Abstract
Oral contraceptives (OCs) are often prescribed to adolescents and young adults for the treatment of health problems and to avoid unwanted pregnancies. We hypothesized that the use of OCs, among adolescents and young adults, is associated with a greater likelihood of pregnancy, abortion, sexually transmitted diseases (STDs), pelvic inflammatory disease (PID), and sexual behaviors that will enhance those problems (i.e., earlier sexual debut and more sexual partners) than adolescents and young adults not using OCs. To test this hypothesis, data from 1,365 adolescents and young adults in the 2011–2013 National Survey of Family Growth (NSFG) were used to describe the influence of ever use of OCs on ever having sex, sexual debut, multiple sexual partners, STDs, PID, pregnancy, and abortion. A secondary purpose was to evaluate protective factors from unhealthy sexual practices like religiosity, church attendance, and intact families. We found that the “ever use” of OCs by US adolescents and young adults results in a greater likelihood of ever having sex, STDs, PID, pregnancy, and abortion compared with those adolescents and young adults who never used OCs. Furthermore, those adolescents who ever used OCs had significantly more male sexual partners than those who never used OCs, and they also had an earlier sexual debut by almost two years. Conversely, we found that frequent church attendance, identification of the importance of religion, and having an intact family among adolescents were associated with less likelihood of unsafe sexual practices. We concluded that the use of OCs by adolescents and young adults might be considered a health risk. Further research is recommended to confirm these associations.
Summary: The purpose of this article was to show the correlation between contraceptive use in adolescents and negative sexual outcomes. We used data from the 2011–2013 NSFG and demonstrated that never married adolescents who used oral hormonal contraception were three times more likely to have an STD, have PID, and to become pregnant, and, surprisingly, ten times more likely of having an abortion compared to noncontracepting adolescents. These are outcomes that contraception is intended to prevent. These data also showed that the contraceptors had significantly more male partners than their contraceptive counterparts. Protective factors such as church attendance and family cohesiveness were associated with a decreased likelihood of sexual activity.
Keywords: contraception, adolescents, young adults, sexually transmitted diseases, abortion, pregnancy, sexual debut, pelvic inflammatory disease, church attendance, intact family, importance of religion
There has been a significant decrease in adolescent birth rates in recent years, from seventy pregnancies per 1,000 adolescent women in 2007 to fifty-two pregnancies per 1,000 in 2011 (Lindberg, Santelli, and Desai 2016). Researchers interested in determining factors responsible for this decline discovered that there was a significant increase in the use of contraceptive methods among adolescents but did not find a significant decline in sexual activity (Lindberg, Santelli, and Desai 2016). Although there was a significant increase in use of contraceptives and a decrease in pregnancies among adolescents, there were other health outcomes of interest and concern for healthcare providers other than pregnancy.
Sexually transmitted diseases (STDs) and behavioral risk factors for STDs, such as early initiation of sexual activity (i.e., sexual debut), and multiple sexual partners must also be taken into consideration for adolescent sexual health. According to the Centers for Disease Control, there was an increase in STDs from 2012 to 2013 in all four reported categories among young people aged fifteen to twenty-four, that is, a 2.8 percent increase in chlamydia, a 5.1 percent increase in gonorrhea, and a 15.1 percent increase in primary and secondary syphilis (CDC and NCH 2015). There was also a 27.5 percent increase in congenital syphilis among live births. Other Centers for Disease Control and Prevention (CDC) researchers have found that one in four female adolescents have an STD (Forhan et al., 2009). Besides being an increased risk for STDs, early sexual debut is also associated with poor family structure and other risk behaviors such as drug use and sexual abuse (Kastbom et al., 2015; Lara and Abdo 2016). Furthermore, many adolescents and young people who are sexually active are at risk of contracting STDs that may impair their future fertility and ability to have children (Tydén, Bjorkelund, and Olsson 1991; Fontes and Roach 2007; Bunting and Boivin 2010; Larsson and Tydén 2006; Tydén et al., 1996; Tydén, Olsson, and Haggstrom Nordin 2001; Tydén, Palmqvist, and Larsson 2012).
Healthcare providers often treat health problems such as acne, dysmenorrhea, migraine headaches, irregular menstrual cycles, unusual uterine bleeding, and polycystic ovarian syndrome with oral hormonal contraceptives with the view of also preventing unintended pregnancies in their adolescent and young adult patients (Rosenfield 2015; Youngster, Laufer, and Divasta 2013). Although health professionals believe that they are providing good health care in preventing unintended pregnancy and alleviating health problems by prescribing oral contraceptives (OCs), the standard practice of prescribing OCs may not be the best approach. From a health standpoint, the use of OCs to treat health problems might actually mask the causes of the problem and make some problems worse. For example, the use of OCs to treat menstrual pain might delay the diagnosis of treatable endometriosis and results in deep infiltrating endometriosis in later years (Chapron et al., 2010; Chapron et al., 2011; F. F. Tu et al., 2014). Use of OCs instead of lifestyle and/or medications to manage polycystic ovarian syndrome might make lipid levels worse (Cheang et al., 2011). Continuous use of OCs among adolescents and young adults also increases the risk of breast cancer (Bhupathiraju et al., 2016; Hemminki et al., 2002; Lanfranchi 2013).
The menstrual cycle is considered a vital sign for health especially among adolescents and young adults (American Academy of Pediatrics and American College of Obstetricians and Gynecologists 2006; Frank-Herrmann et al., 2005; Vigil et al., 2006). Since OCs suppress ovulation, an important vital sign for women’s health is masked. The menstrual cycle can provide early signs that indicate health problems. Anovulation, long cycle lengths, and unusual bleeding are just some examples (Heitmann et al., 2014; Morrison et al., 2011). In addition, the use of OCs for noncontraceptive purposes may lower the barrier to earlier sexual debut and multiple sexual partners. Fear of pregnancy, not wanting to develop STDs, and religious morals are frequent reasons why adolescents and young adults delay sexual intercourse (Fehring et al., 1998). However, fear of pregnancy and acquiring an STD are also reasons why adolescents and young adults use OCs and condoms. Furthermore, teaching so-called safe sex with the use of condoms could promote the notion that STDs can be entirely prevented by the use of a barrier. In reality, the condom barrier provides little protection from skin-to-skin and skin-to-sore diseases, including human papillomavirus, herpes simplex virus, syphilis, and chancroid (Genuis 2004).
There are, however, protective factors that help adolescent and young adult women to remain virgins and to reduce sexual partners. Past research has shown that those adolescents and young women who hold religion to be very important in their lives and identify as going to church at least once a week have an older age of sexual debut, less sexual intercourse, and fewer male sexual partners than those who are less religious (Edwards et al., 2008; Haglund and Fehring 2010; Haglund et al., 2011). Having intact families, good communication with parents, going to private school, and simply pledging being a virgin until marriage are also factors that lead to less sexual risk among adolescents and young adult women (Resnick et al., 1997). There is also some evidence that abstinence-only interventions reduce sexual risk and activity among vulnerable populations of adolescents (Cabezón et al., 2005; Jemmott, Lammott, and Fong 2010). Of course, the most common recommendation for preventing STDs and abortion among sexually active adolescents and young adults is to encourage the use of condoms.
In opposition to the prevailing consensus that the use of OCs is necessary to prevent unintended pregnancy and the use of condoms to prevent STDs among adolescents and young adults (Braverman et al., 2014; Ott et al., 2014), we theorized that the use of OCs to treat health problems and/or to avoid unintended pregnancy along with the teaching of safe sex actually leads to unhealthy sexual activity. Furthermore, unhealthy sexual activity, such as multiple sexual partners and early sexual debut, can lead to significant health problems such as unintended pregnancy, abortion, pelvic inflammatory disease (PID), and STDs. In addition, a previous study among all reproductive-age women, including adolescents and young adults, in an earlier National Survey of Family Growth (NSFG) Cycle 7 data set showed that there was a greater likelihood of abortion among those women who ever used OCs, and other methods of contraception, compared with women who never used contraceptive methods (Fehring 2011). We are now seeking to determine whether this association also occurs only among adolescents and young adults and with a more recent NSFG Cycle 8 data set. Therefore, the purpose of this study was to determine the association of the use of OCs among adolescents and young adults with pregnancy, abortion, STDs, PID, and unhealthy sexual behaviors (i.e., early sexual debut and multiple male sexual partners).
We hypothesized that those adolescents who ever used OCs will more likely ever have had sexual intercourse, an abortion, experience pregnancy, have had an STD or PID, and to have had more male sexual partners and an earlier sexual debut than those adolescents and young adults who never used OCs. We also hypothesized that those adolescents and young adult women who view religion as very important, have frequent church attendance, have attended a sexual-health-with-abstinence program and grew up with intact two-parent families would be less likely to have been sexually active than those who do not hold religion as important, do not have frequent church attendance, and did not grow up in intact families. Finally, we hypothesized that those adolescents and young adults who ever used condoms also will more likely experience STDs and abortion compared to adolescents and young adults who never used condoms.
Method
The NSFG has been conducted by the National Center for Health Statistics (NCHS) and the CDC approximately every five to seven years since 1973 (Mosher and Jones 2010; Mosher 2004; Piccinino and Mosher 1998). The NSFG includes factors that help explain trends in contraception use, infertility, sexual activity, and pregnancy outcomes. Researchers at the NCHS provide the data for legislators and policy makers to plan health services and health education programs. The NSFG is also available to researchers who may use the data set to determine trends in family health, contraceptive use, infertility, and sexual health choices.
The NSFG is conducted by demographic researchers at the University of Michigan using a nationally representative, randomly selected sample of women and (since 2002) men aged fifteen to forty-four in the United States. Interviews are conducted in person, take approximately eighty minutes to complete, and were conducted by female interviewers for women respondents. Sensitive questions (such as past history of abortion) are asked through a self-paced computer-assisted interview program. The response rates of these surveys range from 75 percent to 80 percent. In 2014, data sets were released from Cycle 8 of the 2011–2013 NSFG, which was conducted from September 2011 through September 2013 and includes 5,601women and 4,815 men aged fifteen to forty-four. The response rate for the 2011–2013 NSFG was 73.4 percent for females. The participants for this study were 1,367 females from the age fifteen through twenty-one who were never married. There are over 3,000 variables in the Cycle 8 data set.
The independent variables (and their NSFG labels) for this study were PILL or those women who ever used OCs (birth control pills) versus those who never used OCs and condom or those women who ever used condoms versus those who never used condoms. The health risk outcome variables were (1) EVERSEX, those participants who ever had sexual intercourse with a male; (2) partlif_1, the number of male sexual partners respondent has ever had, asked the first time; and (3) AGEFSTSX, the age of the respondent at first sexual intercourse. The health outcome variables were (1) STDEVER, respondent was ever treated for an STD; (2) PID, respondent was ever treated for PID; (3) EVERPREG, the respondent was ever pregnant; and (4) ABORTION, the respondent ever had an abortion and the frequency. The age entered for those respondents who never had sexual intercourse with a male was the current age at interview for the purposes of the survival analysis for sexual debut (see details below). The variable ABORTION had a lot of missing data. The missing data for this variable were coded as not ever having an abortion. We assumed never having an abortion since most of the nonresponding participants were not sexually active, that is, responded as to never had sex with a male.
The protective variables were importance of religion in respondent’s daily life (RELDLIFE); frequency of attendance at religious services (ATTNDNOW); intact family (INTACT—recoded), that is, always lived with both biological or adoptive parents; and ever attended an abstinence-only sexual education program that promotes waiting until marriage for sexual intercourse (SEDABST). Participants rated the importance of religion in their daily lives as very important, somewhat important, or not important. For the purposes of this analysis, these responses were dichotomized into two categories: (1) very important and (2) somewhat and not important. Participants indicated their frequency of religious service attendance as more than once a week, once a week, one to three times per month, less than once a month, or never. For analysis, these responses were also collapsed into two categories. Frequent attendance at religious services included one or more times per week and infrequent attendance included three times per month or less. Participants indicated whether they had resided within a two-parent family, defined in the original survey as presence of both parents (biological or adoptive) from birth to age eighteen.
Descriptive statistics were used to determine the demographics of the sample, including age, marital status, race, religion, and whether the respondent lived in an intact family with a mother and father. Relative risk odds ratios (OR), were calculated for ever sex or not, ever treated for an STD or not, ever treated for a PID or not, and ever pregnant or not, between those who ever used OCs (the Pill) compared to those adolescents or young adults who never used OCs. Differences in the number of male sexual partners between those adolescents and young adults who ever used OCs compared to those who did not was calculated with a Student’s t-test. Differences in age of sexual debut between respondents who ever had sex compared to those who never had sex was through Survival analysis (Kaplan–Meier), with time being current age or age of sexual debut, and ever sex as the event, and ever sex or not as the two conditions. Statistical significance was set at the .05 probability level; and in order to control for increased error rates with multiple testing, the Bonferroni average of .006 was determined. Survival analysis (in the form of a life table analysis) was used since we were determining how long an adolescent could “survive” before having sexual intercourse with a male. The Bonferroni correction was used as a statistical correction to lower the p value needed to demonstrate a significant difference due to the risk of repetitive sampling errors. Statistical analysis was performed by the use of the Statistical Package for Social Sciences (SPSS version 22). Only those women who indicated that they were heterosexual were included in the data analysis.
The NSFG Cycle 8 data set is available through the NCHS and is downloadable through the Internet into SPSS files. The data set does not contain any identifying variables and is intended for public use for statistical analysis only. Use of this data set was reviewed by the Office of Research Compliance at Marquette University and received exempt status.
Results
Demographics
Of the 5,210 women participants in the Cycle 8 NSFG data set, 1,367 were between the ages of fifteen and twenty-one and never married. Of these participants, the mean age was 17.95 (SD = 1.93). None of the participants were married, but 129 (9 percent) indicated they were cohabitating with the opposite sex. The majority (60.6 percent; N = 828) were listed as White, 24.9 percent (N = 341) were listed as Black, and 14.5 percent (N = 198) were listed as other. The majority (47.9 percent) listed their religion as Protestant, 24.6 percent were Catholic, 10.2 percent other religion, and 20.0 percent no religion. Compared to the general population in this age category, the NSFG has a bias toward non-White participants, that is, the White population is over 70 percent based on population data from 2013 United States Census Bureau (Colby and Ortman 2015).
Likelihood of Ever Sex
The likelihood OR of ever having sex among the adolescents and young adults was 7.25 (95 percent CI [confidence interval] = 5.61–9.38), that is, the use of OCs led to greater than seven times the risk of being sexually active compared to those who never used OCs.
Differences in number of male sexual partners
The adolescents and young adults (N = 545) who ever used OCs had significantly more sexual partners (X = 3.73, SD = 5.10) versus (X = 1.38, SD = 3.55) among the adolescents and young adults (N = 818) who never used OCs (t test = 10.08, df = 1,361, p ≤ .001).
Mean Age of Sexual Debut
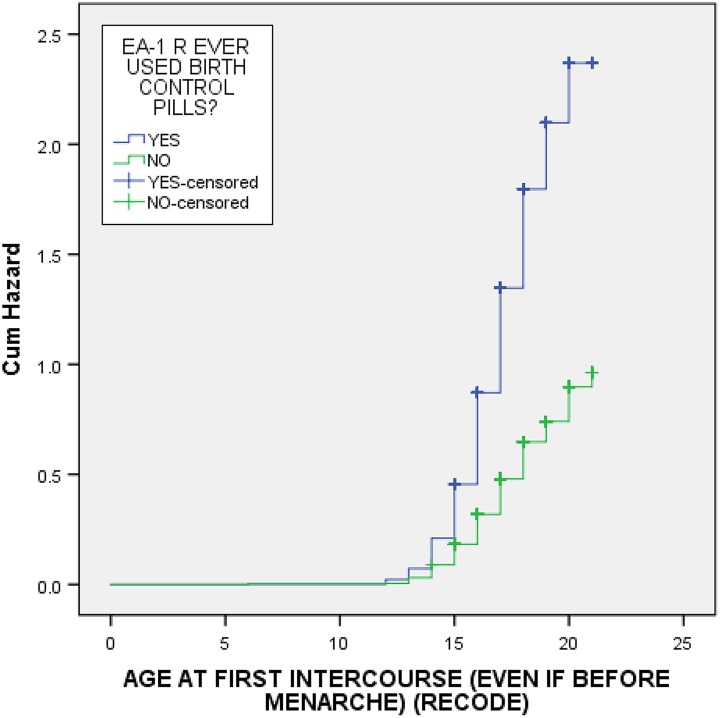
The mean age of sexual debut for the adolescents and young adults who ever used OCs was 16.27 (95 percent CI = 16.08–16.46), and for the adolescents and young adults who never used OCs, 18.20 (95 percent CI = 17.91–18.42). It should be noted that current age was used in the survival analysis for those who had not yet had intercourse. See Table 1 and Figure 1 for the hazard survival curve results. The survival curves show that the curve for those adolescents who ever used OCs rose faster than the curve for those adolescents who never used OCs, thus indicating an earlier age of sexual debut. The curves also show that they depart from each other at a very early age (i.e., around sixteen) indicating that the ever users of OCs initiate sexual intercourse at a very young age compared with never users of OCs.
Table 1.
Mean and Median Age for Sexual Debut and Confidence Levels for Survival Time. Adolescents Who Ever Used the Pill Have an Earlier Mean and Median Age of Sexual Debut Than Those Who Never Used the Pill.
| EA-1 R: Ever Used Birth Control Pills? | Meana | Median | ||||||
|---|---|---|---|---|---|---|---|---|
| Estimate | SE | 95 Percent confidence interval | Estimate | Estimate | SE | 95 Percent confidence interval | ||
| Lower bound | Upper bound | Lower bound | Upper bound | |||||
| Yes | 16.402 | .101 | 16.205 | 16.600 | 16.000 | .099 | 15.806 | 16.194 |
| No | 18.466 | .108 | 18.253 | 18.678 | 19.000 | .360 | 18.294 | 19.706 |
| Overall | 17.531 | .080 | 17.375 | 17.687 | 17.000 | .125 | 16.755 | 17.245 |
Figure 1.
Hazard survival curve showing differences in age of sexual debut between adolescents and young adults (fifteen to twenty-one years old) in the NSFG Cycle 8 who ever used the birth control pill versus those who never used the pill. The top curve is the survival time for those who ever used the pill and the bottom curve for those who never used the pill. The top curve shows a quicker and high rise and thus an earlier age of sexual debut than those adolescents indicated by the bottom line.
Likelihood of Abortion, STDs, Pregnancy, and PID
Table 2 provides the likelihood OR of having a negative health outcome for those adolescents and young adults who ever used an OC compared with adolescents and young adults who never used an OC. The likelihood of having an STD is almost three times greater in OC users, having a pregnancy is over three times the likelihood, and ever having PID is three times the likelihood when compared with adolescents and young adults who never used OCs.
Table 2.
Odds Ratio (OR) of Ever Having an Abortion, STD, PID, or Pregnancy among Adolescents and Young Adults Who Ever Used the Contraceptive Pill Compared to Adolescents and Young Adults Who Never Used the Pill as Found in Cycle 8 of the NSFG.
| Health Risk Problem | OR | 95 Percent Confidence Interval | p Values |
|---|---|---|---|
| Abortion | 10.50 | 4.07–27.07 | <.0001a |
| STD past twelve months | 2.74 | 1.69–4.43 | <.0001 |
| Ever pregnant | 3.35 | 2.48–4.53 | <.0001 |
| PID | 3.06 | 1.31–7.20 | <.003 |
aAbortion results need to be interpreted with a realization of underreporting of having an abortion among the participants.
Protective Factors
Table 3 shows the likelihood OR of ever having sex with potential protective factors for risky sexual behaviors. Those adolescents and young adults who rate religion as very important in their lives, attend church services at least once a week, and grew up in an intact family were significantly less likely to ever have sex than those adolescents and young adults who do not think that religion in their lives is very important, nor attend church services at least once a week, or did not live in an intact family. Attending an abstinence-only sexual education program did not reach significance (p = .044; significant if p < .006).
Table 3.
Odds Ratio (OR) of Ever Having Sex with a Male by Protective Behavior among Adolescents and Young Adults Who Never Used the Pill as Found in Cycle 8 of the NSFG.
| Protective Behaviors | OR | 95 Percent Confidence Interval | p Values |
|---|---|---|---|
| Importance of religion | 0.50 | 0.40–0.63 | <.0001 |
| Church attendance | 0.38 | 0.30–0.48 | <.0001 |
| Intact family | 0.66 | 0.54–0.82 | <.0001 |
| Sex education with abstinence | 0.77 | 0.61–0.99 | <.044* |
*Did not reach the Bonferroni correction for error rate of a p < .006.
Condoms, Abortion, and STDs
The likelihood of being treated for an STD in the past twelve months among adolescents and young adults was 8.11 times more frequent than among those that never used condoms (95 percent CI: 3.87–17.1, p < .0001). There was a 92 percent greater likelihood of ever having an abortion among those adolescents and young adults who ever used a condom compared to those adolescents and young adults who never used condoms (95 percent CI: 1.83–2.03, p < .0001).
Discussion
Findings
According to the data from Cycle 8 of the NSFG, the “ever use” of OCs (i.e., the Pill) by US adolescents and young adults coincides with a significantly greater likelihood of ever having sex, an STD, a PID, an unintended pregnancy, or abortion compared with those adolescents and young adults who never used OCs. Furthermore, those adolescents who ever used OCs had significantly more male sexual partners than those who never used OCs and had an earlier sexual debut by almost two years. The Cycle 8 data set also indicated that those US adolescents and young adults who felt religion to be very important in their lives, attended church at least once a week, and lived in an intact family were less likely to ever have sex than those adolescents and young adults who did not hold religion to be very important or go to church at least once a week or live in an intact family. Attendance in a sexual education program, which encouraged remaining sexually inactive until marriage, did not meet statistical significance, although the probability of this variable was in the right direction in lowering the risk of ever having sex.
This research confirms some earlier studies with Cycles 6 and 7 of the NSFG that showed that adolescents and young adults who held religion as important in their lives and had frequent church attendance were less likely to be sexually active and to have a later age of sexual debut (Edwards et al., 2008; Haglund and Fehring 2010; Haglund et al., 2011). This association of religiosity and sexual activity also held for populations with higher rates of sexual activity, for example, adolescents of Hispanic background. Another study with an earlier version of the NSFG also showed that those women who held religion to be very important and attended church at least once a week also were less likely to ever have an abortion as compared to women who did not feel religion was very important and had less frequent church attendance (Fehring and Ohlendorf 2008). The results of our study showed that those adolescents who ever used OCs were more likely to have had an STD or PID coincide with findings that frequent intercourse is associated with STDs (Forhan et al., 2009; Genuis 2004). As we hypothesized, the standard recommendations for using OCs and condoms to prevent unintended pregnancies and to reduce abortions and STDs were not supported by the data. The adolescents and young adults in the Cycle 8 NSFG were more likely to have had an abortion or an STD compared to those who never used condoms.
We did not find that attending an abstinence-only sexual education program resulted in a lowered likelihood of ever having sex in this population. A recent Cochrane review of sexual education programs concluded that such programs were not very effective in reducing pregnancy and STDs among adolescents (Mason-Jones et al., 2016). The length and content of these programs varied, so it is hard to judge their efficacy. Interestingly, they did find that simple measures like receiving a free uniform may reduce the incidence of some STDs. The Cochrane review did not include studies among adolescents in the United States (studies were from Africa, Latin America, and England). Furthermore, the studies were not population based, and, therefore, it is difficult to make inferences to other populations, especially adolescents in the United States. Of note, earlier studies have shown that sexual education and use of pledging to remain a virgin were associated with lower sexual risk behaviors (Haglund and Fehring 2010). In addition, a randomized comparison study of a chastity-based program in comparison to a contraceptive promotion sexual-health program among African American teens showed that the chastity-based program was more effective in decreasing sexual activity and unwanted pregnancy (Jemmott, Jammott, and Fong 2010). A randomized comparison of a high school, chastity-based sexual education program showed less sexual activity for those students who attended the program versus those that did not (Cabezón et al., 2005). This study involved a holistic approach of fertility awareness and developmentally sensitive curriculum.
Theoretical Understanding of the Findings—Lowering the Barriers
The main reasons provided by adolescents and young adults in the Cycle 8 NSFG for not being sexually active are moral or religious, not having the right partners, fear of pregnancy, and fear of STDs. Providing adolescents with OCs will lessen the fear of pregnancy and thus lower one obvious barrier to having an earlier sexual debut. However, while on OCs, some will also not use condoms due to the sense that it is not natural, not needed to prevent pregnancy, or the sexual partner does not like its use (Keogh 2005). Providing OCs even for noncontraceptive health problems could also lower the normal barriers to becoming sexually active. Healthcare providers may prescribe OCs with the understanding that the risks of OCs are outweighed by avoiding unintended pregnancies and the possibility of more frequent abortions. Our data demonstrate that contrary to this belief, ever use of OCs was associated with a more likely incidence of pregnancy. The provision OCs by health professionals may also suggest to vulnerable adolescents that being on OCs is part of a normal course of development that involves sexual experimentation. Parents too may be fearful of unintended pregnancy in their children and for this reason may request that their child’s healthcare provider prescribe OCs either for contraception or for other health problems that can be effectively managed by other means. However, our findings demonstrate that the use of OCs is associated with an increased likelihood of unhealthy sexual activity.
Limitations of the Study
One limitation of the NSFG data set that has been reported in the literature is the potential underreporting of abortion (Jagannathan 2001; Smith, Adler, and Tschann 1999). The reported lower use of abortion among those adolescents and young adults not using OCs or condoms could be due to abortion being an embarrassment that discourages admitting its use even with an anonymous survey. Abortion is an especially grave matter among Catholics, more conservative Protestants, and among Christians generally.
Another obvious weakness of the study is that the purpose of this study was to show associations, and not cause and effect, between risky sexual activity and other health outcomes with ever use of OCs. In order to provide evidence for cause and effect, researchers would have to randomize adolescents into a contraception-use group and an abstinence-only group and then determine the outcomes over time and ideally before the age of sexual debut. This type of design might be ethically problematic since it would require the researchers to prescribe a method of contraception to those adolescents randomized into the contraceptive use group.
There is also some question as to whether the population sampling technique for the NSFG truly represents the US population, especially among the Hispanic population. According to the US Census, about 68 percent of Hispanics in the United States consider themselves Catholic, while only 57 percent in the NSFG indicated that they are (McDonald et al., 2008). A strength of this study is that it is population based and because of that we can make generalizations to the US population of adolescents and young adults. The findings are also strengthened by having similar results from early versions of NSFG data sets (Edwards et al., 2008; Fehring and Ohlendorf 2008; Haglund and Fehring 2010; Haglund et al., 2011).
Another limitation is the difficulty of trying to measure religiosity among women using a retrospective data set. Religiosity has multiple dimensions that include belief, intrinsic religiosity, religious well-being, and participation in organized religious activity (Koenig, Smiley, and Gonzales 1988). The measure of religiosity in this study was limited to the items used in Cycle 8 of the NSFG. A very important component of religiosity that is missing is whether faith is intrinsic (or extrinsic) to the individual respondent. Finally, this study did not include other factors that are associated with risky sexual behaviors among adolescents and young adults, such as alcohol and illicit drug use.
Recommendations for Future Research
Recommendations for future research include comparing the findings from Cycle 6 (2002), Cycle 7 (2006), and Cycle 8 (2010) of the NSFG data sets. Comparing the results would allow analysis of trends in contraception use, sexual activity, STD rates, and sexual debut. Analysis of current use of OCs versus no method of family planning on health outcomes is another approach that would provide more evidence for the influence of contraception on the reproductive health of adolescents and young adults. Another recommendation is to look at Cycle 8, as was done in this study, and break down the analysis with special subpopulations of interest and, especially, different ethnicities and races. Finally, the influence of faith (i.e., religion) on family-planning patterns, sexual activity, and sexual debut (as expressed in the importance of religion and the frequency of church attendance) would be of interest. These religious variables are available in the NSFG data sets and have been studied in the past (Fehring and Ohlendorf 2007).
Conclusion
The consensus among health professionals is that there is a great need to provide sexually active adolescents with the pill, condoms, and, more recently, hormonal implants and Intrauterine Devices (IUDs), as the best option to prevent unintended pregnancy, abortion, and STDs (Braverman et al., 2014; Lawrence et al., 2011; Lawrence et al., 2011; Ott et al., 2014; Tu et al., 2009). Although the NSFG data did not show that abstinence-based sexual education programs were associated with less likelihood of risky sexual behaviors, the NSFG variable did not include all abstinence programs, including those which have shown favorable efficacy rates in reducing teenage sexual activity (Vigil et al., 2006). Yet, these approaches are not solving the problem of unintended pregnancy, abortion, and STDs. Since the goals of reducing pregnancy and STD rates are not being achieved either (Dueñas et al., 2011), with the widespread use of OCs and sexual education programs, healthcare providers must honestly approach adolescents, young adults, and parents with this information. Healthcare providers should also provide information on other factors that reduce these consequences of risky sexual behaviors. Based on the data reported here and elsewhere, this includes positive social determinants such as religiosity and an intact family, as well as an abstinence pledge (Haglund and Fehring 2010).
The purpose of this article was to show the correlation between contraceptive use in adolescents and outcomes. The National Survey of Family Growth (NSFG) data from 2011 to 2013 have demonstrated that adolescents who were never married and ever used contraception were three times more likely to have an STD, have PID and, surprisingly, three times more likely to become pregnant, the very outcome contraception is intended to prevent, compared to the noncontracepting group. These data also showed that the contraceptors have significantly more male partners than their noncontracepting counterparts and significantly earlier sexual debut. Protective factors such as church attendance and family cohesiveness were found to decrease the likelihood of sexual activity.
Teen pregnancy is ranked among the Centers for Disease Control’s most recent top ten national health concerns (http://www.cdc.gov/psr, 12/2015). One of the aims of the CDC’s “Prevention Status Report” for teen pregnancy is to provide family planning, contraceptive insurance coverage, so that it can be more accessible to more youth. Other strategies, such as sexual health education, positive youth development programs, improving parent–child communication, and parental monitoring of youth behavior, are touted as other components of this teen pregnancy prevention task force.
In light of the NFSG data, contraception as the best means of achieving reduced teen pregnancy rates and improved overall teen health needs to be seriously reconsidered. More efforts need to be given toward encouraging total well-being of the adolescent, including spiritual well-being to promote healthy lifestyles. Providers can also provide mental support and counseling services for adolescents and their families to help maintain family cohesiveness when lacking. Lastly, but most importantly, providers can be trained to provide noncontraceptive support to the adolescent and their parent(s) contemplating contraception, knowing that they are giving the best medical advice.
Biographical Notes
Richard J. Fehring, PhD, RN, FAAN, is Professor Emeritus and director of the Marquette University College of Nursing Institute for Natural Family Planning.
Thomas Bouchard, MD, is a family medicine physician and clinical lecturer at the University of Calgary.
Maria Meyers, MD, is a pediatrician in Birmingham, Alabama, and is affiliated with multiple hospitals and clinics in the area, including Children’s Hospital of Alabama at UAB and Urgent Care for Children.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Maria Meyers, MD  http://orcid.org/0000-0002-3416-0032
http://orcid.org/0000-0002-3416-0032
References
- American Academy of Pediatrics and American College of Obstetricians and Gynecologists. 2006. “Menstruation in Girls and Adolescents: Using the Menstrual Cycle as a Vital Sign.” Pediatrics 118(5) :2245–50. [DOI] [PubMed] [Google Scholar]
- Bhupathiraju S. N., Grodstein F., Stampfer M. J., Willett W. C., Hu F. B., Manson J. E. 2016. “Exogenous Hormone Use: Oral Contraceptives, Postmenopausal Hormone Therapy, and Health Outcomes in the Nurses’ Health Study.” American Journal of Public Health 106(9): 1631–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braverman P. K., Adelman W. P., Alderman E. M., Breuner C. C., Levine D. A., Marcell A. V., O’Brien R. F., and AAP Committee on Adolescence. 2014. “Contraception for Adolescents.” Pediatrics 134(4): e1244–56. [DOI] [PubMed] [Google Scholar]
- Bunting L., Boivin J., 2010. “Development and Preliminary Validation of the Fertility Status Awareness Tool: FertiSTAT.” Human Reproduction 25(7): 1722–33. doi:10.1093/humrep/deq087. [DOI] [PubMed] [Google Scholar]
- Cabezón C, Vigil P., Rojas I., Leiva M. E., Riquelme R., Aranda W., García C. 2005. “Adolescent Pregnancy Prevention: An Abstinence-centered Randomized Controlled Intervention in a Chilean Public High School.” Journal of Adolescent Health 36(1): 64–9. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) and the National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention (NCH). 2015. “Reported STDs in the United States: 2014 National Data for Chlamydia, Gonorrhea, and Syphilis.” CDC Fact Sheet. [Google Scholar]
- Chapron C., Souza C., Borghese B., Lafay-Pillet M. C., Santulli P., Bijaou G., Goffiner F., de Ziegler D. 2011. “Oral Contraceptives and Endometriosis: The Past Use of Oral Contraceptives for Treating Severe Primary Dysmenorrhea Is Associated with Endometriosis, Especially Deep Infiltrating Endometriosis.” Human Reproduction 26:2028–35. [DOI] [PubMed] [Google Scholar]
- Chapron C., Lafay-Pillet M. C., Monceau E., Borghese B., Ngo C., Souza C., de Ziegler D. 2011. “Questioning Patients about Their Adolescent History can Identify Markers Associated with Deep Infiltrating Endometriosis.” Fertility and Sterility 95(3): 877–81. [DOI] [PubMed] [Google Scholar]
- Cheang K. I., Essah P. A., Sharma S., Wickham E. P., Nestler J. E., 2011. “Divergent Effects of a Combined Hormonal Oral Contraceptive on Insulin Sensitivity in Lean Versus Obese Women.” Fertility and Sterility 96(2): 353–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colby S. L., Ortman J. M. 2015. “Projections of the Size and Composition of the U.S. Population: 2014 to 2060 Population Estimates and Projections.” Current Population Reports, U.S. Census Bureau, #P25-1143 (March). [Google Scholar]
- Dueñas J. L., Lete I., Bermejo R., Arbat A., Pérez-Campos E., Martínez-Salmeán J., Serrano I., Doval J. L., Coll C. 2011. “Trends in the Use of Contraceptive Methods and Voluntary Interruption of Pregnancy in the Spanish Population during 1997–2007.” Contraception 83:82–87. [DOI] [PubMed] [Google Scholar]
- Edwards L., Fehring R., Jarrett K. M., Haglund K. 2008. “The Influence of Religiosity on the Sexual Behaviors of Latina/O Adolescents.” Hispanic Journal of Behavioral Sciences 30(4): 447–62. [Google Scholar]
- Fehring R. 2011. “The Influence of Contraception on Abortion among Women of Reproductive Age.” Proceedings of the 24th life and Learning Conference 18:1–18. [Google Scholar]
- Fehring R., Cheever K., German K., Philpot C. 1998. “Religiosity, Sexual Activity, and Attitudes of Sexual Permissiveness among Older Adolescents.” Journal of Religion and Health 37(3): 229–48. [Google Scholar]
- Fehring R., Ohlendorf J. M. 2007. “The Relationship between Religiosity and Contraceptive Use among Roman Catholic Women in the United States.” The Linacre Quarterly 74:135–44. [Google Scholar]
- Fehring R., Ohlendorf J. 2008. “The Influence of Religiosity on Contraceptive Use and Abortion in the United States.” Life and Learning 17:398–416. [Google Scholar]
- Fontes M., Roach P. 2007. “Predictors and Confounders of Unprotected Sex: A UK Web-Based Study.” European Journal of Contraception and Reproductive 12:36–45. [DOI] [PubMed] [Google Scholar]
- Forhan S. E., Gottliebb S. L., Sternberg M. R., Xu F., Datta S. D., McQuillan G. M., Berman S. M., Markowitz L. E. 2009. “Prevalence of Sexually Transmitted Infections among Female Adolescents Aged 14 to 19 in the United Sates.” Pediatrics 124:1505–12. [DOI] [PubMed] [Google Scholar]
- Frank-Herrmann P., Gnoth C., Baur S., Strowitzki T., Freundl G. 2005. “Determination of the Fertile Window: Reproductive Competence of Women—European Cycle Databases.” Gynecological Endocrinology 20:305–12. [DOI] [PubMed] [Google Scholar]
- Genuis S. 2004. “Managing the Sexually Transmitted Disease Pandemic: A Time for Reevaluation.” American Journal of Obstetrics and Gynecology 191(4): 1103–12. [DOI] [PubMed] [Google Scholar]
- Haglund K. A., Fehring R. J. 2010. “The Association of Religiosity, Sexual Education, and Parental Factors with Risky Sexual Behaviors among Adolescents and Young Adults.” Journal of Religion and Health 49:460–72. [DOI] [PubMed] [Google Scholar]
- Haglund K., Edwards L., Fehring R., Pruzynski J. 2011. “Religiosity and Sexual Risk Behaviors among Latina Adolescents: Trends from 1995–2008.” Journal of Women’s Health 20(6): 871–77. [DOI] [PubMed] [Google Scholar]
- Heitmann R. J., Langan K. I., Huang R. R., Chow G. E., Burney R. O. 2014. “Premenstrual Spotting of > 2 Days is Strongly Associated with Histologically Confirmed Endometriosis in Women with Infertility.” American Journal of Obstetrics and Gynecology 211:358.e1–6. [DOI] [PubMed] [Google Scholar]
- Hemminki E., Luostarinen T., Pukkala E., Apter D., Hakulinen T. 2002. “Oral Contraceptive Use before First Birth and Risk of Breast Cancer: A Case Control Study.” BMC Women’s Health 2(9): 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jagannathan R. 2001. “Relying on Surveys to Understand Abortion Behavior: Some Cautionary Evidence.” American Journal of Public Health 91:1825–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jemmott J. B., Lammott L. S., Fong G. T. 2010. “Efficacy of a Theory-based Abstinence-only Intervention over 24 months.” Archives of Pediatric and Adolescent Medicine 164:152–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kastbom Å. A., Sydsjö G., Bladh M., Priebe G., Svedin C. G. 2015. “Sexual Debut Before the Age of 14 Leads to Poorer Psychosocial Health and Risky Behaviour in Later Life.” Acta Paediatrica 104(1): 91–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keogh L. H. 2005. “Understandings of the ‘Natural’ Body: Comparison of the Views of Users and Providers of Emergency Contraception.” Sexual Health 2:109–15. [DOI] [PubMed] [Google Scholar]
- Koenig H. G., Smiley M., Gonzales J. A. P. 1988. Religion, Health, and Aging. A Review and Theoretical Integration. Westport, CT: Greenwood Press. [Google Scholar]
- Lanfranchi A. 2013. “Normal Breast Physiology: The Reasons Hormonal Contraceptives and Induced Abortion Increase Breast-cancer Risk.” The Linacre Quarterly 8:236–49. [PubMed] [Google Scholar]
- Lara L. A., Abdo C. H. 2016. “Age at Time of Initial Sexual Intercourse and Health of Adolescent Girls.” Journal of Pediatric and Adolescent Gynecology 29(5): 417–23. [DOI] [PubMed] [Google Scholar]
- Larsson M., Eurenius K., Westerling R., Tyden T. 2006. Evaluation of a sexual education intervention among Swedish high school students. Scandinavian Journal of Public Health 34(2): 124–131. [DOI] [PubMed] [Google Scholar]
- Lawrence R. E., Rasinski K. A., Yoon J. D., Curlin F. A. 2011. “Adolescents, Contraception and Confidentiality: A National Survey of Obstetrician-gynecologists.” Contraception 84(3):259–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence R. E., Rasinski K. A., Yoon J. D., Curlin F. A. 2011. Factors influencing physicians’ advice about female sterilization in USA: a national survey. Human Reproduction. 26(1): 106–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindberg L., Santelli J., Desai S. 2016. “Understanding the Decline in Adolescent Fertility in the United States 2007–2012.” Journal of Adolescent Health 59(5): 577–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason-Jones A. J., Sinclair D., Mathews C., Kagee A., Hillman A., Lombard C. 2016. “School-based Interventions for Preventing HIV, Sexually Transmitted Infections, and Pregnancy in Adolescents.” Cochrane Data Base of Systematic Reviews 11:CD006417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald J. A., Suellentrop K., Paulozzi L. J., Morrow B. 2008. “Reproductive Health of the Rapidly Growing Hispanic Population: Data from the Pregnancy Risk Assessment Monitoring System, 2002.” Maternal Child Health Journal 12(3): 342–56. [DOI] [PubMed] [Google Scholar]
- Morrison J. A., Glueck C. J., Daniels S., Wang P., Stroop D. 2011. “Ramifications of Adolescent Menstrual Cycles >42 Days in Young Adults.” Fertility and Sterility 96(1): 236–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mosher W. D. 2004. “Use of Contraception and Use of Family Planning Services in the United States: 1982–2002.” Advanced Data 10:1–36. [PubMed] [Google Scholar]
- Mosher W. D., Jones J. 2010. “Use of Contraception in the United States: 1982–2008.” Vital and Health Statistics Series 23(29): 1–771. [PubMed] [Google Scholar]
- Ott M. A., Sucato G. S., Braverman P. K., Adelman W. P., Alderman E. M., Breuner C. C., Levine D. A., Marcell A. V., O’Brien R. F., and AAP Committee on Adolescence. 2014. “Contraception for Adolescents: Technical Report.” Pediatrics 134(4): e1257–81. [DOI] [PubMed] [Google Scholar]
- Piccinino L. J., Mosher W. D. 1998. “Trends in Contraceptive Use in the United States: 1982–1995.” Family Planning Perspectives 30:4–10, 46. [PubMed] [Google Scholar]
- Resnick M. D., Bearman P. S., Blum R. W., Bauman K. E., Harris K. M., Jones J., Tabor J., Beuhring T., Sieving R. E., Shew M., Ireland M., Bearinger L. H., Udry J. R. 1997. “Protecting Adolescents from Harm—Findings from the National Longitudinal Study on Adolescent Health.” Journal of the American Medical Association 278:823–32. [DOI] [PubMed] [Google Scholar]
- Rosenfield R. L. 2015. “The Diagnosis of Polycystic Ovary Syndrome in Adolescents.” Pediatrics 136(6): 1154–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith L. B., Adler N. E., Tschann J. M. 1999. “Underreporting of Sensitive Behaviors: The Case of Young Women’s Willingness to Report Abortion.” Health Psychology 18:37–43. [DOI] [PubMed] [Google Scholar]
- Tu F. F., Du H., Goldstein G. P., Beaumont J. L., Zhou Y., Brown W. J. 2014. “The Influence of Prior Oral Contraceptive Use on Risk of Endometriosis is Conditional on Parity.” Fertility and Sterility 101(6): 1697–704. [DOI] [PubMed] [Google Scholar]
- Tu W., Batteiger B. E., Wiehe S., Ofner S., Van Der Pol B., Katz B. P., Orr D. P., Fortenberry J. D. 2009. “Time from First Intercourse to 11 First Sexually Transmitted Infection Diagnosis among Adolescent Women.“ Archives of Pediatric and Adolescent Medicine 163: 1106–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tydén T., Bjorkelund C., Olsson S. E. 1991. “Sexual Behavior and Sexually Transmitted Diseases among Swedish University Students.” Acta Obstetricia et Gynecologica Scandinavica 70(3): 219–24. [DOI] [PubMed] [Google Scholar]
- Tydén T., Bjorkelund C., Odlind V., Olsson S. E. 1996. Increased use of condoms among female university students: a 5-year follow-up of sexual behavior. Acta Obstetricia et Gynecologica Scandinavica, 75(6) , 579–584. [DOI] [PubMed] [Google Scholar]
- Tyden T., Olsson S. E., Haggstrom-Nordin E. 2001. Improved use of contraceptive, attitudes toward pornography, and sexual harassment among female university students. Womens Health Issues. 11(2): 87–94. [DOI] [PubMed] [Google Scholar]
- Tyden T., Palmqvist M., Larsson M. 2012. A repeated survey of sexual behavior among female university students in Sweden. Acta Obstetricia et Gynecologica. 91(2): 215–219. [DOI] [PubMed] [Google Scholar]
- Vigil P. F., Ceric M. E., Cortez H., Klaus H. 2006. “Usefulness of Monitoring Fertility from Menarche.” Journal of Pediatric Adolescent Gynecology 18:173–9. [DOI] [PubMed] [Google Scholar]
- Youngster M., Laufer M. R., Divasta A. D. 2013. “Endometriosis for the Primary Care Physician.” Current Opinions in Pediatrics 25(4): 454–62. [DOI] [PubMed] [Google Scholar]