Abstract
Objectives
To describe the variation across neonatal intensive care units (NICUs) in missed nursing care in disproportionately black and non‐black‐serving hospitals. To analyze the nursing factors associated with missing nursing care.
Data Sources/Study Setting
Survey of random samples of licensed nurses in four large U.S. states.
Study Design
This was a retrospective, secondary analysis of 1,037 staff nurses in 134 NICUs classified into three groups based on their percent of infants of black race. Measures included the average patient load, individual nurses’ patient loads, professional nursing characteristics, nurse work environment, and nursing care missed on the last shift.
Data Collection
Survey data from a Multi‐State Nursing Care and Patient Safety Study were analyzed (39 percent response rate).
Principal Findings
The patient‐to‐nurse ratio was significantly higher in high‐black hospitals. Nurses in high‐black NICUs missed nearly 50 percent more nursing care than in low‐black NICUs. Lower nurse staffing (an additional patient per nurse) significantly increased the odds of missed care, while better practice environments decreased the odds.
Conclusions
Nurses in high‐black NICUs face inadequate staffing. They are more likely to miss required nursing care. Improving staffing and workloads may improve the quality of care for the infants born in high‐black hospitals.
Keywords: Missed nursing care, nurse staffing, nurse work environment, health disparities, very low birthweight infants
Premature birth accounts for most admissions to neonatal intensive care units (NICUs). More than a third of total infant deaths annually (36 percent) are preterm related (Mathews, MacDorman, and Thoma 2015). Black infants are disproportionately born prematurely, at a rate that is 60 percent higher than for white infants, contributing to the comparatively higher rates of mortality among black infants (Hamilton, Martin, and Osterman 2016). Mortality rates in the first month of life are 2.2 times higher for black infants than for white infants (Mathews, MacDorman, and Thoma 2015). Many studies have investigated the causes for disparities in rates of premature birth, such as socioeconomic status, but little is known about how nursing care that premature infants receive in the NICU contributes to survival and health disparities. Yet this is a critical period as two‐thirds of mortality among black infants occurs in the first month of life when these infants are being cared for in the NICU (Mathews, MacDorman, and Thoma 2015).
Black newborns are concentrated in relatively few hospitals whose quality of care has disproportionate influence on most black infants’ health outcomes (Lake et al. 2015). Prior research demonstrates that all very low birthweight (VLBW) infants, irrespective of race, who are born and cared for in NICUs that serve a disproportionate number of black infants have higher rates of neonatal mortality, nosocomial infection, and lower rates of discharge home on breastmilk (Morales et al. 2005; Howell et al. 2008; Lake et al. 2015). Further, NICUs in disproportionately black hospitals have lower nurse staffing levels and poorer work environments (Lake et al. 2015). These features of the NICU workplace have been demonstrated to be associated with poorer outcomes for VLBW infants, including higher rates of mortality, and nosocomial infection and discharge home on breastmilk (Lake et al. 2015). The mechanisms through which nurse understaffing and poor work environments affect patient outcomes, and therefore disparities, are unknown.
In this study, the authors study missed nursing care, which is a potential mechanism for outcome disparities, Missed nursing care is a process of care measure, defined as required nursing care that is omitted or delayed in response to multiple demands or inadequate resources (Kalisch, Landstrom, and Williams 2009). The objectives of this study were to describe the variation across NICUs in missed nursing care overall and in disproportionately black and non‐black‐serving hospitals. The nursing care missed for all infants, not solely VLBW infants, was the focus. The authors also aimed to identify individual and organizational factors that influence disparities in nursing care and sought to ascertain whether individual and nursing unit factors are associated with missed nursing care. This will enable the authors to identify points of intervention to improve the completion of required care.
Background
Infants cared for in the NICU are the most vulnerable hospitalized infants. Very low birthweight infants, a particularly vulnerable subgroup, account for half of NICU days (Rogowski et al. 2013) Considerable research has focused on this subgroup. Very low birthweight infants suffer a high death rate (22 percent), which occurs largely in the first month of NICU hospitalization (89 percent) (Mathews, MacDorman, and Thoma 2015). Many VLBW infants (15 percent) develop a hospital‐acquired infection (Horbar et al. 2012), which increases the length of stay by 4–7 days (Payne et al. 2004) and more than doubles the mortality risk (Stoll et al. 2002). Lengths of stay in the NICU are among the longest of any population. For VLBW infants, the length of stay is on average 64 days, notably longer than the average of 15 days for other NICU infants (statistics derived from tabulations of Vermont Oxford Network [VON] data, which is a voluntary quality collaborative that contains data on nearly 90 percent of VLBW infants born annually). The long hospital stays increase the potential exposure to poor nursing performance, thus compounding its negative effect.
Prior research demonstrates that inadequate nurse staffing and poor work environments are associated with poorer outcomes for VLBW infants treated in the NICU (Rogowski et al. 2013; Lake et al. 2015, 2016b; Hallowell et al. 2016). Missed nursing care in these situations may be associated with poor outcomes, including hospital‐level outcome disparities. Because of the complexity of care required for NICU infants, their fragile health status, and their anatomic, physiologic, and immunologic immaturity, they simultaneously have a high risk for adverse outcomes and a low tolerance for poor care processes. Optimal care of these infants requires skilled nursing, with the average NICU nurse caring for two or three infants of varying acuity levels (Rogowski et al. 2015). However, the ways in which nurse staffing and the work environment affect outcomes have not been determined. A theoretically plausible mechanism is missed nursing care.
Evidence about missed nursing care, its negative consequences for patient outcomes, and related organizational factors has emerged recently in multiple patient populations internationally (Papastavrou, Andreou, and Efstathiou 2013; Ausserhofer et al. 2014; Jones, Hamilton, and Murry 2015; Kalisch 2015), but there is very little evidence about NICU care. In adult populations, missed nursing care has been linked to patient satisfaction, adverse events, mortality, and readmission (Schubert et al. 2008, 2012; Kalisch, Xie, and Dabney 2013; Brooks Carthon 2015; Lake, Germack, and Viscardi 2016a). Missed nursing care has been linked to disparities for older black adults re‐admitted for acute myocardial infarction (Brooks‐Carthon et al. 2016). The only published evidence on NICU patients comes from three studies: survey data from 230 certified neonatal nurses suggesting that system factors contribute to missed nursing care (Tubbs‐Cooley et al. 2015); nine Quebec NICUs linking the work environment to missed care (Rochefort and Clarke 2010); and a single‐hospital U.S. study linking delayed feeding (a type of missed care) of NICU infants to time required to achieve full oral feedings and length of stay (Tubbs‐Cooley, Pickler, and Meinzen‐Derr 2015). Missed nursing care presents ethical concerns for nurses because they do not have the time or capacity to deliver all needed care (Papastavrou, Andreou, and Efstathiou 2013).
In this study, the authors consider prevalence and determinants of missed nursing care in hospitals with high, medium, and low proportions of black infants. The investigators explore whether earlier evidence of outcome disparities is due to nurses in high‐black hospitals being unable to complete necessary nursing care.
This study contributes to nursing science by extending inquiry on missed care to health disparities. It extends theory on the sources of health disparities. The study contributes to neonatal care by providing an actionable focus for nurse managers if outcome disparities are due to missed nursing care. It also contributes to neonatal care by providing a description of the most and least frequently missed care activities, which draws attention to particular care domains. Separate from potential disparities, the study reveals the extent of missed care in NICUs generally, which is a concern given the critical illness of the infant population.
Methods
The authors used a retrospective cross‐sectional design to conduct a secondary analysis of linked nurse survey and administrative data in four states. The methodological orientation underpinning the study is that nursing system features, such as workload, work environment, and clinical care processes, including missed nursing care, can be measured through multihospital surveys of staff nurses (Aiken, Sochalski, and Lake 1997).
Sample, Setting, and Data Sources
The sample was derived from an existing dataset that was generated from the 2006 University of Pennsylvania Multi‐State Nursing Care and Patient Safety Study (Aiken et al. 2011). Surveys were mailed to the homes of a random samples of licensed registered nurses (n = 272,783) in New Jersey, Pennsylvania, California, and Florida with a 39 percent response rate. Analysis of American Hospital Association (AHA) survey data on the number of employed nurses per hospital showed that the number of respondents per hospital was proportional to employed nurses. A nonresponder survey, with a 91 percent response rate, showed no significant response bias in the original respondent pool on job‐related variables, including assessment of the work environment (Smith 2009). Nurses reported their institution of employment and details of nursing care, including missed nursing care. The nurse sample selection for the current study entailed identifying hospitals that had at least three NICU staff nurse respondents with nonmissing data on patient load, a major nurse‐level independent variable. The minimum of three nurses was based on prior research establishing a minimum to achieve reliable measures at the nursing unit level (Lake et al. 2016b). The study size was arrived at by applying the inclusion criteria and was noted to be similar to another study that achieved significant results (Lake et al. 2016b). This sampling approach yielded 1,037 nurses in 134 nonfederal, acute care hospitals. The sample hospitals represent 16 percent of NICUs nationally, based on authors’ calculations from 2006 AHA data on hospitals with nonzero NICU beds.
The authors received Institutional Review Board approval from the principal investigator's institution before the study began.
Measures
In prior work with the VON, an international neonatal care quality consortium that comprises a large fraction of U.S. NICUs and VLBW births, the authors developed categories of NICUs based on the percent of black VLBW infants. Three terciles of hospitals were identified (<11 percent, 11–31 percent, >31 percent black) from the VLBW infants born in the 578 U.S. Vermont Oxford Network hospitals in 2007–2008 (Lake et al. 2015). Two years of data provided more stable estimates of the percentages of black infants in smaller NICUs. Black‐serving hospital was defined as having a high fraction of black VLBW infants. Hospitals were classified as low, medium, and high black serving. Non‐Hispanic black infants were categorized as black. All other infants were categorized as non‐black.
Missed nursing care was defined as activities that were necessary but left undone due to lack of time. The tool to measure missed nursing care was originally chosen for the study that generated the nurse survey data. This tool was considered satisfactory for the current study because of its extensive use in international research (Ausserhofer et al. 2014) and evidence from an exploratory factor analysis (Bruyneel et al. 2015). The factor analysis of data from 12 European countries identified two domains of missed care (clinical and planning/communication). All items loaded onto one of the two domains. For this tool, nurses responded to the question, “On the most recent day you worked, which of the following activities were necessary but left undone because you lacked the time to complete them?” They marked all items that applied on a list of 12 items. The clinical domain comprises surveillance, skin care, oral hygiene, pain management, treatments and procedures, and administering medication on time. The planning/communication domain comprises comfort/talk with patients, teach/counsel patient/family, documentation, prepare patients/family for discharge, develop/update care plans, and care coordination (Bruyneel et al. 2015). Missed care was measured as when the nurse missed at least one activity, missed a particular activity, and the number of activities missed overall as well as in the clinical and planning/communication domains. Missed care was measured at the hospital level as the percent of nurses who missed at least one activity (considered prevalence of missed care) and the average number of activities missed overall as well as in the two domains.
Nursing variables included the nurse's patient load, nurse professional characteristics, nursing unit staffing, and the nurse work environment. The nurse's patient load was defined as the number of patients assigned on a shift. Nurses’ response to the question “On the most recent shift you worked, how many patients were assigned to you?” measured patient load. Nurse professional characteristics were defined as nursing educational background, length of experience, and specialty certification. The nurse reported their highest degree in nursing. Respondents’ educational levels were either having at least a baccalaureate degree or having a diploma or associate degree. Nurses reported the number of years of experience as a registered nurse and if they had a nationally recognized specialty practice certification. Nursing unit staffing was defined as the average number of patients‐per‐registered nurse on a unit. This was measured from separate survey questions about how many RNs provided direct patient care and how many patients were on your unit on the most recent shift you worked. Nursing unit staffing was calculated as the mean number of patients‐per‐nurse. The nurse work environment was defined as the organizational characteristics that promote or undermine professional nurse autonomy (Lake 2002). The tool to measure the nurse work environment, the Practice Environment Scale of the Nursing Work Index (PES‐NWI) (Lake 2002), was originally chosen for the study that generated the nurse survey data. This tool was considered satisfactory for the current study because it is endorsed as a national nursing performance measure by the National Quality Forum (NQF 2016). The global reliability and validity of this measure have been documented extensively (Warshawsky and Havens 2010). This 31‐item measure asks nurses to “indicate the extent to which you agree that each of the following features is present in your primary job.” The four‐category Likert responses range from strongly disagree to strongly agree. The instrument includes five subscales that measure nurse participation in hospital affairs, the nurse manager's ability and leadership, nursing foundations for quality, nurse–physician collegial relations, and staffing and resource adequacy. A composite score, calculated as the mean of the five subscales, was used for descriptive and regression analyses.
Neonatal intensive care unit characteristics included the level of care and size. NICU level of care was defined as the complexity of treatments. Levels of care defined by the American Academy of Pediatrics (AAP) (American Academy of Pediatrics Committee on Fetus and Newborn 2012) were used. The AAP definitions were based on functional capabilities, principally duration and type of respiratory support, provision of sustained life support, presence of or access to a range of pediatric specialists, and capacity for surgical repair of congenital anomalies or acquired conditions. Neonatal intensive care unit size was defined as number of patients, measured from the nurse survey data as the mean across respondents within a nursing unit of the number of patients on the unit on the most recent shift.
To describe the hospital sample, AHA annual hospital survey data were used to create measures of hospital size, children's hospital status, teaching status, and capability of high technology. Hospital size was defined as the number of inpatient hospital beds. Hospitals were classified into small (under 250 beds), medium (250–500 beds), and large (over 500 beds). Teaching status was defined as teaching commitment to medical interns and residents. Teaching status was classified according to the number of trainees per bed: none, minor (less than one trainee to four beds), and major (one or more trainees to four beds). High‐technology capability was defined as being able to provide services requiring highly sophisticated technology. This capability was indicated by performance of open‐heart surgery or organ transplantation.
Missing data were minimal for all variables. Data for workload were complete based on sample inclusion criteria. Practice Environment Scale of the Nursing Work Index subscale values were missing for up to 2.8 percent of cases. The hospital‐level aggregate PES‐NWI composite score was calculated omitting cases with missing data. Nurse characteristics were missing for education (5.5 percent), certification (1.54 percent), and experience (0.96 percent). The dependent variable, missed nursing care, has no missing data because the respondent indicates only activities that were missed. If all activities are left blank (i.e., not checked), this indicates no missed care.
Data Analysis
This study focused on hospital concentrations of black infants, nursing factors, and missed nursing care. Descriptive and inferential statistical methods were used for the data analysis. Calculation of descriptive statistics with significance tests for comparisons and estimation of regression models were used. Missing data for the nurse professional characteristics were addressed by including dummy variables for missing in the regression models. Characteristics of the hospital and NICU samples were described overall and in the three hospital black‐concentration subgroups. To evaluate sample representativeness, the authors compared hospital characteristics in our sample with those of the universe of hospitals with a NICU identified as having nonzero NICU beds in the AHA survey data.
For each missed care measure, the authors compared the prevalence or frequency in hospitals with high and low concentrations of black infants and calculated a z‐statistic. For these comparisons to best measure the disparity, we excluded the middle tercile because the contrast of interest was between the highly and least concentrated. Nursing unit staffing and work environment were described overall and in the three hospital subgroups. The high to low subgroup values were compared. We estimated four nurse‐level random‐effects logistic regression models by the method of maximum likelihood for the dependent variable “any missed care.” The random effects applied to the hospital level. The first model included only terciles for concentrations of black infants (high, middle, with low as the reference category) as the independent variables. The second added two NICU nursing variables that have been associated with missed nursing care in other populations (staffing and work environment). The third added nurse‐level characteristics: patient load, Bachelor of Science in Nursing degree, years of RN experience, and RN certification. The fourth added two NICU‐level covariates: American Academy of Pediatrics level and census. The random effect corrects the standard errors for within‐hospital correlation (clustering) in nurse outcomes. The analyses were conducted using Stata statistical software version 14 (StataCorp. 2015).
Results
The sample hospitals were predominantly medium‐sized, high‐technology teaching institutions: 51 percent had 250–500 beds; 70 percent had minor or major teaching commitment (Table 1). Almost three‐quarters (74 percent) had high‐technology capability. The majority (73 percent) were not freestanding children's hospitals or children's hospitals within a hospital. Over half (57 percent) of the hospitals were in California; 19 percent were in Pennsylvania; 13 percent were in Florida; and 11 percent in New Jersey. Compared to the universe of hospitals with a NICU in the United States, the sample was representative in that the majority (45 percent) of U.S. hospitals with a NICU were in the 250–500 bed range, and 73 percent had high‐tech status. However, the sample had disproportionately more teaching hospitals (70 percent vs. 46 percent nationally). As compared to low‐black hospitals, the high‐black hospitals were disproportionately larger teaching institutions. High‐black hospitals were located disproportionately in Florida and low‐black hospitals in California.
Table 1.
Characteristics of Hospitals and NICUs (n = 134)
| Participantsa | |||||
|---|---|---|---|---|---|
| Concentration of VLBW Black Infantsb | |||||
| Total | Low (<11%) | Medium (11–31%) | High (>31%) | p Value of High vs. Lowc | |
| Number of hospitals | N = 134 | N = 49 | N = 54 | N = 31 | |
| Hospital characteristics | |||||
| Bed size | .01 | ||||
| ≤250 beds | 20 | 27 | 24 | 3 | |
| 250–500 beds | 51 | 55 | 46 | 55 | |
| >500 beds | 28 | 18 | 30 | 42 | |
| Teaching hospital | .02 | ||||
| Non | 31 | 41 | 24 | 26 | |
| Minor | 46 | 47 | 50 | 35 | |
| Major | 24 | 12 | 26 | 39 | |
| High technology | 74 | 82 | 67 | 74 | .43 |
| Child hospital type | .23 | ||||
| General | 73 | 80 | 69 | 71 | |
| Freestanding | 8 | 8 | 11 | 3 | |
| Nested | 19 | 12 | 20 | 26 | |
| State | .00 | ||||
| California | 57 | 84 | 57 | 13 | |
| Pennsylvania | 19 | 16 | 19 | 26 | |
| Florida | 13 | 0 | 9 | 39 | |
| New Jersey | 11 | 0 | 15 | 23 | |
| NICU characteristics | |||||
| AAP level | .09 | ||||
| II | 8 | 14 | 7 | 0 | |
| III | 71 | 65 | 74 | 74 | |
| IV | 21 | 20 | 19 | 26 | |
| NICU census, mean (SD)d | 24 (14) | 21 (11) | 24 (16) | 29 (14) | .00 |
Data are expressed as % of hospitals unless otherwise indicated.
Concentrations were based on national Vermont Oxford Network 2007–2008 data.
The chi‐square test was used for comparison of categorical variables and the two‐tailed t‐test for continuous variables for comparison of high‐ to low‐black hospitals.
NICU census was measured from the nurse survey data as the mean across respondents within a nursing unit of the number of patients on the unit on the most recent shift.
AAP, American Academy of Pediatrics; NICU, neonatal intensive care unit; VLBW, very low birthweight.
Most sample NICUs (71 percent) were AAP Level III, followed by Levels IV (21 percent) and II (8 percent). This is similar to the AAP distribution across the United States, in which most NICUs were Level III (71 percent). The mean NICU census was 24, which was similar to the national mean of 26. In this sample, NICU level and bed size did not differ across high‐ and low‐black NICUs. There were 1,037 nurses who met sample inclusion criteria. The average number of nurse respondents per hospital was 7.7 (range 3–28).
On average, nurses missed 1.23 care activities of 12 (Table 2). Nurses in high‐black NICUs missed nearly 50 percent more activities than nurses in low‐black NICUs (1.51 vs. 1.05, p = .03). Most of the missed care was in the planning/communication domain (1.00); few activities in the clinical domain were missed (0.23). There were marginally significant differences between the high‐ and low‐black NICUs (p = .06 for the clinical domain; p = .05 for planning/communication). On average, 44 percent of nurses missed one or more necessary nursing activity (Table 2). This proportion differed significantly between high‐ and low‐black NICUs: 52 percent vs. 38 percent. The proportions of nurses who missed particular activities varied from a low of 1.7 percent for pain management to a high of 27.8 percent for “develop or update care plan” (Figure 1). The proportions differed for three activities: teach/counsel patients and family (25.2 percent vs. 16.8 percent, p = .03), administer medications on time (10.1 percent vs. 4.4 percent, p = .01), and comfort/talk with patients (22.6 percent vs. 14.4 percent, p = .02).
Table 2.
Distribution of Missed Care across NICUS, Overall, and by Hospital Concentration of Black VLBW Infants
| Total | Concentration of VLBW Black Infants | p Value of High vs. Lowa | |||
|---|---|---|---|---|---|
| Low (<11%) | Medium (11–31%) | High (>31%) | |||
| Number of hospitals | N = 134 | N = 49 | N = 54 | N = 31 | |
| Missed nursing care | |||||
| Total number of care activities missed, mean total (SD) | 1.23 (0.92) | 1.05 (0.91) | 1.23 (0.89) | 1.51 (0.97) | .03 |
| Clinical activities missed, mean total (SD) | 0.23 (0.37) | 0.17 (0.31) | 0.24 (0.40) | 0.33 (0.40) | .06 |
| Planning/communication activities missed, mean total (SD) | 1.00 (0.66) | 0.89 (0.68) | 1.00 (0.60) | 1.18 (0.74) | .05 |
| At least one activity missed, mean percent (SD) | 44.0 (22.60) | 38.0 (20.51) | 44.8 (23.07) | 51.9 (22.95) | .01 |
Values are means, with SDs in parentheses.
The unpaired two‐tailed t‐test was used for continuous variables for comparison of high‐ to low‐black hospitals.
VLBW, very low birthweight.
Figure 1.
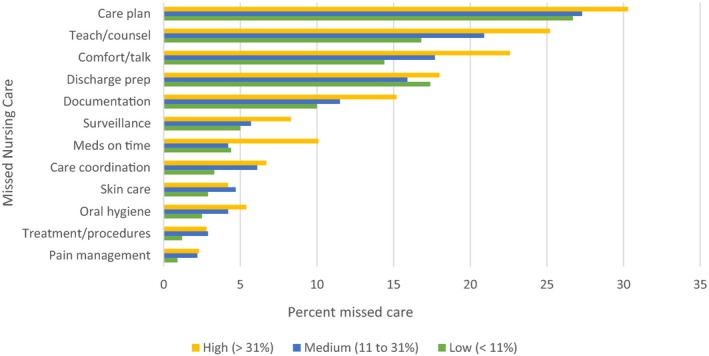
- Note. Percent missed care: High (>31 percent); Medium (11–31 percent); Low (<11 percent).
Regarding NICU nursing characteristics (Table 3), the average patient‐to‐nurse ratio (nursing unit staffing) was 2.32 overall (SD = 0.46). This differed significantly between high‐ and low‐black hospitals: 2.50 and 2.20, respectively (p = .04). The Practice Environment Scale composite across sample units on average was 2.87 and did not differ in the high‐ and low‐black NICUs. For context, an average value of 3.00 indicates nurses “agree” that the 31 desirable features of professional work environments are present in their current job. An average of 2.50 would indicate neither agreement nor disagreement. The NICU nursing staff was highly qualified; half (49 percent) had a bachelor's degree in nursing. Registered nurse experience averaged 18.7 years, and 38 percent of nurses had specialty certification. The profile of staff characteristics was similar in the high‐ and low‐black NICU groups. The mean patient load for the nurse sample was 2.52, SD = 0.88.
Table 3.
Distribution of Neonatal Intensive Care Unit Nursing Characteristics
| Concentration of VLBW Black Infants | |||||
|---|---|---|---|---|---|
| Total | Low (<11%) | Medium (11–31%) | High (>31%) | p Value of High vs. Lowa | |
| Number of hospitals | N = 134 | N = 49 | N = 54 | N = 31 | |
| Unit‐level measures | |||||
| Patients‐per‐registered nurse, mean (SD) | 2.32 (0.46) | 2.20 (0.41) | 2.32 (0.47) | 2.50 (0.46) | .00 |
| Practice environment scale composite, mean (SD) | 2.87 (0.33) | 2.88 (0.30) | 2.89 (0.34) | 2.84 (0.35) | .65 |
Values are means, with SDs in parentheses.
The unpaired two‐tailed t‐test was used for continuous variables for comparison of high‐ to low‐black hospitals.
VLBW, very low birthweight.
In unadjusted regression models (Table 4), the likelihood that a nurse in a high‐black NICU missed necessary care was 1.87 (95 percent CI: 1.25–2.80; p = .00) as compared to a low‐black NICU. After the addition of nursing unit staffing and practice environment, the high‐black effect was reduced but still significant (OR = 1.50; 95 percent CI: 1.03–2.17). Lower nurse staffing (an additional infant per nurse) increased the odds of missed care by 1.39 (95 percent CI: 1.00–1.92; p = .05). A better practice environment (i.e., a one unit increase in the PES‐NWI composite score) decreased the odds by more than half (OR = 0.32; 95 percent CI: 0.20–0.53; p = .00). In a model that added nurse‐level measures, the nurse's patient load was significantly associated with missed care. An additional infant increased the odds of missed care to 1.54 (95 percent CI: 1.30–1.82; p = .00). The unit‐level staffing was no longer significant. Greater nurse experience reduced the odds of missing care; one additional year of experience reduced the odds by 1 percent. In this model, the high‐black effect was no longer significant. In a final model that controlled for NICU level and size, the nurse's patient load and the practice environment remained significant, with odds ratios similar to the previous model. In addition, certified nurses were more likely to miss nursing care (OR = 1.32; 95 percent CI: 1.00–1.74, p = .047).
Table 4.
Odds Ratios Estimating the Association of Hospital Concentration of Black Infants, NICU, and Nursing Variables with a Nurse Missing at Least One Necessary Care Activity
| Odds Ratio | ||||
|---|---|---|---|---|
| Unadjusted | Adjusted for NICU Nursing Characteristics | Adjusted for Nursing and Nurse Characteristics | Adjusted for NICU Nursing, Nurse, and NICU Characteristics | |
| Concentration of black infants | ||||
| Low (<11%) | Reference | Reference | Reference | Reference |
| Medium (11–31%) | 1.38 (0.97–1.97) | 1.33 (0.96–1.83) | 1.31 (0.93–1.84) | 1.27 (0.90–1.78) |
| High (>31%) | 1.87b (1.25–2.80) | 1.50a (1.03–2.17) | 1.39 (0.94–2.05) | 1.24 (0.83–1.85) |
| NICU nursing characteristics | ||||
| Nursing unit average patient load | 1.39 (1.00–1.92) | 1.11 (0.78–1.58) | 1.14 (0.79–1.65) | |
| Practice environment scale composite | 0.32c (0.20–0.53) | 0.33c (0.19–0.55) | 0.35c (0.21–0.59) | |
| Nurse‐level measures | ||||
| Patient load | 1.54c (1.30–1.82) | 1.57c (1.33–1.86) | ||
| BSN degree | 1.21 (0.93–1.59) | 1.18 (0.90–1.55) | ||
| Years as a registered nurse | 0.99a (0.98–1.00) | 0.99 (0.98–1.00) | ||
| Registered nurse certification | 1.32a (1.01–1.74) | 1.32a (1.00–1.74) | ||
| Other NICU characteristics | ||||
| AAP Level II | 0.93 (0.49–1.79) | |||
| AAP Level III | Reference | |||
| AAP Level IV | 1.35 (0.93–1.97) | |||
| NICU census – natural log | 1.32 (0.98–1.78) | |||
Odds ratios were derived from random‐effects logistic regression models. N = 1,037 nurses.
p < .05.
p < .01.
p < .001.
AAP, American Academy of Pediatrics; BSN, Bachelor of Science in Nursing; NICU, neonatal intensive care unit.
Discussion
The authors were motivated to extend earlier work which demonstrated poorer infant outcomes in hospitals with a high concentration of black infants (Lake et al. 2015) by evaluating clinical processes that might explain the disparity. The study objectives were to describe the variation across NICUs in missed nursing care in disproportionately black and non‐black‐serving hospitals and to analyze the nursing factors associated with missing nursing care. This paper broadens the theoretical understanding of how health disparities occur by showing how nursing system disparities yield disparate clinical care processes.
Nurses in high‐black hospitals missed nearly 50 percent more required nursing care activities than nurses in low‐black hospitals (p = .03). Further, a significantly higher percentage of nurses in high‐black hospitals missed at least one required activity (52 percent vs. 38 percent). Although the differences in mean activities missed were numerically small (1.05 in the low‐black cohort to 1.51 in the high‐black cohort), research has shown that small differences can have a significant impact on patient outcomes (Schubert et al. 2009). The results from this sample, comprising 16 percent of U.S. NICUs, generalize principally to NICUs in large teaching hospitals.
The disparities in missed care were principally due to poorer nurse staffing in high‐black hospitals. The patient‐to‐nurse ratio was significantly higher in high‐black hospitals (2.5 and 2.2 patients‐per‐nurse, respectively). The odds of missed care increased by 40 percent in units with poorer staffing (one patient more per nurse). It is likely that staffing is worse in the high‐black hospitals because many treat a disproportionately high percentage of Medicaid and unfunded patients, which creates financial strain. Financial strain may affect clinical processes through allocation of staffing resources.
Nurse staffing is the most commonly observed organizational factor associated with missed nursing care (Jones, Hamilton, and Murry 2015). However, the nurse's own workload was more influential than unit‐level staffing. An additional patient in a nurse's workload increased the likelihood of missed care by 57 percent. Previous research on organizational determinants of missed nursing care has not explored both individual nurse workload and unit‐level staffing. This finding augments the literature by highlighting the influence of each infant assigned to a particular nurse. An additional patient per nurse is a common occurrence in the NICU setting where birth admissions arrive unexpectedly. Fluctuations in patient volume are common but unpredictable in the NICU. Without a requisite staff complement, these fluctuations have a deleterious effect on patient care. The odds of missing care were higher for certified nurses. These nurses care for more complex patients (Rogowski et al. 2015); the related demands may increase missed care.
The nursing practice environment was also influential in whether a nurse missed required care as identified in prior research in adult populations (Jones, Hamilton, and Murry 2015) and a single Canadian NICU study (Rochefort and Clarke 2010). Other work has demonstrated that NICU work environments vary considerably with PES‐NWI composite scores ranging from 2.42 to 3.97 in a sample of 104 hospitals nationally (Hallowell et al. 2014). This evidence demonstrates that better NICU practice environments are achievable in U.S. hospitals.
Neonatal intensive care unit nurses most often miss care planning, teaching families, and comforting infants and families. These results are consistent with evidence from Europe and the United States for nurses caring for hospitalized adults (Ausserhofer et al. 2014; Lake, Germack, and Viscardi 2016a). These planning and communication functions are missed significantly more often in black‐concentration NICUs. Within this domain, two activities are missed by more nurses in high‐black hospitals: teaching/counseling (25.2 percent vs. 16.8 percent) and comfort/talk (22.6 percent vs. 14.4 percent). Missing essential nursing care activities that involve the parents of critically ill infants reduces the potential for parents to be active participants in the infant's care and care decisions, undermines their caretaking abilities postdischarge, and may extend the length of hospital stay. In the clinical domain of missed care activities, giving medications on time differed significantly between high‐ and low‐black hospitals. Medications are an essential responsibility of nurses to maintain the homeostasis of critically ill infants (American Academy of Pediatrics and American College of Obstetricians and Gynecologists 2012).
Our study results have implications for nursing management, education, and practice. The care disparities reported here warrant the attention of managers in high‐black hospitals, which care for seven of ten black VLBW infants (Lake et al. 2015). Nurses in high‐black hospitals face stressful work conditions of insufficient staffing. Poor staffing is a principal driver of nurse burnout and turnover (Lake 1998). Managers should advocate for higher staffing levels, particularly in high‐black hospitals, and work to improve their unit work environment. Managers can evaluate their work environment using the PES‐NWI, which provides a template and domains to guide work environment improvements. Nurse managers should discuss missed nursing care with their staff to open the channels of communication about a problematic, underdiscussed phenomenon and to help them understand management motivation for changes. The implications of our study results for nursing education are to educate nurses about the concept, prevalence, and patterns of missed care and its systemic determinants (staffing; environment). The implications of our study results for practice are that NICU directors should promote conversations among care providers about the prevalence and nature of missed care, as well as promote a supportive culture to maximize care completion.
Future research should examine how missed nursing care contributes to NICU infant outcomes. A study of one missed care activity in the NICU, missed or delayed feeding, showed a significant impact on length of stay (Tubbs‐Cooley et al. 2015). The impact of missing multiple essential activities or activities relevant to the parental role has not been studied.
This study has multiple strengths. We account for both individual and aggregate (nursing unit level) workload. Prior missed care research has focused principally on aggregate staffing levels only, which is potentially problematic because they correlate with unobserved unit or hospital characteristics (Jones, Hamilton, and Murry 2015). Because we focus at the nurse level, those issues are less likely to be a concern. This study generates evidence about clinical disparities from a four‐state sample of 134 NICUs that complements evidence about outcome disparities in high‐black hospitals from an earlier sample of 104 NICUs nationally (Lake et al. 2015).
This study has several limitations. The cross‐sectional design prevents causal inference. However, it is not likely that missing nursing care increases nurse workloads. This sample best represents larger institutions with teaching capability. Although the data are from 2006, the unique content of the dataset is valuable and the relationships examined are not likely to have changed in the interim.
All critically ill infants and their parents deserve nursing care delivered in an effective, timely manner. NICU nurse staffing in hospitals with a high concentration of black infants is significantly worse than in low‐black hospitals, compromising the quality of nursing care as manifest in significantly more care missed. Outcome disparities accounted for by poorer nursing resources in prior research appear to be driven in part by incomplete nursing care. Hospital administrators in high‐black hospitals must attend to the care needs of their most vulnerable patients by cultivating supportive work environments for their staff, assuring that their unit is adequately staffed and that individual nurses are not overloaded.
Supporting information
Appendix SA1: Author Matrix.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This research was supported in part by grants to the Center for Health Outcomes and Policy Research from the National Institute of Nursing Research, National Institutes of Health (T32‐NR‐007104 and R01‐NR‐014855, L. Aiken, PI). This research was supported by the authors’ institutions: University of Pennsylvania, Dartmouth College, University of Vermont, and Rutgers, The State University of New Jersey. Dr. Staiger holds an equity interest in ArborMetric Inc, a company that sells efficiency measurement systems and consulting services to insurers and hospitals. The authors thank Dr. Linda Aiken for providing access to these data and Mr. Tim Cheney for statistical analysis. No other disclosures were reported. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institutes of Health.
Disclosures: None.
Disclaimer: None.
References
- Aiken, L. H. , Sochalski J., and Lake E. T.. 1997. “Studying Outcomes of Organizational Change in Health Services.” Medical Care 35 (11, Suppl.): NS6–18. [DOI] [PubMed] [Google Scholar]
- Aiken, L. H. , Cimiotti J. P., Sloane D. M., Smith H. L., Flynn L., and Neff D.. 2011. “The Effects of Nurse Staffing and Nurse Education on Patient Deaths in Hospitals with Different Nurse Work Environments.” Medical Care 49 (12): 1047–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Academy of Pediatrics and American College of Obstetricians and Gynecologists . 2012. Guidelines for Perinatal Care. Elk Grove Village, IL: American Academy of Pediatrics. [Google Scholar]
- American Academy of Pediatrics Committee on Fetus and Newborn . 2012. “Levels of Neonatal Care.” Pediatrics 130(3): 587–97. [DOI] [PubMed] [Google Scholar]
- Ausserhofer, D. , Zander B., Busse R., Schubert M., De Geest S., Rafferty A. M., Ball J., Scott A., Kinnunen J., Heinen M., Strømseng Sjetne I., Moreno‐Casbas T., Kózka M., Lindqvist R., Diomidous M., Bruyneel L., Sermeus W., Aiken L. H., Schwendimann R., and on behalf of the RN4CAST consortium . 2014. “Prevalence, Patterns and Predictors of Nursing Care Left Undone in European Hospitals: Results from the Multicountry Cross‐Sectional RN4CAST Study.” BMJ Quality & Safety 23 (2): 126–35. [DOI] [PubMed] [Google Scholar]
- Brooks Carthon, J. M. 2015. “The Quality of Hospital Work Environments and Missed Nursing Care Are Linked to Heart Failure Readmissions: A Cross Sectional Study of US Hospitals.” BMJ Quality and Safety 24 (4): 255–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks‐Carthon, J. M. , Lasater K. B., Rearden J., Holland S., and Sloane D. M.. 2016. “Unmet Nursing Care Linked to Rehospitalizations among Older Black AMI Patients: A Cross‐Sectional Study of US Hospitals.” Medical Care 54 (5): 457–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruyneel, L. , Li B., Ausserhofer D., Lesaffre E., Dumitrescu I., Smith H. L., Sloane D. M., Aiken L. H., and Sermeus W.. 2015. “Organization of Hospital Nursing, Provision of Nursing Care, and Patient Experiences with Care in Europe.” Medical Care Research and Review 72 (6): 643–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallowell, S. G. , Spatz D. L., Hanlon A. L., Rogowski J. A., and Lake E. T.. 2014. “Characteristics of the NICU Work Environment Associated with Breastfeeding Support.” Advances in Neonatal Care 14 (4): 290–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallowell, S. G. , Rogowski J. A., Spatz D. L., Hanlon A. L., Kenny M., and Lake E. T.. 2016. “Factors Associated with Infant Feeding of Human Milk at Discharge from Neonatal Intensive Care: Cross‐Sectional Analysis of Nurse Survey and Infant Outcomes Data.” International Journal of Nursing Studies 53: 190–203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton, B. E. , Martin J. A., and Osterman M. J. K.. 2016. “Births: Preliminary Data for 2015.” National Vital Statistics Reports: From the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System 65 (3): 15. [PubMed] [Google Scholar]
- Horbar, J. D. , Carpenter J. H., Badger G. J., Kenny M. J., Soll R. F., Morrow K. A., and Buzas J. S.. 2012. “Mortality and Neonatal Morbidity Among Infants 501 to 1500 Grams From 2000 to 2009.” Pediatrics 129 (6): 1019–26. [DOI] [PubMed] [Google Scholar]
- Howell, E. A. , Hebert P., Chatterjee S., Kleinman L. C., and Chassin M. R.. 2008. “Black/White Differences in Very Low Birth Weight Neonatal Mortality Rates Among New York City Hospitals.” Pediatrics 121 (3): e407–15. [DOI] [PubMed] [Google Scholar]
- Jones, T. , Hamilton P., and Murry N.. 2015. “Unfinished Nursing Care, Missed Care, and Implicitly Rationed Care: State of the Science Review.” International Journal of Nursing Studies 52: 1121–37. [DOI] [PubMed] [Google Scholar]
- Kalisch, B. 2015. Errors of Omission: How Missed Nursing Care Imperils Patients. Silver Spring, MD: American Nurses Association. [Google Scholar]
- Kalisch, B. J. , Landstrom G., and Williams R. A.. 2009. “Missed Nursing Care: Errors of Omission.” Nursing Outlook 57 (1): 3–9. [DOI] [PubMed] [Google Scholar]
- Kalisch, B. J. , Xie B., and Dabney B. W.. 2013. “Patient‐Reported Missed Nursing Care Correlated with Adverse Events.” American Journal of Medical Quality 29 (5): 415–22. [DOI] [PubMed] [Google Scholar]
- Lake, E. T. 1998. “Advances in Understanding and Predicting Nurse Turnover.” Research in the Sociology of Health Care 15: 147–71. [Google Scholar]
- Lake, E. T. . 2002. “Development of the Practice Environment Scale of the Nursing Work Index.” Research in Nursing & Health 25 (3): 176–88. [DOI] [PubMed] [Google Scholar]
- Lake, E. T. , Germack H. D., and Viscardi M. K.. 2016a. “Missed Nursing Care is Linked to Patient Satisfaction: A Cross‐Sectional Study of US Hospitals.” BMJ Quality & Safety 25: 535–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lake, E. T. , Staiger D., Patrick T., Horbar J., Kenny M. J., and Rogowski J.. 2015. “Disparities in Perinatal Quality Outcomes for Very Low Birth Weight Infants in Neonatal Intensive Care.” Health Services Research 50 (2): 374–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lake, E. T. , Hallowell S. G., Kutney‐Lee A., Hatfield L. A., Del Guidice M., Boxer B. A., Ellis L. N., Verica L., and Aiken L. H.. 2016b. “Higher Quality of Care and Patient Safety Associated with Better NICU Work Environments.” Journal of Nursing Care Quality 31 (1): 24–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathews, T. , MacDorman M. F., and Thoma M. E.. 2015. “Infant Mortality Statistics from the 2013 Period Linked Birth/Infant Death Data Set.” National Vital Statistics Reports: From the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System 64 (9): 1–30. [PubMed] [Google Scholar]
- Morales, L. S. , Staiger D., Horbar J. D., Carpenter J., Kenny M., Geppert J., and Rogowski J.. 2005. “Mortality Among Very Low‐Birthweight Infants in Hospitals Serving Minority Populations.” American Journal of Public Health 95 (12): 2206–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Quality Forum . 2016. “Practice Environment Scale ‐ Nursing Work Index (PES‐NWI) (composite and five subscales).” [accessed on April 15, 2016]. Available at http://www.qualityforum.org/QPS/0206
- Papastavrou, E. , Andreou P., and Efstathiou G.. 2013. “Rationing of Nursing Care and Nurse‐Patient Outcomes: A Systematic Review of Quantitative Studies.” International Journal of Health Planning and Management 29 (1): 3–25. [DOI] [PubMed] [Google Scholar]
- Payne, N. , Carpenter J., Badger G., Horbar J., and Rogowski J.. 2004. “Marginal Increase in Cost and Excess Length of Stay Associated with Nosocomial Bloodstream Infections in Surviving Very Low Birth Weight Infants.” Pediatrics 114 (2): 348–55. [DOI] [PubMed] [Google Scholar]
- Rochefort, C. M. , and Clarke S. P.. 2010. “Nurses’ Work Environments, Care Rationing, Job Outcomes, and Quality of Care on Neonatal Units.” Journal of Advanced Nursing 66 (10): 2213–24. [DOI] [PubMed] [Google Scholar]
- Rogowski, J. , Staiger D., Patrick T., Horbar J., Kenny M. J., and Lake E.. 2013. “Nurse Staffing And NICU Infection Rates.” JAMA Pediatrics 167 (5): 444–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogowski, J. A. , Staiger D. O., Patrick T. E., Horbar J. D., Kenny M. J., and Lake E. T.. 2015. “Nurse Staffing in Neonatal Intensive Care Units in the United States.” Research in Nursing & Health 38 (5): 333–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schubert, M. , Glass T. R., Clarke S. P., Aiken L. H., Schaffert‐Witvliet B., Sloane D. M., and De Geest S.. 2008. “Rationing of Nursing Care and Its Relationship to Patient Outcomes: The Swiss Extension of the International Hospital Outcomes Study.” International Journal for Quality in Health Care 20 (4): 227–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schubert, M. , Clarke S., Glass T., Schaffert‐Witvliet B., and De Geest S.. 2009. “Identifying Thresholds for Relationships Between Impacts of Rationing of Nursing Care and Nurse‐ and Patient‐Reported Outcomes in Swiss Hospitals: A Correlational Study.” International Journal of Nursing Studies 46 (7): 884–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schubert, M. , Clarke S. P., Aiken L. H., and de Geest S.. 2012. “Associations Between Rationing of Nursing Care and Inpatient Mortality in Swiss Hospitals.” International Journal for Quality in Health Care 2012 (24): 3. [DOI] [PubMed] [Google Scholar]
- Smith, H. L. 2009. “A Double Sample to Minimize Bias Due to Nonresponse in a Mail Survey.” Population Studies Center Working Papers. Philadelphia, PA: University of Pennsylvania. [Google Scholar]
- StataCorp . 2015. Stata/IC 14 for Windows.College Station, TX: StataCorp. [Google Scholar]
- Stoll, B. J. , Hansen N., Fanaroff A. A., Wright L. L., Carlo W. A., Ehrenkranz R. A., Lemons J. A., Donovan E. F., Stark A. R., Tyson J. E., Oh W., Bauer C. R., Korones S. B., Shankaran S., Laptook A. R., Stevenson D. K., Papile L.‐A., and Poole W. K.. 2002. “Late‐onset Sepsis in Very Low Birth Weight Neonates: The Experience of the NICHD Neonatal Research Network.” Pediatrics 110 (2): 285. [DOI] [PubMed] [Google Scholar]
- Tubbs‐Cooley, H. L. , Pickler R. H., and Meinzen‐Derr J. K.. 2015. “Missed Oral Feeding Opportunities and Preterm Infants’ Time to Achieve Full Oral Feedings and Neonatal Intensive Care Unit Discharge.” American Journal of Perinatology 32 (1): 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tubbs‐Cooley, H. L. , Pickler R. H., Younger J. B., and Mark B. A.. 2015. “A Descriptive Study of Nurse‐Reported Missed Care in Neonatal Intensive Care Units.” Journal of Advanced Nursing 71 (4): 813–24. [DOI] [PubMed] [Google Scholar]
- Warshawsky, N. E. , and Havens D. S.. 2010. “Global Use of the Practice Environment Scale of the Nursing Work Index.” Nursing Research 60 (1): 17–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.


