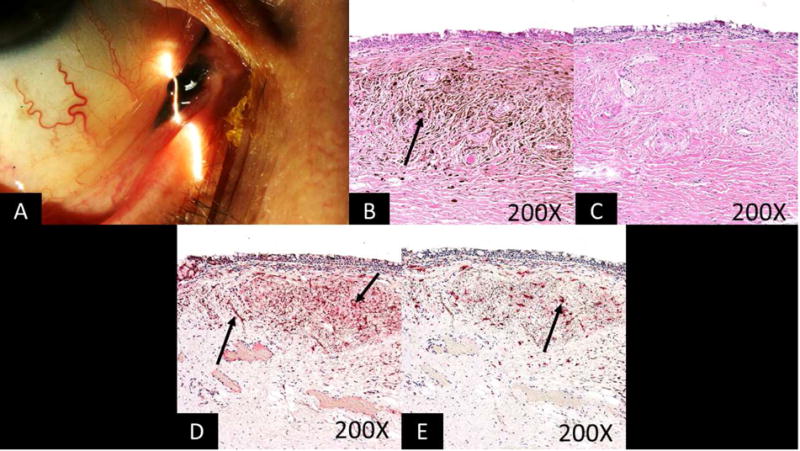
Images from a 61 year old white non-Hispanic female A. Slit lamp image of the right eye showing a darkly pigmented, nodular lesion at the plica semilunaris which had been present for 20 years. Melanoma was suspected prior to removal. B. Photomicrograph revealing plump variably spindle shaped melanocytes and numerous melanophages (arrow) consistent with blue nevus (stain, hematoxylin–eosin; original magnification, ×200). C. Photomicrograph demonstrates removal of the melanin pigment with bleach and morphologically benign variably dendritic cells lacking prominent nucleoli. (stain, permanganate bleach; original magnification, ×200). D. Photomicrograph demonstrating SOX10 staining (arrows) within the dendritic pigmented melanocytes (stain, SOX10 immunostain with red chromagen; original magnification, ×200). E. Photomicrograph demonstrating CD68 positive melanophages (arrow) interspersed with the dendritic melanocytes (stain, CD68 immunostain with red chromagen; original magnification, ×200).
Figure 4.
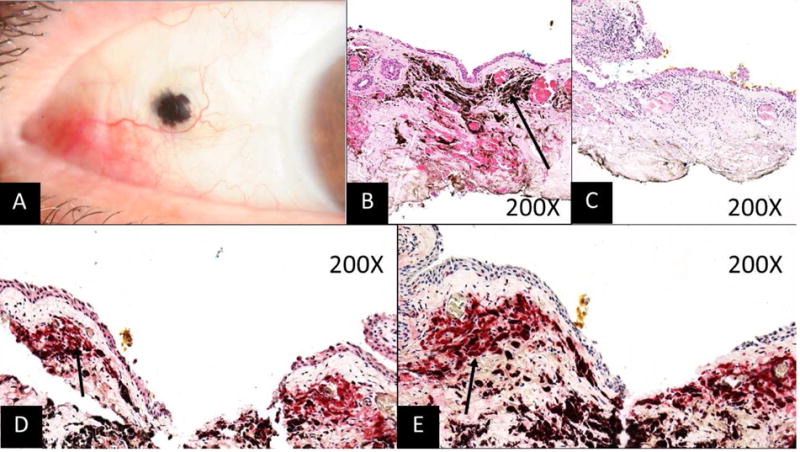
Images from a 79 year old white Hispanic female A: Slit-lamp photograph of the right eye showing a dark brown, flat lesion. Metastasis from a known plantar melanoma was suspected prior to removal. B: Photomicrograph demonstrates heavily pigmented dendritic shaped melanocytes and melanophages within the substantia propria (arrow) consistent with a blue nevus (stain, hematoxylin–eosin; original magnification, ×200). C: Photomicrograph demonstrates removal of melanin pigment with bleach and morphologically benign dendritic melanocytes and macrophages (stain, permanganate bleach; original magnification, ×200). D: Photomicrograph demonstrating SOX10 staining (arrow) within the dendritic shaped melanocytes (stain, SOX10 immunostain with red chromagen; original magnification, ×200). E: Photomicrograph demonstrating CD68 positive melanophages (arrow) interspersed with the dendritic melanocytes (stain, CD68 immunostain with red chromagen; original magnification, ×200).
Initial diagnosis
Eight patients were excised with a pre-biopsy suspicion of a pre-malignant or malignant condition (4 thought to be primary conjunctival melanoma, 1 metastatic melanoma from a prior plantar melanoma, and 3 primary acquired melanosis). The lesions in 5 patients were thought to be benign prior to removal (2 were suspected to be nevi, 1 congenital acquired melanosis, 1 ocular melanocytosis, and 1 an unknown but benign pigmented lesion). Eight lesions were removed incidentally during other ocular procedures.
Surgical technique
The method of removal of the nevus was based on the clinical index of suspicion. Lesions suspected to be benign were removed with margins of 2 mm. Conjunctival lesions suspected of malignancy had margins of at least 4 millimeters, edges were treated with double freeze/slow thaw cryotherapy, followed by closure with or without amniotic membrane graft. Episcleral lesions had 2mm margins taken. A “no touch” technique as proposed by Shields et al was employed.23, 24
Histology
Two patients (9.5%) were found to have cellular blue nevi while the remaining 90.5% had simple blue nevi (Figure 1,4–5). The spindle shaped nevus cells were typically found in the substantia propria (n=23). All specimens were bleached with potassium permenganate. Thirteen patients had sections stained with immunostaining of SOX10 and CD68. The remaining lesions were unable to be stained due to exhausted tissue blocks. Figures (1, 3–5) illustrate the immunostaining.
Figure 5.
Images from a 58 year old white non Hispanic female with a lesion on the tarsal conjunctiva A. Photomicrograph demonstrating densely pigmented plump dendritic shaped melanocytes and melanophages within the substantia propria (stain, hematoxylin-eosin ; original magnification, ×200). B. Photomicrograph demonstrating removal of melanin pigment with bleach and morphologically benign variably dendritic cells lacking prominent nucleoli (stain, permanganate bleach; original magnification, ×200). C. Photomicrograph demonstrating SOX10 (arrows) staining within the dendritic pigmented melanocytes (stain, SOX10 immunostain with red chromagen; original magnification, ×200). D. Photomicrograph demonstrating CD68 positive melanophages (arrow) interspersed with the dendritic melanocytes (stain, CD68 immunostain with red chromagen; original magnification, ×200).
Course
Despite differences in surgical technique, over a mean follow up of 20.2 months (± 28, range 2 weeks to 103 months), but no malignant transformations occurred in any patient. One patient (case 11) initially presented with a deep conjunctival/episcleral lesion. The lesion was debulked and MelanA and SOX10 demonstrated staining consistent with a blue nevus. The lesion was morphologically benign with no evidence of prominent nucleoli, mitotic activity or nuclear pleomorphism. The margins were positive. One year later the lesion was further excised and again showed a benign melanocytic lesion consistent with a blue nevus. The lesion has not recurred with 8.5 years of follow up.
Discussion
To summarize, we found that blue nevus of the conjunctiva presented most often in older, white males. While the nevus is considered congenital,22 its clinical diagnosis in the eye did not occur until on average the 5th decade of life. This is in line with other reports of blue nevus of the conjunctiva where the mean age at diagnosis was 52 years (range 30-93, n=11).1, 7, 13–21 Blue nevi appear to present at an older age in the eye than the skin where individuals are usually diagnosed at an age younger than 40.2, 3 Males outnumbered females in our population which is the reverse of what has been described in prior reports from the eye (where males represented 46% of the population)1, 7, 13–21 and skin (where reported female:male ratios ranged from 2.24 to 8.5:125).
Regarding the clinical presentation, we found that the majority of lesions presented on the bulbar conjunctiva but were also distributed in other locations, as has been described in other publications of blue nevus of the conjunctiva.1, 7, 13–21 In the skin, blue nevi commonly present in the pre-sacral area, the head and neck, and the dorsal extremities26, but can also be found in a wide range of other locations.27–37 Multifocal lesions were not common in our sample and similarly, represented the minority of cases in prior series (27.3%, n=3/117, 17, 20 in the eye; 6.5%, n=13/20025 in the skin). In the skin, multifocal blue nevi may be associated with lentigenes, atrial myxomas, mucocutaneous myxomas, and blue nevi (LAMB)38 syndrome found in association with the Carney Complex.
Regarding the clinical diagnosis, 8 cases in our series were suspected to be malignant or pre-malignant. This is not unexpected as blue nevi on the ocular surface can mimic other melanocytic lesions in location and appearance, such as nevocellular nevi, racial melanosis, primary acquired melanosis and melanoma (Table 3). Due to the lack of the Tyndall effect, they can appear in any shade of brown or black and can vary in size. This is less of a concern in the skin where common blue nevi are generally not confused with melanoma. However, cellular blue nevi of the skin can have a nodular appearance and are usually larger than simple blue nevi so these lesions can be misdiagnosed as a malignancy.39 Given the overlapping presenting characteristics between blue nevi, congenital acquired melanosis, primary acquired melanosis, and melanoma, a biopsy with histologic analysis is needed when malignancy is suspected. Eight lesions were found incidentally after conjunctival removal in the setting of pterygium surgery, retinal detachment repair, and corneal transplantation. These were all benign, fully removed and needed no further intervention. As in our cases, prior reports have described blue nevi that were incidentally discovered after surgery for retinal detachment14 and a pyogenic granuloma.18
Table 3.
Clinicopathologic features of conjunctival blue nevi and differential diagnosis
| Lesion | Location | Histological characteristics | Bleach | Sox 10/Melan A | CD68 | Clinical characteristics |
|---|---|---|---|---|---|---|
| Blue nevus | Substantia propria | Dendritic, heavily pigmented spindle shaped melanocytes, morphologically benign, lack prominent nucleoli, have accompanying melanophages. | Bleaching shows cellular detail | Positive | Positive with surrounding melanophages | Congenital, may be discovered at later age. Usually dark, but may vary in shade and color. |
| Nevocellular nevus | Epithelium (Junctional nevus), Subepithelial, or both (Compound nevus) | Melanocytes with variable pigmentation that are present within the epithelium at a young age and migrate into the substantia propria over time. Epithelial cysts are common. Lack nucleoli and mitotic activity. | Bleaching shows cellular detail | Positive | Usually Negative | Congenital, cystic, may change in size with age and hormonal changes. |
| C-MIN/PAM without atypia | Epithelium | Acquired intraepithelial melanocytes with variable pigmentation in the basal epithelium. No atypia. | Bleaching shows cellular detail | Positive | Negative | Acquired, usually near limbus, can appear as light epithelial pigment dusting. |
| C-MIN/PAM with atypia | Epithelium | Melanocytes show signs of atypia including condensed nuclei with perinuclear clearing, prominent nucleoli, pleomorphism and migration into superficial epithelium. | Bleaching shows cellular detail | Positive | Negative | Acquired, usually near limbus, can appear as light epithelial pigmented dusting. |
| Melanoma in situ | Epithelium (full thickness) | Morphologically similar to PAM with atypia/C-MIN with full thickness involvement of the epithelium without extension into the substantia propria. | Bleaching shows cellular detail | Positive | Negative | Acquired, dark, irregular borders, and often history of prolonged sun exposure. |
| Invasive melanoma | Epithelium invading into substantia propria | Melanocytes with atypia including condensed nuclei with perinuclear clearing, prominent nucleoli, mitotic activity, pleomorphism, extension through the basement membrane into the underlying substantia propria. | Bleaching shows cellular detail | Positive | Negative within tumor, may be positive in surrounding macrophages | Acquired, dark, irregular borders, nodular and often history of prolonged sun exposure |
| Extraocular extension of uveal melanoma | Extending through sclera into substantia propria | Spindle and epithelioid cells with prominent nucleoli and mitotic figures. Typically, with no epithelial involvement. Often evidence of involvement at deep aspect of excised tissue and history of uveal melanoma. | Bleaching shows cellular detail | Positive | Negative within tumor, may be positive in surrounding macrophages | Acquired, dark, subconjunctival, immobile lesion with irregular borders. Extension confirmed with B-scan ultrasound. |
| Pigmented ocular surface squamous neoplasia | Epithelium +/− invasion into substantia propria | Atypical epithelial proliferation, may show pigmented dendritic melanocytes in epithelium which lack morphological atypia. | Bleaching shows cellular detail | Positive for dendritic melanocytes in epithelium | Negative | Opalescent lesions, can be pigmented in patients with tan/dark complexion. |
| Foreign body | Variable location | Variable appearance depending on foreign material/ink. | Does not typically bleach. Iron stain helpful for demonstrating hemosiderin. | Negative | Variably positive if macrophages engulfing foreign material | Variable presentation. |
C-MIN: conjunctival melanocytic intraepithelial neoplasia; PAM: primary acquired melanosis
Typical histological features of blue nevi include dendritic spindle shaped, heavily pigmented cells with variable amounts of melanin and histocytes (melanophages) present within the dermis/substantia propria. Bleaching with potassium permanganate confirms that the intracellular pigment is melanin and allows for morphological evaluation of cellular features. SOX10 is a transcription factor involved in neural crest development which can be targeted with an antibody stain to identify melanocytes and demonstrate melanocytic differentiation. Similarly, MelanA targets melanocytic cells. CD68 is a marker for tissue histiocytes including melanophages which are often present in blue nevi.
The differential diagnosis of a pigmented lesion on the ocular surface includes, nevocellular nevi, primary acquired melanosis with or without atypia (PAM), conjunctival melanoma in situ (C-MIN), invasive conjunctival melanoma, extraocular extension of a ciliary body melanoma, pigmented squamous carcinoma in situ/invasive carcinoma, and foreign body (Table 3)40. These entities are best differentiated by history, clinical examination, and careful pathological examination.
With regard to location, blue nevi are present in the substantia propria, while junctional nevi, PAM, C-MIN, and pigmented intraepithelial squamous tumors are present exclusively in the epithelium. Sub-epithelial nevi, compound nevi, will have morphologically benign melanocytes present in the substantia propria. Invasive melanoma, and extraocular extension of uveal melanoma will have atypical melanocytes present in the substantia propria. Pigmented squamous cell carcinoma may show dendritic melanocytes lacking morphological atypia within a thickened atypical epithelial proliferation and within the substantia propria. (Table 3).
Clinically, benign nevi appear regular in shape, cystic and discovered at a younger age. PAM and C-MIN40 have acquired superficial epithelial conjunctival pigmentation. Pigmented squamous carcinomas have features of ocular surface squamous neoplasia such as thickened epithelium, keratinization, and/or opalescence. All lesions containing melanocytes will stain positive for SOX10 and MelanA, including pigmented squamous carcinoma41, 42 and surrounding histiocytes that engulf pigment will stain positive for CD68. This is valuable in excluding the phenomenon of pigment incontinentia and foreign pigmented material.
Pathologically, as in prior reports,1, 7, 13–21 most of the lesions in this study were of the simple type and only two were found to be cellular.7, 13, 14, 17, 19 While none of our patients experienced malignant transformation, this has been described in 1 patient with a cellular blue nevus of the conjunctiva.19 This situation is very rare, as malignant transformation does not often occur in the setting of a blue nevus. Malignant transformation of blue nevi has been reported in the orbit,43, 44 occasionally in the setting of a nevus of Ota.13, 45
While usually isolated, blue nevi have been associated with Carney Complex,46, 47 a rare hereditary condition associated with myxomas, blue nevi, endocrine tumors and other mucocutaneous lentigines. None of the patients had this complex, but two of the patients in this series did have other malignancies. One patient was a 79 year old woman who had a history of a plantar melanoma raising the question of a metastasis prior to excision, as well as a concurrent thyroid carcinoma. The other was a 65 year old black man with a history of lymphoma and undergoing chemotherapy.
As in all studies, our findings must be interpreted while considering our study limitations which include a retrospective design with limited patient numbers. However, as blue nevus of the conjunctiva is rare, our case series is the largest to date. To conclude, we found that blue nevus of the conjunctiva can be confused with other melanocytic lesions of the conjunctiva. Histologic confirmation is needed to make the diagnosis but when made, the patient can be assured that the clinical prognosis is excellent.
Blue nevus is a melanocytic tumor that is commonly described in the skin. In the conjunctiva, it can be clinically misdiagnosed as a malignancy. We present a series emphasizing typical characteristics, histopathologic findings and course.
Acknowledgments
Financial support: Supported by the Florida Lions Eye Bank (Dr Dubovy), the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Clinical Sciences Research EPID-006-15S (Dr. Galor), R01EY026174 (Dr. Galor), NIH Center Core Grant P30EY014801 and Research to Prevent Blindness Unrestricted Grant, The Ronald and Alicia Lepke Grant, The Lee and Claire Hager Grant, The Elaine and Robert Baer Grant, The H. Scott Huizenga Grant, The Emilyn Page and Mark Feldberg Grant, The Gordon Charitable Foundation and the Richard Azar Family Grant (Dr. Karp/institutional grants).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Meeting presentation: American Academy of Ophthalmology Annual Meeting, 2016
Conflicts of interest: No conflicting relationship exists for any author
References
- 1.Kirzhner M, Jakobiec FA, Kim N. Focal Blue Nevus of the Eyelid Margin (Mucocutaneous Junction): A Report of a Unique Case With a Review of the Literature. Ophthalmic Plastic & Reconstructive Surgery. 2011;27(5):338–42. doi: 10.1097/IOP.0b013e318213f743. [DOI] [PubMed] [Google Scholar]
- 2.Murali R, McCarthy SW, Scolyer RA. Blue nevi and related lesions: a review highlighting atypical and newly described variants, distinguishing features and diagnostic pitfalls. Adv Anat Pathol. 2009;16(6):365–82. doi: 10.1097/PAP.0b013e3181bb6b53. [DOI] [PubMed] [Google Scholar]
- 3.Zembowicz A, Phadke PA. Blue nevi and variants: an update. Archives of pathology & laboratory medicine. 2011;135(3):327–36. doi: 10.5858/2009-0733-RA.1. [DOI] [PubMed] [Google Scholar]
- 4.Rodriguez HA, Ackerman LV. Cellular blue nevus. Clinicopathologic study of forty-five cases. Cancer. 1968;21(3):393–405. doi: 10.1002/1097-0142(196803)21:3<393::aid-cncr2820210309>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 5.Jakobiec FA, Colby K, Bajart AM, et al. Immunohistochemical studies of atypical conjunctival melanocytic nevi. Archives of ophthalmology. 2009;127(8):970–80. doi: 10.1001/archophthalmol.2009.171. [DOI] [PubMed] [Google Scholar]
- 6.González-Cámpora R, Galera-Davidson H, Vázquez-Ramírez FJ, Díaz-Cano S. Blue nevus: classical types and new related entities. A differential diagnostic review. Pathology, Research and Practice. 1994;190(6):627–35. doi: 10.1016/S0344-0338(11)80402-4. [DOI] [PubMed] [Google Scholar]
- 7.Blicker JA, Rootman J, White VA. Cellular blue nevus of the conjunctiva. Ophthalmology. 1992;99(11):1714–7. doi: 10.1016/s0161-6420(92)31742-7. [DOI] [PubMed] [Google Scholar]
- 8.Baran JL, Duncan LM. Combined melanocytic nevi: histologic variants and melanoma mimics. Am J Surg Pathol. 2011;35(10):1540–8. doi: 10.1097/PAS.0b013e31822e9f5e. [DOI] [PubMed] [Google Scholar]
- 9.Crawford JB, Howes EL, Jr, Char DH. Combined nevi of the conjunctiva. Arch Ophthalmol. 1999;117(9):1121–7. [PubMed] [Google Scholar]
- 10.Grossniklaus HE, Green WR, Luckenbach M, Chan CC. Conjunctival lesions in adults. A clinical and histopathologic review. Cornea. 1987;6(2):78–116. doi: 10.1097/00003226-198706020-00002. [DOI] [PubMed] [Google Scholar]
- 11.Gerner N, Norregaard JC, Jensen OA, Prause JU. Conjunctival naevi in Denmark 1960–1980. A 21-year follow-up study. Acta Ophthalmol Scand. 1996;74(4):334–7. doi: 10.1111/j.1600-0420.1996.tb00703.x. [DOI] [PubMed] [Google Scholar]
- 12.Shields CL, Fasiuddin AF, Fasiudden A, et al. Conjunctival nevi: clinical features and natural course in 410 consecutive patients. Archives of Ophthalmology. 2004;122(2):167–75. doi: 10.1001/archopht.122.2.167. [DOI] [PubMed] [Google Scholar]
- 13.Speakman JS, Phillips MJ. Cellular and malignant blue nevus complicating oculodermal melanosis (nevus of Ota syndrome) Can J Ophthalmol. 1973;8(4):539–47. [PubMed] [Google Scholar]
- 14.Smith TR, Brockhurst RJ. Cellular blue nevus of the sclera. Arch Ophthalmol. 1976;94(4):618–20. doi: 10.1001/archopht.1976.03910030302010. [DOI] [PubMed] [Google Scholar]
- 15.Boudet C, Arnaud B, Pincemin D, Navarre L. Blue nevus localized in the limbus: anatomical evolution and therapeutic approach. Bulletin Des Sociétés D’ophtalmologie De France. 1977;77(8–9):867–70. [PubMed] [Google Scholar]
- 16.Eller AW, Bernardino VB. Blue nevi of the conjunctiva. Ophthalmology. 1983;90(12):1469–71. doi: 10.1016/s0161-6420(83)34359-1. [DOI] [PubMed] [Google Scholar]
- 17.Holbach L, Nagel G, Naumann GO. Blue nevi of the conjunctiva. Klin Monbl Augenheilkd. 1994;205(4):242–3. doi: 10.1055/s-2008-1045521. [DOI] [PubMed] [Google Scholar]
- 18.Tucker SM, Linberg JV, Doshi HM. Conjunctival blue nevus associated with pyogenic granuloma. Can J Ophthalmol. 1994;29(2):95–6. [PubMed] [Google Scholar]
- 19.Demirci H, Shields CL, Shields JA, Eagle RC. Malignant melanoma arising from unusual conjunctival blue nevus. Archives of Ophthalmology. 2000;118(11):1581–4. doi: 10.1001/archopht.118.11.1581. [DOI] [PubMed] [Google Scholar]
- 20.Berman EL, Shields CL, Sagoo MS, et al. Multifocal Blue Nevus of the Conjunctiva. Survey of Ophthalmology. 2008;53(1):41–9. doi: 10.1016/j.survophthal.2007.10.009. [DOI] [PubMed] [Google Scholar]
- 21.Jakobiec FA, Nguyen J, Bhat P, Fay A. Recurrent blue nevus of the corneoscleral limbus. Cornea. 2010;29(8):947–51. doi: 10.1097/ICO.0b013e3181ca6d1b. [DOI] [PubMed] [Google Scholar]
- 22.Folberg R, Jakobiec FA, Bernardino VB, Iwamoto T. Benign conjunctival melanocytic lesions. Clinicopathologic features. Ophthalmology. 1989;96(4):436–61. doi: 10.1016/s0161-6420(89)32878-8. [DOI] [PubMed] [Google Scholar]
- 23.Shields JA, Shields CL, De Potter P. Surgical management of conjunctival tumors. The 1994 Lynn B. McMahan Lecture. Arch Ophthalmol. 1997;115(6):808–15. doi: 10.1001/archopht.1997.01100150810025. [DOI] [PubMed] [Google Scholar]
- 24.Shields CL, Shields JA. Tumors of the conjunctiva and cornea. Survey of Ophthalmology. 2004;49(1):3–24. doi: 10.1016/j.survophthal.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 25.Dorsey CS, Montgomery H. Blue nevus and its distinction from Mongolian spot and the nevus of Ota. J Invest Dermatol. 1954;22(3):225–36. doi: 10.1038/jid.1954.28. [DOI] [PubMed] [Google Scholar]
- 26.Zimmermann AA, Cornbleet T. The development of epidermal pigmentation in the Negro fetus. J Invest Dermatol. 1948;11(5):383–95. [PubMed] [Google Scholar]
- 27.Vidal S, Sanz A, Hernandez B, et al. Subungual blue naevus. Br J Dermatol. 1997;137(6):1023–5. doi: 10.1111/j.1365-2133.1997.tb01580.x. [DOI] [PubMed] [Google Scholar]
- 28.Hasse CD, Zoutendam GL, Gombas OF. Intraoral blue (Jadassohn-Tieche) nevus. Oral Surg Oral Med Oral Pathol. 1978;45(5):755–61. doi: 10.1016/0030-4220(78)90151-2. [DOI] [PubMed] [Google Scholar]
- 29.Chuang WY, Hao SP, Yeh CJ, Jung SM. Blue nevi of the sinonasal mucosa: a report of two cases and review of the literature. Laryngoscope. 2007;117(2):371–2. doi: 10.1097/01.mlg.0000244372.24116.9f. [DOI] [PubMed] [Google Scholar]
- 30.Ferrara G, Boscaino A, De Rosa G. Bronchial blue naevus. A previously unreported entity. Histopathology. 1995;26(6):581–3. doi: 10.1111/j.1365-2559.1995.tb00281.x. [DOI] [PubMed] [Google Scholar]
- 31.Lam KY, Law S, Chan GS. Esophageal blue nevus: an isolated endoscopic finding. Head Neck. 2001;23(6):506–9. doi: 10.1002/hed.1068. [DOI] [PubMed] [Google Scholar]
- 32.Epstein JI, Erlandson RA, Rosen PP. Nodal blue nevi. A study of three cases. Am J Surg Pathol. 1984;8(12):907–15. doi: 10.1097/00000478-198412000-00003. [DOI] [PubMed] [Google Scholar]
- 33.Fitzhugh VA, Houck K, Heller DS. Vaginal blue nevus: report of a case and review of the literature. J Low Genit Tract Dis. 2011;15(4):325–7. doi: 10.1097/LGT.0b013e318213f3b8. [DOI] [PubMed] [Google Scholar]
- 34.Zevallos-Giampietri EA, Barrionuevo C. Common blue nevus of the uterine cervix: case report and review. Appl Immunohistochem Mol Morphol. 2004;12(1):79–82. doi: 10.1097/00129039-200403000-00015. [DOI] [PubMed] [Google Scholar]
- 35.Shintaku M, Tsuta K, Matsumoto T. Blue nevus of the endometrium. Int J Gynecol Pathol. 2003;22(3):294–6. doi: 10.1097/01.PGP.0000070847.25718.DE. [DOI] [PubMed] [Google Scholar]
- 36.de Giorgi V, Massi D, Brunasso G, et al. Eruptive multiple blue nevi of the penis: a clinical dermoscopic pathologic case study. J Cutan Pathol. 2004;31(2):185–8. doi: 10.1111/j.0303-6987.2004.00153.x. [DOI] [PubMed] [Google Scholar]
- 37.Martinez Martinez CJ, Garcia Gonzalez R, Castaneda Casanova AL. Blue nevus of the prostate: report of two new cases with immunohistochemical and electron-microscopic studies. Eur Urol. 1992;22(4):339–42. doi: 10.1159/000474783. [DOI] [PubMed] [Google Scholar]
- 38.Rhodes AR, Silverman RA, Harrist TJ, Perez-Atayde AR. Mucocutaneous lentigines, cardiomucocutaneous myxomas, and multiple blue nevi: the “LAMB” syndrome. J Am Acad Dermatol. 1984;10(1):72–82. doi: 10.1016/s0190-9622(84)80047-x. [DOI] [PubMed] [Google Scholar]
- 39.Sugianto JZ, Ralston JS, Metcalf JS, et al. Blue nevus and “malignant blue nevus:” A concise review. Semin Diagn Pathol. 2016;33(4):219–24. doi: 10.1053/j.semdp.2016.04.006. [DOI] [PubMed] [Google Scholar]
- 40.Damato B, Coupland SE. Conjunctival melanoma and melanosis: a reappraisal of terminology, classification and staging. Clin Exp Ophthalmol. 2008;36(8):786–95. doi: 10.1111/j.1442-9071.2008.01888.x. [DOI] [PubMed] [Google Scholar]
- 41.Shields CL, Manchandia A, Subbiah R, et al. Pigmented squamous cell carcinoma in situ of the conjunctiva in 5 cases. Ophthalmology. 2008;115(10):1673–8. doi: 10.1016/j.ophtha.2008.01.020. [DOI] [PubMed] [Google Scholar]
- 42.Mikami T, Furuya I, Kumagai A, et al. Pigmented squamous cell carcinoma of oral mucosa: clinicopathologic study of 3 cases. J Oral Maxillofac Surg. 2012;70(5):1232–9. doi: 10.1016/j.joms.2011.03.048. [DOI] [PubMed] [Google Scholar]
- 43.Gündüz K, Shields JA, Shields CL, Eagle RC. Periorbital cellular blue nevus leading to orbitopalpebral and intracranial melanoma. Ophthalmology. 1998;105(11):2046–50. doi: 10.1016/S0161-6420(98)91122-8. [DOI] [PubMed] [Google Scholar]
- 44.Odashiro AN, Arthurs B, Pereira PR, et al. Primary orbital melanoma associated with a blue nevus. Ophthal Plast Reconstr Surg. 2005;21(3):247–8. doi: 10.1097/01.iop.0000161716.46032.90. [DOI] [PubMed] [Google Scholar]
- 45.Buntinx-Krieg T, Ouyang J, Cartwright M. An Orbital Malignant Melanoma Arising in Cellular Blue Nevus in a Patient with Nevus of Ota. Cureus. 2016;8(7):e698. doi: 10.7759/cureus.698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cohen C, Turner ML, Stratakis CA. Pigmented lesions of the conjunctiva in Carney’s complex. J Am Acad Dermatol United States. 2000;42 doi: 10.1016/s0190-9622(00)90027-6. [DOI] [PubMed] [Google Scholar]
- 47.Stratakis CA, Kirschner LS, Carney JA. Clinical and molecular features of the Carney complex: diagnostic criteria and recommendations for patient evaluation. J Clin Endocrinol Metab. 2001;86(9):4041–6. doi: 10.1210/jcem.86.9.7903. [DOI] [PubMed] [Google Scholar]


