Abstract
Background
The emerging mobile colistin resistance gene, mcr-1, is an ongoing worldwide concern and an evaluation of clinical isolates harboring this gene is required in Korea. We investigated mcr-1-possessing Enterobacteriaceae among Enterobacteriaceae strains isolated in Korea, and compared the genetic details of the plasmids with those in Escherichia coli isolates from livestock.
Methods
Among 9,396 Enterobacteriaceae clinical isolates collected between 2010 and 2015, 1,347 (14.3%) strains were resistant to colistin and those were screened for mcr-1 by PCR. Colistin minimum inhibitory concentrations (MICs) were determined by microdilution, and conjugal transfer of the mcr-1-harboring plasmids was assessed by direct mating. Whole genomes of three mcr-1-positive Enterobacteriaceae clinical isolates and 11 livestock-origin mcr-1-positive E. coli isolates were sequenced.
Results
Two E. coli and one Enterobacter aerogenes clinical isolates carried carried IncI2 plasmids harboring mcr-1, which conferred colistin resistance (E. coli MIC, 4 mg/L; E. aerogenes MIC, 32 mg/L). The strains possessed the complete conjugal machinery except for E. aerogenes harboring a truncated prepilin peptidase. The E. coli plasmid transferred more efficiently to E. coli than to Klebsiella pneumoniae or Enterobacter cloacae recipients. Among the three bacterial hosts, the colistin MIC was the highest for E. coli owing to the higher mcr-1-plasmid copy number and mcr-1 expression levels. Ten mcr-1-positive chicken-origin E. coli strains also possessed mcr-1-harboring IncI2 plasmids closely related to that in the clinical E. aerogenes isolate, and the remaining one porcine-origin E. coli possessed an mcr-1-harboring IncX4 plasmid.
Conclusions
mcr-1-harboring IncI2 plasmids were identified in clinical Enterobacteriaceae isolates. These plasmids were closely associated with those in chicken-origin E. coli strains in Korea, supporting the concept of mcr-1 dissemination between humans and livestock.
Keywords: mcr-1, Colistin resistance, Enterobacteriaceae, IncI2 plasmid
INTRODUCTION
One of the few remaining options for the treatment of infectious diseases caused by multiple-drug resistant gram-negative bacilli is colistin [1]. Accordingly, the emerging mobile colistin resistance gene, mcr-1, encoding a phosphoethanolamine transferase has become a critical threat to public health [2]. Following its initial report [2], studies examining the global dissemination of this gene have rapidly emerged. Various Enterobacteriaceae carrying mcr-1-plasmids from humans, animals, and environments have been identified in Asia, Europe, Africa, and North and South America [3]. The subsequently detected mcr-1.2 derivative [4] and other subtypes (mcr-2 [5], mcr-3 [6], and mcr-4 [7]) are an additional threat. Extensive colistin usage in farm animals [8] and unrestricted international migration of humans [9], livestock, and agricultural products have facilitated the rapid spread of the mcr genes [10].
The mcr-1 gene is carried by conjugative plasmids belonging to various incompatibility groups: IncI2, IncX4, IncHI1B, IncHI2A, IncFII, and IncFIB [11]. The genomic environment of the mcr-1 gene differs by plasmid type [12], frequently being bracketed by one or two copies of ISApl1 [13].
The co-harboring of resistance genes for third generation cephalosporins and carbapenems adds further complications. Additional plasmids carrying blaCTX-M encoding extended-spectrum beta-lactamases (ESBLs) [14,15], blaNDM [14,16] and blaIMP [15] encoding metallo-beta-lactamases, and blaKPC [17] encoding serine carbapenemases are often found in mcr-1-possessing strains. Moreover, the mcr-1 gene is co-carried by a plasmid containing the blaCTX-M-55, -14, -65, and blaNDM-5 genes [18,19]. Plasmids carrying multiple resistance genes are of further concern because bacteria could become extensively- or pan-drug resistant by a single event of horizontal gene transfer.
An E. coli strain carrying a mcr-1 plasmid was first reported in 2015 in livestock and humans [2]; however, based on a retrospective analysis, the emergence of the gene dates back to the 1980s in E. coli from chicken specimens [8]. Similar to the case of NDM-1 [20], the mcr-1 gene was reported as a novel emerging resistance gene following worldwide dissemination [3]. The origin of this problematic gene is still controversial; however, based on the fact that the gene is predominant in bacteria from food animals and that colistin is extensively used in the livestock industry [8], food animals are considered responsible for spreading the mcr-1 gene.
We investigated mcr-1-possessing Enterobacteriaceae among Enterobacteriaceae strains isolated in Korea. We identified one Enterobacter aerogenes strain harboring an IncI2 plasmid co-carrying mcr-1 and blaCTX-M-55 and two E. coli strains possessing a mcr-1-carrying IncI2 plasmid along with plasmids containing multiple-drug resistant genes, including blaCTX-M-55 and blaNDM-9, from clinical specimens. The mcr-1-carrying plasmids were examined in terms of horizontal gene transfer, plasmid copy number, and gene expression, and the genetic details of the plasmids were compared with those in E. coli strains from livestock.
METHODS
1. Bacterial strains
We retrospectively analyzed a total of 5,206 clinical isolates, including 2,547 Klebsiella pneumoniae and 2,659 E. coli strains, collected between 2011 and 2015 through the Korean Antimicrobial Resistance Monitoring System, and 4,190 carbapenemase-producing Enterobacteriaceae (CPE) clinical isolates, including 2,738 K. pneumoniae, 565 E. coli, and 887 Enterobacter spp. strains, collected between 2010 and 2015 at the National Laboratory Surveillance of CPE. Eleven E. coli strains from livestock (10 chicken and one porcine) [21] were included in the study for whole genome sequencing.
2. Determination of the minimum inhibitory concentration (MIC) of colistin
From the 9,396 Enterobacteriaceae clinical isolates, colistin-resistant strains were first obtained using 1 mg/L colistin media. For the selected putative colistin-resistant strains, the MIC of colistin was determined using the microdilution method with Mueller–Hinton (MH) broth, following the recommendations of the Joint CLSI-EUCAST Polymyxin Breakpoints Working Group [22], and the confirmed colistin-resistant strains exhibiting colistin MIC ≥2 mg/L were used for further analysis.
3. DNA manipulation and conventional PCR
Genomic DNA of colistin-resistant strains was extracted by the boiling method, and PCR was performed using the AccuPower Taq PCR Premix (Bioneer, Daejeon, Korea). Using the genomic DNA as a template, conventional PCR was carried out to amplify the mcr-1 [2], mcr-3 [6], and mcr-4 [7] genes, as previously described. The mcr-2 gene was amplified using newly designed primers mcr-12-281F (5′-CTTATGGCACGGTCTATGA-3′) and mcr-12-93R (5′-CACATTTTCTTGGTATTTGG-3′) under the following conditions: 30 seconds at 97℃ for pre-denaturation; 30 cycles of 10 seconds at 97℃, 20 seconds at 53℃, and 30 seconds at 72℃ for amplification; and 5 minutes at 72℃ for final amplification. Amplified products were subjected to direct sequencing.
4. Whole genome sequencing and comparative genomics
The whole bacterial genomes of the three clinical Enterobacteriaceae isolates harboring the mcr-1 gene underwent single-molecule real-time (SMRT) sequencing using a PacBio RSII instrument (Pacific Biosciences, Menlo Park, CA, USA), as previously described [23]. The 11 mcr-1-possessing plasmids in E. coli strains from livestock isolated between 2013 and 2015 in Korea [21] were sequenced by SMRT. Further, these plasmids were comparatively analyzed with the three pUSU-ECO-12704_4, pCREC-527_4, and pCRENT-301_1 plasmids from clinical isolates. The 324-bp sequences of the replication origin were obtained from the 11 plasmids, and molecular phylogeny was analyzed together with the three plasmids in the clinical Enterobacteriaceae strains.
5. Determination of gene copy number by quantitative PCR (qPCR)
For the three clinical Enterobacteriaceae isolates, the total DNA was extracted by boiling and used for qPCR. The CLR5-F and -R primers targeting the mcr-1 gene and primer pair incI2_63-86 (5′-GATTTGTAAATGCAGAAAACGAGG-3′) and incI2_273-250 (5′-GAGTTGATATTTCCTTCTCATGGA-3′) targeting the incI2 gene were used. The plasmid copy number was normalized to that of the gyrB gene using gyrB-F_1466-1489 (5′-GTTATCACAGCATCATCATCATGA-3′) and gyrB-R_1650-1627 (5′-TTCGTCGTCTTTAATGTACTGTTC-3′) and that of rpoD using rpoD-F_883-906 (5′-C-3′) and rpoD-R_1085-1062 (5′-TTGATATCTTTAACCTGCTCGATG-3′). Standard curves were generated using five 10-fold serial dilutions of DNA for each target gene. All experiments were carried out in duplicate and at least twice independently.
6. RNA isolation and reverse transcription (RT) qPCR
Total RNA was extracted at the exponential phase using the RNeasy plus mini kit (Qiagen, Hilden, Germany). The mcr-1 transcriptome was determined using the LightCycler RNA amplification kit with SYBR green I (Roche Diagnostics, Basel, Switzerland) and normalized to that of rpoD and gyrB using the primer sets mentioned above. Experiments were carried out in duplicate at least twice independently.
7. Plasmid transfer by bacterial conjugation
Spontaneous rifampin-resistant mutants of E. coli J53, K. pneumoniae ATCC 13883, and E. cloacae ATCC 23355 were used as recipients. K. pneumoniae ATCC 13883 possesses undisturbed IncFII and IncFIA plasmids, and E. cloacae ATCC 23355 does not contain marked plasmids, as determined by plasmid mini prep. Equal amounts of exponential cultures of the donor and the recipient strains were mixed, incubated either in MH broth or on a membrane filter (Merck Millipore, Darmstadt, Germany) for 12 hours, and then spread on Brain Heart Infusion agar containing rifampin (40 mg/L) and colistin (2 mg/L). Each colony was tested by the disk diffusion method and confirmed by PCR. The plasmid transfer frequency was calculated based on the number of transconjugants per donor.
8. Accession numbers
Nucleotide sequence data are available in the GenBank nucleotide database under accession numbers KY657478 (pUSU-ECO-12704_4), KY657476 (pCREC-527_4), and KY657477 (pCRENT-301_1).
RESULTS
1. Identification of three Enterobacteriaceae clinical isolates carrying the mcr-1 gene
Of the 9,396 clinical Enterobacteriaceae strains tested, 14.3% (1,347/9,396) strains, including 15.3% (810/5,285) K. pneumoniae, 10.5% (340/3,224) E. coli, and 22.2% (197/887) Enterobacter spp. strains, exhibited colistin MIC ≥2 mg/L. Among these, the mcr-1 gene was identified by PCR in two E. coli isolates, USU-ECO-12704 and CREC-527, collected in 2012 and 2015, respectively, and in one E. aerogenes strain, CRENT-301, isolated in 2013. These strains were all isolated from urine specimens collected in different provinces of Korea (Table 1). The mcr-2, mcr-3, and mcr-4 genes were not detected in any of the isolates. No known amino acid substitution in PmrABC conferring colistin resistance was observed in the three chromosomes. The E. aerogenes CRENT-301 strain had the highest colistin MIC (32 mg/L), and the E. coli USU-ECO-12704 and CREC-527 strains exhibited identical colistin MICs of 4 mg/L (Table 2).
Table 1. Clinical isolates used in the study.
| Strain | Isolated* in | Resistant to [33] | |
|---|---|---|---|
| City | Year | ||
| Escherichia coli USU-ECO-12704 | Ulsan | 2012 | Gentamicin, tobramycin, tetracycline, ciprofloxacin, ampicillin, ceftazidime, colistin |
| Enterobacter aerogenes CRENT-301 | Incheon | 2013 | Cefotaxime, colistin |
| E. coli CREC-527 | Seoul | 2015 | Tetracycline, ampicillin, ceftazidime, imipenem, colistin |
*All isolates were from urine specimens.
Table 2. Colistin MICs in the mcr-1 harboring Enterobacteriaceae.
| Strain | Colistin MIC (mg/L) |
|---|---|
| Escherichia coli USU-ECO-12704 | 4 |
| Enterobacter aerogenes CRENT-301 | 32 |
| E. coli CREC-257 | 4 |
| E. coli ATCC 25922 | 0.5 |
| E. coli EJ53-RifR | 0.5 |
| E. coli EJ53-RifR / pUSU-ECO-12704_4 | 4 |
| Klebsiella pneumoniae Kpn-RifR | 2 |
| K. pneumoniae Kpn-RifR / pUSU-ECO-12704_4 | 8 |
| Enterobacter cloacae Ecl-RifR | 0.5 |
| E. cloacae Ecl-RifR / pUSU-ECO-12704_4 | 1 |
Abbreviation: MIC, minimal inhibitory concentration.
2. Colistin MICs conferred by mcr-1
Transconjugants carrying the mcr-1-possessing pUSU-ECO-12704_4 exhibited various MICs of colistin according to the bacterial host. The E. coli transconjugant carrying the plasmid exhibited an 8-fold-elevated colistin MIC (4 mg/L), while the K. pneumoniae transconjugant had a 4-fold higher MIC (8 mg/L), and the E. cloacae transconjugant presented a 2-fold higher colistin MIC (1 mg/L; Table 2). The transconjugant plasmid copy number was the highest (11 copies/genome equivalent [GE]) in the E. coli host, six copies/GE in K. pneumoniae, and the lowest (one copy/GE) in E. cloacae. mcr-1 gene expression corresponded to the plasmid copy number of the bacterial hosts.
3. Genomic insights into the three mcr-1-positive Enterobacteriaceae strains
The genome of E. coli USU-ECO-12704 sequence type (ST) 1011 (adk-fumC-gyrB-icd-mdh-purA-recA, 6-4-159-44-112-1-17) consisted of a 5.0-Mb chromosome containing seven drug resistance genes (blaTEM-1, dfrA, aadA, sul1, mphA, aac(3)-II, and blaCTX-M-55) and five plasmids: a 94,115-bp p0111-type plasmid possessing a tet(A) gene; a 89,509-bp IncFIB 1/IncFII 34 plasmid carrying oqxA/oqxB genes; a 70,600-bp IncFII plasmid containing the blaTEM-1, blaCTX-M-55, and fosA genes; a 60,948-bp IncI2 plasmid carrying the mcr-1 gene; and a 20,902-bp cryptic plasmid of unidentified incompatibility group.
The E. coli CREC-527 strain belonged to ST101 (43-41-15-18-11-7-6). Its genome consisted of a 4.8-Mb chromosome possessing the blaTEM-1, dfrA, tet(A), aph(3‚)-1, mph(A), and catA drug resistance genes and five plasmids: a 118,328-bp p0111-type plasmid carrying fosA, dfrA, aadA2, sul1, mphA, and blaNDM-9; a cryptic 96,521-bp p0111-type plasmid; a 79,911-bp IncFIB plasmid carrying strA and blaCTX-M-27; a 60,959-bp IncI2 plasmid carrying the mcr-1 gene; and a cryptic 8,678-bp plasmid of unidentified incompatibility group.
The genome of E. aerogenes CRENT-301 consisted of a 5.3-Mb chromosome without any acquired resistance determinants and two plasmids: a 67,073-bp IncI2 plasmid carrying mcr-1 and blaCTX-M-55 genes and a 33,722-bp cryptic plasmid.
4. IncI2 plasmids carrying the mcr-1 gene in clinical E. coli isolates
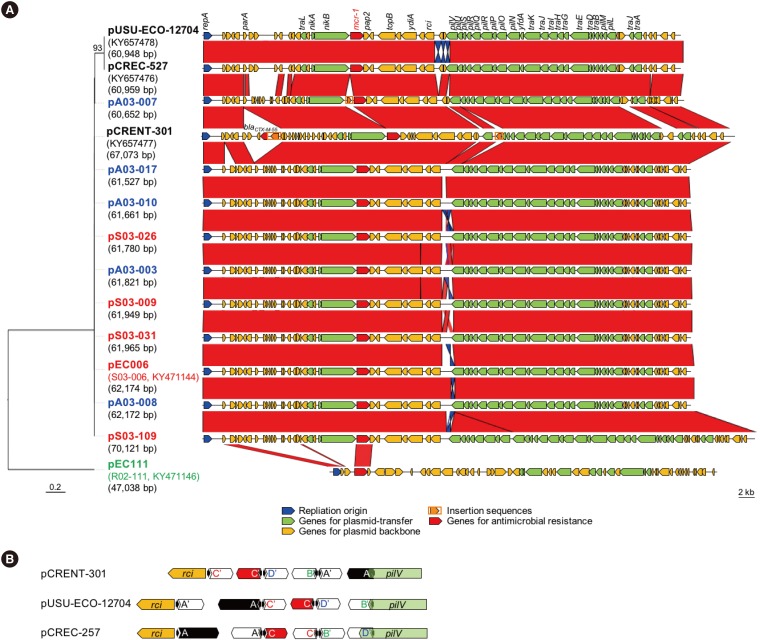
The three mcr-1-plasmids were designated as pUSU-ECO-12704_4 in E. coli USU-ECO-12704, pCREC-527_4 in E. coli CREC-527, and pCRENT-301_1 in E. aerogenes CRENT-301. The structure of the three IncI2 plasmids differed from that of the first identified pHNSHP45 containing a type IV secretion system and a relaxase [2]. pCRENT-301_1 shared the most similarity with pHNSHP45 (Fig. 1A); compared with pHNSHP45, pCRENT-301_1 contains ISEcp1-blaCTX-M-55 downstream of the parA gene, IS903B interrupting a pilU gene resulting in a 93-aa-premature 211-aa pilU protein, and a differently arranged shufflon. The other two plasmids in E. coli strains were indistinguishable (99% nucleotide identity) and have a replication initiation protein sharing 97.95% aa identity (97.57% nucleotide identity) with that in pHNSHP45. Interestingly, pCREC-527_4 has nucleotide substitutions in the 5′-region of pilS, resulting in a shortened PilS protein, a truncated hypothetical protein following a one nucleotide deletion of the heptameric adenine, and a rearranged shufflon (Fig. 1B).
Fig. 1. Comparative analyses of the mcr-1-plasmids from clinical Enterobacteriaceae strains and livestock-origin Escherichia coli strains. (A) Left, molecular phylogeny was conducted by neighbor joining analysis of nucleotide sequences (324 bp) of the replication origin of the mcr-1-plasmids. Multiple sequence alignments were performed with MUSCLE v3.8, and the phylogenetic tree was reconstructed using the distance method implemented in the BioNJ program [34]. Plasmid names are indicated in each taxon along with the size in brackets. Strain name and GenBank accession number are indicated below the plasmid name, if available. Color codes: Black, clinical Enterobacteriaceae strains; blue, E. coli from healthy chickens; red, E. coli from chicken carcasses; and green, E. coli from diseased pig. Right, schematic representation of plasmid structures. The sequence of each plasmid was aligned using BlastN and compared using the Artemis Comparison Tool. Highly-conserved regions (>96% nucleic acid identity) are indicated in red, and moderately conserved regions (>92% nucleic acid identity) are indicated in blue. Open arrows, open reading frames; blue, the replication origin; red, antimicrobial resistance; yellow, plasmid backbone; orange, transposases; and green, plasmid transfer. (B) The yellow arrow indicates the site-specific recombinase rci gene, and the green arrow indicates the pilUs assembly pilV gene. Black arrowheads represent the six 19-bp repeats. Open reading frames in the direction of translation are indicated by arrows.
The −35 and −10 sequences of the mcr-1 promoter region were identified by 5′ rapid PCR amplification of cDNA ends and compared with the pAf23 plasmid from a clinical E. coli strain isolated in South Africa [24]. The sequences in pUSU-ECO-12704_4 and pCREC-527_4 were identical to those of pAf23, while that in pCRENT-301_1 contained a substitution in the -10 sequence generating a weaker consensus sequence (TAAAAT vs TATAAT) relative to the other two plasmids. The putative ribosomal binding site (RBS) of mcr-1 in pCRENT-301_1 was GAGTAG, identical to that in pAf23, while the RBS of the other two plasmids had a one nucleotide difference, GATTAG.
The frequency of pUSU-ECO-12704_4 plasmid transfer was the highest, 2.8×10−5 on the membrane surface and 1.1×10−5 in liquid. Plasmid pCREC-527_4 transfer frequency was 9.6×10−7 on the membrane surface and <1.0×10−10 in liquid. Plasmid pCRENT-301_1 transfer frequency was below the 1.0×10−10 detection threshold, both on the membrane surface and in liquid. For E. coli USU-ECO-12704, which had the highest conjugal efficiency, mating was carried out with K. pneumoniae and E. cloacae recipients, and plasmid transfer was observed in only liquid media with a frequency of 3.0×10−9 in K. pneumoniae and 1.1×10−10 in E. cloacae.
An IncI2 plasmid possessing the mcr-1 gene found in an E. coli isolate from the blood culture of a patient with cholangitis identified in Korea [25] exhibits a nearly identical structure to that of pCRENT-301_1, except for one copy of insertion sequence IS679 downstream of the replication origin (Fig. 1A). The promoter sequences of the two plasmids are also identical.
5. Comparison of mcr-1-plasmids in E. coli strains from those in livestock
Ten of the 11 mcr-1-plasmids in E. coli strains from either healthy chickens or chicken carcasses were IncI2 type, the same as the three plasmids in clinical Enterobacteriaceae strains. Interestingly, one E. coli plasmid from a diseased pig belonged to type IncX4. The 10 IncI2-type plasmids were 60,652 to 70,121 bp in length, and the plasmid backbone was indistinguishable from that of pCRENT-301_1, except the shufflon region (Fig. 1A). The longest pS03-109 plasmid had a 7,758-bp duplication of the region including conjugative elements resulting in a length of 70,121 bp. Remarkably, pA03-007 possessed a copy of insertion sequence ISApl1 upstream of the mcr-1 gene. The only IncX4-type plasmid was 46,931 bp in length. This plasmid shared only the mcr-1 gene and the downstream partial pap2 with the ten IncI2 plasmids. None of the 11 plasmids in livestock isolates possessed known antimicrobial resistance determinants except for mcr-1.
The phylogeny corresponded to plasmid structure analysis. The pCRENT-301_1 plasmid in clinical E. aerogenes was included in the clade of 11 plasmids in livestock isolates, while the other two plasmids in clinical E. coli strains belonged to a clade split from the other IncI2-type plasmids.
DISCUSSION
Following a report on livestock-origin mcr-1-positive E. coli strains isolated between 2013 and 2015 in Korea [21], we report three clinical Enterobacteriaceae strains carrying the gene, identified in 2012, 2013, and 2015. The three strains were well-prepared in terms of fitness in clinical settings. pCRENT-301_1 in E. aerogenes co-carried the blaCTX-M-55 gene encoding ESBL, which could provide a great advantage when encountering the third generation cephalosporins; the two mcr-1-positive E. coli strains harbored secondary plasmids carrying multiple genes for antimicrobial resistance, including blaCTX-M-55 and blaCTX-M-27 encoding ESBLs and blaNDM-9 encoding a carbapenemase.
In terms of molecular epidemiology, the three strains, one E. aerogenes and two E. coli belonging to either ST1011 or ST101, were clearly distinct. Among the 11 livestock isolates from Korea, only one E. coli strain was ST101 [21]. An E. coli ST101 clinical isolate from Brazil harboring an IncX4 mcr-1-plasmid has been identified [26], and an E. coli ST1011 strain possessing an IncX4 mcr-1-plasmid has been isolated from a sputum specimen in Egypt [27].
Despite the divergent hosts, the incompatibility type of all mcr-1-plasmids in clinical isolates was IncI2. The representative IncI2 plasmid, R721, possesses pil and tra gene clusters assembling thin and thick conjugal pili, respectively [28], necessary for plasmid transfer [29]. Among the three IncI2 plasmids, pCRENT-301_1 completely lost conjugal capacity, possibly owing to a truncated pilU prepilin peptidase, which is essential for thin pilUs formation [30]. The pCREC-527_4 plasmid produces a premature PilS pilin precursor resulting in diminished plasmid transfer efficiency. In addition, the rearrangement of the pilV gene due to rci-derived DNA reshuffling allowed recipient-specificity [31]; pUSU-ECO-12704_4 exhibited higher conjugal efficiency in E. coli compared with the other species recipients. Interestingly, the pUSU-ECO-12704_4 plasmid conferred a different level of colistin resistance in each of the bacterial hosts, which was compatible with plasmid copy number. The relatively lower plasmid transfer rates compared with that of the first identified mcr-1 plasmid, pHNSHP45 [2], could be because of bacterial host background, corresponding with the diverse transfer efficiency of IncI2 mcr-1-plasmids in livestock isolates [21].
The notably higher colistin MIC of E. aerogenes CRENT-301 compared with the other two E. coli strains could also be associated with bacterial host background. Enterobacteriaceae strains harboring the mcr-1 plasmid varied in colistin susceptibilities by species (Table 2). In addition, plasmid copy number, which was likely responsible for the elevated colistin MIC from the recipient strain, was dependent on bacterial species.
The 11 mcr-1-plasmids in livestock isolates belonged to two incompatibility groups and differed according to the isolate origin: the plasmids in chicken isolates were IncI2, similar to pHNSHP45 and the plasmids in clinical isolates, while the plasmid in the pig isolate was type IncX4. Except for incompatibility type, no specific trait differences were identified in the pig isolates [21]. ISApl1 was likely involved in mcr-1 gene acquisition [13,32] in the plasmids, and the insertion sequence was identified in one of the 11 plasmids. Unfortunately, only the nucleotide sequences of the mcr-1-possessing plasmids were available for the 11 livestock isolates; thus, no further analyses were possible.
This study has an obvious limitation concerning the clarification of mechanisms involved in colistin resistance. Among the subjected isolates, 1,347 were resistant to colistin; however, only three of those conferred resistance by harboring the mcr-1 gene, and the others remained unknown. The mechanism of resistance, moreover, a novel type of mcr gene, should be investigated in the future.
The mcr-1-possessing strains identified in this study support this concept. Better stewardship for the proper usage of antimicrobials, as well as collaborative surveillance in terms of One Health, is essential.
Acknowledgment
This research was supported by a fund (2016ER230100#) from the Research Program of Korea Centers for Disease Control and Prevention.
Footnotes
Authors' Disclosures of Potential Conflicts of Interest: No potential conflicts of interest relevant to this article were reported.
References
- 1.Giamarellou H, Poulakou G. Multidrug-resistant gram-negative infections: what are the treatment options? Drugs. 2009;69:1879–1901. doi: 10.2165/11315690-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 2.Liu YY, Wang Y, Walsh TR, Yi LX, Zhang R, Spencer J, et al. Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China: a microbiological and molecular biological study. Lancet Infect Dis. 2016;16:161–168. doi: 10.1016/S1473-3099(15)00424-7. [DOI] [PubMed] [Google Scholar]
- 3.Skov RL, Monnet DL. Plasmid-mediated colistin resistance (mcr-1 gene): three months later, the story unfolds. Euro Surveill. 2016;21:30155. doi: 10.2807/1560-7917.ES.2016.21.9.30155. [DOI] [PubMed] [Google Scholar]
- 4.Di Pilato V, Arena F, Tascini C, Cannatelli A, Henrici De Angelis L, Fortunato S, et al. mcr-1.2, a new mcr variant carried on a transferable plasmid from a colistin-resistant KPC carbapenemase-producing Klebsiella pneumoniae strain of sequence type 512. Antimicrob Agents Chemother. 2016;60:5612–5615. doi: 10.1128/AAC.01075-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xavier BB, Lammens C, Ruhal R, Kumar-Singh S, Butaye P, Goossens H, et al. Identification of a novel plasmid-mediated colistin-resistance gene, mcr-2, in Escherichia coli, Belgium, June 2016. Euro Surveill. 2016;21:30280. doi: 10.2807/1560-7917.ES.2016.21.27.30280. [DOI] [PubMed] [Google Scholar]
- 6.Yin W, Li H, Shen Y, Liu Z, Wang S, Shen Z, et al. Novel plasmid-mediated colistin resistance gene mcr-3 in Escherichia coli. MBio. 2017;8:e00543-17. doi: 10.1128/mBio.00543-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Carattoli A, Villa L, Feudi C, Curcio L, Orsini S, Luppi A, et al. Novel plasmid-mediated colistin resistance mcr-4 gene in Salmonella and Escherichia coli, Italy 2013, Spain and Belgium, 2015 to 2016. Euro Surveill. 2017;22:30589. doi: 10.2807/1560-7917.ES.2017.22.31.30589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shen Z, Wang Y, Shen Y, Shen J, Wu C. Early emergence of mcr-1 in Escherichia coli from food-producing animals. Lancet Infect Dis. 2016;16:293. doi: 10.1016/S1473-3099(16)00061-X. [DOI] [PubMed] [Google Scholar]
- 9.von Wintersdorff CJ, Wolffs PF, van Niekerk JM, Beuken E, van Alphen LB, Stobberingh EE, et al. Detection of the plasmid-mediated colistin-resistance gene mcr-1 in faecal metagenomes of Dutch travellers. J Antimicrob Chemother. 2016;71:3416–3419. doi: 10.1093/jac/dkw328. [DOI] [PubMed] [Google Scholar]
- 10.Robinson TP, Bu DP, Carrique-Mas J, Fèvre EM, Gilbert M, Grace D, et al. Antibiotic resistance is the quintessential One Health issue. Trans R Soc Trop Med Hyg. 2016;110:377–380. doi: 10.1093/trstmh/trw048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gao R, Hu Y, Li Z, Sun J, Wang Q, Lin J, et al. Dissemination and mechanism for the MCR-1 colistin resistance. PLoS Pathog. 2016;12:e1005957. doi: 10.1371/journal.ppat.1005957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Falgenhauer L, Waezsada SE, Yao Y, Imirzalioglu C, Kasbohrer A, Roesler U, et al. Colistin resistance gene mcr-1 in extended-spectrum beta-lactamase-producing and carbapenemase-producing Gram-negative bacteria in Germany. Lancet Infect Dis. 2016;16:282–283. doi: 10.1016/S1473-3099(16)00009-8. [DOI] [PubMed] [Google Scholar]
- 13.Snesrud E, Ong AC, Corey B, Kwak YI, Clifford R, Gleeson T, et al. Analysis of Serial Isolates of mcr-1-positive Escherichia coli reveals a highly active ISApl1 transposon. Antimicrob Agents Chemother. 2017;61:e00056-17. doi: 10.1128/AAC.00056-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Du H, Chen L, Tang YW, Kreiswirth BN. Emergence of the mcr-1 colistin resistance gene in carbapenem-resistant Enterobacteriaceae. Lancet Infect Dis. 2016;16:287–288. doi: 10.1016/S1473-3099(16)00056-6. [DOI] [PubMed] [Google Scholar]
- 15.Zhang XF, Doi Y, Huang X, Li HY, Zhong LL, Zeng KJ, et al. Possible transmission of mcr-1-harboring Escherichia coli between companion animals and human. Emerg Infect Dis. 2016;22:1679–1681. doi: 10.3201/eid2209.160464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang RS, Feng Y, Lv XY, Duan JH, Chen J, Fang LX, et al. Emergence of NDM-5- and MCR-1-producing Escherichia coli clones ST648 and ST156 from a single muscovy duck (Cairina moschata) Antimicrob Agents Chemother. 2016;60:6899–6902. doi: 10.1128/AAC.01365-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Teo JQ, Ong RT, Xia E, Koh TH, Khor CC, Lee SJ, et al. mcr-1 in multidrug-resistant blaKPC-2-producing clinical Enterobacteriaceae isolates in Singapore. Antimicrob Agents Chemother. 2016;60:6435–6437. doi: 10.1128/AAC.00804-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sun J, Li XP, Yang RS, Fang LX, Huo W, Li SM, et al. Complete nucleotide sequence of an IncI2 plasmid coharboring blaCTX-M-55 and mcr-1. Antimicrob Agents Chemother. 2016;60:5014–5017. doi: 10.1128/AAC.00774-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Quan J, Li X, Chen Y, Jiang Y, Zhou Z, Zhang H, et al. Prevalence of mcr-1 in Escherichia coli and Klebsiella pneumoniae recovered from bloodstream infections in China: a multicentre longitudinal study. Lancet Infect Dis. 2017;17:400–410. doi: 10.1016/S1473-3099(16)30528-X. [DOI] [PubMed] [Google Scholar]
- 20.Moellering RC., Jr NDM-1—a cause for worldwide concern. N Engl J Med. 2010;363:2377–2379. doi: 10.1056/NEJMp1011715. [DOI] [PubMed] [Google Scholar]
- 21.Lim SK, Kang HY, Lee K, Moon DC, Lee HS, Jung SC. First detection of the mcr-1 gene in Escherichia coli isolated from livestock between 2013 and 2015 in South Korea. Antimicrob Agents Chemother. 2016;60:6991–6993. doi: 10.1128/AAC.01472-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.The Joint CLSI-European Committee on Antimicrobial Susceptibility Testing (EUCAST) Polymyxin Breakpoints Working Group. Recommendations for MIC determination of colistin (polymyxin E) Wayne, PA: Clinical and Laboratory Standards Institute; 2016. [Updated on Mar 2016]. http://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/General_documents/Recommendations_for_MIC_determination_of_colistin_March_2016.pdf. [Google Scholar]
- 23.Hong JS, Yoon EJ, Lee H, Jeong SH, Lee K. Clonal Dissemination of Pseudomonas aeruginosa sequence type 235 isolates carrying blaIMP-6 and emergence of blaGES-24 and blaIMP-10 on novel genomic islands PAGI-15 and -16 in South Korea. Antimicrob Agents Chemother. 2016;60:7216–7223. doi: 10.1128/AAC.01601-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Poirel L, Kieffer N, Brink A, Coetze J, Jayol A, Nordmann P. Genetic features of MCR-1-producing colistin-resistant Escherichia coli isolates in South Africa. Antimicrob Agents Chemother. 2016;60:4394–4397. doi: 10.1128/AAC.00444-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim ES, Chong YP, Park SJ, Kim MN, Kim SH, Lee SO, et al. Detection and genetic features of MCR-1-producing plasmid in human Escherichia coli infection in South Korea. Diagn Microbiol Infect Dis. 2017;89:158–160. doi: 10.1016/j.diagmicrobio.2017.06.020. [DOI] [PubMed] [Google Scholar]
- 26.Fernandes MR, McCulloch JA, Vianello MA, Moura Q, Pérez-Chaparro PJ, Esposito F, et al. First report of the globally disseminated IncX4 plasmid carrying the mcr-1 gene in a colistin-resistant Escherichia coli Sequence Type 101 isolate from a human infection in Brazil. Antimicrob Agents Chemother. 2016;60:6415–6417. doi: 10.1128/AAC.01325-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Elnahriry SS, Khalifa HO, Soliman AM, Ahmed AM, Hussein AM, Shimamoto T, et al. Emergence of plasmid-mediated colistin resistance gene mcr-1 in a clinical Escherichia coli isolate from Egypt. Antimicrob Agents Chemother. 2016;60:3249–3250. doi: 10.1128/AAC.00269-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bradley DE, Coetzee JN. The determination of two morphologically distinct types of pilus by plasmids of incompatibility group I2. J Gen Microbiol. 1982;128:1923–1926. doi: 10.1099/00221287-128-8-1923. [DOI] [PubMed] [Google Scholar]
- 29.Yoshida T, Kim SR, Komano T. Twelve pil genes are required for biogenesis of the R64 thin pilus. J Bacteriol. 1999;181:2038–2043. doi: 10.1128/jb.181.7.2038-2043.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Akahane K, Sakai D, Furuya N, Komano T. Analysis of the pilU gene for the prepilin peptidase involved in the biogenesis of type IV pili encoded by plasmid R64. Mol Genet Genomics. 2005;273:350–359. doi: 10.1007/s00438-005-1143-8. [DOI] [PubMed] [Google Scholar]
- 31.Komano T, Kim SR, Yoshida T, Nisioka T. DNA rearrangement of the shufflon determines recipient specificity in liquid mating of IncI1 plasmid R64. J Mol Biol. 1994;243:6–9. doi: 10.1006/jmbi.1994.1625. [DOI] [PubMed] [Google Scholar]
- 32.Sun J, Fang LX, Wu Z, Deng H, Yang RS, Li XP, et al. Genetic analysis of the IncX4 plasmids: implications for a unique pattern in the mcr-1 acquisition. Sci Rep. 2017;7:424. doi: 10.1038/s41598-017-00095-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yoon EJ, Yang JW, Kim JO, Lee H, Lee KJ, Jeong SH. Carbapenemase-producing Enterobacteriaceae in South Korea: a report from the National Laboratory Surveillance System. Future Microbiol. 2018;13:771–783. doi: 10.2217/fmb-2018-0022. [DOI] [PubMed] [Google Scholar]
- 34.Edgar RC. MUSCLE: multiple sequence alignment with high accuracy and high throughput. Nucleic Acids Res. 2004;32:1792–1797. doi: 10.1093/nar/gkh340. [DOI] [PMC free article] [PubMed] [Google Scholar]