Abstract
Objective
We test whether nursing homes serving predominately low‐income and racial minority residents (compositional explanation) or located in neighborhoods with higher concentrations of low‐income and racial minority residents (contextual explanation) have worse financial outcomes and care quality.
Data Sources
Healthcare Cost Report Information System, Nursing Home Compare, Online Survey Certification and Reporting Certification, and American Community Survey.
Study Design
A cross‐sectional study design of nursing homes within U.S. metropolitan areas.
Data Collection/Extraction Methods
Data were obtained from Centers for Medicare & Medicaid Services and U.S. Census Bureau.
Principal Findings
Medicaid‐dependent nursing homes have a 3.5 percentage point lower operating ratio. Those serving primarily racial minorities have a 2.64‐point lower quality rating. A 1 percent increase in the neighborhood population living in poverty is associated with a 1.20‐point lower quality rating, on a scale from 10 to 50, and a 1 percent increase in the portion of neighborhood black residents is associated with a 0.8 percentage point lower operating ratio and a 0.37 lower quality rating.
Conclusions
Medicaid dependency (compositional effect) and concentration of racial minority residents in neighborhoods (contextual effect) are associated with higher fiscal stress and lower quality of care, indicating that nursing homes’ geographic location may exacerbate long‐term care inequalities.
Keywords: Nursing homes, health care disparities, neighborhoods, poverty areas
Inequalities in long‐term care in the United States are an understudied but critical issue. By 2029, more than 20 percent of the U.S. population is projected to be 65 years and older (Colby and Ortman 2015). While life expectancy among the elderly has been improving for many decades (Lubitz et al. 2003), there remain high disparities in long‐term care across socioeconomic groups. Given that 35 percent of those now turning 65 are expected to use nursing facilities (Kemper, Komisar, and Alecxih 2005) despite a shift toward home or community‐based services, nursing homes are important sites for studying unequal access to long‐term care among the elderly.
While geographic proximity is one important factor for access (Office of Disease Prevention and Health Promotion 2014), there are many nursing home closures due to financial problems (Castle et al. 2009). Approximately 16 percent of nursing facilities closed in the United States from 1999 to 2008, and these closures disproportionately affect neighborhoods with a high concentration of racial and ethnic minorities and poverty (Feng et al. 2011). Because location is the single most cited priority in nursing home selection (Shugarman and Brown 2006), the disproportionate rate of nursing home closures in low‐income and minority neighborhood may exacerbate limited access to care for elderly residents, thereby increasing long‐term care disparities (Feng et al. 2011).
Although higher nursing home closure rates have been documented in disadvantaged neighborhoods, the underlying causes for these geographical patterns are complex. It is critical to understand whether these mechanisms are due to either “composition” or “context” effects to answer the question of whether we should pay more attention to financial support for individual residents or the role of the environment, including reducing residential segregation by racial–socioeconomic class. In the Diez Roux (2001) framework, a neighborhood provides both “material and social characteristics” that may be related to health. To establish a conceptual framework for geographical patterning of access to nursing home services, we used a distinction between composition and context: Composition represents “the characteristics of individuals concentrated in particular places”; and context means “opportunity structures in the local physical and social environment” (i.e., area or group properties) (Duncan, Jones, and Moon 1998; Diez Roux 2001). For example, if an area exhibits a high smoking rate, it can be because the area has a high concentration of current smokers (compositional explanation) or because many cigarette retail outlets are located in the area (contextual explanation) (Diez Roux 2001; Macintyre, Ellaway, and Cummins 2002).
Similar to the effects of neighborhood composition and context on individuals’ health, past studies on nursing home performance offer mechanisms that can fit into this framework. One set of studies on nursing home finance has focused on compositional explanation, finding that that the demographic composition of nursing homes is correlated with quality of care and health outcomes. Historically, Medicaid, which disproportionately serves poor and minorities, has a lower reimbursement rate than Medicare and private insurance (Henry J. Kaiser Family Foundation 2013). Consequently, nursing homes with Medicaid dependency have fewer financial resources (Mor et al. 2004), which has been shown to contribute to lower quality of care, less staffing, less compliance with specific care elements (Mor et al. 2004; Bowblis 2011), and worse health outcomes (Harkey and Vraciu 1992). In addition, nursing homes with high proportion of black residents have lower financial viability and quality of care (Chisholm et al. 2013).
A second set of studies highlight the importance of neighborhood context, although not all studies are specific to nursing homes. Disadvantaged neighborhoods are less likely to have features of the physical and social environment that are conducive to health (Diez Roux 2001; Diez Roux and Mair 2010; Bower et al. 2014; Lee et al. 2015). This is because it is more difficult to attract and retain health care providers to economically and socially disadvantaged neighborhoods due to their limited health care infrastructures and frequent clinical, logistical, and administrative challenges (Fiscella and Williams 2004; White, Haas, and Williams 2012). This contributes to differences in qualifications and competency between physicians who primarily treat black patients versus physicians who primarily treat white patients (Bach et al. 2004). In addition, physicians working for plans with a high proportion of black patients provide a lower quality of care compared to those working for plans with a high proportion of white patients (Schneider, Zaslavsky, and Epstein 2002). These differences in quality of care are also observed among pharmacies: pharmacies located in segregated neighborhood are less likely to provide adequate medication supplies (Morrison et al. 2000).
In this study, we empirically tested the relationship between compositional factors (operationalized as the proportions of Medicaid‐dependent and racial minority residents within individual nursing homes) and contextual factors (operationalized as the proportion of low‐income and minority residents within the surrounding neighborhoods) on the fiscal stress and quality of care among nursing homes. The social epidemiology literature typically studies these effects on population health outcomes (LeClere, Rogers, and Peters 1998; Matteson, Burr, and Marshall 1998; Cubbin, LeClere, and Smith 2000; Truong and Ma 2006; Papas et al. 2007; Mair, Roux, and Galea 2008; Larson, Story, and Nelson 2009) and not on institutional outcomes such as facility closure rates, financial performances, or quality of care. At the same time, there is a robust health services literature on the determinants of these institutional outcomes, but the role of neighborhood contextual factors is understudied. Some of these relationships have previously only been assumed in the literature, and others have not yet been studied in the context of access to long‐term care. We used a hierarchical modeling strategy (with nursing homes nested within neighborhoods) to test the relationship between nursing homes’ fiscal stress and quality of care and (1) composition of nursing homes (variation in proportions of low‐income and racial minorities within nursing homes); and (2) neighborhood context (variation in proportions of racial minorities and low‐income residents within surrounding neighborhoods). We hypothesize that if compositional (high proportion of low‐income or racial minority residents in nursing home) and contextual (poverty concentrated or racial minority neighborhood) elements are present, there will be significant negative relationships between these compositional and contextual factors and financial viability and quality. By investigating the relationship between compositional and contextual factors and nursing homes’ fiscal stress and quality of care, we can infer the reason why there are geographical disparities in access to financially viable and high‐quality long‐term care institutions.
Methods
Study Design
A cross‐sectional study design was used to identify the relationship between compositional and contextual factors on nursing home fiscal stress and quality of care. The cross‐sectional design assesses whether individual nursing homes are systematically different from another (between variation), rather than changes in individual nursing homes over time (within variation). The unit of analysis of this study is approximately 9,800 skilled nursing homes (at a lower level) nested in zip codes (at a higher level) for every year from 2011 to 2013 in 350 U.S. metropolitan statistical areas (MSAs). The main outcomes are nursing home fiscal stress, measured by their operating ratios, and quality of care, measured by the Nursing Home Five‐Star Quality Rating.
Data
The data for this analysis come from three sources from 2011 to 2013. First, the Skilled Nursing Facility Cost Report (CMS‐2540‐96 and CMS‐2540‐10) from the Healthcare Cost Reporting Information System (HCRIS) was used. By law, all nursing facilities participating in the Medicare program are required to submit expense reports on an annual basis, and information cannot be carried forward to future years. The reports are “a true and accurate representation of the data on file at CMS.” CMS has reviewed the reports to improve data quality such as completeness and accuracy (Centers for Medicare and Medicaid Services 2017a). The HCRIS breaks down this information for cost and changes by cost center for every fiscal year since 1996 (Center for Medicare & Medicaid Services 2015).
Second, the Nursing Home Five‐Star Quality Rating System is used. The CMS created the system to help nursing home residents, families, and caregivers compare nursing homes’ quality of care (Centers for Medicare and Medicaid Services 2017b). Since December 2008, the CMS includes a set of quality ratings for each nursing home in Nursing Home Compare.
Third, the Online Survey Certification and Reporting (OSCAR) Certification and Survey Provider Enhanced Reporting (CASPER) data were merged with HCRIS and the Five‐Star Quality Rating System using the provider identifier. OSCAR/CASPER is a national administrative database collected by survey agencies during nursing facility annual certification inspections. These inspections occur at least once every 15 months and are maintained by the CMS (Brown University Center for Gerontology and Healthcare Research and the National Institute on Aging 2016).
Lastly, neighborhood characteristics of zip code–tabulated areas from 2011 through 2013 were downloaded from the American Community Survey (ACS) 5‐year estimates (U.S. Census Bureau 2016b). This survey is conducted every year with a randomly selected sample of addresses in every state and the District of Columbia.
Variables
Dependent Variables
Fiscal stress represents the situation where there are limited resources to provide services (Douglas and Gaddie 2002; Wang, Dennis, and Tu 2007). The first dependent variable, nursing homes’ fiscal stress, is operationalized by the operating ratio. This measure is commonly used in the research literature and monitors whether income derived from the organization's core business operations is sufficient to cover its expenses. It is calculated as the operating revenue divided by the operating expenses, with financially secure organizations having higher operating ratio values (Wang, Dennis, and Tu 2007; Stone et al. 2015). If operating ratios are smaller than 1, the nursing homes’ revenues do not cover its operating expenses, related to its main activities. There is no particular operating ratio that guarantees financially sustainable organization, and the definition of “high” or “low” operating ratios varies by industry. For nursing homes in this study, the median value of operating ratios is 1.19, which translates to 20 percent higher operating revenue than operating costs.
The Medicare payment system for nursing facilities, which may affect their revenues, changed minimally during the study period. Medicare payment is made following prospective payment system, where rates are adjusted for case mix and geographic variation, following the Balanced Budget Act of 1997 (Centers for Medicare and Medicaid Services 2013). Although states have changed Medicaid reimbursement rates, the effect of these changes on this cross‐sectional study design is minimal.
The second dependent variable is nursing homes’ five‐star quality rating. The score, ranging from 10 to 50, incorporates three separate aspects of nursing home overall quality: (1) health inspection, which reports deficiencies weighted by scope and severity during the three most recent annual inspection surveys and the most recent 36 months of complaint investigations; (2) staffing, measured as care hours by nursing staff per resident per day and adjusted for nursing homes’ severity of need; and (3) quality measures, describing how well nursing homes meet the physical and clinical needs of their residents (Centers for Medicare and Medicaid Services 2017b).
To better understand the specific mechanism of facility management, Appendix SA2 presents the correlation of nursing home overall quality rating (a dependent variable) and staffing information. Overall, staffing rating has the highest weight in determining the quality rating (0.47, p < .01). Registered nurses hours (correlation = 0.28, p < .01) and total licensed practical and vocational nurses (correlation = 0.23, p < .01) are highly positively correlated with quality rating. In addition, hourly wage is positively correlated with overall nursing home quality rating (correlation = 0.07, p < .01).
Independent Variables
Two levels of independent variables are used in this analysis. At the nursing home level (compositional explanation), the main independent variables were (1) Medicaid dependency (85 percent or more of the residents are supported by Medicaid and less than 8 percent are supported by Medicare); and (2) racial minority composition (40 percent or more of the residents are nonwhite) within nursing homes. Mor et al. (2004) defines “a lower‐tier facility” as a nursing home with 85 percent or more of the residents supported by Medicaid, less than 10 percent supported by private payers, and less than 8 percent supported by Medicare within nursing homes. Due to many missing values in private payer variable in our dataset, we omit the criteria for private payer to define Medicaid dependency. Nursing homes can shift costs by charging private payers more to compensate shortfalls in Medicaid payments within nursing homes (Frakt 2011). Two independent variables at the nursing home level are dichotomized because relatively extreme payer‐mix configurations yield minimum opportunities for cross‐subsidizing the residents’ care across Medicaid, private pay, and Medicare within nursing homes (Mor et al. 2004). When we did a robustness check using continuous variables for nursing home composition (nursing homes with high Medicaid and racial minority residents), the direction and significance of independent variables did not change. At the neighborhood level (contextual explanation), we use (1) the natural log of the population living under the poverty line in zip codes; and (2) the natural log of the number of racial minorities in zip codes (Schulz et al. 2002; Feng et al. 2011). The U.S. Census Bureau defines poverty using a set of income thresholds, which does not vary by geographical region, depending on family size and composition. If family's total income is below the family's income threshold, then all family members are considered impoverished (U.S. Census Bureau 2016a). Appendix SA3 presents the correlation among independent variables. Although all four independent variables are positively correlated, multicollinearity may not be a problem because correlation coefficients are low and the sample size is large.
Control Variables
We control for multiple nursing facility organizational characteristics that are commonly associated with financial performance and quality of care. For example, 62 percent skilled nursing facilities operate as chain, so the fiscal stress and quality of care in one facility should be explained by this factor. The first is organizational characteristics of the nursing homes: number of beds, occupancy rates, chain, market concentration (Herfindahl–Hirschman index, defined as the sum of squares of the number of beds within neighborhood), and ownership types (Chisholm et al. 2013). The second is facilities’ case mix (the spectrum of severity of cases that a specific nursing home handles [Chisholm et al. 2013; Weech‐Maldonado et al. 2012; Zinn et al. 2009]), and a cognitive function performance measure (proportion of residents with low cognitive impairment) to identify the nursing homes primarily focusing on mental disorders. The size of neighborhood is also controlled.
Model Specifications
We used two sets of models for our analyses: (1) ordinary least square (OLS) to estimate the relationship between nursing home composition and fiscal stress and quality of care; and (2) varying intercept hierarchical linear models (HLM), an extension of regression in which datasets consist of more than one level. We used HLM containing covariates at both the nursing home (compositional explanation) and neighborhood levels (contextual explanation) within the same model. These models are useful for nested data, with multiple nursing homes existing within neighborhoods. As there are nursing homes with multiple observations across years, information on specific nursing homes or neighborhoods may not greatly change over time. If this is the case, it is unlikely that all observations in a dataset are unrelated. To provide correct estimations, we used clustered standard error by nursing homes for nursing home–level estimations and repeated the same analysis for each year of the 3‐year period from 2011 to 2013 as a robustness check. Nursing home fixed effects estimation is not appropriate because it relies completely on variation within groups.
Results
Table 1 illustrates the summary characteristics of nursing homes in 350 MSAs from 2011 to 2013. The average operating ratio across all years in this study is 1.20, which is relatively consistent from 2011 to 2013. On average, 59.0 percent Medicaid residents and 18.0 percent racial minorities reside in nursing homes. The neighborhoods where nursing homes are located have, on average, 15.1 percent population under the poverty line and 12.4 percent of racial minorities. The summary statistics for the control variables in the regression analysis are also presented in Table 1.
Table 1.
Summary Characteristics of Nursing Homes in 350 Metropolitan Statistical Areas from 2011 to 2013
| Variable | 2011 | 2012 | 2013 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Min | Max | Mean | SD | Min | Max | Mean | SD | Min | Max | |
| Dependent Variables | ||||||||||||
| Operating ratio, mean | 1.18 | 0.26 | 0.00 | 3.96 | 1.21 | 0.29 | 0.00 | 5.41 | 1.22 | 0.30 | 0.00 | 5.76 |
| Overall rating, mean | 29.67 | 12.50 | 10.00 | 50.00 | 30.21 | 12.20 | 10.00 | 50.00 | 31.54 | 12.44 | 10.00 | 50.00 |
| Independent Variables | ||||||||||||
| Nursing home characteristics | ||||||||||||
| Percentage of Medicaid payer | 59.27 | 22.22 | 0 | 100 | 59.18 | 22.30 | 0 | 100 | 58.59 | 22.32 | 0 | 100 |
| Percentage of racial minorities | 18.25 | 20.52 | 0 | 100 | 18.42 | 20.39 | 0 | 100 | 17.16 | 19.89 | 0 | 100 |
| Neighborhood characteristics | ||||||||||||
| Percentage of population below poverty level | 14.61 | 8.86 | 0 | 100 | 15.12 | 8.98 | 0 | 100 | 15.50 | 9.09 | 0 | 100 |
| Percentage of black/ African American | 12.27 | 17.59 | 0 | 100 | 12.32 | 17.51 | 0 | 98.48 | 12.62 | 17.85 | 0 | 98.35 |
| Control Variables | ||||||||||||
| Nursing home characteristics | ||||||||||||
| Number of beds (hundreds) | 1.13 | 0.55 | 0.03 | 7.25 | 1.13 | 0.55 | 0.04 | 7.25 | 1.12 | 0.56 | 0.03 | 7.25 |
| Occupancy rates | 0.84 | 0.13 | 0.01 | 1.00 | 0.84 | 0.13 | 0.02 | 1.00 | 0.84 | 0.13 | 0.02 | 1.00 |
| Percentage of chain nursing homes | 61.58 | 48.64 | 0 | 100 | 61.15 | 48.74 | 0 | 100 | 62.90 | 48.31 | 0 | 100 |
| Herfindahl–Hirschman Index | 0.16 | 0.20 | 0.01 | 1.00 | 0.15 | 0.20 | 0.01 | 1.00 | 0.17 | 0.20 | 0.01 | 1.00 |
| Percentage of for‐profit nursing homes | 76.71 | 42.27 | 0 | 100 | 75.53 | 43.00 | 0 | 100 | 73.73 | 44.01 | 0 | 100 |
| Percentage of nonprofit nursing homes | 19.95 | 39.97 | 0 | 100 | 20.63 | 40.47 | 0 | 100 | 21.94 | 41.39 | 0 | 100 |
| Percentage of nursing homes owned by government | 2.90 | 16.79 | 0 | 100 | 3.36 | 18.02 | 0 | 100 | 3.99 | 19.57 | 0 | 100 |
| Case mix | 1.14 | 0.14 | 0.62 | 3.37 | 1.16 | 0.14 | 0.64 | 3.24 | 1.16 | 0.14 | 0.65 | 3.34 |
| Low cognitive function score | 0.31 | 0.11 | 0.00 | 1.00 | 0.33 | 0.12 | 0.00 | 1.00 | 0.35 | 0.12 | 0.00 | 1.00 |
| Neighborhood characteristics | ||||||||||||
| Population | 27,122 | 15,285 | 0 | 114,941 | 27,435 | 15,461 | 0 | 115,538 | 26,765 | 15,233 | 0 | 114,734 |
| N | 7, 009 | 7,028 | 5,870 | |||||||||
| 1.7 Number of nursing homes per zip code | ||||||||||||
All 5‐Digit ZIP Code Tabulation Areas within United States and Puerto Rico from American Community Survey (ACS).
Percentage of population below poverty level is measured in the past 12 months.
Table 2 shows the differences in operating ratios and quality ratings by nursing home and neighborhood characteristics. First, we examine the differences in operating ratios and overall nursing home quality rating by two nursing home characteristics (Medicaid dependency and predominantly minority). Medicaid‐dependent nursing homes have slightly lower operating ratios (0.07, p < .001) and overall rating (2.56, p < .001) than non‐Medicaid‐dependent nursing homes. Predominantly nonwhite nursing homes have a 4.59 lower nursing home quality (p < .001). The second panel presents the operating ratio and quality rating by neighborhood characteristics (poverty and racial minority concentration). The quality rating is 1.68 points lower in nursing homes located in poverty‐concentrated neighborhoods; and 2.48 points lower in nursing homes located in racial minority‐concentrated neighborhoods.
Table 2.
Bivariate Differences in Operating Ratios and Quality of Care, by Nursing Home and Neighborhood Characteristics
| Nursing Home Characteristics | ||||||
|---|---|---|---|---|---|---|
| Non‐Medicaid‐Dependent Nursing Homes | Medicaid‐Dependent Nursing Homes | p | Predominantly White Nursing Homes | Predominantly Racial Minority Nursing Homes | p | |
| Operating ratio | 1.21 | 1.14 | <.001 | 1.20 | 1.22 | .045 |
| Overall rating | 30.56 | 28.00 | <.001 | 31.00 | 26.41 | <.001 |
| Neighborhood Characteristics | ||||||
|---|---|---|---|---|---|---|
| Less Poverty‐Concentrated Neighborhoods | Poverty‐Concentrated Neighborhoods | p | Predominantly White Neighborhoods | Predominantly Racial Minority Neighborhoods | p | |
| Operating ratio | 1.21 | 1.19 | .003 | 1.20 | 1.19 | .034 |
| Overall rating | 30.80 | 29.12 | <.001 | 30.85 | 28.37 | <.001 |
Medicaid dependency represents that 85 percent or more of the residents are supported by Medicaid and less than 8 percent are supported by Medicare; and racial minority composition indicates that 40 percent or more of the residents are nonwhite. Poverty‐concentrated neighborhoods represent that population below poverty line is more than 20 percent in neighborhoods; and predominantly racial minority neighborhoods indicate that neighborhoods with that minority population is more than 20 percent.
To extend the analysis further to contextual factors by focusing on predominantly racial minority neighborhoods, Figure 1 shows maps of four largest MSAs by population to depict the spatial concentration of nursing homes. The blue H represents nursing homes in the top 20 percent of operating ratios; and the red L shows nursing homes in the bottom 20 percent of operating ratios. As observed in New York, nursing homes with sufficient financial resources (depicted as H) are mainly located in predominantly white neighborhoods. We observed the same geographical patterns in Los Angeles, Chicago, and Dallas.
Figure 1.
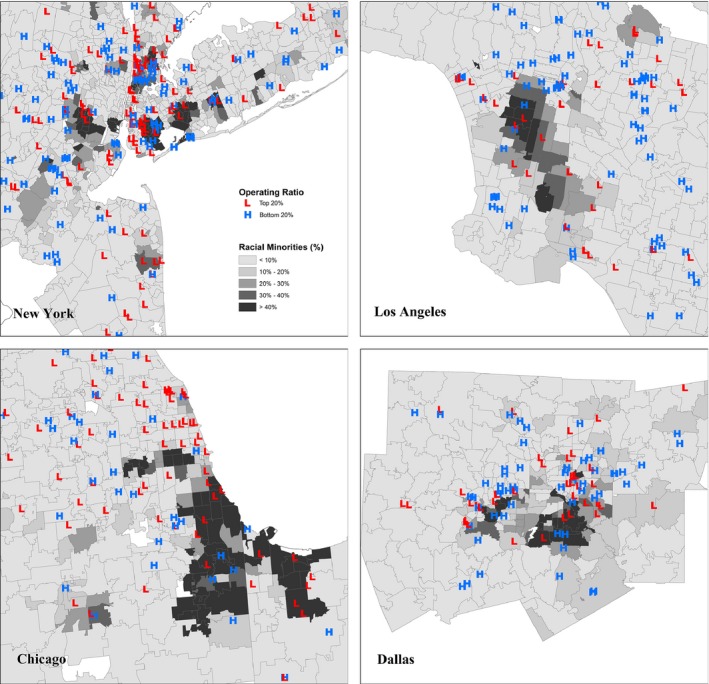
Spatial Concentration of Nursing Homes with High Operating Ratios against Racial Minority Communities in 2013 [Color figure can be viewed at http://www.wileyonlinelibrary.com/]
Table 3 shows the regression results that test the relationship between nursing homes’ fiscal stress and quality rating and their composition of nursing home residents (Medicaid dependency and racial minorities) and neighborhood context (proportion of residents who are low‐income or racial minorities in the surrounding zip code), controlling for nursing home characteristics, including number of beds, occupancy rates, and chain.
Table 3.
Association of Nursing Homes and Neighborhood Characteristics on Operating Ratios and Quality Ratings
| Dependent Variable | Operating Ratio | Quality Rating |
|---|---|---|
| Nursing Home Level | ||
| Medicaid (≥85%; and Medicare <8%) | −0.035*** | −0.671 |
| (0.010) | (0.404) | |
| Nonwhite (≥40%) | −0.012 | −2.641*** |
| (0.007) | (0.320) | |
| Neighborhood Level | ||
| Log poverty by zip code | 0.010 | −1.197*** |
| (0.006) | (0.265) | |
| Log black or African American by zip code | −0.008** | −0.373** |
| (0.003) | (0.128) | |
| Nursing Home Level | ||
| Number of beds | 0.060*** | −3.537*** |
| (0.005) | (0.193) | |
| Occupancy rates | 0.290*** | 10.089*** |
| (0.020) | (0.852) | |
| Chain | 0.045*** | −1.966*** |
| (0.005) | (0.201) | |
| HHI | −0.002 | 0.588 |
| (0.017) | (0.739) | |
| Nonprofit | −0.122*** | 5.470*** |
| (0.006) | (0.263) | |
| Government | −0.177*** | 2.196*** |
| (0.014) | (0.545) | |
| Case mix | 0.197*** | 2.695*** |
| (0.018) | (0.774) | |
| Low Cognitive Function Score | 0.131*** | 1.611* |
| (0.019) | (0.805) | |
| Neighborhood Level | ||
| Log population | 0.011* | 0.070 |
| (0.005) | (0.213) | |
| Constant | 0.372*** | 17.704*** |
| (0.105) | (4.635) | |
| State fixed | Yes | Yes |
| Year fixed | Yes | Yes |
| Observations | 14,886 | 15,792 |
| Number of zip codes | 3,717 | 3,815 |
| Variance: zip codes | 0.03 | 54.41 |
| Variance: nursing homes | 0.04 | 82.53 |
| Interclass correlation coefficient | 0.40 | 0.40 |
Theses hierarchical linear models use a varying intercept, multilevel. Ordered logit models yield similar findings (not shown).
Standard errors in parentheses.
***p < .001, **p < .01, *p < .05.
The first column in Table 3 shows that Medicaid‐dependent nursing homes have a 3.5 percentage point lower operating ratio (p < .001). Even after controlling for composition of nursing home residents, neighborhood context still matters: Nursing homes located in predominantly black or African American communities have higher fiscal stress. A 1 percent increase in the black or African American population is associated with 0.8 percentage point lower operating ratio (p < .01). Forty percent of the total variance in operating ratios is accounted for by differences between neighborhoods (based on the intraclass correlation coefficient). Additional models that include each main effect individually have consistent findings on the direction of effect (see Appendix SA4).
The second column in Table 3 shows the nursing homes with predominantly nonwhite residents have a 2.64 lower quality rating score (p < .001). In addition, even after controlling for nursing homes’ composition, nursing homes in the surrounding zip code with high proportion of low‐income or racial minority residents have lower overall quality ratings, respectively (1.20 and 0.37, p < .001). Forty percent of the total variance in operating ratios is accounted for by differences between neighborhoods (based on the intraclass correlation coefficient). Additional models that include each main effect individually have consistent findings on the direction of effect (see Appendix SA5).
Figure 2 presents the coefficients from a separate regression by year using the models in Table 3. For each year (X‐axis), Y‐axis shows the coefficients with 95% confidence interval from the estimations of the effect of neighborhoods characteristics on operating ratios and quality ratings. First, Figure 2(a) shows that there is no statistically significant relationship between poverty‐concentrated neighborhoods and operating ratios of nursing homes. Figure 2(b), on the other hand, shows that nursing homes located in minority‐concentrated neighborhoods are more likely to have lower operating ratios, although the relationship in 2011 is not statistically significant at the 95% confidence level. Figure 2(c) and (d) presents the changes in quality rating depending on neighborhood context. Although the effect of racial minority neighborhoods on nursing homes’ quality rating in 2013 is not statistically significant, we have consistent findings that the proportion of low‐income or racial minority residents in surrounding zip codes is negatively correlated with nursing homes’ quality ratings across years.
Figure 2.

Coefficients of Neighborhood Characteristics on Operating Ratio and Quality Rating by Year
Discussion
In this paper, we assessed the contributions of both compositional (i.e., nursing homes with high Medicaid and racial minority residents) and contextual factors (i.e., disadvantaged neighborhoods) on nursing homes’ fiscal stress and quality of care. Examining nursing homes’ fiscal stress and quality of care is important because nursing homes in disadvantaged neighborhoods are more likely to close, in turn worsening access to long‐term care via institutions in these communities. Using OLS and HLM with HCRIS, Nursing Home Five‐Star Quality Rating System, OSCAR/CASPER datasets, and ACS from 2011 to 2013, we found both compositional and contextual factors are related to nursing homes’ fiscal stress and quality of care. To assess the substantive effect, an “average” nursing home with mean values of all covariates in the dataset is used. The predicted values from the regression models indicate that increasing the composition of black or African American residents from 10 percent to 40 percent within a neighborhood is associated with a 0.01 decrease in the operating ratio. This translates into a $100,000 decrease in total patient revenue of an average nursing home, assuming that operating expenses remain the same. In addition, increasing the neighborhood's population living in poverty from 10 percent to 40 percent within a neighborhood leads to a 1.7 point predicted drop in nursing home quality rating for an average home. Furthermore, increasing the percentage of black neighborhood residents from 10 percent to 40 percent would lower the predicted quality rating for an average nursing home by 0.52.
First, we observed a compositional effect within nursing homes: Nursing homes where Medicaid residents predominantly reside are more likely to be under fiscal stress and provide lower quality care. The results are consistent with previous studies on “two‐tiered” systems of nursing homes (Mor et al. 2004; Smith et al. 2007). Although Medicare margins remain high relative to service costs (Medicare Payment Advisory Commission [MedPAC] 2012), profit margins for Medicaid and private payers are lower than Medicare (Harrington et al. 2013). This is because Medicaid reimbursement rates for nursing homes are traditionally lower than Medicare or private payers; therefore, nursing homes disproportionately serving Medicaid residents have lower revenue, which may lead to poor quality of care. This study provides empirical evidence that there is a positive relationship between Medicaid dependency and fiscal stress of nursing homes and suggests some plausible mechanisms for why Medicaid‐dependent nursing homes are more likely to provide lower quality of care.
Further, we explored the relationship between neighborhood contexts (poverty and racial minority‐concentrated neighborhoods) and nursing homes’ fiscal stress and quality of care, even after controlling for nursing homes’ compositional factors. Although there has been significant study of the plight of low‐income racial minorities within lower‐tier nursing homes (Mor et al. 2004; Smith et al. 2007; Chisholm et al. 2013), there has been limited systematic research on how underlying neighborhood contexts are exacerbating fiscal stress. For example, Chisholm et al. (2013) claimed that nursing homes’ financial performance is influenced by the racial composition of nursing home residents because minorities are disproportionately covered by Medicaid. As they claimed, nursing homes’ Medicaid dependency is negatively related to operating ratios. However, we further showed that racial minority concentration within neighborhoods matters more than racial composition of nursing home residents to explain nursing homes’ fiscal stress. We can potentially interpret the result as evidence that nursing homes with high operating ratios are less likely to provide services in predominantly racial minority communities, rather than a result of a correlation between Medicaid dependency and racial minority residents within nursing homes.
This study has several limitations. With our cross‐sectional design, we did not provide evidence for a causal relationship between compositional and contextual factors and nursing home fiscal stress and quality of care. Although we find two outcome variables, fiscal stress and quality of care, are related to compositional and contextual factors, further analysis is required to support inference. Second, we limited our dependent variable for financial performance to operating ratios, which only captures the ability to continue operations over the medium term. This may lead to a bias because different financial performance indicators measure slightly different dimensions of fiscal health (Stone et al. 2015). Third, the operating ratios are operationalized as operating revenues relative to operating costs, and thus are determined by both measures. This does not allow us to fully account for the underlying source of variation. However, we use this measure to be consistent with the public financial management literature. Fourth, we focused only on institutional long‐term care, while there has been a shift toward home or community‐based services. As neighborhood contexts may be more critical issue for noninstitutional long‐term care, it needs to be clarified further in future research.
More broadly, this study suggests that different policy designs may be needed to ensure the fiscal health of Medicaid‐dependent nursing homes located in racial minority neighborhoods in order to ensure that all elderly have adequate access to financially viable and high‐quality long‐term care institutions regardless of where they live. Formal racial discrimination and segregation within nursing homes were abolished after the civil rights movement (Smith et al. 2008). However, racial disparities in the access to financially sustainable long‐term care facilities persist (Smith et al. 2007; Virnig et al. 2009; Chisholm et al. 2013). The findings of this study aligned with the claims that “bias, prejudice, and stereotyping on the part of health care providers may contribute to differences in care (Smedley, Stith, and Nelson 2002)” at the institutional level. Although racial minorities may not be overtly barred from residing in certain nursing homes, institutional racism may remain through health care providers’ business decisions and individuals’ nursing home selection process based primarily on geographical proximity. Finally, the results from our study suggest that as the U.S. population ages, making nursing homes an increasingly critical source of health care, addressing disparities in access to high‐quality long‐term care will be an important dimension of promoting equity.
Supporting information
Appendix SA1: Author Matrix.
Appendix SA2: Correlation Coefficients among Overall Nursing Home Quality Ratings and Staff Characteristics.
Appendix SA3: Correlation Coefficients among Independent Variables.
Appendix SA4: Association of Nursing Homes and Neighborhood on Operating Ratios Using OLS (Model 1 and Model 2) and HLM Varying‐Intercept (Model 3 and Model 4).
Appendix SA5: Association of Nursing Homes and Neighborhood on Quality Ratings Using OLS (Model 1 and Model 2) and HLM Varying‐Intercept (Model 3 and Model 4).
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The authors thank Johannes Karreth for statistical advice and David Matkin, Kiwoong Park, and David Hoffman for comments on an early draft.
No financial support.
Disclosures: During the time of manuscript preparation, Young Joo Park was an employee of the University at Albany and New York State Department of Health. Erika Martin is an employee of the University at Albany and the Rockfeller Institute of Government of the State University of New York. The views in the manuscript are those of the authors and do not reflect these organizations.
Disclaimers: None.
References
- Bach, P. B. , Pham H. H., Schrag D., Tate R. C., and Hargraves J. L.. 2004. “Primary Care Physicians Who Treat Blacks and Whites.” New England Journal of Medicine 351 (6): 575–84. [DOI] [PubMed] [Google Scholar]
- Bowblis, J. R. 2011. “Staffing Ratios and Quality: An Analysis of Minimum Direct Care Staffing Requirements for Nursing Homes.” Health Services Research 46 (5): 1495–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bower, K. M. , Thorpe R. J., Rohde C., and Gaskin D. J.. 2014. “The Intersection of Neighborhood Racial Segregation, Poverty, and Urbanicity and Its Impact on Food Store Availability in the United States.” Preventive Medicine 58: 33–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown University Center for Gerontology and Healthcare Research and the National Institute on Aging . 2016. “The Shaping Long‐Term Care in America Project.”
- Castle, N. G. , Engberg J., Lave J., and Fisher A.. 2009. “Factors Associated with Increasing Nursing Home Closures.” Health Services Research 44 (3): 1088–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Medicare & Medicaid Services . 2015. “Cost Reports” [accessed on August 16, 2015]. Available at https://www.cms.gov/Research-Statistics-Data-and-Systems/Downloadable-Public-Use-Files/Cost-Reports/?redirect=/CostReports/
- Centers for Medicare and Medicaid Services . 2013. “Skilled Nursing Facility PPS.”
- Centers for Medicare and Medicaid Services . 2017a. “Cost Reports.”
- Centers for Medicare and Medicaid Services . 2017b. “Five‐Star Quality Rating System.”
- Chisholm, L. , Weech‐Maldonado R., Laberge A., Lin F.‐C., and Hyer K.. 2013. “Nursing Home Quality and Financial Performance: Does the Racial Composition of Residents Matter?” Health Services Research 48 (6 Pt 1): 2060–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colby, S. L. , and Ortman J. M.. 2015. “Projections of the Size and Composition of the US Population: 2014 to 2060.” U.S. Census Bureau, Ed: 25‐1143.
- Cubbin, C. , LeClere F. B., and Smith G. S.. 2000. “Socioeconomic Status and Injury Mortality: Individual and Neighbourhood Determinants.” Journal of Epidemiology and Community Health 54 (7): 517–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux, A. V. 2001. “Investigating Neighborhood and Area Effects on Health.” American Journal of Public Health 91 (11): 1783–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux, A. V. , and Mair C.. 2010. “Neighborhoods and Health.” Annals of the New York Academy of Sciences 1186 (1): 125–45. [DOI] [PubMed] [Google Scholar]
- Douglas, J. W. , and Gaddie R. K.. 2002. “State Rainy Day Funds and Fiscal Crises: Rainy Day Funds and the 1990–1991 Recession Revisited.” Public Budgeting and Finance 22 (1): 19–30. [Google Scholar]
- Duncan, C. , Jones K., and Moon G.. 1998. “Context, Composition and Heterogeneity: Using Multilevel Models in Health Research.” Social Science & Medicine 46 (1): 97–117. [DOI] [PubMed] [Google Scholar]
- Feng, Z. , Lepore M., Clark M. A., Tyler D., Smith D. B., Mor V., and Fennell M. L.. 2011. “Geographic Concentration and Correlates of Nursing Home Closures: 1999–2008.” Archives of Internal Medicine 171 (9): 806–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiscella, K. , and Williams D. R.. 2004. “Health Disparities Based on Socioeconomic Inequities: Implications for Urban Health Care.” Academic Medicine 79 (12): 1139–47. [DOI] [PubMed] [Google Scholar]
- Frakt, A. B. 2011. “How Much Do Hospitals Cost Shift? A Review of the Evidence.” The Milbank Quarterly 89 (1): 90–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harkey, J. , and Vraciu R.. 1992. “Quality of Health Care and Financial Performance: Is There a Link?” Health Care Management Review 17 (4): 55–63. [PubMed] [Google Scholar]
- Harrington, C. , Ross L., Mukamel D., and Rosenau P.. 2013. Improving the Financial Accountability of Nursing Facilities. Washington, DC: Kaiser Commission on Medicaid and the Uninsured. [Google Scholar]
- Henry J. Kaiser Family Foundation . 2013. “Improving the Financial Accountability of Nursing Facilities.”
- Kemper, P. , Komisar H. L., and Alecxih L.. 2005. “Long‐Term Care over an Uncertain Future: What Can Current Retirees Expect?” INQUIRY: The Journal of Health Care Organization, Provision, and Financing 42 (4): 335–50. [DOI] [PubMed] [Google Scholar]
- Larson, N. I. , Story M. T., and Nelson M. C.. 2009. “Neighborhood Environments: Disparities in Access to Healthy Foods in the US.” American Journal of Preventive Medicine 36 (1): 74–81. e10. [DOI] [PubMed] [Google Scholar]
- LeClere, F. B. , Rogers R. G., and Peters K.. 1998. “Neighborhood Social Context and Racial Differences in Women's Heart Disease Mortality.” Journal of Health and Social Behavior 39 (2): 91–107. [PubMed] [Google Scholar]
- Lee, J. G. , Henriksen L., Rose S. W., Moreland‐Russell S., and Ribisl K. M.. 2015. “A Systematic Review of Neighborhood Disparities in Point‐of‐Sale Tobacco Marketing.” American Journal of Public Health 105 (9): e8–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubitz, J. , Cai L., Kramarow E., and Lentzner H.. 2003. “Health, Life Expectancy, and Health Care Spending Among the Elderly.” New England Journal of Medicine 349 (11): 1048–55. [DOI] [PubMed] [Google Scholar]
- Macintyre, S. , Ellaway A., and Cummins S.. 2002. “Place Effects on Health: How Can We Conceptualise, Operationalise and Measure Them?” Social Science & Medicine 55 (1): 125–39. [DOI] [PubMed] [Google Scholar]
- Mair, C. F. , Roux A. V. D., and Galea S.. 2008. “Are Neighborhood Characteristics Associated with Depressive Symptoms? A Critical Review.” Journal of Epidemiology and Community Health 2007: 066605. [DOI] [PubMed] [Google Scholar]
- Matteson, D. W. , Burr J. A., and Marshall J. R.. 1998. “Infant Mortality: A Multi‐Level Analysis of Individual and Community Risk Factors.” Social Science & Medicine 47 (11): 1841–54. [DOI] [PubMed] [Google Scholar]
- Medicare Payment Advisory Commission (MedPAC) . 2012. “Skilled Nursing Facility Services: Assessing Payment Adequacy and Updating Payments.” 171–208.
- Mor, V. , Zinn J., Angelelli J., Teno J. M., and Miller S. C.. 2004. “Driven to Tiers: Socioeconomic and Racial Disparities in the Quality of Nursing Home Care.” Milbank Quarterly 82 (2): 227–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison, R. S. , Wallenstein S., Natale D. K., Senzel R. S., and Huang L.‐L.. 2000. ““We Don't Carry That”—Failure of Pharmacies in Predominantly Nonwhite Neighborhoods to Stock Opioid Analgesics.” New England Journal of Medicine 342 (14): 1023–6. [DOI] [PubMed] [Google Scholar]
- Office of Disease Prevention and Health Promotion . 2014. “Healthy People 2020” [accessed on July 15, 2016]. Available at https://www.healthypeople.gov/2020/topics-objectives/topic/Access-to-Health-Services
- Papas, M. A. , Alberg A. J., Ewing R., Helzlsouer K. J., Gary T. L., and Klassen A. C.. 2007. “The Built Environment and Obesity.” Epidemiologic Reviews 29 (1): 129–43. [DOI] [PubMed] [Google Scholar]
- Schneider, E. C. , Zaslavsky A. M., and Epstein A. M.. 2002. “Racial Disparities in the Quality of Care for Enrollees in Medicare Managed Care.” Journal of the American Medical Association 287 (10): 1288–94. [DOI] [PubMed] [Google Scholar]
- Schulz, A. J. , Williams D. R., Israel B. A., and Lempert L. B.. 2002. “Racial and Spatial Relations as Fundamental Determinants of Health in Detroit.” Milbank Quarterly 80 (4): 677–707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shugarman, L. R. , and Brown J. A.. 2006. “Nursing Home Selection: How Do Consumers Choose? Volume I: Findings from Focus Groups of Consumers and Information Intermediaries.” Nursing 10: 01. [Google Scholar]
- Smedley, B. , Stith A., and Nelson A.. 2002. Unequal Treatment: What Healthcare Providers Need to Know about Racial and Ethnic Disparities in Healthcare. Washington, DC: National Academy Press. [Google Scholar]
- Smith, D. B. , Feng Z., Fennell M. L., Zinn J. S., and Mor V.. 2007. “Separate and Unequal: Racial Segregation and Disparities in Quality across U.S. Nursing Homes.” Health Affairs 26 (5): 1448–58. [DOI] [PubMed] [Google Scholar]
- Smith, D. B. , Feng Z., Fennell M. L., Zinn J., and Mor V.. 2008. “Racial Disparities in Access to Long‐Term Care: The Illusive Pursuit of Equity.” Journal of Health Politics, Policy and Law 33 (5): 861–81. [DOI] [PubMed] [Google Scholar]
- Stone, S. B. , Singla A., Comeaux J., and Kirschner C.. 2015. “A Comparison of Financial Indicators: The Case of Detroit.” Public Budgeting & Finance 35 (4): 90–111. [Google Scholar]
- Truong, K. D. , and Ma S.. 2006. “A Systematic Review of Relations between Neighborhoods and Mental Health.” Journal of Mental Health Policy and Economics 9 (3): 137. [PubMed] [Google Scholar]
- U.S. Census Bureau . 2016a. “How the Census Bureau Measures Poverty.”
- U.S. Census Bureau . 2016b. “American Factfinder.”
- Virnig, B. A. , Baxter N. N., Habermann E. B., Feldman R. D., and Bradley C. J.. 2009. “A Matter of Race: Early‐Versus Late‐Stage Cancer Diagnosis.” Health Affairs 28 (1): 160–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, X. , Dennis L., and Tu Y. S. J.. 2007. “Measuring Financial Condition: A Study of US States.” Public Budgeting & Finance 27 (2): 1–21. [Google Scholar]
- Weech‐Maldonado, R. , Laberge A., Pradhan R., Johnson C. E., and Hyer K.. 2012. “Nursing Home Financial Performance: The Role of Ownership and Chain Affiliation.” Health Care Management Review 37: 235–45. [DOI] [PubMed] [Google Scholar]
- White, K. , Haas J. S., and Williams D. R.. 2012. “Elucidating the Role of Place in Health Care Disparities: The Example of Racial/Ethnic Residential Segregation.” Health Services Research 47 (3pt2): 1278–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zinn, J. , Mor V., Feng Z., and Intrator O.. 2009. “Determinants of Performance Failure in the Nursing Home Industry.” Social Science & Medicine (1982) 68 (5): 933–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Appendix SA2: Correlation Coefficients among Overall Nursing Home Quality Ratings and Staff Characteristics.
Appendix SA3: Correlation Coefficients among Independent Variables.
Appendix SA4: Association of Nursing Homes and Neighborhood on Operating Ratios Using OLS (Model 1 and Model 2) and HLM Varying‐Intercept (Model 3 and Model 4).
Appendix SA5: Association of Nursing Homes and Neighborhood on Quality Ratings Using OLS (Model 1 and Model 2) and HLM Varying‐Intercept (Model 3 and Model 4).


