Enterotoxigenic Escherichia coli (ETEC) causes diarrheal illness in infants in the developing world and travelers to countries where the disease is endemic, including military personnel. ETEC infection of the host involves colonization of the small intestinal epithelium and toxin secretion, leading to watery diarrhea.
KEYWORDS: ETEC, CfaE, HuMAb, fimbriae, adhesins
ABSTRACT
Enterotoxigenic Escherichia coli (ETEC) causes diarrheal illness in infants in the developing world and travelers to countries where the disease is endemic, including military personnel. ETEC infection of the host involves colonization of the small intestinal epithelium and toxin secretion, leading to watery diarrhea. There is currently no vaccine licensed to prevent ETEC infection. CFA/I is one of the most common colonization factor antigens (CFAs). The CFA/I adhesin subunit, CfaE, is required for ETEC adhesion to host intestinal cells. Human antibodies against CfaE have the potential to block colonization of ETEC and serve as an immunoprophylactic against ETEC-related diarrhea. Mice transgenic for human immunoglobulin genes were immunized with CfaE to generate a panel of human monoclonal IgG1 antibodies (HuMAbs). The most potent IgG1 antibodies identified in the in vitro functional assays were selected and isotype switched to secretory IgA (sIgA) and tested in animal colonization assays via oral administration. Over 300 unique anti-CfaE IgG1 HuMAbs were identified. The lead IgG1 anti-CfaE HuMAbs completely inhibited hemagglutination and blocked adhesion of ETEC to Caco-2 cells. Epitope mapping studies revealed that HuMAbs recognized epitopes in the N-terminal domain of CfaE near the putative receptor binding site. Oral administration of anti-CfaE antibodies in either IgG or sIgA isotypes inhibited intestinal colonization in mice challenged with ETEC. A 2- to 4-log decrease in CFU was observed in comparison to mice challenged with irrelevant isotype controls. We identified fully human monoclonal antibodies against the CfaE adhesion domain that can be potentially employed as an immunoprophylactic to prevent ETEC-related diarrhea.
INTRODUCTION
Enterotoxigenic Escherichia coli (ETEC) is one of the main causes of diarrhea in infants in the developing world as well as the major cause of traveler's diarrhea (1). Transmission of ETEC occurs when contaminated food or water is ingested. ETEC infections are characterized by diarrhea, vomiting, stomach cramps, and in some cases mild fever. Symptoms usually occur 1 to 3 days after infection and last for a few days (2). When adult travelers develop ETEC diarrhea, a short course of antibiotics can decrease the duration and volume of diarrhea. However, ETEC strains are becoming increasingly resistant to antibiotics (3–5), and there are currently no licensed vaccines for protecting travelers against ETEC diarrhea.
ETEC mediates small intestine adherence through filamentous bacterial surface structures known as colonization factors (CF). Once bound to the small intestine, the bacteria produce heat-labile toxins (LT) and/or heat-stable toxins (ST) that, through a cascade process, cause a net flow of water from the cell into the intestinal lumen, resulting in watery diarrhea (6, 7). ETEC vaccine development efforts have focused on the induction of host immunity against CFs or toxins by using cellular or subunit-based approaches. LT has been considered a possible target based on its strong immunogenicity, while ST was not initially considered due to poor immunogenicity and potent toxicity. Progress has been made recently in the identification of effective LT-ST toxoids (8, 9). However, anti-ST and anti-LT antibody responses may not be sufficient for effective protection against ETEC diarrhea (8). Instead, the toxin itself may be useful as an adjuvant to improve immunogenicity and efficacy when combined with the anticolonization response (10).
Development of an effective immunoprophylactic against ETEC bacterial attachment and colonization has long been considered an effective approach to prevent ETEC diarrhea (11, 12). The attachment and colonization steps are critical for bacteria to effectively produce toxin and represent a potential strategic target for preventing ETEC infection. The first human-specific ETEC fimbria to be described was colonization factor antigen I (CFA/I) (13). CFA/I is one of the most prevalent colonization factor antigens expressed by pathogenic ETEC isolates (14, 15). CFA/I is composed of a minor adhesin subunit (CfaE) at the tip of the fimbria that stabilizes the structure and a long homopolymeric subunit (CfaB) that makes up the stalk of the structure.
Recent studies have demonstrated that the adhesin subunit itself can provide sufficient immunity to prevent ETEC adhesion and subsequent infection (16, 17). In animal models, maternal vaccination with CfaE resulted in passive protection of neonatal mice from lethal challenge with ETEC strain H10407. In human clinical trials, a hyperimmune bovine IgG (bIgG) was generated by immunization of a cow with a recombinant form of CfaE and evaluated as a prophylactic treatment in healthy volunteers challenged with ETEC. Oral administration of bIgG antibodies raised against the CFA/I minor pilin subunit, CfaE, led to the protection of over 60% of the test group, suggesting that adhesin-based protective antibodies could be used as immunoprophylaxis against ETEC infection (16).
Here we describe the identification of a panel of anti-CfaE human monoclonal antibodies (HuMAbs) that are active against wild-type (or fully virulent) ETEC with high potency in functional assays. Oral administration of the lead HuMAbs in either the IgG form or the secretory IgA (sIgA) form, the immunoglobulin predominantly secreted at mucosal surfaces, led to 1- to 2-log10 decreases in CFU in an animal model with ETEC challenge. These anti-CfaE HuMAbs have the potential to be explored as oral immunoprophylaxis against ETEC infection.
RESULTS
Generation of anti-CfaE HuMAbs.
The N-terminal portion of the adhesin CfaE acts as the receptor binding domain of CFA/I adhesion to host cells (18, 19). To generate a panel of HuMAbs that can provide antiadhesive immunity, eight mice transgenic for human immunoglobulin heavy and light chain genes (Bristol-Myers Squibb; HuMAb mice) were immunized with the N-terminal adhesin domain of CfaE fused to maltose binding protein (MBP–CfaE-N). Serum response to MBP–CfaE-N was measured by enzyme-linked immunosorbent assay (ELISA). Spleens from mice with a positive ELISA response were harvested and fused to melanoma cells to generate hybridomas. A total of 1,895 hybridomas were found reactive to MBP–CfaE-N but not the MBP tag itself. Reverse transcription (RT)-PCR was performed on 900 hybridomas to determine the antibody heavy chain gene sequences. A total of 360 HuMAbs with unique sequences were selected for further characterization.
Selection of 10 lead HuMAbs in MRHA assays.
All 360 unique HuMAbs were purified and tested for their ability to inhibit mannose-resistant hemagglutination (MRHA) of human group A erythrocytes. MRHA has long been considered a surrogate method for the assessment of ETEC adhesion to the intestinal mucosa (20). The results of the MRHA assays were reported as the maximal inhibitory concentration (IC100). Thirty-six of all 360 HuMAbs showed IC100 activity in the nanomolar concentration range. Ten HuMAbs were selected as lead candidates, with IC100 values between 0.13 μg/ml and 0.24 μg/ml. The heavy chain and light chain gene regions of the lead HuMAbs were amplified from hybridoma cells and cloned into an immunoglobulin G1 expression vector for antibody expression and purification as previously described. Heavy and light chain variable gene families of the lead HuMAbs are reported in Table 1.
TABLE 1.
Anti-CfaE HuMAb heavy and light chain variable gene families
| Clone | Gene family for: |
||||
|---|---|---|---|---|---|
| Heavy chain |
Light chain |
||||
| VH | D | JH | VL | JK | |
| 68-51 | 4-34 | 2-08 | 3 | 1-12 | 2 |
| 68-61 | 1-69 | 2-21 | 3 | 1-16 | 2 |
| 68-97 | 4-34 | 7-27 | 3 | 1-12 | 2 |
| 68-90 | 4-34 | 7-27 | 3 | 1-12 | 2 |
| 68-75 | 4-34 | 2-02 | 6 | 1-13 | 1 |
| 67-102 | 4-34 | 2-15 | 3 | 1-12 | 4 |
| 840-53 | 30-30 | 7-27 | 4b | 1-06 | 1 |
| 68-48 | 4-34 | 7-27 | 6 | 1-13 | 1 |
| 837-6 | 3-23 | 6-06 | 2 | 1-27 | 5 |
| 68-06 | 1-69 | 4-17 | 3 | 1-16 | 2 |
Anti-CfaE HuMAbs bind to recombinant CfaE and live ETEC strain.
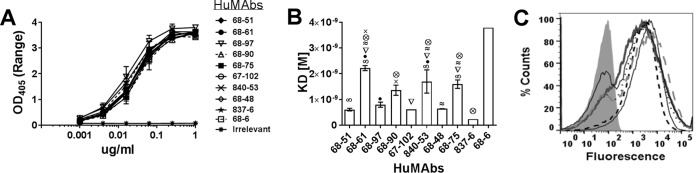
ELISA results showed that the concentration-dependent binding activities to CfaE by the lead HuMAbs were indistinguishable (Fig. 1A). To further differentiate the CfaE-binding activities of HuMAbs, antibody affinity was analyzed by surface plasmon resonance using recombinant MBP–CfaE-N. All 10 HuMAbs showed high affinities to MBP–CfaE-N with dissociation constant (Kd) values in the low nanomolar range (0.6 nM to 1.2 nM) (Fig. 1B). HuMAb 837-6 showed the highest affinity of the 10, with a Kd value of 2.3 × 10−10. HuMAbs 68-51, 68-97, 67-102, 68-48, and 837-6 were found to have higher affinities than HuMAbs 68-61, 68-90, 840-53, and 68-75.
FIG 1.
Binding of anti-CfaE MAbs. (A) ELISA. IgG bound to immobilized recombinant CfaE-N was detected with an anti-human IgG Fc chain-specific alkaline phosphatase-conjugated antibody. Error bars represent the range in OD values observed in two independent experiments. The binding curves of the 10 anti-CfaE MAbs are superimposed. (B) Surface plasmon resonance was used to measure the equilibrium dissociation constant (Kd). Error bars represent the standard deviation of results of two independent experiments. Results for all of the anti-CfaE antibodies were significantly different from those for the 68-6 HuMAb (P < 0.0001). Symbols represent significant differences (P < 0.01) between the anti-CfaE HuMAbs using one-way ANOVA. (C) Direct binding to live bacterial cells measured by flow cytometry. The gray filled area represents bacteria incubated with an irrelevant antibody.
To assess HuMAb recognition of CfaE expressed by live bacteria, strain H10407 was grown under an iron starvation condition to induce CfaE protein expression (21). The bacteria were then incubated with each of the lead 10 HuMAbs, followed by fluorescence-conjugated secondary antibody and fluorescence-activated cell sorting (FACS) analysis. All HuMAbs showed strong binding activity to strain H10407. The binding activities were comparable among all 10 antibodies (Fig. 1C).
Anti-CfaE HuMAbs prevent ETEC adherence to intestinal cells at low concentrations.
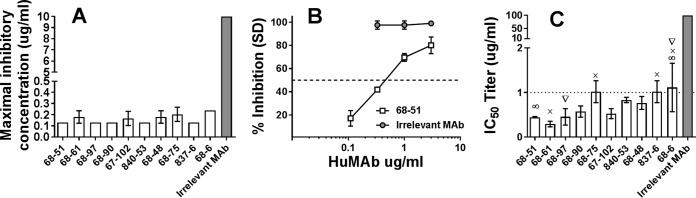
To determine whether the lead HuMAbs were capable of inhibiting bacterial adhesion, a cell adhesion assay with Caco-2 cells (a human intestinal epithelial cell line) was performed. An example of a concentration-dependent inhibition curve is shown in Fig. 2B. The minimal inhibitory concentration needed to prevent 50% (IC50) of bacterial adhesion was reported as representing antibody potency. All 10 HuMAbs showed strong potency to block bacterial adhesion at IC50 concentrations between 0.3 and 1.3 μg/ml. HuMAbs 68-51, 68-61, and 68-97 were found to have the lowest IC50s (Fig. 2C). Interestingly, HuMAbs showing comparable activities in MRHA assays (Fig. 2A) were more variable in their activities in Caco-2 cell adhesion assays.
FIG 2.
In vitro functional activity of anti-CfaE HuMAbs. (A) Hemagglutination assay. The ability of the MAbs to prevent hemagglutination is reported as the minimal inhibitory concentration (IC100). Error bars represent the standard deviation of results observed in three independent experiments using different blood donors. (B) Caco-2 adhesion assay. Example of inhibition curve obtained with HuMAb 68-51 and an irrelevant control. (C) The minimal effective IgG dose to prevent 50% (IC50) of bacterial adhesion to intestinal Caco-2 cells was used to determine antibody potency ranking. Error bars represent the standard deviation of results of three or four independent experiments. Results for all the anti-CfaE HuMAbs were significantly different from those for the irrelevant MAb (P<0.0001). Symbols represent significant differences (P < 0.01) within the anti-CfaE HuMAbs based on one-way ANOVA.
Epitope mapping of lead anti-CfaE HuMAbs.
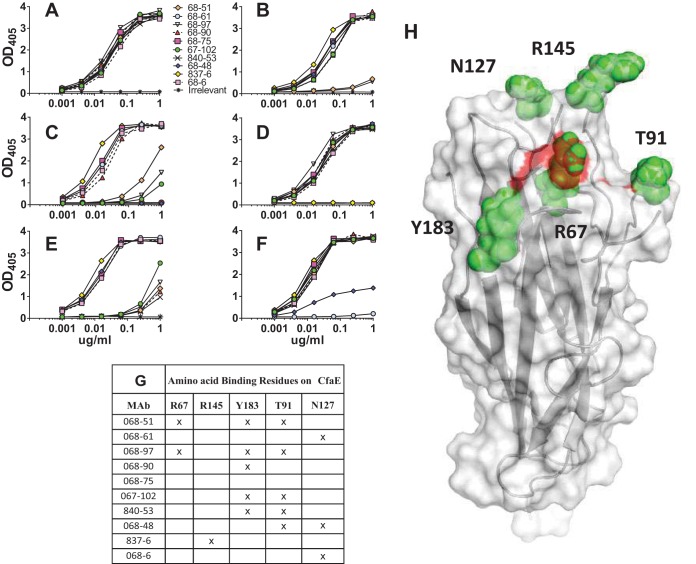
To define the antibody-binding epitope, putative antibody-antigen interaction models were established based on a previously resolved CfaE structure (PDB ID 2HB0) and the lead HuMAb sequences using an antibody modeling program, BioLuminate (Schrodinger). This software suite develops models of antibody structures from their sequences, followed by computational docking to identify high-confidence antibody-antigen complex models. Based on these models, the software identified potential residues critical for the binding interaction. The effect of these residues on the binding activity of the HuMAbs was analyzed by experimental alanine scanning, followed by ELISA. ELISA results indicated that mutating five of the predicted residues to alanine affected HuMAb binding (Fig. 3). The R67A mutation eliminated the binding activity of HuMAbs 68-51 and 68-97 (Fig. 3B), while the Y183A mutation affected the binding activity of HuMAbs 68-51, 68-97, 68-90, 67-102, and 840-53 (Fig. 3E). The R145A mutation abolished the binding activity of HuMAb 837-5 (Fig. 3D). The T91A mutation eliminated the binding activity of HuMAb 840-53 and reduced the binding activities of HuMAbs 68-51, 68-61, 840-53, and 68-48 (Fig. 3C). The N127A mutation eliminated the binding activity of HuMAb 68-61 and reduced the binding of HuMAbs 68-48 and 68-6 (Fig. 3F). A summary of the residues discovered to affect binding are shown in Fig. 3G. All mutations were found on the surface-exposed loops of the N-terminal domain of the CfaE (Fig. 3H). No residues involved in the binding of MAb 68-75 to CfaE were identified.
FIG 3.
Epitope mapping studies. Binding of anti-CfaE MAbs to mutants of recombinant CfaE as measured by ELISA. (A) Wild-type CfaE; (B) Arg67Ala mutant; (C) Thr91Ala mutant; (D) Arg145Ala mutant; (E) Tyr183Ala mutant; (F) Asn127Ala mutant. (G) Summary of the amino acid residues discovered to affect binding of anti-CfaE MAbs. (H) Crystal structure of N-terminal CfaE molecule with the five residues involved in the anti-CfaE MAb binding shown as green spheres. Highlighted in red are the three arginines forming the putative receptor binding domain.
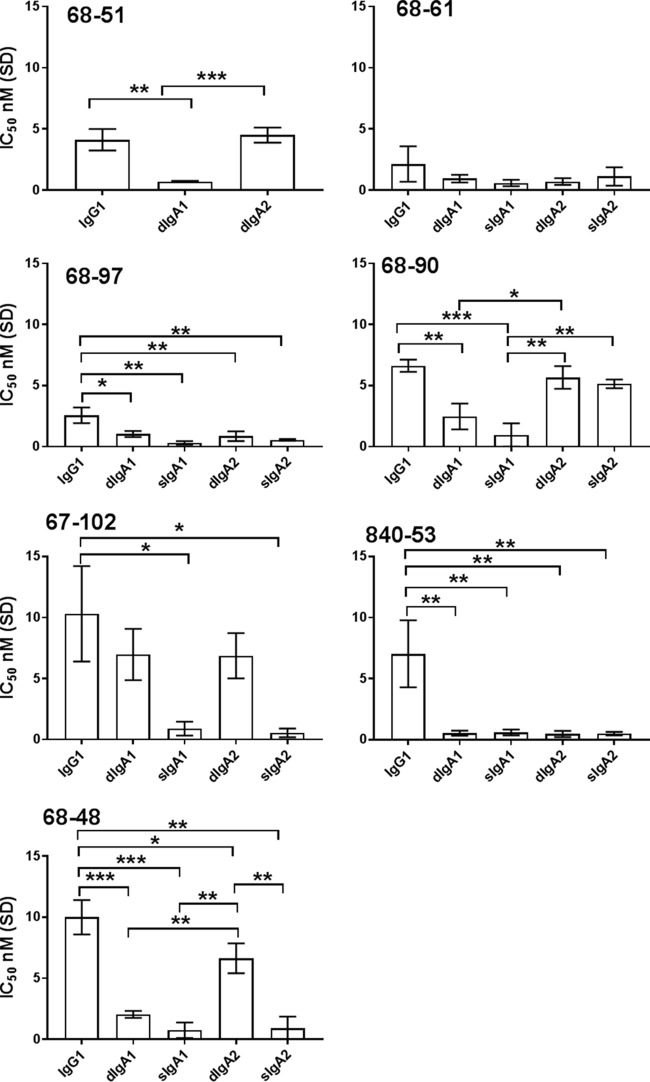
Isotype switch of anti-CfaE HuMAbs to sIgA.
Seven IgG1 HuMAbs (68-51, 68-61, 68-97, 68-90, 67-102, 68-48, and 840-53) found to have the lowest IC50s in Caco-2 cell adhesion assays were selected as the leads for further characterization in immunoglobulin class switching. Antibody variable regions were cloned into an expression vector with an IgA constant region to generate monomeric IgA. Monomeric IgA antibodies were also coexpressed with J chain with or without the secretory component to produce dimeric IgA (dIgA) and secretory IgA (sIgA), respectively. Antibodies with various isotypes were tested for their functionality in Caco-2 cell adhesion assays (Fig. 4). In general, all the antibodies retained or increased in vitro functional activity when converted into dIgA or sIgA. Specifically, the in vitro functional activity of 68-61 was not altered significantly when converted to either the dimeric or secretory IgA molecule. In contrast, Ig class switching to either dimeric or secretory IgA forms caused significant improvement of functional activity for HuMAbs 68-97, 840-53, and 68-48. Interestingly, HuMAb 68-90 saw a significant improvement only with an Ig class switch to dimeric or secretory IgA1. Additionally, conversion from an IgG1 to a dimeric IgA1 or IgA2 did not affect functional activity of HuMAb 67-102, but switching from dimeric to secretory IgA1 or IgA2 did significantly increase the in vitro activity of 67-102. Due to low expression yields, we were not able to generate sufficient 68-51 sIgA1 or sIgA2 for in vitro testing.
FIG 4.
Ig class switching of anti-CfaE MAbs, tested using the Caco-2 adhesion assay. The minimal effective IgG dose to prevent 50% (IC50) of bacterial adhesion to intestinal Caco-2 cells was used to determine antibody potency ranking. Error bars represent the standard deviation of results of three or four independent experiments. *, P < 0.01; **, P < 0.001; ***, P < 0.0001.
Anti-CfaE HuMAbs prevent ETEC colonization in the small intestine of a mouse model.
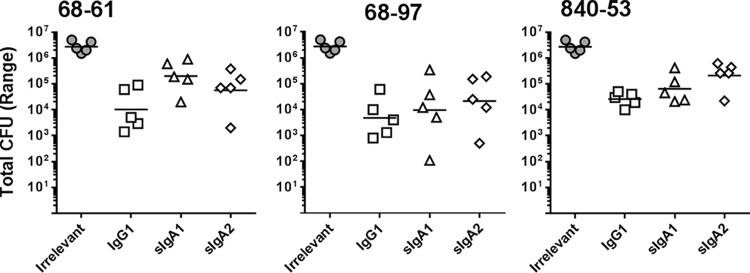
HuMAbs 68-61, 68-97, and 840-53 were found to have the lowest IC50s as IgG1, sIgA1, and sIgA2 and were selected as the leads for further characterization in animal studies (Fig. 5). Groups of five DBA/2 mice were given a mixture of bacteria and anti-CfaE HuMAbs (10 mg/kg of body weight) by oral gavage. At 24 h after challenge, the mice were euthanized and the CFU in the small intestine were counted as described in Materials and Methods. The efficacy of the anti-CfaE HuMAbs was assessed by determining whether the HuMAbs could prevent adhesion of bacteria to the small intestine, in comparison to an irrelevant isotype control. In the 68-61 group, treatment with IgG1 decreased the number of CFU by100-fold in comparison to the irrelevant antibody control. A similar result was observed for 68-61 treated with sIgA2 in comparison to the irrelevant control. The group of mice treated with 68-61 sIgA1 showed slightly higher CFU than the 68-61 IgG1 and sIgA2 groups. However, the differences were not significant. The reductions in CFU observed in the 68-97 group in comparison to the irrelevant control were similar across the different subclasses. In the 840-53 group, mice treated with IgG1 showed fewer bacteria than those treated with sIgA2, while those treated with sIgA1 also showed a decrease in the number of bacteria relative to those treated with sIgA2, though these differences were not significant.
FIG 5.
In vivo studies. DBA/2 mice were challenged intragastrically with 107 CFU preincubated with 10 mg/kg of HuMAbs. Animals were euthanized 24 h after challenge, and bacterial colonies in the small intestine were counted. Five animals were tested for each condition. Results for all the anti-CfaE HuMAbs were significantly different from those for the irrelevant MAb (P < 0.001).
DISCUSSION
Recent studies from our laboratory and others demonstrated the feasibility of using HuMAbs for preexposure prophylaxis against infectious diseases (22). A similar strategy could be used to prevent diarrhea disease caused by enteric pathogens such as ETEC. ETEC fimbrial adhesin subunits mediate adherence of the bacteria to the small intestine as the first step of a cascade of events leading to diarrhea. Studies in animal models and in human vaccine clinical trials have demonstrated that immunity against adhesion is sufficient to elicit effective protection against ETEC infection (16, 17). In the present study, we produced and characterized HuMAbs that recognize the N-terminal portion of CfaE (CfaE-N), the adhesin subunit involved in bacterial adhesion to host cells. Among the 300 isolated HuMAbs, 10 lead candidates were selected based on their ability to block mannose-resistant hemagglutination (MRHA) and to inhibit adhesion of ETEC to Caco-2 cells. When administered orally to mice by premixing with ETEC, the selected lead HuMAbs significantly decrease colony formation in the small intestine.
Structural analyses have revealed a positively charged binding pocket in the N-terminal domain of CfaE that is responsible for ETEC interaction with the negatively charged sialic acid of the host epithelial cells (shown as a red surface in Fig. 3H). The binding pocket is formed by three arginine residues, Arg67, Arg181, and Arg182, and a cluster of surrounding residues, which are all highly conserved among the class 5 fimbrial adhesins. Mutations of the arginine residues result in a complete loss of binding activity of ETEC to host cells (18). Putative antibody-antigen interaction models were established utilizing the sequences of CfaE (PDB ID 2HB0) and the anti-CfaE HuMAbs with the aid of an antibody modeling program (BioLuminate; Schrödinger). A set of residues predicted to be important for the binding interaction based on the top-ranked model were selected for experimental alanine scanning and were confirmed to be energetically critical using ELISA. HuMAbs 68-51 and 68-97, the antibodies with the highest in vitro functional activity, were found to bind directly to Arg67 (part of the putative receptor binding domain). Four more residues, Arg145, Thr91, Tyr183, and Asn127, located in the proximity of the receptor binding domain, were recognized by the other nine lead anti-CfaE HuMAbs (Fig. 3). Together, our data suggest that the protective HuMAbs are likely to be elicited by epitopes within or near the positively charged binding pocket. HuMAbs binding to ETEC, either directly to the putative receptor binding domain or its proximity region, may result in the blockage of ETEC and host cell interactions. Unfortunately, we did not identify any residues involved in the binding of HuMAb 68-75 to CfaE, for which a substitution different from alanine may be required in order to elucidate the location of the epitope recognized by this MAb.
The development of novel immunoprophylaxis to prevent disease depends on the availability of animal models that faithfully recapitulate the disease in humans. This is particularly the case for the development of immunoprophylaxis against ETEC, since the colonization factors are highly species specific. In a recent study, a neonatal mouse model using DBA/2 mice was reported to be effective in investigating an adhesin-based vaccine. A lethal dose was determined, and the pups were rescued by maternal vaccination or by oral administration of hyperimmune anti-CFA/I and anti-CfaE bovine colostral IgG (16). To evaluate the potency of lead HuMAbs, we have tried to established the same model described by Luiz et al. (16). However, maternal aggression and high rates of pup cannibalism limited our capability to successfully conduct the assay. Alternatively, we established an adult colonization mouse model using DBA/2 mice. Six-week-old mice were challenged with a nonlethal dose of ETEC that would lead to a consistent level of bacterial burden in the small intestine, as described in other studies (23, 24). The ability of HuMAb to inhibit the adherence of ETEC was measured as a reduction in colony count in comparison to an irrelevant isotype control.
IgG and sIgA are both present in the small intestine as effector molecules of the mucosal immune system. sIgA is considered to be one of the most important effector molecules because it constitutes the primary immune defense against pathogens at the mucosal surface (25). In secretory IgA, two IgA monomers are covalently linked by a joining chain (J chain) and stabilized by a polypeptide called the secretory component that makes the molecule more resistant to digestion in the small intestine than IgG (26). Early studies also have suggested that the secretory component may have its own antimicrobial activity to block epithelial adhesion of enterotoxigenic E. coli (27). To assess the functional differences between IgG and sIgA, three lead HuMAbs, 68-61, 840-53, and 68-97, were selected and class switched to IgA1 and IgA2 in both the dimeric and secretory forms. The antibody activities in vivo were generally well preserved after the class switch. Preincubation of bacteria with either the sIgA or IgG form led to a significant reduction in CFU in the small intestine in comparison to the irrelevant controls (P < 0.001). 68-61 and 840-53 IgG1 showed greater activity than their sIgA1 and sIgA2 forms, respectively, but the differences were not significant. No significant differences were observed in the 68-97 group. Overall, a class switch to sIgA did not show benefits over the IgG form, possibly due to the limitation of our methods to assess antibody efficacy. In particular, full-length immunoglobulin instead of a Fab fragment was used in our studies. We could not rule out the possibility of nonspecific effects of the Fc portion of the anti-CfaE antibodies that may cause aggregation of the bacteria prior to addition to the cells. In both cell adherence assays and mouse intestinal colonization assays, the bacteria preincubated with the IgG or IgA CfaE-specific antibodies might not have been in exactly the same state of aggregation when they were applied directly to the Caco2 cell monolayers or used to challenge the mice. To resolve the effect of potential aggregation caused by the Fc portion, future work could be conducted by testing the efficacy of the Fab portion of the immunoglobulin (13).
In conclusion, we identified a panel of HuMAbs that potently inhibit ETEC binding to intestinal epithelial cells in vitro and in vivo. Additional preclinical studies are planned to demonstrate the safety and efficacy in an Aotus monkey model with ETEC challenge (28, 29). To date, over 25 human-specific ETEC colonization factor antigen (CFA) types have been described, and most CFAs are fimbrial proteins (30). Eight common fimbriae (CFA/I, CS4, CS14, CS1, CS17, CS19, PCF071, and CS2) belonging to class 5 are expressed by pathogenic strains that cause the majority of moderate to severe ETEC diarrheal cases (13, 14, 31). Anti-CfaE monoclonal antibodies have been previously shown to cross-react and cross-protect with heterologous CFAs of the class 5 fimbriae (32). For this reason, further investigation is needed to explore the cross-protectivity of the anti-CfaE HuMAb against heterologus CFA ETEC strains. In the absence of a vaccine for ETEC, our study provides the first proof of concept that oral administration of protective antibody could potentially be an effective strategy for prophylaxis against ETEC.
MATERIALS AND METHODS
ETEC test strains.
H10407 expressing CFA/I fimbriae was purchased from ATCC (ATCC 35401). ETEC strain H10407 was cultured on 2% agar containing 1% Casamino Acids (Sigma) and 0.15% yeast extract (Fisher Bioreagents) plus 0.005% MgSO4 (Sigma) and 0.0005% MnCl2 (Sigma) (CFA agar plates) overnight at 37°C. A total of 1 × 108 CFU/ml were resuspended in 20% glycerol (Sigma) in phosphate-buffered saline (PBS) solution and kept frozen at −80°C until needed.
Antigen cloning, expression, and purification.
The nucleic acid sequences of N-terminal adhesin domains of CfaE (GenBank M55661) was cloned into a pMAL-C5X vector (Addgene) in-frame with an MBP tag to express as periplasmic proteins with improved solubility (MBP–CfaE-N).
The donor strand complement was included to ensure the overall protein expression and stability, as reported previously (33). All cloned constructs were transformed into SHuffleT7 Competent Escherichia coli (NEB), and expression was induced with 1 mM IPTG (isopropyl-β-d-thiogalactopyranoside). Bacteria were lysed, and proteins were purified with amylose resin (NEB) and eluted with 20 and 50 mM maltose (Sigma).
Mouse immunization, hybridoma generation, and antibody cloning.
Transgenic mice containing human immunoglobulin genes and inactivated mouse heavy chain and κ light chain genes (Bristol-Myers Squibb) were immunized with 50 μg of MBP–CfaE-N weekly with the Sigma adjuvant system (Sigma) for 6 to 10 weeks. The anti-CfaE titer in mouse serum was measured by enzyme-linked immunosorbent assay (ELISA). Hybridomas were generated following a standard polyethylene glycol (PEG) fusion protocol (22). Hybridoma supernatants were screened for reactivity to MBP–CfaE-N, and positive cell clones were selected for antibody sequencing. The heavy chain and light chain variable regions were amplified from hybridoma cells and cloned into two pcDNA 3.1 (Thermo Fisher) vectors containing κ light chain constant region and IgG1 heavy chain constant region, respectively, as previously described (22).
IgA class switching.
Primers were designed to amplify the variable heavy chain of each IgG antibody, and products were digested and ligated into a pcDNA 3.1 vector containing heavy constant IgA1 and IgA2 chains. Each vector was transformed in NEB5-α competent cells, and sequences were verified ahead of transient transfection. In order to get dimeric IgA, the heavy and light chain vectors were cotransfected with pcDNA-containing DNA for the connecting J chain using an ExpiCHO expression system (Life Technology). For secretory IgA expression, a pcDNA-containing secretory component was added to the transfection reaction in a 1:1 ratio. Supernatant was run through a column of CaptoL resin to capture the light chains of antibodies (GE Life Sciences). Antibodies were dialyzed against phosphate-buffered saline before being moved into size exclusion chromatography to separate out the desired dimeric or secretory antibodies using a HiLoad 26/600 Superdex 200-pg size exclusion column (GE Healthcare Life Sciences). The desired fractions were pooled, concentrated, and quality tested by SDS-PAGE and Western blotting (see Fig. S1 in the supplemental material).
ELISA.
For binding activity of purified HuMAbs against CfaE, 96-well plates (Nunc) were coated overnight at 4°C with 2 μg/ml of purified MBP–CfaE-N. The plates were blocked with 1% BSA plus 0.05% Tween 20 in PBS. Purified HuMAbs were diluted in 1× PBS plus 0.1% Tween 20 and added to the plates for 1 h. The plates were stained with alkaline phosphatase-conjugated goat anti-human IgG Fcγ (Jackson ImmunoResearch Laboratories) (1:1,000) for 1 h and developed using p-nitrophenyl phosphate (ThermoFisher Scientific). Absorbance at an optical density at 405 nm (OD405) was measured on an Emax precision plate reader (Molecular Devices).
SPR analysis.
Surface plasmon resonance (SPR) technology was used to assess the binding properties of the HuMAbs (Biacore T200 instrument; GE Healthcare). A total of 2,700 response units (RU) of anti-human IgG MAb (human antibody capture kit; GE Healthcare) was coupled to a CM5 sensor chip using standard amine coupling chemistry. In multicycle kinetics experiments, 25 to100 RU of each anti-CfaE HuMAb was captured on the anti-human IgG MAb-bound sensor chip. Various concentrations of soluble recombinant MBP–CfaE-N antigen ranging from 1.56 nM to 50 nM were injected over the chip surface at a flow rate of 30 μl/min. An association step of 60 s was followed by a dissociation step of 180 s, and the final dissociation step was 600 s. Regeneration of the sensor chip surface was accomplished using 3 M MgCl2. Experiments were performed at 25°C. Kinetic data were analyzed using Biacore T200 Evaluation (version 3.0) software and a 1:1 binding model. All chemicals for the Biacore experiment were purchased from GE Healthcare.
Flow cytometry.
Binding of the HuMAbs to the surface of live bacteria was measured by flow cytometry as described previously (34). H10407, which expresses the target CFA/I antigen, was used as the test strain. Briefly, bacteria were grown in CFA medium supplemented with 50 μM deferoxamine overnight at 37°C with gentle shaking (21). To measure HuMAb binding, a fixed concentration of anti-CfaE HuMAb (10 μg/ml) or, as a negative control, 100 μg/ml of an irrelevant MAb was incubated with 107 bacteria/ml. Bound antibody was detected using CF488-conjugated goat anti-human IgG (Biotium).
Mannose-resistant hemagglutination assay of human group A erythrocytes.
ETEC cultures were taken from frozen cell banks and diluted in a sterile 0.15 M saline solution until an OD600 of 1 was reached for the assay. Type A-positive human erythrocytes stored in K3EDTA were washed three times with 0.15 M saline solution and resuspended in the same solution to a final concentration of 1.5% (vol/vol). In a U-bottom 96-well plate (Nunc Thermo Scientific), 100 μl of HuMAb was added in duplicate to the top row and diluted 1:2 down the plate in a 0.15 M saline solution. Fifty microliters of appropriately diluted ETEC was added to each well together with 50 μl of a 0.1 M d-mannose solution (sigma). The plate was incubated for 10 min at room temperature. After incubation, 50 μl of blood solution was added to the plate and mixed well (200 μl final volume). Plates were allowed to sit stagnant at 4°C for 2 h. Hemagglutination was then observed without the aid of magnification. The absence of a pellet of erythrocytes at the bottom of the well is indicative of positive hemagglutination. Blood was ordered fresh every week (BioreclamationIVT).
Caco-2 adhesion assay.
Caco-2 cells seeded at 1 × 105 cells/ml were grown in 24-well tissue culture plates containing Dulbecco's modified Eagle's medium (DMEM), at 37°C in 5% CO2 statically. Frozen bacterial banks were streaked on CFA agar plates and grown overnight at 37°C. The next day, bacteria were resuspended in PBS and diluted until an OD600 nm of 0.1 was reached. HuMAb dilutions were set up in a deep well plate. Antibody dilutions and bacteria were combined at a 1:10 ratio and allowed to shake at 300 rpm for 1 h at room temperature. After incubation, 0.2 ml of the mixture of antibody and bacteria was added to each well containing Caco-2 cells. The cells were then incubated statically for 3 h at 37°C. The cells were then washed four times with 1 ml PBS to remove nonadherent ETEC cells. Afterwards, Caco-2 cells were dislodged with 0.2 ml of 0.25% trypsin. Cells were collected via gentle centrifugation and resuspended in 1 ml PBS. Dilutions were plated on CFA agar plates, and colonies were counted the next day. IC50 was defined as the concentration of HuMAb needed to inhibit 50% of ETEC adhesion to the Caco-2 cells, compared to an irrelevant isotype antibody.
Animal assays.
Six- to 8-week-old DBA/2 mice were pretreated with streptomycin (5 g/liter) in the drinking water for 24 to 48 h. Twelve hours prior to bacterial administration, the water was replaced with regular drinking water. One hour prior to bacterial administration, mice received cimetidine (50 mg/kg) intraperitoneally to reduce the effect of stomach acid on ETEC. A total of 107 CFU of ETEC strain H10407 diluted in PBS were incubated with 10 mg/kg of an anti-CfaE HuMAb or an irrelevant MAb (purified human secretory IgA; MP Biomedicals) 1 h prior to challenge. Bacteria and HuMAbs were administered in a 200-μl volume by oral gavage using 20-gauge bulb-tip feeding needles. The mice were allowed to survive for 24 h. At 12 h before euthanasia, food was withdrawn. Following isolation of the small intestine, two segments of ileum (3 cm each), beginning within 0.5 cm of the ileocecal junction and extending proximally 6 cm, were removed and placed in 1 ml sterile PBS (23). Tissues were mechanically homogenized. Samples were serially diluted on MacConkey agar plates and incubated overnight at 37°C. Bacterial CFU were counted the next day. To confirm that recovered bacteria were the inoculum strain, bacterial colonies grown on culture plates were routinely tested by PCR using specific primers (23) which flank the eltAB operon encoding the LT holotoxin of H10407.
Epitope mapping.
BioLuminate software (Schrödinger) was used to identify CfaE residues involved in antibody-antigen recognition. A total of 22 amino acids predicted by the software to be involved in the interaction between anti-CfaE HuMAbs and the N-terminal portion of CfaE were individually mutated to alanine using the BioXp 3200 system (SGI-DNA). The genes were cloned into pMAL-C5x vector, and the resulting 22 constructs were transformed, expressed, and purified as described above. An ELISA was performed to determine binding of the HuMAbs to the mutant proteins in comparison to that to the wild type.
Statistical analysis.
Statistical calculations were performed using the software Prism version 7.03 (GraphPad Software, La Jolla, CA). Comparisons between the hemagglutination or Caco-2 titers of respective antibodies were performed using multiple comparisons, the Bonferroni test, and one-way analysis of variance (ANOVA).
Supplementary Material
ACKNOWLEDGMENTS
This work was supported by the Defense Advanced Research Project Agency (DARPA-BAA-13-03) and the Bill & Melinda Gates Foundation (OPP1173647).
Footnotes
Supplemental material for this article may be found at https://doi.org/10.1128/IAI.00355-18.
REFERENCES
- 1.Bourgeois AL, Wierzba TF, Walker RI. 2016. Status of vaccine research and development for enterotoxigenic Escherichia coli. Vaccine 34:2880–2886. doi: 10.1016/j.vaccine.2016.02.076. [DOI] [PubMed] [Google Scholar]
- 2.Evans DJ Jr, Evans DG. 1996. Escherichia coli in diarrheal disease. In Baron S. (ed), Medical microbiology, 4th ed University of Texas Medical Branch at Galveston, Galveston, TX. [PubMed] [Google Scholar]
- 3.Oh KH, Kim DW, Jung SM, Cho SH. 2014. Molecular characterization of enterotoxigenic Escherichia coli strains isolated from diarrheal patients in Korea during 2003-2011. PLoS One 9:e96896. doi: 10.1371/journal.pone.0096896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ochoa TJ, Ecker L, Barletta F, Mispireta ML, Gil AI, Contreras C, Molina M, Amemiya I, Verastegui H, Hall ER, Cleary TG, Lanata CF. 2009. Age-related susceptibility to infection with diarrheagenic Escherichia coli among infants from periurban areas in Lima, Peru. Clin Infect Dis 49:1694–1702. doi: 10.1086/648069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Estrada-Garcia T, Cerna JF, Paheco-Gil L, Velazquez RF, Ochoa TJ, Torres J, DuPont HL. 2005. Drug-resistant diarrheogenic Escherichia coli, Mexico. Emerg Infect Dis 11:1306–1308. doi: 10.3201/eid1108.050192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Madhavan TP, Sakellaris H. 2015. Colonization factors of enterotoxigenic Escherichia coli. Adv Appl Microbiol 90:155–197. doi: 10.1016/bs.aambs.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 7.Sears CL, Kaper JB. 1996. Enteric bacterial toxins: mechanisms of action and linkage to intestinal secretion. Microbiol Rev 60:167–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ruan X, Robertson DC, Nataro JP, Clements JD, Zhang W, STa Toxoid Vaccine Consortium Group . 2014. Characterization of heat-stable (STa) toxoids of enterotoxigenic Escherichia coli fused to double mutant heat-labile toxin peptide in inducing neutralizing anti-STa antibodies. Infect Immun 82:1823–1832. doi: 10.1128/IAI.01394-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang W, Zhang C, Francis DH, Fang Y, Knudsen D, Nataro JP, Robertson DC. 2010. Genetic fusions of heat-labile (LT) and heat-stable (ST) toxoids of porcine enterotoxigenic Escherichia coli elicit neutralizing anti-LT and anti-STa antibodies. Infect Immun 78:316–325. doi: 10.1128/IAI.00497-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Czerkinsky C, Holmgren J. 2010. Topical immunization strategies. Mucosal Immunol 3:545–555. doi: 10.1038/mi.2010.55. [DOI] [PubMed] [Google Scholar]
- 11.McArthur MA, Maciel M Jr, Pasetti MF. 2017. Human immune responses against Shigella and enterotoxigenic E. coli: current advances and the path forward. Vaccine 35:6803–6806. doi: 10.1016/j.vaccine.2017.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Walker RI, Wierzba TF, Mani S, Bourgeois AL. 2017. Vaccines against Shigella and enterotoxigenic Escherichia coli: a summary of the 2016 VASE Conference. Vaccine 35:6775–6782. doi: 10.1016/j.vaccine.2017.09.045. [DOI] [PubMed] [Google Scholar]
- 13.Anantha RP, McVeigh AL, Lee LH, Agnew MK, Cassels FJ, Scott DA, Whittam TS, Savarino SJ. 2004. Evolutionary and functional relationships of colonization factor antigen i and other class 5 adhesive fimbriae of enterotoxigenic Escherichia coli. Infect Immun 72:7190–7201. doi: 10.1128/IAI.72.12.7190-7201.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Qadri F, Svennerholm AM, Faruque AS, Sack RB. 2005. Enterotoxigenic Escherichia coli in developing countries: epidemiology, microbiology, clinical features, treatment, and prevention. Clin Microbiol Rev 18:465–483. doi: 10.1128/CMR.18.3.465-483.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Qadri F, Das SK, Faruque AS, Fuchs GJ, Albert MJ, Sack RB, Svennerholm AM. 2000. Prevalence of toxin types and colonization factors in enterotoxigenic Escherichia coli isolated during a 2-year period from diarrheal patients in Bangladesh. J Clin Microbiol 38:27–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Luiz WB, Rodrigues JF, Crabb JH, Savarino SJ, Ferreira LC. 2015. Maternal vaccination with a fimbrial tip adhesin and passive protection of neonatal mice against lethal human enterotoxigenic Escherichia coli challenge. Infect Immun 83:4555–4564. doi: 10.1128/IAI.00858-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Savarino SJ, McKenzie R, Tribble DR, Porter CK, O'Dowd A, Cantrell JA, Sincock SA, Poole ST, DeNearing B, Woods CM, Kim H, Grahek SL, Brinkley C, Crabb JH, Bourgeois AL. 2017. Prophylactic efficacy of hyperimmune bovine colostral antiadhesin antibodies against enterotoxigenic Escherichia coli diarrhea: a randomized, double-blind, placebo-controlled, phase 1 trial. J Infect Dis 216:7–13. doi: 10.1093/infdis/jix144. [DOI] [PubMed] [Google Scholar]
- 18.Li YF, Poole S, Rasulova F, McVeigh AL, Savarino SJ, Xia D. 2007. A receptor-binding site as revealed by the crystal structure of CfaE, the colonization factor antigen I fimbrial adhesin of enterotoxigenic Escherichia coli. J Biol Chem 282:23970–23980. doi: 10.1074/jbc.M700921200. [DOI] [PubMed] [Google Scholar]
- 19.Baker KK, Levine MM, Morison J, Phillips A, Barry EM. 2009. CfaE tip mutations in enterotoxigenic Escherichia coli CFA/I fimbriae define critical human intestinal binding sites. Cell Microbiol 11:742–754. doi: 10.1111/j.1462-5822.2009.01287.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hagberg LU, Jodal U, Korhonen TK, Lidin-Janson G, Lindberg U, Svanborg Eden C. 1981. Adhesion, hemagglutination, and virulence of Escherichia coli causing urinary tract infections. Infect Immun 31:564–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Haines S, Arnaud-Barbe N, Poncet D, Reverchon S, Wawrzyniak J, Nasser W, Renauld-Mongenie G. 2015. IscR regulates synthesis of colonization factor antigen I fimbriae in response to iron starvation in enterotoxigenic Escherichia coli. J Bacteriol 197:2896–2907. doi: 10.1128/JB.00214-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang Y, Kern A, Boatright NK, Schiller ZA, Sadowski A, Ejemel M, Souders CA, Reimann KA, Hu L, Thomas WD Jr, Klempner MS. 2016. Pre-exposure prophylaxis with OspA-specific human monoclonal antibodies protects mice against tick transmission of Lyme disease spirochetes. J Infect Dis 214:205–211. doi: 10.1093/infdis/jiw151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Allen KP, Randolph MM, Fleckenstein JM. 2006. Importance of heat-labile enterotoxin in colonization of the adult mouse small intestine by human enterotoxigenic Escherichia coli strains. Infect Immun 74:869–875. doi: 10.1128/IAI.74.2.869-875.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Albert MJ, Haridas S, Ebenezer M, Raghupathy R, Khan I. 2015. Immunization with a double-mutant (R192G/L211A) of the heat-labile enterotoxin of Escherichia coli offers partial protection against Campylobacter jejuni in an adult mouse intestinal colonization model. PLoS One 10:e0142090. doi: 10.1371/journal.pone.0142090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brandtzaeg P. 2007. Induction of secretory immunity and memory at mucosal surfaces. Vaccine 25:5467–5484. doi: 10.1016/j.vaccine.2006.12.001. [DOI] [PubMed] [Google Scholar]
- 26.Stelwagen K, Carpenter E, Haigh B, Hodgkinson A, Wheeler TT. 2009. Immune components of bovine colostrum and milk. J Anim Sci 87:3–9. doi: 10.2527/jas.2008-1377. [DOI] [PubMed] [Google Scholar]
- 27.Brandtzaeg P. 2003. Mucosal immunity: integration between mother and the breast-fed infant. Vaccine 21:3382–3388. doi: 10.1016/S0264-410X(03)00338-4. [DOI] [PubMed] [Google Scholar]
- 28.Sincock SA, Hall ER, Woods CM, O'Dowd A, Poole ST, McVeigh AL, Nunez G, Espinoza N, Miller M, Savarino SJ. 2016. Immunogenicity of a prototype enterotoxigenic Escherichia coli adhesin vaccine in mice and nonhuman primates. Vaccine 34:284–291. doi: 10.1016/j.vaccine.2015.11.017. [DOI] [PubMed] [Google Scholar]
- 29.Jones FR, Hall ER, Tribble D, Savarino SJ, Cassels FJ, Porter C, Meza R, Nunez G, Espinoza N, Salazar M, Luckett R, Scott D. 2006. The New World primate, Aotus nancymae, as a model for examining the immunogenicity of a prototype enterotoxigenic Escherichia coli subunit vaccine. Vaccine 24:3786–3792. doi: 10.1016/j.vaccine.2005.07.029. [DOI] [PubMed] [Google Scholar]
- 30.Begum YA, Baby NI, Faruque AS, Jahan N, Cravioto A, Svennerholm AM, Qadri F. 2014. Shift in phenotypic characteristics of enterotoxigenic Escherichia coli (ETEC) isolated from diarrheal patients in Bangladesh. PLoS Negl Trop Dis 8:e3031. doi: 10.1371/journal.pntd.0003031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Isidean SD, Riddle MS, Savarino SJ, Porter CK. 2011. A systematic review of ETEC epidemiology focusing on colonization factor and toxin expression. Vaccine 29:6167–6178. doi: 10.1016/j.vaccine.2011.06.084. [DOI] [PubMed] [Google Scholar]
- 32.Rudin AM, Svennerholm A. 1994. Monoclonal antibodies against enterotoxigenic Escherichia coli colonization factor antigen I (CFA/I) that cross-react immunologically with heterologous CFAs. Infect Immun 62:4339–4346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Poole ST, McVeigh AL, Anantha RP, Lee LH, Akay YM, Pontzer EA, Scott DA, Bullitt E, Savarino SJ. 2007. Donor strand complementation governs intersubunit interaction of fimbriae of the alternate chaperone pathway. Mol Microbiol 63:1372–1384. doi: 10.1111/j.1365-2958.2007.05612.x. [DOI] [PubMed] [Google Scholar]
- 34.Giuntini S, Granoff DM, Beernink PT, Ihle O, Bratlie D, Michaelsen TE. 2016. Human IgG1, IgG3, and IgG3 hinge-truncated mutants show different protection capabilities against meningococci depending on the target antigen and epitope specificity. Clin Vaccine Immunol 23:698–706. doi: 10.1128/CVI.00193-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.