Abstract
Objectives
To examine the effects of Medicare's revised ambulatory surgery center (ASC) payment schedule on overall payments for outpatient surgery.
Data Sources
Twenty percent sample of national Medicare beneficiaries.
Study Design
We conducted a pre–post study of Medicare beneficiaries who underwent outpatient surgery in a hospital outpatient department (HOPD), ASC, or physician office between 2004 and 2011. Specifically, we used multivariable regression to compare temporal trends in outpatient surgery before and after implementation of Medicare's revised payment schedule in 2008, which reduced ASC facility payments to roughly two‐thirds that of HOPDs. Our outcome measures included overall Medicare payments, utilization rates, per beneficiary spending, and average episode payments for outpatient surgery.
Principal Findings
Between the last quarters of 2007 and 2008, overall Medicare payments for outpatient surgery grew by $334 million—an amount nearly three times higher than would have been expected without the policy change (p < .001 for the difference). While utilization rates of outpatient surgery were attenuated, per beneficiary spending and average surgical episode payments increased by 10.4 percent and 7.8 percent, respectively, over the same period. By the end of 2011, Medicare payments for outpatient surgery reached $5.1 billion. Without the policy change, they would have totaled only $4.1 billion.
Conclusions
Despite lessening demand, reduced ASC facility payments did not curb spending for outpatient surgery. In fact, overall payments actually increased following the policy change, driven by higher average episode payments.
Keywords: Outpatient surgery, ambulatory surgery center, Medicare spending
This year alone, Medicare beneficiaries will undergo 17 million outpatient surgical procedures (Cullen, Hall, and Golosinskiy 2009). Payments for related services account for 11 percent of per capita spending and are rising at a rate of 5.5 percent annually (Health Care Cost Institute 2014; Medicare Payment Advisory Commission 2015), making outpatient surgery one of the largest and fastest‐growing health care sectors for the Medicare Program. Much of this growth is due to the rising popularity of ambulatory surgery centers (ASCs), visits to which have increased 300 percent over the last decade (Cullen, Hall, and Golosinskiy 2009). These freestanding facilities—many owned by the surgeons who staff them (Choudhry, Choudhry, and Brennan 2005)—have incentives that spur utilization (Hollingsworth et al. 2010, 2011). Thus, efforts to curb spending for outpatient surgery should include a focus on ASCs.
Recognizing this, the Centers for Medicare and Medicaid Services (CMS) revised its ASC payment schedule in accordance with the Medicare Prescription Drug, Improvement, and Modernization Act of 2003 (Centers for Medicare and Medicaid Services 2007). Using the outpatient prospective payment system (PPS) relative payment weights as a guide, CMS reduced ASC facility payments to roughly two‐thirds that of hospital outpatient departments (HOPDs) for the same services (Medicare Learning Network 2014). Paying ASCs less than HOPDs for the same services, combined with the movement of more outpatient surgical procedures away from hospitals (Hollingsworth et al. 2012a), has the potential to reduce overall spending for outpatient surgery.
However, it remains unclear whether the intended effects of this policy change were realized. In this context, we conducted a pre–post study using a 20 percent sample of national Medicare data. Specifically, we evaluated trends in overall Medicare payments, utilization, per beneficiary spending, and episode payments for outpatient surgery following CMS's implementation of its revised ASC payment schedule in January 2008. Our study will be of immediate interest to decision makers at CMS, as findings from it will provide actionable insights moving forward for the redesign of policies to reduce payments for outpatient surgery and curtail growth in surgery spending more broadly.
Methods
Data Source and Study Population
Our study was based on Research Identifiable File (RIF) data from a 20 percent sample of national Medicare beneficiaries. Produced by CMS, these files contain a nationally representative random sample of Medicare beneficiaries with claims submitted on their behalf over an 8‐year interval between January 1, 2004, and December 31, 2011. We limited our study to beneficiaries age 66 and older with continuous enrollment in Medicare parts A and B 6 months prior to their index surgical encounter. We excluded Medicare Advantage beneficiaries because the services provided to them are captured inconsistently in their claims.
Identifying and Characterizing Beneficiaries Who Underwent Outpatient Surgery
We applied relevant Health Care Procedure Coding System codes to identify beneficiaries with encounters for surgery on the integumentary (10,040–19,499), musculoskeletal (20,005–29,999), respiratory (30,000–32,999), cardiovascular (33,010–39,599, 92,950–92,998, 93,451–93,662), digestive (40,490–49,999), urinary (50,010–53,899), male (54,000–55,980) and female genital (56,405–59,899), endocrine (60,000–60,699), nervous (61,000–64,999), ocular (65,091–68,899), or auditory system (69,000–69,990).
Given our interest in outpatient surgery, we then used appropriate place of service codes embedded within claims from the Carrier and Outpatient RIFs to distinguish procedures performed in a physician's office (11), HOPD (22), or ASC (24). Further, we limited our analysis to beneficiaries who were treated by procedural‐based specialists through line Medicare specialty codes for general surgery (02, 28, 91), otolaryngology (04), cardiothoracic surgery (33, 78), obstetrics and gynecology (09), neurosurgery (14), ophthalmology (16), orthopedic surgery (20, 40), plastic and reconstructive surgery (24, 85), urology (34), and vascular surgery (76, 77).
We determined each beneficiary's age at the time of surgery, gender, race, and level of comorbid illness [using an adaption of the Charlson index (Klabunde et al. 2000)]. For analytic purposes, we then assigned all beneficiaries to health care markets, as defined by the Dartmouth Atlas's hospital referral region (HRR) boundaries (Dartmouth Atlas of Health Care 2016). With county‐level data from the American Community Survey and Area Health Resource Files (United Status Census Bureau 2015; Health Resources and Services Administration 2016), we characterized these HRRs according to the percentage of their residents living below the federal poverty limit, the percentage of their residents achieving a bachelor's degree, their residents’ average annual income, and the number of allopathic physicians serving them (per 10,000 population).
Primary and Secondary Outcomes
Our primary outcome was overall Medicare payments for outpatient surgery. To calculate this outcome, we selected a time frame around the service date wide enough to capture all expenditures plausibly related to surgery. Because postoperative complications and unplanned admissions are uncommon following outpatient surgery (Hollingsworth et al. 2012b), we used a 24‐hour claims window to define an outpatient surgical episode and extracted all payments from the Carrier and Outpatient RIFs that fell within the window. For each HRR, we then summed up these payments by quarter.
In addition, we had three secondary outcomes. To understand how overall payments related to use, we calculated overall utilization rates for outpatient surgery, where the numerator was a count of the number of outpatient procedures performed in a physician's office, HOPD, or ASC for a given HRR‐quarter, and the denominator was the number of beneficiaries residing in the HRR. To determine whether changes in overall payments were driven by changes in the population at risk, we calculated per beneficiary spending, aggregating episode payments across procedures for each HRR‐quarter and dividing by the number of beneficiaries residing in the HRR at that time. Finally, to examine the association between overall payments for outpatient surgery and spending during the surgical encounter, we measured average episode payments for each HRR‐quarter.
Statistical Analysis
With the HRR‐quarter serving as our unit of analysis, we then fitted separate regression models to assess the impact that CMS's revised ASC payment schedule had on overall payments, overall utilization rates, per beneficiary spending, and average episode payments for outpatient surgery. We modeled overall payments, per beneficiary spending, and average episode payments using ordinary least squares regression (Greene 2003). Given the non‐normal distributions of per beneficiary spending and average episode payments, we log transformed these variables (Manning and Mullahy 2001). We modeled overall utilization rates using Poisson regression (Greene 2003).
Our model specification had to satisfy three objectives. First, it must allow us to estimate the counterfactual trend in our outcomes after January 1, 2008 (i.e., if CMS's policy change had not occurred). Second, our specification had to accommodate the possibility of drift in the policy's effects over time. Third, it had to be exempt from multicollinearity issues, while maintaining a high degree of flexibility in modeling both baseline time trends and potential policy impact drift. To achieve these objectives, we used polynomial transformation of time trends in modeling the counterfactual trends and policy effects (Long and Ryoo 2010). Further, we improved our models’ stability through basis‐spline transformation as appropriate (Eilers and Marx 1996).
All models included the time, in quarters, since implementation of the revised payment policy. This was set to 0 during the last quarter of 2007, −1 for the third quarter of 2007, +1 for the first quarter of 2008, and so on. We adjusted for the sociodemographic and case mix variables (aggregated to the HRR‐level) described above. We also controlled for the availability of freestanding ASCs in each HRR.
We performed our analyses using the statistical software package R. All tests were two‐tailed, and we set the probability of Type 1 error at 0.05. Our Institutional Review Board deemed that this study using de‐identified data was exempt from its oversight.
Results
Table 1 displays characteristics of our study population at three time points. In this nationally representative sample, there were 6,565,430 outpatient surgical episodes in 2005, 6,889,023 episodes in 2008 (coinciding with CMS's launch of its revised ASC payment schedule), and 7,341,625 episodes in 2011. Sociodemographic characteristics and comorbid conditions were relatively consistent across study years. The 10 most common outpatient surgical procedures are displayed in Table S1.
Table 1.
Descriptive Statistics for Our Study Population
| Characteristic | Calendar Year | ||
|---|---|---|---|
| 2005 | 2008 | 2011 | |
| No. of eligible beneficiaries in the 20% sample | 5,016,615 | 4,733,462 | 4,850,533 |
| No. of outpatient surgical episodes | 6,565,430 | 6,889,023 | 7,341,625 |
| Average age at the time of surgery, in years (SD) | 70.6 (1.2) | 70.4 (1.2) | 70.2 (1.2) |
| % of patients undergoing surgery who were male (SE) | 44.5 (1.6) | 45.0 (1.5) | 45.5 (1.4) |
| % of patients undergoing surgery who were white (SE) | 86.9 (11.1) | 86.4 (11.3) | 85.6 (11.4) |
| Average Charlson score at the time of surgery (SD) | 2.5 (0.3) | 2.5 (0.3) | 2.5 (0.3) |
| Average per capita income, in 1,000 USD (SD) | 31.2 (6.1) | 36.7 (7.1) | 38.3 (6.8) |
| % of population living below federal poverty limit (SE) | 14.1 (4.4) | 14.0 (3.8) | 16.6 (4.0) |
| % of population with bachelor's degree (SE) | 27.2 (4.7) | 24.6 (6.2) | 25.2 (6.3) |
| No. of active MDs, per 10,000 population (SD) | 20.7 (7.7) | 21.7 (8.4) | 21.2 (8.3) |
No., number; SD, standard deviation; SE, standard error.
The distribution of outpatient surgery by place of service was relatively stable over the study interval (Figure 1). The percentage of outpatient surgical encounters to ASCs and physician offices increased slightly from 6.7 percent and 73.6 percent in 2004 to 7.7 percent and 74.7 percent in 2011, respectively. This was accompanied by a small decrease in the percentage of encounters to HOPDs, from 19.7 percent to 17.6 percent over the same time period.
Figure 1.
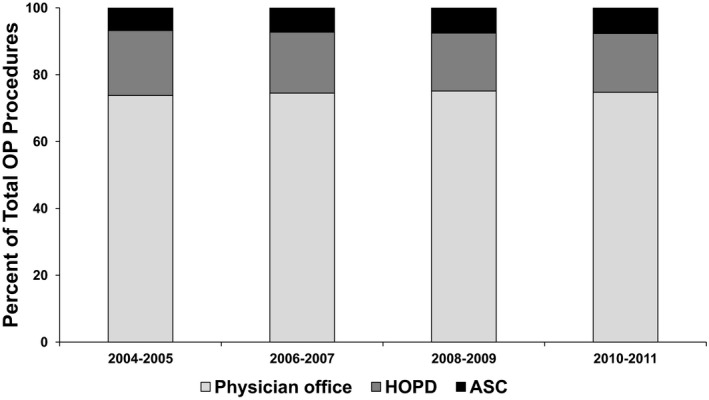
- Note. ASC, ambulatory surgery center; HOPD, hospital outpatient department; OP, outpatient.
Figure 2 shows that the rate of rise in overall Medicare payments for outpatient surgery was not blunted by implementation of CMS's revised ASC payment schedule. Between the last quarters of 2007 and 2008, overall Medicare payments for outpatient surgery grew by $334 million. This amount was nearly three times higher than would have been expected if CMS maintained its old ASC payment schedule (p < .001 for the difference). This spending growth occurred despite the fact that overall use of outpatient surgery was attenuated by the policy change (utilization rates rose 6.9 percent following the policy change but would have been expected to increase by 29.1 percent absent the change; p = .004). Further, this spending growth was not due to a shift in the delivery of care from costly inpatient stays to cheaper ambulatory settings, as payments for inpatient surgery increased in concert with outpatient surgical spending from $17.1 to $19.5 billion over the study interval.
Figure 2.
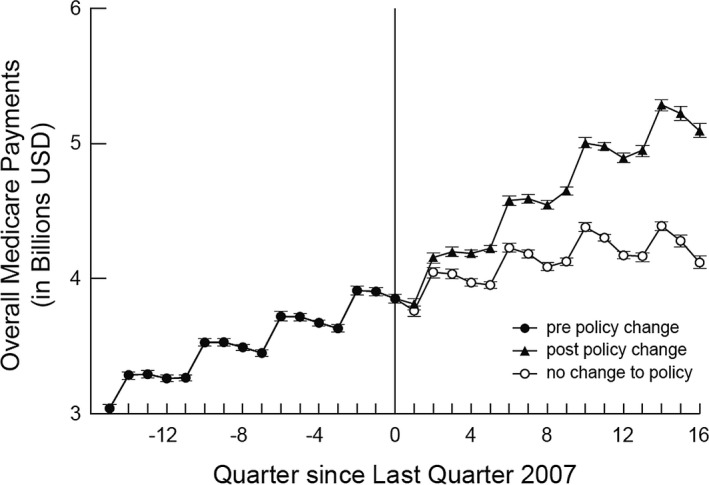
- Note. USD, United States dollars.
Figure 3 suggests that rising overall Medicare payments for outpatient surgery were due to higher per beneficiary spending (A) and, more specifically, higher average episode payments (B), which rose 10.4 percent and 7.8 percent, respectively, between the last quarters of 2007 and 2008. Both increases were higher than would have been expected if CMS maintained its old ASC payment schedule (p < .001 for the differences). Driven by these increases, Medicare payments for outpatient surgery reached $5.1 billion in the last quarter of 2011. In the absence of the policy change, outpatient surgery spending in this quarter would have been only $4.1 billion.
Figure 3.
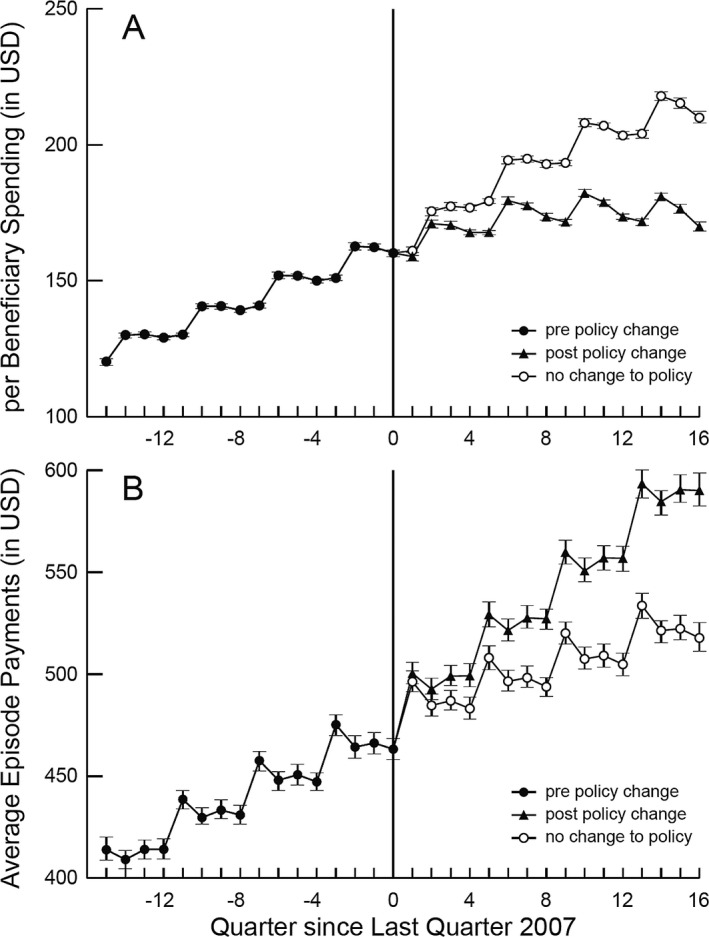
- Note. USD, United States dollars.
To explore unbundling or upcoding as possible explanations for our findings, we examined temporal trends in coding intensity for outpatient surgical episodes, observing an increase over time in the mean number of line items per episode. When we collapsed these data into the pre‐ and postpolicy periods (Table S2), we noted a significant increase in the mean number of line items per episode following implementation of the new ASC payment schedule (p < .001).
Comment
In our study, we examined the impact that CMS's revised ASC payment schedule had on Medicare spending for outpatient surgery. Despite reduced ASC facility payments, we found that spending actually grew at a faster rate than would have been anticipated in the absence of the policy change. This growth was not due to more outpatient surgical encounters among Medicare beneficiaries or changes in the population at risk, but rather it was driven by dramatic increases in episode payments. Collectively, our findings suggest that decision makers at CMS may need to consider additional strategies to rein in spending for outpatient surgery.
Given that ASCs are no longer paid on par with HOPDs, our findings are somewhat surprising. One plausible explanation relates to an expansion in the number of ASC‐covered procedures. Historically, CMS used a complex set of criteria to determine which procedures were eligible for payment when performed in an ASC. However, under the revised payment policy, facility payment to an ASC is allowed for nearly all procedures. Insofar as previously uncovered procedures were already being performed in ASCs, overall payments would rise even if there was no change in outpatient surgery trends.
Our findings may also be explained by a higher intensity of care delivery. CMS allows ASC payment for multiple procedures. Although subject to a multiple‐procedure discount (i.e., Medicare pays 100 percent of the highest paying procedure on a claim, plus 50 percent of the payment rate for the other covered procedures), an increase in the average number of procedures performed during the same encounter could contribute to outpatient spending growth. So, too, could the unbundling of procedure billing codes into component procedures. This practice was observed during CMS's rollout of its inpatient PPS (Gay and Kronenfeld 1990). Our exploratory analysis, which revealed a significant increase in the mean number of line items per episode following implementation of the new payment schedule, supports this possibility.
Several limitations of our study merit further discussion. To begin, revisions to CMS's ASC payment schedule were implemented simultaneously nationally. Thus, we could not observe the counterfactual trends. Due to this limitation, we estimated the policy change's effect based on the following three assumptions. First, for a given outcome, its counterfactual measurements (i.e., those without the policy change) during the postimplementation period and its preimplementation observations formed a curvilinear trend line. Second, bending of the curvilinear trend line at 2008 was due to the impact of the policy change. Third, the curvilinear trend line could be perturbed by market changes and seasonality factors.
In addition, we interpreted the observed trends in our outcomes as being due to the policy change. While we adopted highly flexible splines to capture the curvilinear trends, we must acknowledge that unmeasured variation may have occurred during 2008 that could add noise into our results. That being said, CMS's revised ASC payment schedule was a system‐wide policy change that occurred across the 2008 timeline. As such, we would argue that our analysis correctly captures the impact of the policy change to the first degree of approximation. Finally, although increasing average episode payments appear to underlie the growth in overall payments for outpatient surgery, the determinants of episode costs remain unclear.
Limitations notwithstanding, our study has important implications for ongoing payment and delivery system reforms. To reduce outpatient surgery spending, decision makers at CMS might consider extending inpatient episode‐based bundling programs such as the Bundled Payments for Care Improvement Initiative and the Comprehensive Care for Joint Replacement model to outpatient surgical procedures (Centers for Medicare and Medicaid Services 2016). For example, rather than paying providers (e.g., facilities, physicians, nonphysician clinicians) for each individual service that they provide, providers would accept a lump sum payment based on the clinical condition being treated for the entire outpatient episode. Providers would then divide the payment among themselves, thereby limiting their incentive to do more.
Alternatively, decision makers could try to affect upstream clinical decision making. One way of doing this would be to bring surgical providers into the fold of accountable care organization (ACO) formation (Dupree et al. 2014). If ACO participants reduce their expenditures below benchmarks, they are rewarded with a portion of the savings. To the extent that participating surgeons are motivated by such shared savings or feel pressure from referring primary care physicians to lower their treatment costs, they may selectively limit their use of discretionary procedures, lowering overall Medicare spending for outpatient surgery.
In summary, our findings suggest that CMS's revised ASC payment schedule did not accomplish the intended effect of reducing overall payments for outpatient surgery. While the policy change did curb overall utilization rates, average episode payments increased. Moving forward, research in this area should focus on examining the root of this unintended consequence by unpacking outpatient surgical episodes. Moreover, CMS may want to consider alternative payment models for outpatient surgery that reward surgeons who perform high‐value, low‐cost outpatient surgical care.
Supporting information
Appendix SA1: Author Matrix.
Table S1. Ten Most Common Outpatient Surgical Procedures among Medicare Fee‐for‐Service Beneficiaries.
Table S2. Trends in Coding Intensity for Outpatient Surgical Episodes.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: Research grants from the Agency for Healthcare Research and Quality (1R01HS024525 01A1 and 1R01HS024728 01 to JMH) and the National Institutes on Aging (R01AG048071 to BKH) provided financial support for the project.
Disclaimer: None.
Disclosures: None.
References
- Centers for Medicare and Medicaid Services . 2016. “Bundled Payments for Care Improvement Initiative.” CMS.gov website [accessed on October 16, 2016]. Available at http://innovation.cms.gov/initiatives/bundled-payments/
- Centers for Medicare and Medicaid Services HHS . 2007. “Medicare Program: Revised Payment System Policies for Services Furnished in Ambulatory Surgical Centers (ASCs) beginning in CY 2008. Final Rule.” Federal Register 72: 42469–626. [PubMed] [Google Scholar]
- Choudhry, S. , Choudhry N. K., and Brennan T. A.. 2005. “Specialty versus Community Hospitals: What Role for the Law?” Health Affairs 24 (Suppl Web Exclusives):W5‐361‐72. [DOI] [PubMed] [Google Scholar]
- Cullen, K. A. , Hall M. J., and Golosinskiy A.. 2009. “Ambulatory Surgery in the United States, 2006.” National Health Statistics Reports 11: 1–25. [PubMed] [Google Scholar]
- Darmouth Atlas of Health Care . Geographic Crosswalks and Boundary Files . 2016. “Dartmouth Atlas of Health Care Web Site” [accessed on October 16, 2016]. Available at http://www.dartmouthatlas.org/tools/downloads.aspx?tab=39
- Dupree, J. M. , Patel K., Singer S. J., West M., Wang R., Zinner M. J., and Weissman J. S.. 2014. “Attention to Surgeons and Surgical Care Is Largely Missing From Early Medicare Accountable Care Organizations.” Health Affairs 33: 972–9. [DOI] [PubMed] [Google Scholar]
- Eilers, P. H. C. , and Marx B. D.. 1996. “Flexible Smoothing with B‐Splines and Penalties.” Statistical Science 11: 89–102. [Google Scholar]
- Gay, E. G. , and Kronenfeld J. J.. 1990. “Regulation, Retrenchment—the DRG Experience: Problems from Changing Reimbursement Practice.” Social Science & Medicine 31: 1103–18. [DOI] [PubMed] [Google Scholar]
- Greene, W. H. Econometric Analysis. 5th edition Lebanon, IN: Prentice‐Hall; 2003. [Google Scholar]
- Health Care Cost Institute . 2014. “Health Care Cost and Utilization Report.” October 2013 [accessed on August 6, 2015]. Available at http://www.healthcostinstitute.org/files/2013%20HCCUR%2012-17-14.pdf
- Health Resources and Services Administration . Area Health Resources Files . 2016. “Health Resources and Services Administration website” [accessed on October 16, 2016]. Available at http://ahrf.hrsa.gov/
- Hollingsworth, J. M. , Ye Z., Strope S. A., Krein S. L., Hollenbeck A. T., and Hollenbeck B. K.. 2010. “Physician‐Ownership of Ambulatory Surgery Centers Linked to Higher Volume of Surgeries.” Health Affairs 29: 683–9. [DOI] [PubMed] [Google Scholar]
- Hollingsworth, J. M. , Krein S. L., Ye Z. J., Kim H. M., and Hollenbeck B. K.. 2011. “Opening of Ambulatory Surgery Centers and Procedure Use in Elderly Patients Data from Florida.” Archives of Surgery 146: 187–93. [DOI] [PubMed] [Google Scholar]
- Hollingsworth, J. M. , Saigal C. S., Lai J. C., Dunn R. L., Strope S. A., and Hollenbeck B. K.. 2012a. “Urologic Diseases in America Project. Surgical Quality among Medicare Beneficiaries Undergoing Outpatient Urological Surgery.” Journal of Urology 188: 1274–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingsworth, J. M. . Saigal C. S., Lai J. C., Dunn R. L., Strope S. A., and Hollenbeck B. K.. 2012b. “Urologic Diseases in America Project. Medicare Payments for Outpatient Urological Surgery by Location of Care.”Jounral of Urology 188: 2323–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klabunde, C. N. , Potosky A. L., Legler J. M., and Warren J. L.. 2000. “Development of a Comorbidity Index Using Physician Claims Data.” Journal of Clinical Epidemiology 53: 1258–67. [DOI] [PubMed] [Google Scholar]
- Long, J. , and Ryoo J.. 2010. “Using Fractional Polynomials to Model Non‐Linear Trends in Longitudinal Data.” British Journal of Mathematical and Statistical Psychology 63: 177–203. [DOI] [PubMed] [Google Scholar]
- Manning, W. G. , and Mullahy J.. 2001. “Estimating Log Models: To Transform or Not to Transform?” Journal of Health Economics 20: 461–94. [DOI] [PubMed] [Google Scholar]
- Medicare Learning Network . 2014. “Payment System Fact Sheet Series: Ambulatory Surgical Center Fee Schedule” CMS.gov website [accessed on August 6, 2015]. Available at https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/AmbSurgCtrFeepymtfctsht508-09.pdf
- Medicare Payment Advisory Commission . 2015. “Report to the Congress: Medicare Payment Policy. Chapter 5: Ambulatory Surgical Center Services” MedPAC website [accessed on August 6, 2015]. Available at http://www.medpac.gov/documents/reports/chapter-5-ambulatory-surgical-center-services-(march-2015-report).pdf?sfvrsn=0
- United Status Census Bureau . American Community Survey . 2015. “Census.gov website” [accessed on October 16, 2016]. Available at https://www.census.gov/programs-surveys/acs/data.html
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Table S1. Ten Most Common Outpatient Surgical Procedures among Medicare Fee‐for‐Service Beneficiaries.
Table S2. Trends in Coding Intensity for Outpatient Surgical Episodes.


