Abstract
Background
We estimated annual burden and costs of hospitalization in patients with chronic gastrointestinal and liver diseases, and identified characteristics of high-need, high-cost patients, in a nationally representative sample.
Methods
Using Nationwide Readmissions Database 2013, we identified patients with at least 1 hospitalization between January-June 2013, and a diagnosis of inflammatory bowel diseases (IBD), chronic liver diseases (CLDs), functional gastrointestinal disorders (FGIDs), gastrointestinal hemorrhage, or pancreatic diseases, with 6 months or more of follow up. We calculated days spent in hospital/month and estimated costs of entire cohort, and identified characteristics of high-need, high-cost patients (top decile of days spent in hospital/month).
Results
Patients with IBD (n=47,402), CLDs (n=376,810), FGIDs (n=351,583), gastrointestinal hemorrhage (n=190,881), or pancreatic diseases (n=98,432), hospitalized at least once, spent a median of 6–7 days (inter-quartile range, 3–14) in the hospital each year (total for all diseases). Compared to patients in the lowest decile (median 0.13–0.14 days/month spent in the hospital), patients in the highest decile spent a median 3.7–4.1 days/month in hospital (total for all diseases), with hospitalization costs ranging from $7502/month to $8925/month and 1 hospitalization every 2 months. Gastrointestinal diseases, infections, and cardiopulmonary causes were leading reasons for hospitalization of these patients. Based on multivariate logistic regression, ‘high-need, high-cost’ patients were more likely to have Medicare/Medicaid insurance, lower income status, index hospitalization in a large rural hospital, high comorbidity burden, obesity and infection-related hospitalization.
Conclusions
In a nation-wide database analysis of patients with IBD, CLD, FGID, gastrointestinal hemorrhage or pancreatic diseases hospitalized at least once, we found that a small fraction of high-need, high-cost patients contribute disproportionately to hospitalization costs. Population health management directed towards these patients would facilitate high value care.
Keywords: healthcare spending, utilization, population health management, high risk
INTRODUCTION
Gastrointestinal and liver diseases are prevalent, expensive and contribute to substantial healthcare utilization in the United States. Recent estimates suggest that annually over $103 billion is spent on the management of gastrointestinal and chronic liver diseases, of which 62% is attributed to inpatient care, and 20% to ambulatory care.1 Previous cross-sectional analyses of burden of healthcare utilization with gastrointestinal and liver disease have helped identify leading causes and estimated costs of ambulatory visits, emergency department visits and hospitalizations.2,3
There is limited information on the annual burden and costs of hospitalization in patients with chronic gastrointestinal and liver diseases. Identifying patients at high risk for frequent hospitalizations and long hospital stays is imperative to improve population health and reduce healthcare costs. Metrics focusing on 30-day readmissions risk fail to capture overall burden of hospitalization from a patient as well as health system standpoint, since (a) some patients who eventually become ‘high-need, high-cost’ (HNHC) patients may not be readmitted within 30-days of index admission; (b) even among patients with 30-day readmission, there may be some who have multiple subsequent hospitalizations and others with just one-time readmission; and (c) patients may have varying lengths of hospitalization, with disproportionate costs.4,5 An alternative metric of high-value care may be ‘total days spent in hospital’, a concept developed as an outcome measure in patients with terminal illnesses.6,7 A detailed understanding of variability in hospitalization-related burden and healthcare costs of chronic gastrointestinal diseases will allow identification and characterization of HNHC patients of hospitalization-related care and facilitate population health management targeting at-risk population to decrease costs.8,9
We used the Nationwide Readmissions Database (NRD) 2013, an all-payer database of hospital inpatient stays, developed as part of the Healthcare Cost and Utilization Project (HCUP), which longitudinally captures over 85% inpatient discharges from 21 state inpatient databases, to estimate the annual burden and patterns of hospitalization in patients with five common chronic gastrointestinal and liver diseases (inflammatory bowel diseases [IBD], chronic liver diseases [CLDs], functional gastrointestinal disorders [FGIDs], gastrointestinal hemorrhage and pancreatic diseases). This database has been used to calculate rates and risk factors associated with 30-day readmissions in various conditions.10–13
METHODS
We constructed a retrospective cohort within NRD 2013 (see online supplement).14,15 This study was exempt from Institutional Review Board as the NRD is a publicly available database that contains de-identified patient information.
Study Population, Patient and Hospital Characteristics
We included all adults (age ≥18y) with ≥1 hospitalization between January–June 2013, with a primary or secondary discharge diagnosis of IBD, CLDs, FGIDs, gastrointestinal hemorrhage, or pancreatic disorders, based on International Classification of Diseases, Ninth Edition, Clinical Modification (ICD-9-CM) codes and the Clinical Classifications Software (CCS) for ICD-9-CM (eTable 1, online supplement).2 The ‘at-risk for re-hospitalization’ period was defined as the period from discharge data following any of the above gastrointestinal or liver diseases to the end of the study year, December 31, 2013 or death. We excluded patients whose index hospitalization was between July–December, 2013, were transferred from another hospital, or had missing data for length of hospital stays or charges for a given admission.
Details of reported patient and hospital characteristics in this database are shown in online supplement. Across all hospital admissions, gastrointestinal or hepatic procedures (such as endoscopy, colonoscopy, paracentesis, etc.), abdominal surgeries, blood transfusions, and parenteral or enteral nutrition were captured (eTable 1).
Outcomes Measured
We measured overall annual burden and patterns of hospitalization, using total days spent in the hospital as primary metric. Due to variability in follow-up time (depending on month of index hospitalization, when ‘at-risk for hospitalization’ time started), this was normalized and presented as per-month of follow-up (calculated by summing the “length of stay” variable, across all hospital admissions, divided by the total number of follow-up months). Hence, our primary outcome of interest was number of days spent in hospital per month, and secondary outcomes were number of all-cause hospitalizations per month and costs of hospitalization per month. Cost of hospitalizations was computed by multiplying charges for each hospitalization with the cost-to-charge ratios for each hospital for a given year, and inflation was adjusted to the year 2016. To measure variability and better characterize HNHC patients, the primary outcome (number of days spent in hospital per month) was stratified into deciles, and HNHC patients were defined as patients in the highest decile by total days spent in hospital/month, for each gastrointestinal or liver disease.
In order to understand causes of admissions in these patients, we categorized all hospitalizations as cardiac, respiratory, infections, genitourinary, gastrointestinal, endocrine/metabolic, neuropsychiatric, hematological or solid organ neoplasms, and others, based on primary CCS diagnosis codes (eTable 2).10 In order to characterize HNHC patients, we compared patient-, hospital- and index hospitalization-characteristics between patients in the lowest and highest decile of hospitalization burden, as well as procedural burden, and mortality across all admissions. Furthermore, we investigated the proportion of preventable hospital admissions by utilizing ICD9 codes for Prevention Quality Indicators (PQIs), which are a set of measures, developed by AHRQ, that can be used with hospital inpatient discharge data as a “screening tool” to identify ambulatory conditions for which high-quality, community-based outpatient care can potentially prevent hospitalization, complications, or more severe disease (eTable 3).16
Statistical analysis
Descriptive statistics were used to describe baseline demographics, hospital characteristics, and index hospitalization characteristics among the five diagnoses groups, and compared between patients using Pearson χ2 test for categorical variables and Student’s t-test for continuous variables. Categorical variables are expressed as percentages and continuous variables as median (interquartile range [IQR] and 5th to 95th percentile). We performed multivariate logistic regression, based on patient-, hospital- and index hospitalization-related factors to identify patients who eventually become HNHC patients, across different gastrointestinal conditions. Model performance was estimated using area under the receiver operating characteristic curve (AUC). All hypothesis testing was performed using a two-sided p-value with a statistical significance threshold <0.05. To account for the increased risk of a type I error with multiple statistical tests, we applied a Bonferroni adjustment. All statistical analyses were performed with Stata MP (StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP), using sample-level analysis.
RESULTS
From 14,325,172 discharge records available in NRD 2013, 10,931,271 records (8,214,048 unique patients) were available for analysis (eFigure 1). From these, we identified 47,402 patients with a primary or secondary discharge diagnosis of IBD, 376,810 patients with CLDs, 351,583 patients with FGIDs, 190,881 patients with gastrointestinal hemorrhage and 98,432 patients with pancreatic diseases, at their index hospitalization, admitted between January–June 2013. Approximately 20% patients had overlap with two or more candidate gastrointestinal or liver conditions present at index hospitalization (eTable 4). Across diseases, monthly length of hospital stay and costs were highest for patients with CLDs and FGIDs (Table 1).
Table 1.
Overall burden of hospitalizations due to common chronic gastrointestinal and liver diseases
| Diagnosis | Number of index admissions |
Total follow-up time (months) |
Days spent in the hospital |
Total number of hospital admissions |
Total charges across all hospitalizations (in dollars) |
||||
|---|---|---|---|---|---|---|---|---|---|
| Median | IQR | Median | IQR | Median | IQR | Median | IQR | ||
| Inflammatory bowel disease | 47402 | 10 | 8–11 | 6 | 3–12 | 1 | 1–2 | 12716 | 6223–27329 |
| Chronic liver diseases | 376810 | 10 | 8–11 | 7 | 3–14 | 1 | 1–2 | 20890 | 9992–44625 |
| Functional/motility disorders | 351583 | 10 | 8–11 | 7 | 3–14 | 1 | 1–2 | 23298 | 10886–48956 |
| Gastrointestinal hemorrhage | 190881 | 10 | 8–11 | 6 | 3–14 | 1 | 1–2 | 14756 | 7362–30228 |
| Pancreatic disease | 98432 | 10 | 8–11 | 6 | 3–13 | 1 | 1–2 | 12985 | 6784–27250 |
| Standardized by per month of follow-up | |||||||||
| Inflammatory bowel disease | - | - | - | 0.60 | 0.30–1.29 | 0.14 | 0.10–0.25 | 1342 | 661–2864 |
| Chronic liver diseases | - | - | - | 0.70 | 0.33–1.50 | 0.14 | 0.10–0.25 | 1606 | 786–3462 |
| Functional/motility disorders | - | - | - | 0.71 | 0.36–1.50 | 0.14 | 0.10–0.25 | 1569 | 783–3216 |
| Gastrointestinal hemorrhage | - | - | - | 0.67 | 0.33–1.45 | 0.14 | 0.10–0.25 | 1481 | 723–3324 |
| Pancreatic disease | - | - | - | 0.63 | 0.33–1.33 | 0.14 | 0.10–0.25 | 1390 | 724–2900 |
A. Inflammatory Bowel Diseases
Over a median follow-up of 10m (IQR, 8–11), 47,402 patients with IBD spent a median 6 days (IQR, 3–12) in the hospital annually (median, 0.60 days/month [IQR, 0.30–1.29]), with median hospitalization costs of $12,716 (IQR, 6,223–27,329) (Table 1).
Hospitalization burden by deciles
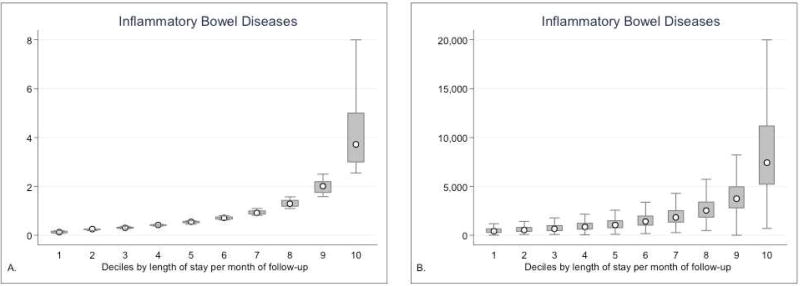
As compared to median 0.13 days/month spent in hospital in the lowest decile (IQR, 0.10–0.17) with hospitalization cost of $427/month (IQR, 291–662), patients in the highest decile (HNHC patients, defined as patients in the highest decile by total days spent in hospital/month, n=4,717) spent 3.71 days/month in the hospital (IQR, 3.00–5.08), with hospitalization costs of $7,502/month (IQR, 5,270–11,348) (Figure 1, Table 2, eTable 5, eFigure 2A). Even within the highest decile, there was considerable variability in burden of hospitalization, with patients at the 99th centile spending 9.1 days/month in the hospital, with one hospitalization/month, at costs of $22,805/month (eFigure 3A, 4A). Cumulatively, patients in highest decile contributed to 38% of hospitalization costs, and patients in the top two deciles contributed 55% of total hospitalization costs. Based on primary discharge diagnosis, most common causes of admissions were classified as being due to gastrointestinal diseases (39–45% across deciles, of which half were classified as due to IBD), followed by infections (4–12%, with higher rate of infections in patients in the top decile) and cardiac complications (6–16%) (eFigure 5A). Using PQIs as indicators of preventable admissions, compared to patients in the lowest deciles, HNHC patients had significantly higher rates of preventable admissions (eTable 16).
Figure 1.
Burden of inflammatory bowel diseases: (A) Total days spent in hospital per month, and (B) total costs of hospitalization per month, by deciles. High-need, high-cost patients were defined as patients in the highest decile by total days spent in hospital/month. The white dot represents median, the box plots represent interquartile range and whiskers represent 5th and 95th percentile within that decile.
Table 2.
Burden of hospitalizations due to chronic gastrointestinal and liver diseases, by deciles and standardized by per month of follow-up. High-need, high-cost (HNHC) patients were defined as patients in the highest decile by total days spent in hospital/month.
| Deciles | Inflammatory bowel disease |
Chronic liver diseases | Functional/motility disorders |
Gastrointestinal hemorrhage |
Pancreatic disease |
|---|---|---|---|---|---|
|
| |||||
| Median IQR 5th–95th range |
Median IQR 5th–95th range |
Median IQR 5th–95th range |
Median IQR 5th–95th range |
Median IQR 5th–95th range |
|
|
| |||||
| Total days spent in the hospital | |||||
|
| |||||
| 1st | 0.13 | 0.13 | 0.14 | 0.13 | 0.14 |
| 0.10–0.17 | 0.10–0.17 | 0.10–0.18 | 0.10–0.17 | 0.10–0.18 | |
| 0.08–0.18 | 0.08–0.18 | 0.08–0.20 | 0.08–0.18 | 0.08–0.20 | |
|
| |||||
| 5th | 0.55 | 0.6 | 0.64 | 0.6 | 0.57 |
| 0.50–0.57 | 0.57–0.67 | 0.58–0.67 | 0.57–0.64 | 0.56–0.60 | |
| 0.45–0.60 | 0.55–0.70 | 0.57–0.71 | 0.55–0.67 | 0.55–0.63 | |
|
| |||||
| 10th (HNHC patients) | 3.71 | 4.14 | 4.13 | 4.12 | 3.90 |
| 3.00–5.08 | 3.42–5.63 | 3.36–5.63 | 3.36–5.58 | 3.18–5.40 | |
| 2.63–9.10 | 3.00–9.89 | 3.00–9.86 | 2.92–9.82 | 2.75–9.56 | |
|
| |||||
| Total charges across all hospitalizations (in dollars) | |||||
|
| |||||
| 1st | 427 | 480 | 452 | 414 | 422 |
| 291–662 | 308–788 | 298–735 | 291–600 | 294–627 | |
| 153–1529 | 166–1713 | 161–1639 | 165–1166 | 171–1190 | |
|
| |||||
| 5th | 1053 | 1295 | 1273 | 1261 | 1190 |
| 758–1497 | 912–1877 | 891–1884 | 931–1743 | 871–1633 | |
| 471–2926 | 537–3522 | 536–3780 | 603–3035 | 569–2733 | |
|
| |||||
| 10th (HNHC patients) | 7502 | 8925 | 7794 | 8983 | 8221 |
| 5270–11348 | 6045–13858 | 5353–11742 | 6269–13560 | 5722–12579 | |
| 3391–22805 | 3475–28473 | 3082–22946 | 3969–27575 | 3546–26461 | |
Patient, Hospital, and Hospitalization Characteristics
As compared to patients in the lowest decile, patients in the highest decile were slightly older at time of index hospitalization (51.0y vs. 54.9y, p<0.01), more frequently on Medicare/Medicaid (42% vs. 66%, p<0.01) and in the bottom quartile of household income (20% vs. 26%, p<0.01) (eTable 6). On multivariate logistic regression, after adjusting for multiple confounders, younger age, male sex, Medicare/Medicaid insurance, low income, depression, obesity, high comorbidity burden and index hospitalization at a large and rural hospital for a serious infection (as compared to IBD-related complication) were associated with high healthcare utilization (AUC=0.66) (eTable 7). During their index hospitalization, and across all hospitalizations, patients in the highest decile underwent more gastrointestinal procedures and surgeries, and frequently received blood transfusion and enteral or parenteral nutrition. Overall, across all admissions, 3% of the patients in the lowest decile died in-hospital, whereas 10% patients in the highest decile died.
B. Chronic Liver Diseases
Over a follow-up of 10m (IQR, 8–11), 376,810 patients with CLDs spent 7 days (IQR, 3–14) in the hospital annually (median, 0.70 days/month [IQR, 0.33–1.50]), with median hospitalization costs of $20,890 (IQR, 9,992–44,625) (Table 1).
Hospitalization burden by deciles
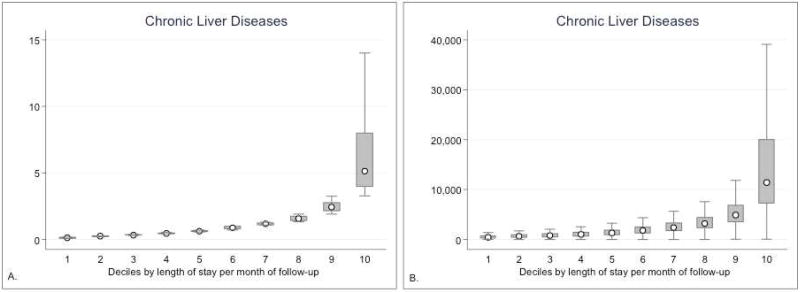
As compared to patients in the lowest decile (median days spent in hospital/month, 0.13 [IQR, 0.10–0.17]; cost, $480/month [IQR, 308–788]), patients in the highest decile (HNHC patients, n=37,293) spent 4.14 days/month in the hospital (IQR, 3.42–5.63), with hospitalization costs of $8,925/month (IQR, 6,045–13,858) (Figure 2, Table 2, eTable 5, eFigure 2B). Even within the highest decile, there was considerable variability with patients at the 99th centile spending 9.89 days/month in the hospital, with one hospitalization/month, at costs of $28,473/month (eFigure 3B, 4B). Cumulatively, patients in highest decile contributed to 36% of hospitalization costs, and patients in the top two deciles contributed 55% of total hospitalization costs. Based on primary discharge diagnosis, most common causes of admissions were classified as being due to gastrointestinal diseases (20.1–23.9% across deciles, of which 10–12% were for gastrointestinal hemorrhage, 7–13% for renal failure, 5.6–8.7% for neuropsychiatric illness), followed by infectious (7–12%, with higher rate of infections in patients in the top decile) and cardiac complications (10–16%) (eFigure 5B; eTable 17).
Figure 2.
Burden of chronic liver diseases: (A) Total days spent in hospital per month, and (B) total costs of hospitalization per month, by deciles.
Patient, Hospital, and Hospitalization Characteristics
On multivariate logistic regression, after adjusting for multiple confounders, younger age, male sex, Medicare/Medicaid insurance, low income, depression, obesity, high comorbidity burden and index hospitalization at a large and rural hospital for a serious infection or respiratory complications were associated with high healthcare utilization (AUC=0.66) (eTable 8 and eTable 9). Overall, few patients in the lowest decile underwent liver transplantation, whereas 2% of patients in the highest decile underwent liver transplantation; in-hospital mortality was significantly higher for patients in the highest decile (lowest vs. highest decile: 10% vs. 16%, p<0.01).
C. Functional gastrointestinal disorders
Over a median follow-up of 10m (IQR, 8–11), 351,583 patients with functional disorders spent 7 days (IQR, 3–14) in the hospital annually (median, 0.71 days/month [IQR, 0.36–1.50]), with median hospitalization costs of $23,298 (IQR, 10,886–48,956) (Table 1).
Hospitalization burden by deciles
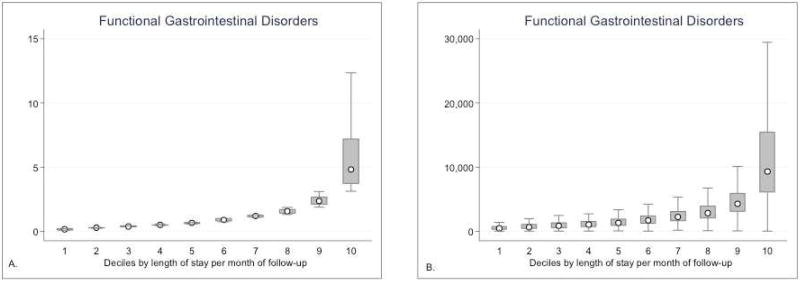
The variability and pattern of hospitalization burden and costs was similar to that observed for patients with IBD or CLDs. As compared to patients in the lowest decile, patients in the highest decile (HNHC patients, n=34,910) spent 4.13 days/month in the hospital (IQR, 3.36–5.63), with hospitalization costs of $7,794/month (IQR, 5,353–11,742); these patients were hospitalized almost every other month (IQR, 0.27–0.63) (Figure 3, Table 2, eTable 5, eFigure 2C, 3C and 4C). Cumulatively, patients in the highest, and top two deciles, contributed 34% and 52% of annual hospitalization costs, respectively. Similar to patients with IBD and CLDs, gastrointestinal diseases (18–24%), infections (4–12%) and cardiac complications (10.0–17%) were leading causes of hospitalization in patients with FGIDs (eFigure 5C, eTable 18).
Figure 3.
Burden of functional gastrointestinal diseases: (A) Total days spent in hospital per month, and (B) total costs of hospitalization per month, by deciles.
Patient, Hospital, and Hospitalization Characteristics
Similar to patients with IBD and CLDs, patients with FGIDs in the highest decile, were frequently on Medicare/Medicaid and in the bottom quartile of household income (AUC=0.68) (eTable 10 and eTable 11); HNHC patients were more frequently males, had obesity, anemia and higher comorbidity burden, though rates of depression at index hospitalization were similar; they also underwent more procedures across all hospitalizations.
D. Gastrointestinal hemorrhage
Over a median follow-up of 10m (IQR, 8–11), 190,881 patients with gastrointestinal hemorrhage spent 6 days (IQR, 3–14) in the hospital annually (median, 0.67 days/month [IQR, 0.33–1.45]), with median hospitalization costs of $14,756 (IQR, 7,362–30,228) (Table 1).
Hospitalization burden by deciles
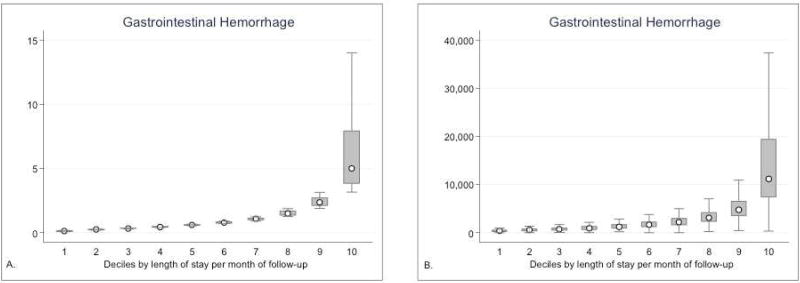
The variability and pattern of hospitalization burden and costs was similar to other chronic gastrointestinal diseases. As compared to patients in the lowest decile, patients in the highest decile (HNHC patients, n=18,864) spent 4.12 days/month in the hospital (IQR, 3.36–5.58), with hospitalization costs of $8,983/month (IQR, 6,269–13,560) (Figure 4, Table 2, eTable 5, eFigure 2D, 3D and 4D). Cumulatively, patients in the highest, and top two deciles, contributed 38% and 56% of annual hospitalization costs, respectively. Though gastrointestinal diseases (25–36%) and infections (2–14%) were dominant causes of hospitalization, malignancy and cardiorespiratory causes were frequent, particularly for patients in the lowest decile (eFigure 5D, eTable 19).
Figure 4.
Burden of gastrointestinal hemorrhage: (A) Total days spent in hospital per month, and (B) total costs of hospitalization per month, by deciles.
Patient, Hospital, and Hospitalization Characteristics
A similar pattern of differences in patients in the lowest and highest decile of hospitalization was observed (eTable 12), and multivariate regression identified younger age, Medicare/Medicaid insurance, low income, obesity, high comorbidity burden and index hospitalization at a large and rural hospital for cardiovascular, respiratory or hematologic complications being associated with high healthcare utilization (AUC=0.72) (eTable 13). At least 60% of patients across deciles underwent a gastrointestinal procedure at their index hospitalization; patients in the highest decile frequently received blood transfusion (lowest vs. highest decile: 32% vs. 53%, p<0.01). Approximately 30% of patients in the highest decile underwent 3 or more gastrointestinal procedures, and 22% received blood transfusions during 3 or more hospitalizations. In-hospital mortality was 19% for patients in highest decile, whereas 10% of the patients in the lowest decile died in-hospital.
E. Pancreatic Diseases
Over a median follow-up of 10m (IQR, 8–11), 98,432 patients with gastrointestinal hemorrhage spent 6 days (IQR, 3–13) in the hospital annually (median, 0.63 days/month [IQR, 0.33–1.33]), with median hospitalization costs of $12,985 (IQR, 6,784–27,250) (Table 1).
Hospitalization burden by deciles
As compared to patients in the lowest decile patients in the highest decile (HNHC patients, n=9,648) spent 3.90 days/month in the hospital (IQR, 3.18–5.40), with median one hospitalization every 2 months (IQR, 0.25–0.64); monthly hospitalization costs for the highest decile were $8,221/month (IQR, 5,722–12,579) (Table 2, eTable 5, eFigure 2E, 3E and 4E, eFigure 6). Cumulatively, patients in highest decile contributed to 39% of hospitalization costs, and patients in the top two deciles contributed 57% of total hospitalization costs. Based on primary discharge diagnosis, most common causes of admissions were classified as being due to gastrointestinal diseases (37.0–49.0%), followed by cardiac (7.0–12.0%) and endocrinological causes (6.0–11.0%); infections were a frequent cause for hospitalization in HNHC patients (10%) (eFigure 5E, eTable 20).
Patient, Hospital, and Hospitalization Characteristics
Systematic differences were observed in HNHC patients and patients in the lowest decile similar to other diseases (AUC=0.71) (eTable 14 and eTable 15). Overall, 4% of the patients in the lowest decile died in-hospital, whereas 12% patients in the highest decile died in-hospital.
DISCUSSION
In this all-payer, nationally representative study of patients who were hospitalized at least once during the index year, we made several key observations. First, there is considerable variability in burden and costs of hospitalization in patients with gastrointestinal and liver diseases, with a small fraction of HNHC patients (defined as patients in the highest decile by total days spent in hospital/month) contributing to the majority of the hospitalization burden and costs. Across a spectrum of common gastrointestinal and liver diseases, patients in the highest decile of hospitalization burden for each condition spent a median 3.7–5.1 days/month in the hospital, with one hospitalization every 2 months for each of these conditions, and with hospitalization costs averaging between $7,438–11,425/month. Second, patient-, hospital- and index-hospitalization characteristics of HNHC patients are fairly similar across diseases – these patients have Medicare/Medicaid insurance, lower income status, index hospitalization in a large rural hospital, high comorbidity burden, obesity and infection-related hospitalization, and more frequently underwent gastrointestinal procedures, received blood transfusions and enteral or parenteral nutrition at their index as well as subsequent hospitalizations, consistent with prior findings.17,18 At a patient-level, modifiable risk factors may include tackling the obesity epidemic and mental health issues and minimizing risk of iatrogenic or healthcare-associated infections, whereas at a health system level interventions may include better access to care and connectivity between rural and specialty hospitals. Third, among patients hospitalized once with chronic gastrointestinal or liver diseases, gastrointestinal causes constitute the most common causes for subsequent hospitalizations, and infections and cardiopulmonary causes are other common reasons for readmission, particularly in patients with frequent hospitalizations.
The first step in population health management is identifying patients with highest healthcare utilization and sources of variability in outcomes. Our study identified key patient-, hospital- and hospitalization characteristics, which are largely comparable across five common gastrointestinal and liver diseases. We anticipate that similar patterns would be observed across other chronic non-gastrointestinal conditions, wherein a small fraction of patients account for majority hospitalization-related care. HNHC patients include two sets of patients: one who are chronically high utilizers, who have established disease-related complications at very high risk of repeated decompensation (for example, patients with decompensated cirrhosis) and second, compensated patients who are not chronically ill, but at high-risk of complications (for example, patients with controlled inflammatory bowel disease, who develop a severe flare). In our analysis, over a one-year cycle, we are unable to distinguish what proportion of patients are in the first category of chronically being high-need, high cost vs. patients who transiently develop high healthcare needs (for example, related to post-operative complications, etc.). The next step in population health management is implementation of multi-component chronic care models which are focused on effective and efficient team care with proactively planned healthcare interactions, self-management support assisted by effective use of community resources, and health information technology aided-clinical decision support.19 Understanding healthcare utilization commonalities across different diseases would help target system-level interventions to improve population health and decrease costs across diseases, and enable adoption of interventions that have been successful in other diseases to the field of gastroenterology.
The strengths of our study include (a) use of a nationally representative database to study longitudinal hospitalization-related care, (b) a novel, patientcentered metric of burden of hospitalization in ‘total days spent in hospital’, (c) comprehensive comparative assessment of patient-, hospital- and index hospitalization characteristics of patients in the lowest and highest decile of hospitalization-related care, and (d) assessment of causes of admissions, across deciles of hospitalization burden.
Our study has several limitations. First, the analyses are based on administrative codes, and only focus on inpatient use, without details of outpatient clinic visits, medication use and laboratory variables. Second, causes of readmissions were identified using primary discharge diagnoses, which were grouped by disease system to allow interpretation. Third, since the NRD uses data from state inpatient databases, it does not track patients across state boundaries. However, in validation studies performed by HCUP, the rate of cross-state hospitalizations were found to be <5% of all admissions for patients, thereby unlikely to substantially affect our estimates.14 Fourth, the concept of PQIs is more widely prevalent in primary care as standard hospital-wide quality measures and none of these are gastrointestinal or liver disease-specific, which somewhat limits their relevance to our field. Fifth, there was potential overlap in patients between different gastrointestinal diseases; approximately 20% patients had two or more candidate gastrointestinal or liver condition at index hospitalization. Since our focus was on identifying burden and costs of hospitalizations with certain defined gastrointestinal diseases, rather than due to those diseases, this overlap would not significantly influence interpretation of results for patients with overlapping conditions. Finally, the NRD does not capture out-of-hospital mortality, which may bias ‘at-risk for hospitalization’ time period; however, for most gastrointestinal and liver diseases, out-of-hospital mortality is a rare occurrence.
In conclusion, in this nationally representative study of patients hospitalized at least once during the index year, we observed considerable variability in burden of hospitalization across five common chronic gastrointestinal and liver diseases, including IBD, CLDs, FGIDs, gastrointestinal hemorrhage and pancreatic diseases, with a small fraction of patients contributing disproportionately to total hospitalization burden and costs. The characteristics of these HNHC patients were remarkably similar across different diseases. Population health management strategies directed towards identifying HNHC patients and implementing multi-component chronic care models may improve quality of care and reduce costs of care.
Supplementary Material
eFigure 1. Selection of patients for constructing study cohort from hospital records in the Nationwide Readmissions Database 2013.
eFigure 2. Total number of hospitalizations per month, by deciles in patients with (A) inflammatory bowel diseases, (B) chronic liver diseases, (C) functional gastrointestinal diseases, (D) gastrointestinal bleeding and (E) pancreatic diseases. The red dot represents median, the box plots represent interquartile range and whiskers represent 5th and 95th percentile within that decile.
eFigure 3. Variability in total days spent in hospital per month by HNHC patients with (A) inflammatory bowel diseases, (B) chronic liver diseases, (C) functional gastrointestinal diseases, (D) gastrointestinal bleeding and (E) pancreatic diseases. The red dot represents median, the box plots represent interquartile range and whiskers represent 5th and 95th percentile within that centile. Overall, X-axis represents patients at 90th, 91st, 92nd … 99th centile, by length of stay.
eFigure 4. Variability in total hospitalization costs per month by HNHC patients with (A) inflammatory bowel diseases, (B) chronic liver diseases, (C) functional gastrointestinal diseases, (D) gastrointestinal bleeding and (E) pancreatic diseases. The red dot represents median, the box plots represent interquartile range and whiskers represent 5th and 95th percentile within that centile. Overall, X-axis represents patients at 90th, 91st, 92nd … 99th centile, by length of stay.
eFigure 5. Causes of hospitalizations based on primary discharge diagnosed grouped by CCS codes and organ systems, in patients in the 1st, 5th and 10th decile, with (A) inflammatory bowel diseases, (B) chronic liver diseases, (C) functional gastrointestinal diseases, (D) gastrointestinal bleeding and (E) pancreatic diseases.
eFigure 6. Burden of pancreatic diseases: (A) Total days spent in hospital per month, and (B) total costs of hospitalization per month, by deciles in patients with pancreatic diseases. The red dot represents median, the box plots represent interquartile range and whiskers represent 5th and 95th percentile within that decile.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: Dr. Singh is supported by the American College of Gastroenterology and Crohn’s and Colitis Foundation, and has received research grants from Pfizer and AbbVie unrelated to the current work. Dr. Ohno-Machado is supported by PCORI CDRN-1306-04819 and NHLBI iDASH (NIH U54HL108460).
Conflicts of Interest: None of the authors have any relevant conflicts of interest.
- Study concept and design: SS
- Acquisition of data: NHN, SS
- Analysis and interpretation of data: NHN, RK, SS
- Drafting of the manuscript: NHN, SS
- Critical revision of the manuscript for important intellectual content: RK, LOM, WJS
- Approval of the final manuscript: NHN, RK, LOM, WJS, SS
- Guarantor of Article: SS
References
- 1.Dieleman JL, Baral R, Birger M, et al. US Spending on Personal Health Care and Public Health, 1996–2013. JAMA. 2016;316:2627–2646. doi: 10.1001/jama.2016.16885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peery AF, Crockett SD, Barritt AS, et al. Burden of Gastrointestinal, Liver, and Pancreatic Diseases in the United States. Gastroenterology. 2015;149:1731–1741. doi: 10.1053/j.gastro.2015.08.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peery AF, Dellon ES, Lund J, et al. Burden of gastrointestinal disease in the United States, 2012 update. Gastroenterology. 2012;143:1179–87. doi: 10.1053/j.gastro.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boccuti CC, G . In: Aiming for Fewer Hospital U-turns: The Medicare Hospital Readmissions Reduction Program. Foundation THJKF, editor. 2015. [Google Scholar]
- 5.Thorpe JHC, T Medicare Hospital Readmissions Reduction Program. Legal Notes. 2011;3:1–4. [Google Scholar]
- 6.Groff AC, Colla CH, Lee TH. Days Spent at Home - A Patient-Centered Goal and Outcome. N Engl J Med. 2016;375:1610–1612. doi: 10.1056/NEJMp1607206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sayer C. In: "Time Spent at Home" - A patient-defined outcome. Catalyst N, editor. Vol. 2016. 2016. [Google Scholar]
- 8.Blumenthal D, Chernof B, Fulmer T, et al. Caring for High-Need, High-Cost Patients - An Urgent Priority. N Engl J Med. 2016;375:909–11. doi: 10.1056/NEJMp1608511. [DOI] [PubMed] [Google Scholar]
- 9.Bleich SN, Sherrod C, Chiang A, et al. Systematic Review of Programs Treating High-Need and High-Cost People With Multiple Chronic Diseases or Disabilities in the United States, 2008–2014. Prev Chronic Dis. 2015;12:E197. doi: 10.5888/pcd12.150275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kolte D, Khera S, Sardar MR, et al. Thirty-Day Readmissions After Transcatheter Aortic Valve Replacement in the United States: Insights From the Nationwide Readmissions Database. Circ Cardiovasc Interv. 2017;10 doi: 10.1161/CIRCINTERVENTIONS.116.004472. [DOI] [PubMed] [Google Scholar]
- 11.Veeranki SP, Sharma K, Ohabughiro MU, et al. 30-Day Readmissions in Hospitalized Adults With Asthma Exacerbations: Insights From the Nationwide Readmission Database. Chest. 2016;150:1162–1165. doi: 10.1016/j.chest.2016.07.043. [DOI] [PubMed] [Google Scholar]
- 12.Mayr FB, Talisa VB, Balakumar V, et al. Proportion and Cost of Unplanned 30-Day Readmissions After Sepsis Compared With Other Medical Conditions. JAMA. 2017;317:530–531. doi: 10.1001/jama.2016.20468. [DOI] [PubMed] [Google Scholar]
- 13.Poojary P, Saha A, Chauhan K, et al. Predictors of Hospital Readmissions for Ulcerative Colitis in the United States: A National Database Study. Inflamm Bowel Dis. 2017;23:347–356. doi: 10.1097/MIB.0000000000001041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.NRD Itt. Healthcare Cost and Utilization Project (HCUP) Agency for Healthcare Research and Quality; Rockville, MD: 2015. [PubMed] [Google Scholar]
- 15.Overview H. Healthcare Cost and Utilization Project (HCUP) Agency for Healthcare Research and Quality; Rockville, MD: 2016. [PubMed] [Google Scholar]
- 16.Patel KK, Vakharia N, Pile J, et al. Preventable Admissions on a General Medicine Service: Prevalence, Causes and Comparison with AHRQ Prevention Quality Indicators-A Cross-Sectional Analysis. J Gen Intern Med. 2016;31:597–601. doi: 10.1007/s11606-016-3615-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Basu J, Avila R, Ricciardi R. Hospital Readmission Rates in U.S. States: Are Readmissions Higher Where More Patients with Multiple Chronic Conditions Cluster? Health Serv Res. 2016;51:1135–51. doi: 10.1111/1475-6773.12401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cohen S, Yu W. Statistical Brief #124. Rockville, MD: Agency for Healthcare Research and Quality; 2006. The persistence in the level of health care expenditures over time: estimates for the U.S. population, 2002–2003. [Google Scholar]
- 19.Martinez-Gonzalez NA, Berchtold P, Ullman K, et al. Integrated care programmes for adults with chronic conditions: a meta-review. Int J Qual Health Care. 2014;26:561–70. doi: 10.1093/intqhc/mzu071. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Selection of patients for constructing study cohort from hospital records in the Nationwide Readmissions Database 2013.
eFigure 2. Total number of hospitalizations per month, by deciles in patients with (A) inflammatory bowel diseases, (B) chronic liver diseases, (C) functional gastrointestinal diseases, (D) gastrointestinal bleeding and (E) pancreatic diseases. The red dot represents median, the box plots represent interquartile range and whiskers represent 5th and 95th percentile within that decile.
eFigure 3. Variability in total days spent in hospital per month by HNHC patients with (A) inflammatory bowel diseases, (B) chronic liver diseases, (C) functional gastrointestinal diseases, (D) gastrointestinal bleeding and (E) pancreatic diseases. The red dot represents median, the box plots represent interquartile range and whiskers represent 5th and 95th percentile within that centile. Overall, X-axis represents patients at 90th, 91st, 92nd … 99th centile, by length of stay.
eFigure 4. Variability in total hospitalization costs per month by HNHC patients with (A) inflammatory bowel diseases, (B) chronic liver diseases, (C) functional gastrointestinal diseases, (D) gastrointestinal bleeding and (E) pancreatic diseases. The red dot represents median, the box plots represent interquartile range and whiskers represent 5th and 95th percentile within that centile. Overall, X-axis represents patients at 90th, 91st, 92nd … 99th centile, by length of stay.
eFigure 5. Causes of hospitalizations based on primary discharge diagnosed grouped by CCS codes and organ systems, in patients in the 1st, 5th and 10th decile, with (A) inflammatory bowel diseases, (B) chronic liver diseases, (C) functional gastrointestinal diseases, (D) gastrointestinal bleeding and (E) pancreatic diseases.
eFigure 6. Burden of pancreatic diseases: (A) Total days spent in hospital per month, and (B) total costs of hospitalization per month, by deciles in patients with pancreatic diseases. The red dot represents median, the box plots represent interquartile range and whiskers represent 5th and 95th percentile within that decile.