Abstract
Importance
Tracheal intubation is common during adult in-hospital cardiac arrest, but little is known about the association between tracheal intubation and survival in this setting.
Objective
To determine whether tracheal intubation during adult in-hospital cardiac arrest is associated with survival to hospital discharge.
Design, Setting, and Participants
Observational cohort study of adult patients who had an in-hospital cardiac arrest from January 2000 through December 2014 included in the Get With The Guidelines–Resuscitation registry, a US-based multicenter registry of in-hospital cardiac arrest. Patients who had an invasive airway in place at the time of cardiac arrest were excluded. Patients intubated at any given minute (from 0-15 minutes) were matched with patients at risk of being intubated within the same minute (ie, still receiving resuscitation) based on a time-dependent propensity score calculated from multiple patient, event, and hospital characteristics.
Exposure
Tracheal intubation during cardiac arrest.
Main Outcomes and Measures
The primary outcome was survival to hospital discharge. Secondary outcomes included return of spontaneous circulation (ROSC) and a good functional outcome. A cerebral performance category score of 1 (mild or no neurological deficit) or 2 (moderate cerebral disability) was considered a good functional outcome.
Results
The propensity-matched cohort was selected from 108 079 adult patients at 668 hospitals. The median age was 69 years (interquartile range, 58-79 years), 45 073 patients (42%) were female, and 24 256 patients (22.4%) survived to hospital discharge. Of 71 615 patients (66.3%) who were intubated within the first 15 minutes, 43 314 (60.5%) were matched to a patient not intubated in the same minute. Survival was lower among patients who were intubated compared with those not intubated: 7052 of 43 314 (16.3%) vs 8407 of 43 314 (19.4%), respectively (risk ratio [RR] = 0.84; 95%CI, 0.81-0.87; P < .001). The proportion of patients with ROSC was lower among intubated patients than those not intubated: 25 022 of 43 311 (57.8%) vs 25 685 of 43 310 (59.3%), respectively (RR = 0.97; 95%CI, 0.96-0.99; P < .001). Good functional outcome was also lower among intubated patients than those not intubated: 4439 of 41 868 (10.6%) vs 5672 of 41 733 (13.6%), respectively (RR = 0.78; 95%CI, 0.75-0.81; P < .001). Although differences existed in prespecified subgroup analyses, intubation was not associated with improved outcomes in any subgroup.
Conclusions and Relevance
Among adult patients with in-hospital cardiac arrest, initiation of tracheal intubation within any given minute during the first 15 minutes of resuscitation, compared with no intubation during that minute, was associated with decreased survival to hospital discharge. Although the study design does not eliminate the potential for confounding by indication, these findings do not support early tracheal intubation for adult in-hospital cardiac arrest.
Mortality after adult in-hospital cardiac arrest remains high, and little is known about the effect of most interventions during cardiac arrest, including drugs and the use of advanced airway management.1 Since 2010, guidelines have deemphasized the importance of tracheal intubation during cardiac arrest in adults, and the most optimal approach to airway management during cardiac arrest remainsunknown.1 The 2015 guidelines of both the American Heart Association and the European Resuscitation Council state that either a bag-valve-mask device or an advanced airway may be used for ventilation and oxygenation during cardiac arrest, and the guidelines make no distinction between the out-of-hospital and in-hospital setting.2,3
A large Japanese observational study of out-of-hospital cardiac arrest showed that advanced airway management was associated with a decreased chance of good outcome.4 However, similar data are lacking for the in-hospital setting, where patient characteristics, the cause of cardiac arrest, the timing of interventions, the skills and experience of the health care professionals, and overall outcomes are significantly different.1,5
The aim of the current study was to evaluate the association between tracheal intubation during adult in-hospital cardiac arrest and survival to hospital discharge using the multicenter Get With The Guidelines–Resuscitation (GWTG-R) registry. This study also aimed to assess whether this association was modified by the first documented rhythm (shockable vs nonshockable) or other patient and event factors explored in prespecified subgroups.
Methods
Data Source
This study retrospectively analyzed data from the GWTG-R registry, a prospective quality improvement registry of in hospital cardiac arrest in US hospitals; the registry is sponsored by the American Heart Association, which has regimented data collection methods and reliability checks.6 Data are collected on all patients with in-hospital cardiac arrest who do not have prior do-not-resuscitate orders. Cardiac arrest is defined as pulselessness requiring chest compressions and/or defibrillation, with a hospital-wide or unit-based emergency response. Integrity of the data is ensured through online certification of data entry personnel and the use of standardized software.7 Data from January 1, 2000, through December 31, 2014, were used. Hospital-level data were obtained from the American Hospital Association's Annual Survey from 2013.8
All participating hospitals are required to comply with local regulatory guidelines. Because data are used primarily at the local site for quality improvement, sites are granted a waiver of informed consent under the common rule. The Committee on Clinical Investigations at Beth Israel Deaconess Medical Center confirmed that this is not considered human subjects research under the common law and therefore waived the need for informed consent.
Patient Population
This study included adult patients (aged ≥ 18 years) with an index cardiac arrest for which they received chest compressions. Patients who had an invasive airway in place at the time of the cardiac arrest (including tracheal tube, tracheostomy, laryngeal mask airway, or other invasive airways but not including nasopharyngeal or oropharyngeal airways) were not included. Hospital visitors and employees were not included. For the main analysis, patients with missing data on tracheal intubation, covariates (except race, for which a “not reported” category was created), and survival were excluded. This included patients with missing or inconsistent data on timing of tracheal intubation, timing of epinephrine administration, or timing of defibrillation (in those with a shockable rhythm). These patients were included after imputation of missing values in a preplanned sensitivity analysis (see “Statistical Analysis”).
Race was included in the analysis because previous research has suggested that race might be associated with outcomes.9 Race was self-reported by the patient or family or, if these were not available, by the clinical physician or institution. Race was reported as American Indian/Alaska Native, Asian, black or African American, Native Hawaiian/Pacific Islander, white, or unable to determine. Given small sample sizes in some groups, these were recategorized into white, black, other, and not reported.
Tracheal Intubation
Tracheal intubation was defined as insertion of a tracheal or tracheostomy tube during the cardiac arrest. The end of the cardiac arrest was when the patient had return of spontaneous circulation (ROSC) or when resuscitation was terminated without ROSC. Unsuccessful intubation attempts are not registered as intubations in the registry. The time to tracheal intubation was defined as the interval in whole minutes from loss of pulses until the tracheal tube was inserted. All times in the GWTG-R registry are collected in whole minutes. As such, a time to tracheal intubation of 0 minutes indicates that the tracheal intubation was performed within the same whole minute that pulses were lost, a time of 1 minute indicates that tracheal intubation was performed within the next whole minute, and so on.
Outcomes
The primary outcome was survival to hospital discharge. Secondary outcomes were ROSC and favorable functional outcome at hospital discharge. ROSC was defined as no further need for chest compressions (including cardiopulmonary bypass) sustained for at least 20 minutes. A cerebral performance category score of 1 (mild or no neurological deficit) or 2 (moderate cerebral disability) was considered a good functional outcome consistent with current Utstein guidelines.10 The cerebral performance category score was determined by data abstractors reviewing the medical record. Abstractors assessing outcomes were not blinded to exposure status but were unaware of the hypothesis of the current study.
Statistical Analysis
The statistical analysis plan for the current study largely follows that of a recent, similar GWTG-R study in children.11 Categorical variables are presented as counts (frequencies), and continuous variables are presented as medians (interquartile ranges [IQRs]). Independent categorical variables were compared with the χ2 test, and the Cochran-Armitage test was used to test for trends in tracheal intubation over time.
To assess the adjusted association between tracheal intubation during cardiac arrest and survival to hospital discharge, this study used time-dependent propensity scorematching.12 This approach has previously been used in studies analyzing time-dependent cardiac arrest interventions,11,13 and it is designed to account for the fact that the intubation procedure might not occur during the cardiac arrest if ROSC or termination of efforts occurs first. The propensity score was calculated based on a Cox proportional hazards model with intubation during the cardiac arrest as the dependent variable and with all variables included in Table 1 as independent variables. Additional details are provided in the eAppendix in the Supplement.
Table 1. Patient, Hospital, and Event Characteristics Among Patients With In-Hospital Cardiac Arrest Without vs With Intubation in the First 15 Minutes of Resuscitation in the Full Cohort.
| Characteristic | Patients, No. (%) | ||
|---|---|---|---|
| Total (N = 108 079) | No Intubation (n = 36 464) | Intubation (n = 71 615) | |
| Patient Characteristics | |||
| Demographic | |||
| Age, median (IQR), y | 69 (58-79) | 68 (56-78) | 70 (59-80) |
| Sex | |||
| Male | 63 006 (58) | 21 047 (58) | 41 959 (59) |
| Female | 45 073 (42) | 15 417 (42) | 29 656 (41) |
| Race | |||
| White | 76 731 (71) | 26 208 (72) | 50 523 (71) |
| Black | 21 517 (20) | 6836 (19) | 14 681 (21) |
| Other | 3398 (3) | 1148 (3) | 2250 (3) |
| Not reported | 6433 (6) | 2272 (6) | 4161 (6) |
| Illness category | |||
| Medical | |||
| Cardiac | 40 565 (38) | 15 032 (41) | 25 533 (36) |
| Noncardiac | 48 318 (45) | 14 856 (41) | 33 462 (47) |
| Surgical | |||
| Cardiac | 6049 (6) | 2383 (7) | 3666 (5) |
| Noncardiaca | 11 315 (10) | 3414 (9) | 7901 (11) |
| Trauma | 1832 (2) | 779 (2) | 1053 (1) |
| Preexisting conditionb | |||
| Cardiac | |||
| History of myocardial infarction | 18 204 (17) | 5830 (16) | 12 374 (17) |
| Myocardial infarction this admission | 17 477 (16) | 6520 (18) | 10 957 (15) |
| History of heart failure | 24 830 (23) | 7784 (21) | 17 046 (24) |
| Heart failure this admission | 19 446 (18) | 6218 (17) | 13 228 (18) |
| Noncardiac | |||
| Respiratory insufficiency | 37 474 (35) | 12 951 (36) | 24 523 (34) |
| Diabetes mellitus | 35 075 (32) | 11 081 (30) | 23 994 (34) |
| Renal insufficiency | 36 334 (34) | 11 507 (32) | 24 827 (35) |
| Metastatic or hematologic malignancy | 13 572 (13) | 4226 (12) | 9346 (13) |
| Hypotension or hypoperfusion | 22 135 (20) | 7863 (22) | 14 272 (20) |
| Pneumonia | 13 456 (12) | 4524 (12) | 8932 (12) |
| Baseline depression in CNS function | 11 312 (10) | 3559 (10) | 7753 (11) |
| Metabolic or electrolyte abnormality | 15 696 (15) | 5223 (14) | 10 473 (15) |
| Septicemia | 14 516 (13) | 5204 (14) | 9312 (13) |
| Acute CNS nonstroke event | 6796 (6) | 2205 (6) | 4591 (6) |
| Hepatic insufficiency | 7031 (7) | 2273 (6) | 4758 (7) |
| Acute stroke | 4095 (4) | 1343 (4) | 2752 (4) |
| Major trauma | 2623 (2) | 1111 (3) | 1512 (2) |
| Hospital Characteristics | |||
| Bed size, No. | |||
| 1-249 | 20 083 (19) | 7011 (19) | 13 072 (18) |
| 250-499 | 42 853 (40) | 13 949 (38) | 28 904 (40) |
| ≥500 | 45 143 (42) | 15 504 (43) | 29 639 (41) |
| Teaching status | |||
| Major | 37 409 (35) | 13 274 (36) | 24 135 (34) |
| Minor | 33 054 (31) | 10 912 (30) | 22 142 (31) |
| Nonteaching | 37 616 (35) | 12 278 (34) | 25 338 (35) |
| Ownership | |||
| Military | 2218 (2) | 774 (2) | 1444 (2) |
| Nonprofit | 77 690 (72) | 26 076 (72) | 51 614 (72) |
| Government | 16 322 (15) | 5738 (16) | 10 584 (15) |
| Private | 11 849 (11) | 3876 (11) | 7973 (11) |
| Location | |||
| Rural | 5774 (5) | 1928 (5) | 3846 (5) |
| Urban | 102 305 (95) | 34 536 (95) | 67 769 (95) |
| Geographical location | |||
| Northeast | 15 190 (14) | 5214 (14) | 9976 (14) |
| Southeast | 32 372 (30) | 10 592 (29) | 21 780 (30) |
| Midwest | 22 856 (21) | 7696 (21) | 15 160 (21) |
| South central | 22 069 (20) | 7244 (20) | 14 825 (21) |
| West | 15 592 (14) | 5718 (16) | 9874 (14) |
| In-Hospital Cardiac Arrest Characteristics | |||
| Year of cardiac arrest | |||
| 2000-2002 | 9973 (9) | 2707 (7) | 7266 (10) |
| 2003-2004 | 15 522 (14) | 4271 (12) | 11 251 (16) |
| 2005-2006 | 16 057 (15) | 4701 (13) | 11 356 (16) |
| 2007-2008 | 16 154 (15) | 5365 (15) | 10 789 (15) |
| 2009-2010 | 15 058 (14) | 5486 (15) | 9572 (13) |
| 2011-2012 | 16 418 (15) | 6702 (18) | 9716 (14) |
| 2013-2014 | 18 897 (17) | 7232 (20) | 11 665 (16) |
| In place at time of cardiac arrest | |||
| Noninvasive assisted ventilation | 11 117 (10) | 8164 (22) | 2953 (4) |
| Dialysisc | 2912 (3) | 944 (3) | 1968 (3) |
| Implantable cardiac defibrillator | 1913 (2) | 539 (1) | 1374 (2) |
| Intra-arterial catheter | 4485 (4) | 2209 (6) | 2276 (3) |
| Electrocardiogram | 80 864 (75) | 30 069 (82) | 50 795 (71) |
| Pulse oximeter | 62 634 (58) | 24 678 (68) | 37 956 (53) |
| Vasoactive agentsd | 16 056 (15) | 7822 (21) | 8234 (12) |
| Antiarrhythmic agentse | 3348 (3) | 1641 (5) | 1707 (2) |
| Location | |||
| Emergency department | 10 965 (10) | 3695 (10) | 7270 (10) |
| Floor with telemetry | 22 215 (21) | 6243 (17) | 15 972 (22) |
| Floor without telemetry | 27 249 (25) | 6091 (17) | 21 158 (30) |
| Intensive care unit | 38 547 (36) | 17 398 (48) | 21 149 (30) |
| OR, PACU, or interventional unit | 6471 (6) | 2289 (6) | 4182 (6) |
| Otherf | 2632 (2) | 748 (2) | 1882 (3) |
| Time of day | |||
| Day, 7:00 AM to 10:59 PM | 72 547 (67) | 24 853 (68) | 47 694 (67) |
| Night, 11:00 PM to 6:59 AM | 35 532 (33) | 11 611 (32) | 23 921 (33) |
| Day | |||
| Weekday, Monday 7 AM to Friday 11 PM | 74 578 (69) | 25 209 (69) | 49 369 (69) |
| Weekend, Friday 11 PM to Monday 7 AM | 33 501 (31) | 11 255 (31) | 22 246 (31) |
| Hospital-wide cardiac arrest response activated | 89 561 (83) | 28 597 (78) | 60 964 (85) |
| Witnessed | 84 473 (78) | 30 788 (84) | 53 685 (75) |
| First documented pulseless rhythm | |||
| Asystole | 39 119 (36) | 11 607 (32) | 27 512 (38) |
| Pulseless electrical activity | 49 630 (46) | 15 878 (44) | 33 752 (47) |
| Ventricular fibrillation | 12 569 (12) | 5522 (15) | 7047 (10) |
| Pulseless ventricular tachycardia | 6761 (6) | 3457 (9) | 3304 (5) |
| Time to compressions, min | |||
| 0 | 98 949 (92) | 33 648 (92) | 65 301 (91) |
| 1 | 4819 (4) | 1559 (4) | 3260 (5) |
| ≥2 | 4311 (4) | 1257 (3) | 3054 (4) |
| Epinephrine administration | 96 046 (89) | 27 737 (76) | 68 309 (95) |
| Time to epinephrine administration, median (IQR), min | 2 (0-5) | 1 (0-4) | 2 (1-5) |
| Defibrillationg | 17 479 (90) | 8019 (89) | 9460 (91) |
| Time to defibrillation, median (IQR), min | 1 (0-3) | 1 (0-2) | 2 (0-4) |
Abbreviations: CNS, central nervous system; IQR, interquartile range; OR, operating room; PACU, postanesthesia care unit.
Includes patients with an obstetric admission (n = 135).
See eTable 1 in the Supplement for definitions of preexisting conditions.
Hemodialysis or peritoneal dialysis, continuous arteriovenous dialysis, or venovenous hemofiltration or dialysis.
Dobutamine, dopamine (>3 μg/kg/min), epinephrine, nitroglycerin, norepinephrine, phenylephrine, vasopressin, and/or “other vasoactive agent(s).”
Continuous infusion of amiodarone, lidocaine, procainamide, and/or “other antiarrhythmic(s).”
Ambulatory and outpatient areas; delivery suite; rehabilitation, skilled nursing, and mental health facilities; same-day surgical areas; and “other.”
Includes only patients with a first documented pulseless rhythm of pulseless ventricular tachycardia or ventricular fibrillation.
Next, 1:1 risk set matching on the propensity score was performed using a nearest neighbor–matching algorithm with a maximum caliber of 0.01 of the propensity score. Patients being intubated at any given minute (from minute 0 to minute 15) were separately and sequentially propensity score matched with a patient who was at risk of being intubated within the same minute.11 At-risk patients included those who were still undergoing resuscitation and were not intubated before or within the same minute. At-risk patients therefore also included patients who were intubated later, as the matching should not be dependent on future events.11-14 As such, the matched group with no intubation includes patients who subsequently were intubated (although later than their matched counterpart). For additional details on the rationale for and interpretation of this type of analysis and matching, see the eAppendix in the Supplement.
To assess the performance of the matching, baseline characteristics were compared with standardized differences where a difference less than 0.1 is generally considered negligible.15 Using the matched cohort, modified Poisson regression was performed to assess the association between tracheal intubation during cardiac arrest and survival to hospital discharge, obtaining risk ratios (RRs) with robust variance estimates.16,17 To account for the matching and potential clustering within hospitals, generalized estimating equations were used as described by Miglioretti and Heagerty.18 Results are reported from the regression models as RRs with 95% confidence intervals. The analysis was repeated for the secondary outcomes.
This study tested whether the association between tracheal intubation and survival to hospital discharge differed according to a number of pre specified subgroups: initial rhythm (shockable [pulseless ventricular tachycardia or ventricular fibrillation] vs nonshockable [asystole or pulseless electrical activity]), timing of the matching (0-4, 5-9, and 10-15 minutes), illness category, whether the patient had preceding respiratory insufficiency (see eTable 1 in the Supplement for definition), and the location of the event. Subgroup differences were tested by adding an interaction between the intubation variable and the subgroup variable of interest to the modified Poisson regression model in the propensity-matched cohort. As a post hoc analysis, this study also considered the interaction when treating timing of the matching as a continuous linear variable. To account for missing data, multiple imputations were performed as described in thee Appendix in the Supplement. As a post hoc analysis, we used non–time-dependent propensity score matching (see the eAppendix in the Supplement for details).
All hypothesis tests were 2-sided, with a significance level of P < .05. All secondary analyses should be considered exploratory as no adjustments were made for multiple comparisons.19 Statistical analyses were conducted using SAS software version 9.4 (SAS Institute Inc). The statistical analysis plan was outlined and agreed on by the entire author group before any analyses were performed unless stated otherwise.
Results
Patient Characteristics
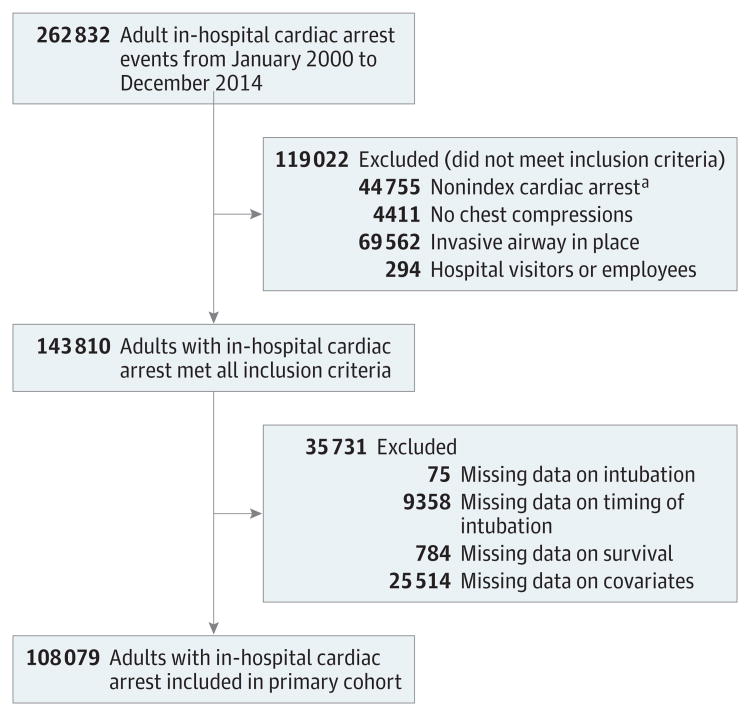
The study population included 108079 patients (Figure 1) from 668 hospitals. Baseline characteristics in the overall group and according to intubation are provided in Table 1. The median age was 69 years (IQR, 58-79 years), and 45 073 patients (42%) were female. Among the population, 75 579 patients (69.9%) were intubated, with 71 615 (66.3% of all patients and 94.8% of those intubated) intubated within the first 15 minutes. Over time, there was a decrease in the proportion of patients intubated within 15 minutes (70.0% in 2000 vs 63.6% in 2014; P < .001 for trend; eFigure 1 in the Supplement). The median time to tracheal intubation in those intubated within the first 15 minutes was 5 minutes (IQR, 3-8 minutes). The distribution of timing of intubation and the cumulative proportion of patients intubated over the first 15 minutes are provided in eFigure 2 in the Supplement. Of those intubated within the first 15 minutes, 336 (0.5%) received a tracheostomy. The intubation confirmation methods in those intubated are presented in eTable 2 in the Supplement, and drugs administered during the cardiac arrest other than epinephrine are listed in eTable 3 in the Supplement.
Figure 1. Diagram of Derivation of the Study Population.
a Cardiac arrests that were not the first cardiac arrest during the current admission.
Among 88749 patients with an initial nonshockable rhythm, 61 264 (69.0%) were intubated within 15 minutes, with a median time to intubation of 5 minutes (IQR, 3-8 minutes). Among 19 330 patients with an initial shockable rhythm, 10 351 (53.5%) were intubated within 15 minutes. The median time to intubation in these patients was 5 minutes (IQR, 3-8 minutes).
Overall Outcomes and Unadjusted Analyses
A total of 24 256 patients (22.4%) survived to hospital discharge. In the unadjusted analysis, patients intubated within the first 15 minutes had lower survival compared with those not intubated: 12 140 of 71 615 (17.0%) vs 12 116 of 36 464 (33.2%), respectively (RR = 0.58; 95% CI, 0.57-0.59; P < .001).
Among the study population, 67 540 patients (62.5%) had ROSC (data were missing for 7 patients). The proportion of patients with ROSC was lower in those intubated within the first 15 minutes compared with those not intubated: 42 366 of 71 611 (59.2%) vs 25 174 of 36 461 (69.0%), respectively (RR = 0.75; 95% CI, 0.73-0.76; P < .001). A total of 4631 patients (4.3%) had missing data on functional outcome. Of the 103 448 patients without missing data on functional outcome, 16 504 (16.0%) had a good functional outcome. The proportion of patients with a good functional outcome was lower in those intubated within the first 15 minutes compared with those not intubated: 7717 of 69 212 (11.2%) vs 8787 of 34 236 (25.7%), respectively (RR = 0.55; 95% CI, 0.54-0.56; P < .001).
Time-Dependent Propensity Score–Matched Analysis
A total of 86 628 patients were included in the propensity matched cohort (43 314 intubated patients [exposed group] matched 1:1 to 43 314 patients without intubation during the same minute [unexposed group], although these patients could have been intubated later). For patients in the exposed group, the median time to tracheal intubation was 4 minutes (IQR, 2-6 minutes). Among the unexposed group, 29 539 patients (68.2%) were intubated at some time point after the matching. For these patients, the time to intubation was 8 minutes (IQR, 5-12 minutes). Characteristics of the matched cohort according to exposure status are provided in Table 2. The patients were well matched on all included characteristics. In this matched cohort, survival was lower among the exposed group than among the unexposed group: 7052 of 43 314 (16.3%) vs 8407 of 43 314 (19.4%), respectively (RR = 0.84; 95% CI, 0.81- 0.87; P < .001). The proportion of patients with ROSC was lower among the exposed group than among the unexposed group: 25 022 of 43 311 (57.8%) vs 25 685 of 43 310 (59.3%), respectively (RR = 0.97; 95% CI, 0.96-0.99; P < .001). Good functional outcome was also lower among the exposed group than among the unexposed group: 4439 of 41 868 (10.6%) vs 5672 of 41 733 (13.6%), respectively (RR = 0.78; 95% CI, 0.75-0.81; P < .001). The results are summarized in Table 3.
Table 2. Patient, Hospital, and Event Characteristics Among Patients With In-Hospital Cardiac Arrest Without vs With Intubation in the First 15 Minutes of Resuscitation in the Matched Cohorta.
| Characteristic | Patients, No. (%) | Standardized Difference | |
|---|---|---|---|
| No Intubation (n = 43 314) | Intubation (n = 43 314) | ||
| Patient Characteristics | |||
| Demographic | |||
| Age, median (IQR), y | 70 (58-79) | 70 (58-80) | .014 |
| Sex | |||
| Male | 25 332 (58) | 25 486 (59) | .007 |
| Female | 17 982 (42) | 17 828 (41) | .007 |
| Race | |||
| White | 30 547 (71) | 30 713 (71) | .008 |
| Black | 8837 (20) | 8710 (20) | .007 |
| Other | 1361 (3) | 1321 (3) | .005 |
| Not reported | 2569 (6) | 2570 (6) | <.001 |
| Illness category | |||
| Medical | |||
| Cardiac | 15 779 (36) | 15 716 (36) | .003 |
| Noncardiac | 19 979 (46) | 20 017 (46) | .002 |
| Surgical | |||
| Cardiac | 2274 (5) | 2197 (5) | .008 |
| Noncardiacb | 4623 (11) | 4708 (11) | .006 |
| Trauma | 659 (2) | 676 (2) | .003 |
| Preexisting conditionc | |||
| Cardiac | |||
| History of myocardial infarction | 7477 (17) | 7370 (17) | .007 |
| Myocardial infarction this admission | 6786 (16) | 6697 (15) | .006 |
| History of heart failure | 10 186 (24) | 10 170 (23) | .001 |
| Heart failure this admission | 7852 (18) | 7947 (18) | .006 |
| Noncardiac | |||
| Respiratory insufficiency | 14 822 (34) | 14 845 (34) | .001 |
| Diabetes mellitus | 14 264 (33) | 14 334 (33) | .003 |
| Renal insufficiency | 14 893 (34) | 14 739 (34) | .007 |
| Metastatic or hematologic malignancy | 5579 (13) | 5663 (13) | .006 |
| Hypotension or hypoperfusion | 8659 (20) | 8741 (20) | .005 |
| Pneumonia | 5381 (12) | 5351 (12) | .002 |
| Baseline depression in CNS function | 4629 (11) | 4636 (11) | .001 |
| Metabolic or electrolyte abnormality | 6300 (15) | 6306 (15) | <.001 |
| Septicemia | 5598 (13) | 5707 (13) | .007 |
| Acute CNS nonstroke event | 2708 (6) | 2756 (6) | .005 |
| Hepatic insufficiency | 2837 (7) | 2841 (7) | <.001 |
| Acute stroke | 1639 (4) | 1652 (4) | .002 |
| Major trauma | 962 (2) | 954 (2) | .001 |
| Hospital Characteristics | |||
| Bed size, No. | |||
| 1-249 | 8132 (19) | 8016 (19) | .007 |
| 250-499 | 17 367 (40) | 17 444 (40) | .004 |
| ≥500 | 17 815 (41) | 17 854 (41) | .002 |
| Teaching status | |||
| Major | 14 747 (34) | 14 609 (34) | .007 |
| Minor | 13 252 (31) | 13 357 (31) | .005 |
| Nonteaching | 15 315 (35) | 15 348 (35) | .002 |
| Ownership | |||
| Military | 905 (2) | 928 (2) | .004 |
| Nonprofit | 31 189 (72) | 31 195 (72) | <.001 |
| Government | 6444 (15) | 6385 (15) | .004 |
| Private | 4776 (11) | 4806 (11) | .002 |
| Location | |||
| Rural | 2342 (5) | 2348 (5) | .001 |
| Urban | 40 972 (95) | 40 966 (95) | .001 |
| Geographical location | |||
| Northeast | 6032 (14) | 6077 (14) | .003 |
| Southeast | 13 184 (30) | 13 123 (30) | .003 |
| Midwest | 9090 (21) | 9160 (21) | .004 |
| South central | 8977 (21) | 8898 (21) | .005 |
| West | 6031 (14) | 6056 (14) | .002 |
| In-Hospital Cardiac Arrest Characteristics | |||
| Year of cardiac arrest | |||
| 2000-2002 | 4319 (10) | 4480 (10) | .012 |
| 2003-2004 | 6783 (16) | 6642 (15) | .009 |
| 2005-2006 | 6691 (15) | 6824 (16) | .008 |
| 2007-2008 | 6484 (15) | 6486 (15) | <.001 |
| 2009-2010 | 5837 (13) | 5709 (13) | .009 |
| 2011-2012 | 5965 (14) | 6030 (14) | .004 |
| 2013-2014 | 7235 (17) | 7143 (16) | .006 |
| In place at time of cardiac arrest | |||
| Noninvasive assisted ventilation | 2296 (5) | 2377 (5) | .008 |
| Dialysisd | 1185 (3) | 1176 (3) | .001 |
| Implantable cardiac defibrillator | 827 (2) | 780 (2) | .008 |
| Intra-arterial catheter | 1455 (3) | 1417 (3) | .005 |
| Electrocardiogram | 31 224 (72) | 31 059 (72) | .008 |
| Pulse oximeter | 23 623 (55) | 23 524 (54) | .005 |
| Vasoactive agentse | 5430 (13) | 5426 (13) | <.001 |
| Antiarrhythmic agentsf | 1123 (3) | 1093 (3) | .004 |
| Location | |||
| Emergency department | 4422 (10) | 4546 (11) | .009 |
| Floor with telemetry | 9342 (22) | 9373 (22) | .002 |
| Floor without telemetry | 12 263 (28) | 12 331 (28) | .003 |
| Intensive care unit | 13 556 (31) | 13 384 (31) | .009 |
| OR, PACU, or interventional unit | 2585 (6) | 2550 (6) | .003 |
| Otherg | 1146 (3) | 1130 (3) | .002 |
| Time of day | |||
| Day, 7:00 AM to 10:59 PM | 28 953 (67) | 28 878 (67) | .004 |
| Night, 11:00 PM to 6:59 AM | 14 361 (33) | 14 436 (33) | .004 |
| Day | |||
| Weekday, Monday 7 AM to Friday 11 PM | 29 809 (69) | 28 886 (69) | .004 |
| Weekend, Friday 11 PM to Monday 7 AM | 13 505 (31) | 13 428 (31) | .004 |
| Hospital-wide cardiac arrest response activated | 36 562 (84) | 36 529 (84) | .002 |
| Witnessed | 32 884 (76) | 32 835 (76) | .003 |
| First documented pulseless rhythm | |||
| Asystole | 16 324 (38) | 16 574 (38) | .012 |
| Pulseless electrical activity | 20 344 (47) | 20 065 (46) | .013 |
| Ventricular fibrillation | 4478 (10) | 4501 (10) | .002 |
| Pulseless ventricular tachycardia | 2168 (5) | 2174 (5) | .001 |
| Time to compressions, min | |||
| 0 | 39 465 (91) | 39 537 (91) | .006 |
| 1 | 1963 (5) | 1931 (4) | .004 |
| ≥2 | 1886 (4) | 1846 (4) | .005 |
| Epinephrine administered before matching | 23 084 (53) | 23 226 (54) | .007 |
| Time to epinephrine administration, median (IQR), min | 1 (1-3) | 1 (1-3) | .027 |
| Defibrillation before matchingh | 3895 (59) | 3859 (58) | .016 |
| Time to defibrillation, median (IQR), min | 1 (0-2) | 1 (0-2) | .050 |
Abbreviations: CNS, central nervous system; IQR, interquartile range; OR, operating room; PACU, postanesthesia care unit.
Patients being intubated at any given minute (from 0-15 minutes; intubation group) were matched with patients at risk of being intubated within the same minute (ie, still receiving resuscitation; no intubation group) based on a time-dependent propensity score calculated from multiple patient, event, and hospital characteristics.
Includes patients with an obstetric admission (n = 110).
See eTable 1 in the Supplement for definitions of preexisting conditions.
Hemodialysis or peritoneal dialysis, continuous arteriovenous dialysis, or venovenous hemofiltration or dialysis.
Dobutamine, dopamine (>3 μg/kg/min), epinephrine, nitroglycerin, norepinephrine, phenylephrine, vasopressin, and/or “other vasoactive agent(s).”
Continuous infusion of amiodarone, lidocaine, procainamide, and/or “other antiarrhythmic(s).”
Ambulatory and outpatient areas; delivery suite; rehabilitation, skilled nursing, and mental health facilities; same-day surgical areas; and “other.”
Includes only patients with a first documented pulseless rhythm of pulseless ventricular tachycardia or ventricular fibrillation.
Table 3. Outcomes for Patients With In-Hospital Cardiac Arrest Without vs With Intubation in the First 15 Minutes of Resuscitation in the Overall and Time-Dependent Propensity Score–Matched Cohorts.
| Outcome | Unadjusted Analysis | Propensity Score–Matched Analysisa | ||||
|---|---|---|---|---|---|---|
| No. of Patients With Outcome/Total Patients (%) | Risk Ratio (95% CI) | No. of Patients With Outcome/Total Patients (%) | Risk Ratio (95% CI) | |||
| No Intubation | Intubation | No Intubation | Intubation | |||
| ROSC | 25 174/36 461 (69.0) | 42 366/71 611 (59.2) | 0.75 (0.73-0.76) | 25 685/43 310 (59.3) | 25 022/43 311 (57.8) | 0.97 (0.96-0.99) |
| Survival to hospital discharge | 12 116/36 464 (33.2) | 12 140/71 615 (17.0) | 0.58 (0.57-0.59) | 8407/43 314 (19.4) | 7052/43 314 (16.3) | 0.84 (0.81-0.87) |
| Favorable functional outcomeb | 8787/34 236 (25.7) | 7717/69 212 (11.2) | 0.55 (0.54-0.56) | 5672/41 733 (13.6) | 4439/41 868 (10.6) | 0.78 (0.75-0.81) |
Abbreviation: ROSC, return of spontaneous circulation.
Patients being intubated at any given minute (from 0-15 minutes; intubation group) were matched with patients at risk of being intubated within the same minute (ie, still receiving resuscitation; no intubation group) based on a time-dependent propensity score calculated from multiple patient, event, and hospital characteristics.
A cerebral performance category score of 1 (mild or no neurological deficit) or 2 (moderate cerebral disability) at hospital discharge was considered a good functional outcome.
Subgroup Analyses
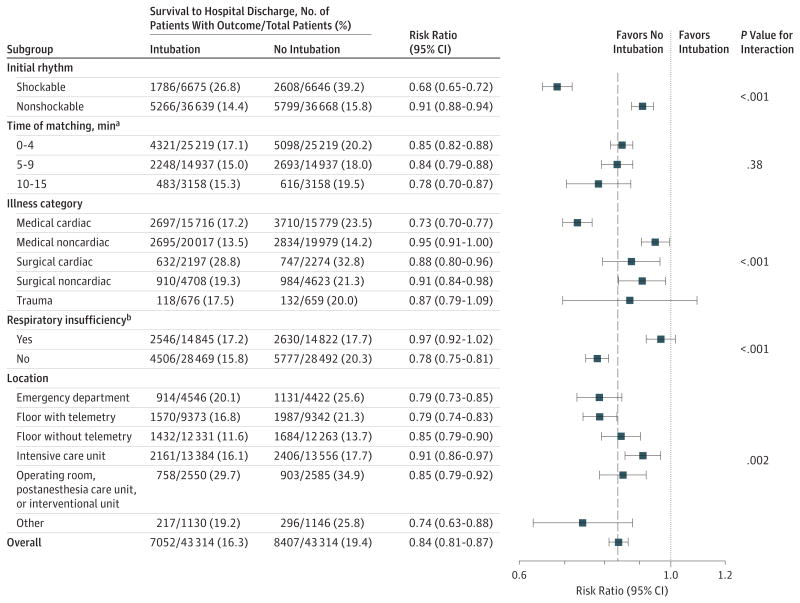
The results of the subgroup analyses for survival are presented in Figure 2. There was a significant interaction for initial rhythm (P < .001) such that tracheal intubation was more strongly associated with a lower likelihood of survival in those with an initial shockable rhythm (RR = 0.68; 95% CI, 0.65- 0.72) compared with those with an initial non shockable rhythm (RR = 0.91; 95% CI, 0.88-0.94). The association between tracheal intubation and survival was also modified by preexisting respiratory insufficiency (P for interaction < .001). In those without preexisting respiratory insufficiency, intubation was associated with lower likelihood of survival (RR = 0.78; 95% CI, 0.75-0.81), whereas no association was seen in those with preexisting respiratory insufficiency (RR = 0.97; 95% CI, 0.92- 1.02). There were also subgroup differences according to illness category (P < .001) and location (P = .002) (Figure 2). There was no significant interaction for the time of matching (P = .38), indicating that the association between intubation and survival did not change during the first 15 minutes of the cardiac arrest. There was also no significant interaction when treating time of matching as a continuous linear variable (P = .22; eFigure 3 in the Supplement).
Figure 2. Forest Plot of Subgroup Analyses of Survival to Hospital Discharge in the Propensity-Matched Cohort.
Risk ratios with 95% confidence intervals for predefined subgroup analyses. The P value represents the type III P value for the interaction between intubation and a given subgroup. The dashed vertical line represents the risk ratio in the overall cohort; the dotted vertical line, a risk ratio of 1.0 (ie, no effect). Except for the time of the matching, there were significant differences according to all other subgroups.
a The minute at which patients in the intubation group were intubated and matched with a patient not intubated before or within that same minute.
b Evidence of acute or chronic respiratory insufficiency within 4 hours up to the time of the event (see eTable 1 in the Supplement for additional details).
Sensitivity Analyses
Data were missing or inconsistent for at least 1 variable for 35 731 patients (24.8%), with a median number of missing variables of 0 (IQR, 0-0 variables; mean [SD], 0.5 [1.4] variables). A total of 143 810 patients were included in the sensitivity analysis accounting for missing data. Between 112 684 and 113 076 patients were propensity score matched in the 20 imputed data sets. The results from these analyses were similar to the primary analyses. Tracheal intubation was associated with lower likelihood of survival (RR = 0.84; 95% CI, 0.81-0.87; P < .001), ROSC (RR = 0.97; 95% CI, 0.97-0.98; P < .001), and good functional outcome (RR = 0.81; 95% CI, 0.79-0.84; P < .001).
In a post hoc analysis using non–time-dependent propensity score matching, 61 262 patients were matched. The patients were well matched on all included covariates (standardized differences between −0.03 and 0.03). In this cohort, intubation as compared with no intubation was associated with a lower likelihood of survival: 5968 of 30 631 patients (19.5%) vs 11 074 of 30 631 patients (36.2%), respectively (RR = 0.54; 95% CI, 0.52-0.56; P < .001). Intubation was also associated with a decreased likelihood of ROSC (18 885 of 30629 intubated patients [61.7%] vs 21 465 of 30628 patients not intubated [70.1%]; RR = 0.88; 95% CI, 0.87-0.89; P < .001) and a good functional outcome (3850 of 29403 intubated patients [13.1%] vs 8129 of 28 669 patients not intubated [28.4%]; RR = 0.46; 95% CI, 0.44-0.48; P < .001).
Discussion
In this large, multicenter, retrospective, observational, matched cohort study, tracheal intubation at any minute within the first 15 minutes during in-hospital cardiac arrest, compared with no intubation during that minute, was associated with a 3% absolute reduction and 16% relative reduction in survival to hospital discharge. Intubation was also associated with a 2% absolute reduction and 3% relative reduction in ROSC and a 3% absolute reduction and 22% relative reduction in good functional outcome at hospital discharge.
Studies of tracheal intubation during adult in-hospital cardiac arrest are scarce, and no randomized clinical trials comparing intubation with no intubation in this setting were identified.1,2 An observational study (n = 470) from 1990 of patients with in-hospital cardiac arrest found that tracheal intubation during the cardiac arrest was associated with increased mortality,20 similar to an observational study from 2001 (n = 445).21 A large observational study(n = 649359) from Japan found that tracheal intubation during out-of-hospital cardiac arrest was associated with decreased odds of neurologically favorable survival.4 However, an observational study (n = 32 513) from Korea found that intubation during out-of-hospital cardiac arrest was associated with good neurological outcome at hospital discharge.22 In both studies, tracheal intubation was rare (6% and 4%, respectively) and rates of good outcome were low.4,22 A meta-analysis from 2013 of observational out-of-hospital cardiac arrest studies found that tracheal intubation compared with basic airway management was not associated with ROSC but was associated with decreased survival.23 None of these previous studies accounted for the time-dependent nature of tracheal intubation during cardiac arrest as done in the current study (see the eAppendix in the Supplement for additional discussion of the importance of this approach).
Multiple mechanisms could explain a potential causal relationship between tracheal intubation and poor outcomes.11,24 First, tracheal intubation might lead to a prolonged interruption in chestcompressions.25 Second, tracheal intubation might lead to hyperventilation and hyperoxia, which are associated with poor outcomes.26,27 Third, tracheal intubation could delay other interventions such as defibrillation or epinephrine administration.28,29 Fourth, delays in the time to success of intubation could result in inadequate ventilation or oxygenation by other means. Fifth, unrecognized esophageal intubation or dislodgement of the tube during the cardiac arrest could lead to fatal outcomes. Potential beneficial effects of intubation include better control of ventilation and oxygenation as well as protection from aspiration.24 Moreover, once an advanced airway is established, chest compressions may be provided in a more continuous fashion.30,31 However, continuous chest compressions may not improve outcomes.32
In this study, there were important differences in several prespecified subgroup analyses. Tracheal intubation was associated much more strongly with decreased survival among patients with an initial shockable rhythm (32% relative decrease) compared with those with an initial nonshockable rhythm(9% relative decrease). Similar subgroup differences have been reported in the out-of-hospital setting.4 These findings may indicate that the potential detrimental effects of intubation are more pronounced in patients with a shockable rhythm, for who mother interventions such as early defibrillation are more relevant. The current study also identified an important subgroup difference according to preexisting respiratory insufficiency: intubation was not significantly associated with outcomes in those with preexisting respiratory insufficiency. A proportion of patients with preexisting respiratory insufficiency might have had cardiac arrest as a consequence of respiratory failure, and early advanced airway management could be beneficial for these patients. Although the effect estimate varied according to subgroup, intubation was not associated with improved survival in any of the subgroups.
A few relatively small randomized trials have been conducted in the out-of-hospital setting comparing various airway devices vs usual care or tracheal intubation, finding no differences in clinical outcomes between groups.33-35 However, at least 3 currently ongoing randomized phase 3 trials are assessing advanced airway management during cardiac arrest in the out-of-hospital setting (clinicaltrials.gov identifiers NCT02419573 and NCT02327026 and isrctn.com identifier ISRCTN08256118). While these trials assess the efficacy of advanced airway management in the out-of-hospital setting, the results might not translate to the in-hospital setting given important differences in cardiac arrest etiology, skills of health care professionals, and timing of interventions. Given that intubation is very common during in-hospital cardiac arrest (70% in the current study) and that very little, if any, evidence exists to support this practice, randomized clinical trials in the in-hospital setting are needed and appear justified. However, based on the estimates from this study, such studies would likely need to be very large to be powered adequately to detect a significant difference.
The results of this study should be interpreted in relation to the observational design and certain limitations. Potential confounders such as the skills and experience of health care professionals, the underlying cause of the cardiac arrest, the quality of chest compressions, and the indication for intubation were not available in the registry. As such, confounding by indication could have influenced the results.36 In the data registry, data on unsuccessful intubation attempts are not available. Limited published data are available on unsuccessful intubation in the global in-hospital setting. However, data from the emergency department37 and out-of-hospital setting38 indicate that failed intubation is associated with poor outcomes. Because these patients were classified as having no intubation in the GWTG-R registry, this would potentially bias the results toward the null and therefore probably cannot explain the findings reported herein. Misclassification of variables might have occurred, especially in relation to the timing of interventions.39 However, it is most likely that these misclassifications are unrelated to outcomes40 and therefore would be unlikely to explain the findings. In addition, although missing data were relatively uncommon in general (median of 0 missing variables [IQR, 0-0 missing variables] of more than 40 variables included), data were missing on at least 1 variable for 25% of the patients. This study aimed to address this by using multiple imputations techniques, which showed results similar to those of the primary analysis.
Conclusions
Among adult patients with in-hospital cardiac arrest, initiation of tracheal intubation within any given minute during the first 15 minutes of resuscitation, compared with no intubation during that minute, was associated with decreased survival to hospital discharge. Although the study design does not eliminate the potential for confounding by indication, these findings do not support early tracheal intubation for adult in-hospital cardiac arrest.
Supplementary Material
Key Points.
Question
Is tracheal intubation during adult in-hospital cardiac arrest associated with survival?
Findings
In a study of 86 628 adults with in-hospital cardiac arrest using a propensity-matched cohort, tracheal intubation within the first 15 minutes was associated with a significantly lower likelihood of survival to hospital discharge compared with not being intubated (16.3% vs 19.4%, respectively).
Meaning
These findings do not support early tracheal intubation for adult in-hospital cardiac arrest.
Acknowledgments
Funding/Support: Dr Donnino is supported by grant 1K24HL127101-01 from the National Heart, Lung, and Blood Institute.
Role of the Funder/Sponsor: The funding agency had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Author Contributions: Dr Andersen had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: All authors.
Acquisition, analysis, or interpretation of data: All authors.
Drafting of the manuscript: Andersen, Donnino.
Critical revision of the manuscript for important intellectual content: All authors.
Statistical analysis: Andersen, Kurth.
Supervision: All authors.
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Dr Callaway reported receiving a grant from the National Institutes of Health and serving as volunteer chair of the Emergency Cardiovascular Care Committee of the American Heart Association. Dr Kurth reported receiving honoraria from BMJ and Cephalalgia for editorial services. Dr Donnino reported serving as a paid consultant for the American Heart Association. No other disclosures were reported.
Get With The Guidelines–Resuscitation (GWTG-R) Investigators: The Get With The Guidelines–Resuscitation Adult Research Task Force includes authors Michael W. Donnino, MD, and Steven M. Bradley, MD, MPH, as well as Saket Girotra, MBBS, SM(University of Iowa Carver College of Medicine); Paul S. Chan, MD, MSc (University of Missouri–Kansas City); Monique L. Anderson, MD (Duke University School of Medicine); Matthew M. Churpek, MD, MPH, PhD, and Dana P. Edelson, MD,MS (University of Chicago); Robert T. Faillace, MD, ScM (Jacobi Medical Center); Romergryko Geocadin, MD (Johns Hopkins University School of Medicine); Ahamed H. Idris, MD (University of Texas Southwestern Medical Center); Raina M. Merchant, MD, MSHP (University of Pennsylvania Perelman School of Medicine); Vincent N. Mosesso Jr, MD (University of Pittsburgh School of Medicine); Joseph P. Ornato, MD, and Mary Ann Peberdy, MD (Virginia Commonwealth University Medical Center); Sarah M. Perman, MD, MSCE (University of Colorado School of Medicine); and Mindy Smyth, MSN, RN.
Disclaimer: The American Heart Association maintains the GWTG-R registry and oversees and approves data queries and manuscript submissions. However, the author group is responsible for the conception of the project, all data analyses, and manuscript writing.
Meeting Presentation: This article was presented at the 46th Critical Care Congress of the Society of Critical Care Medicine; January 24, 2017; Honolulu, Hawaii.
Additional Contributions: Francesca Montillo, MM, Emergency Department, Beth Israel Deaconess Medical Center, Boston, Massachusetts, provided editorial assistance. She did not receive any specific financial compensation for her role in the current study.
Contributor Information
Lars W. Andersen, Research Center for Emergency Medicine, Aarhus University Hospital, Aarhus, Denmark; Department of Anesthesiology, Aarhus University Hospital, Aarhus, Denmark; Department of Emergency Medicine, Beth Israel Deaconess Medical Center, Boston, Massachusetts.
Asger Granfeldt, Department of Anesthesiology, Aarhus University Hospital, Aarhus, Denmark.
Clifton W. Callaway, Department of Emergency Medicine, University of Pittsburgh, Pittsburgh, Pennsylvania.
Steven M. Bradley, Division of Cardiology, Department of Medicine, VA Eastern Colorado Health Care System, Denver; Now with Minneapolis Heart Institute, Minneapolis, Minnesota.
Jasmeet Soar, Anaesthesia and Intensive Care Medicine, Southmead Hospital, Bristol, England.
Jerry P. Nolan, University of Bristol, Bristol, England; Department of Anaesthesia and Intensive Care Medicine, Royal United Hospital, Bath, England.
Tobias Kurth, Institute of Public Health, Charité-Universitätsmedizin Berlin, Berlin, Germany.
Michael W. Donnino, Department of Emergency Medicine, Beth Israel Deaconess Medical Center, Boston, Massachusetts; Division of Pulmonary and Critical Care Medicine, Department of Medicine, Beth Israel Deaconess Medical Center, Boston, Massachusetts.
References
- 1.Callaway CW, Soar J, Aibiki M, et al. Advanced Life Support Chapter Collaborators. Part 4: advanced life support: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation. 2015;132(16) suppl 1:S84–S145. doi: 10.1161/CIR.0000000000000273. [DOI] [PubMed] [Google Scholar]
- 2.Link MS, Berkow LC, Kudenchuk PJ, et al. Part 7: adult advanced cardiovascular life support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132(18) suppl 2:S444–S464. doi: 10.1161/CIR.0000000000000261. [DOI] [PubMed] [Google Scholar]
- 3.Soar J, Nolan JP, Böttiger BW, et al. Adult Advanced Life Support Section Collaborators. European Resuscitation Council Guidelines for Resuscitation 2015: section 3: adult advanced life support. Resuscitation. 2015;95:100–147. doi: 10.1016/j.resuscitation.2015.07.016. [DOI] [PubMed] [Google Scholar]
- 4.Hasegawa K, Hiraide A, Chang Y, Brown DF. Association of prehospital advanced airway management with neurologic outcome and survival in patients with out-of-hospital cardiac arrest. JAMA. 2013;309(3):257–266. doi: 10.1001/jama.2012.187612. [DOI] [PubMed] [Google Scholar]
- 5.Fredriksson M, Aune S, Bång A, et al. Cardiac arrest outside and inside hospital in a community: mechanisms behind the differences in outcome and outcome in relation to time of arrest. Am Heart J. 2010;159(5):749–756. doi: 10.1016/j.ahj.2010.01.015. [DOI] [PubMed] [Google Scholar]
- 6.Peberdy MA, Kaye W, Ornato JP, et al. Cardiopulmonary resuscitation of adults in the hospital: a report of 14720 cardiac arrests from the National Registry of Cardiopulmonary Resuscitation. Resuscitation. 2003;58(3):297–308. doi: 10.1016/s0300-9572(03)00215-6. [DOI] [PubMed] [Google Scholar]
- 7.Peberdy MA, Ornato JP, Larkin GL, et al. National Registry of Cardiopulmonary Resuscitation Investigators. Survival from in-hospital cardiac arrest during nights and weekends. JAMA. 2008;299(7):785–792. doi: 10.1001/jama.299.7.785. [DOI] [PubMed] [Google Scholar]
- 8.American Hospital Association. [Accessed July 21, 2015];AHA Annual Survey Database fiscal year 2013. 2014 https://www.ahadataviewer.com/book-cd-products/aha-survey/
- 9.Chan PS, Nichol G, Krumholz HM, et al. American Heart Association National Registry of Cardiopulmonary Resuscitation (NRCPR) Investigators. Racial differences in survival after in-hospital cardiac arrest. JAMA. 2009;302(11):1195–1201. doi: 10.1001/jama.2009.1340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Perkins GD, Jacobs IG, Nadkarni VM, et al. Utstein Collaborators. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update of the Utstein resuscitation registry templates for out-of-hospital cardiac arrest: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian and New Zealand Council on Resuscitation, Heart and Stroke Foundation of Canada, Inter American Heart Foundation, Resuscitation Council of Southern Africa, Resuscitation Council of Asia); and the American Heart Association Emergency Cardiovascular Care Committee and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Resuscitation. 2015;96:328–340. doi: 10.1016/j.resuscitation.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 11.Andersen LW, Raymond TT, Berg RA, et al. American Heart Association's Get With The Guidelines–Resuscitation Investigators. Association between tracheal intubation during pediatric in-hospital cardiac arrest and survival. JAMA. 2016;316(17):1786–1797. doi: 10.1001/jama.2016.14486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lu B. Propensity score matching with time-dependent covariates. Biometrics. 2005;61(3):721–728. doi: 10.1111/j.1541-0420.2005.00356.x. [DOI] [PubMed] [Google Scholar]
- 13.Nakahara S, Tomio J, Takahashi H, et al. Evaluation of pre-hospital administration of adrenaline (epinephrine) by emergency medical services for patients with out of hospital cardiac arrest in Japan: controlled propensity matched retrospective cohort study. BMJ. 2013;347:f6829. doi: 10.1136/bmj.f6829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li YP, Propert KJ, Rosenbaum PR. Balanced risk set matching. J Am Stat Assoc. 2001;96(455):870–882. doi: 10.1198/016214501753208573. [DOI] [Google Scholar]
- 15.Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46(3):399–424. doi: 10.1080/00273171.2011.568786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 17.Zou GY, Donner A. Extension of the modified Poisson regression model to prospective studies with correlated binary data. Stat Methods Med Res. 2013;22(6):661–670. doi: 10.1177/0962280211427759. [DOI] [PubMed] [Google Scholar]
- 18.Miglioretti DL, Heagerty PJ. Marginal modeling of nonnested multilevel data using standard software. Am J Epidemiol. 2007;165(4):453–463. doi: 10.1093/aje/kwk020. [DOI] [PubMed] [Google Scholar]
- 19.Rothman KJ. No adjustments are needed for multiple comparisons. Epidemiology. 1990;1(1):43–46. [PubMed] [Google Scholar]
- 20.Tortolani AJ, Risucci DA, Rosati RJ, Dixon R. In-hospital cardiopulmonary resuscitation: patient, arrest and resuscitation factors associated with survival. Resuscitation. 1990;20(2):115–128. doi: 10.1016/0300-9572(90)90047-i. [DOI] [PubMed] [Google Scholar]
- 21.Dumot JA, Burval DJ, Sprung J, et al. Outcome of adult cardiopulmonary resuscitations at a tertiary referral center including results of “limited” resuscitations. Arch Intern Med. 2001;161(14):1751–1758. doi: 10.1001/archinte.161.14.1751. [DOI] [PubMed] [Google Scholar]
- 22.Kang K, Kim T, Ro YS, Kim YJ, Song KJ, Shin SD. Prehospital endotracheal intubation and survival after out-of-hospital cardiac arrest: results from the Korean nationwide registry. Am J Emerg Med. 2016;34(2):128–132. doi: 10.1016/j.ajem.2015.09.036. [DOI] [PubMed] [Google Scholar]
- 23.Fouche PF, Simpson PM, Bendall J, Thomas RE, Cone DC, Doi SA. Airways in out-of-hospital cardiac arrest: systematic review and meta-analysis. Prehosp Emerg Care. 2014;18(2):244–256. doi: 10.3109/10903127.2013.831509. [DOI] [PubMed] [Google Scholar]
- 24.Benoit JL, Prince DK, Wang HE. Mechanisms linking advanced airway management and cardiac arrest outcomes. Resuscitation. 2015;93:124–127. doi: 10.1016/j.resuscitation.2015.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Maignan M, Koch FX, Kraemer M, et al. Impact of laryngeal tube use on chest compression fraction during out-of-hospital cardiac arrest: a prospective alternate month study. Resuscitation. 2015;93:113–117. doi: 10.1016/j.resuscitation.2015.06.002. [DOI] [PubMed] [Google Scholar]
- 26.Aufderheide TP, Sigurdsson G, Pirrallo RG, et al. Hyperventilation-induced hypotension during cardiopulmonary resuscitation. Circulation. 2004;109(16):1960–1965. doi: 10.1161/01.CIR.0000126594.79136.61. [DOI] [PubMed] [Google Scholar]
- 27.Kilgannon JH, Jones AE, Shapiro NI, et al. Emergency Medicine Shock Research Network (EMShockNet) Investigators. Association between arterial hyperoxia following resuscitation from cardiac arrest and in-hospital mortality. JAMA. 2010;303(21):2165–2171. doi: 10.1001/jama.2010.707. [DOI] [PubMed] [Google Scholar]
- 28.Chan PS, Krumholz HM, Nichol G, Nallamothu BK American Heart Association National Registry of Cardiopulmonary Resuscitation Investigators. Delayed time to defibrillation after in-hospital cardiac arrest. N Engl J Med. 2008;358(1):9–17. doi: 10.1056/NEJMoa0706467. [DOI] [PubMed] [Google Scholar]
- 29.Donnino MW, Salciccioli JD, Howell MD, et al. American Heart Association's Get With The Guidelines-Resuscitation Investigators. Time to administration of epinephrine and outcome after in-hospital cardiac arrest with non-shockable rhythms: retrospective analysis of large in-hospital data registry. BMJ. 2014;348:g3028. doi: 10.1136/bmj.g3028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yeung J, Chilwan M, Field R, Davies R, Gao F, Perkins GD. The impact of airway management on quality of cardiopulmonary resuscitation: an observational study in patients during cardiac arrest. Resuscitation. 2014;85(7):898–904. doi: 10.1016/j.resuscitation.2014.02.018. [DOI] [PubMed] [Google Scholar]
- 31.Kramer-Johansen J, Wik L, Steen PA. Advanced cardiac life support before and after tracheal intubation—direct measurements of quality. Resuscitation. 2006;68(1):61–69. doi: 10.1016/j.resuscitation.2005.05.020. [DOI] [PubMed] [Google Scholar]
- 32.Nichol G, Leroux B, Wang H, et al. ROC Investigators. Trial of continuous or interrupted chest compressions during CPR. N Engl J Med. 2015;373(23):2203–2214. doi: 10.1056/NEJMoa1509139. [DOI] [PubMed] [Google Scholar]
- 33.Goldenberg IF, Campion BC, Siebold CM, McBride JW, Long LA. Esophageal gastric tube airway vs endotracheal tube in prehospital cardiopulmonary arrest. Chest. 1986;90(1):90–96. doi: 10.1378/chest.90.1.90. [DOI] [PubMed] [Google Scholar]
- 34.Rabitsch W, Schellongowski P, Staudinger T, et al. Comparison of a conventional tracheal airway with the Combitube in an urban emergency medical services system run by physicians. Resuscitation. 2003;57(1):27–32. doi: 10.1016/s0300-9572(02)00435-5. [DOI] [PubMed] [Google Scholar]
- 35.Benger J, Coates D, Davies S, et al. Randomised comparison of the effectiveness of the laryngeal mask airway supreme, i-gel and current practice in the initial airway management of out of hospital cardiac arrest: a feasibility study. Br J Anaesth. 2016;116(2):262–268. doi: 10.1093/bja/aev477. [DOI] [PubMed] [Google Scholar]
- 36.Kyriacou DN, Lewis RJ. Confounding by indication in clinical research. JAMA. 2016;316(17):1818–1819. doi: 10.1001/jama.2016.16435. [DOI] [PubMed] [Google Scholar]
- 37.Kim J, Kim K, Kim T, et al. The clinical significance of a failed initial intubation attempt during emergency department resuscitation of out-of-hospital cardiac arrest patients. Resuscitation. 2014;85(5):623–627. doi: 10.1016/j.resuscitation.2014.01.017. [DOI] [PubMed] [Google Scholar]
- 38.Wnent J, Franz R, Seewald S, et al. German Resuscitation Registry Study Group. Difficult intubation and outcome after out-of-hospital cardiac arrest: a registry-based analysis. Scand J Trauma Resusc Emerg Med. 2015;23:43. doi: 10.1186/s13049-015-0124-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Peace JM, Yuen TC, Borak MH, Edelson DP. Tablet-based cardiac arrest documentation: a pilot study. Resuscitation. 2014;85(2):266–269. doi: 10.1016/j.resuscitation.2013.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Frisch A, Reynolds JC, Condle J, Gruen D, Callaway CW. Documentation discrepancies of time-dependent critical events in out of hospital cardiac arrest. Resuscitation. 2014;85(8):1111–1114. doi: 10.1016/j.resuscitation.2014.05.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.