Abstract
Purpose
High-risk human papillomavirus (HPV) infection progression should be considered a critical factor for preventing cervical cancer, although most infections are transient and rarely persist. This study aimed to examine the specific types of HPV infections, their change patterns, and the potential risk factors among Korean women.
Materials and Methods
We included 4,588 women who visited hospitals in Busan and Suwon for cervical cancer screening, and 1,224 of thesewomen attended a 2-yearfollow-up. Infection statuswas evaluated using HPV DNA testing (Hybrid Capture 2) and genotyping testing (Linear Array). Data regarding the potential risk factors for HPV infection were collected by trained nurses using structured questionnaires.
Results
Among the 1,224 women (mean age, 47 years), 105 women (8.6%) were HPV-positive at baseline. HPV infections had been cleared among 92 women (87.6%) within 2 years. Only 13 infections (12.4%) were remained, and the 10 cases of them are high-risk HPV types including genotype 33, 45, 16, 35, and 52. Among women who were negative at baseline, the HPV incidence was 4.8%. The HPV incidence was marginally associated with having multiple sexual partners (odds ratio, 2.0; 95% confidence interval, 1.0 to 3.9), although it was not significantly associated with HPV persistence.
Conclusion
Most HPV infections (88%) among Korean women were cleared within 2 years, with only a small number of persistent infections. The persistent HPV genotypes were different in our study, compared to those from previous studies. Having multiple sexual partners was associated with acquiring a HPV infection, but not with persistence.
Keywords: Human papillomavirus, Genotype, Persistence, Clearance, Incidence
Introduction
Human papillomavirus (HPV) infection can cause cervical cancer, and the cancer burden attributed to this infection varies according to geographical region and the genotype of people who are infected with HPV. It is most prevalent in Africa, Asia, and some European countries, compared to other regions of the world. Thirteen high-risk HPV (HRHPV) types, which are carcinogenic or presumed to be carcinogenic in humans, are frequently detected in patients who develop cervical cancer. For example, HPV types 16 and 18 account for approximately 70% of all cervical cancer cases [1]. Several epidemiological studies have evaluated the genotype-specific prevalences of HPV, factors that influence HPV acquisition, and the risk of cervical cancer development according to HPV infection status [1-4]. Furthermore, there are various factors that influence cervical cancer development, including viral infection and host factors. Thus, the prevention of cervical cancer relies on our understanding of the progression of HR-HPV infections, which involves persistence, clearance, new infections, and other determinant factors. However, most HPV infections are transient and rarely persist [5,6]. Only a few studies in specific countries and populations have considered the HPV genotype-specific incidence, persistence, clearance, and new infections [7-17]. Furthermore, only a few studies have evaluated the natural history of HPV infections in Asian countries, where the prevalence of HPV is high. Moreover, the association with cervical cancer development has been highlighted as a major health issue among women. In Korea, the prevalence of HPV is approximately 20% among women with normal cytology, based on the Papanicolaou test (Pap test) [18]. In addition, cervical cancer is a leading cancer among Korean women, with an age-standardized incidence of 9.5/100,000 women in 2012 [19]. Despite these data, there is a lack of Korean studies regarding changes in HPV infection status and the factors that contribute to these changes. Therefore, the present study aimed to examine HPV type-specific infections, their change patterns, and the factors that were involved in these changes, based on two HPV tests that were performed 2 years apart for Korean women who visited two centers.
Materials and Methods
1. Study population
This retrospective study evaluated prospectively collected data from a baseline test and a test at the 2-year follow-up. A total of 4,595 women visited government-affiliated hospitals in Busan and Suwon (Korea) for baseline testing between November 2004 and December 2006, as part of the National Cervical Cancer Screening Program. Among these women, 1,224 women subsequently attended the follow-up testing during 2007 and 2008. The details of the baseline testing have been described elsewhere [5], and Fig. 1 shows the inclusion and exclusion criteria for the present study.
Fig. 1.
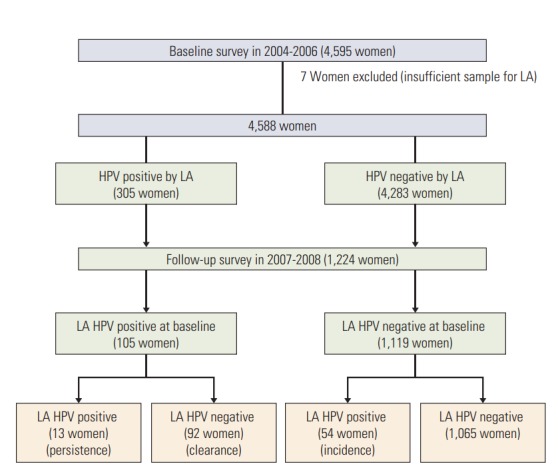
Participants in baseline and follow-up survey and their classification by the status of human papillomavirus (HPV) infection. LA, linear array.
2. Data collection
Data regarding the potential risk factors for HPV infection were obtained using questionnaires at the baseline test. A trained research nurse interviewed each participant and completed the structured questionnaire regarding their socio-demographic characteristics (age, marital status, educational level, and age at marriage), lifestyle behaviors (smoking, alcohol drinking, and number of sexual partners), obstetrical and reproductive history (parity, age of women at first childbirth, oral contraceptive use, intrauterine device use, and hormone therapy), and clinical characteristics (sexually transmitted disease histories for the participant and their partner, family and individual cancer history, and cervical screening history).
The outcome variable was based on the results from two HPV tests at the baseline and follow-up testing. The results were categorized according to the HPV infection change status: (1) type-specific persistence (positivity for the same HPV DNA type in both tests), (2) type-specific HPV clearance (a negative result for a specific HPV type after a previously positive result), and (3) incident HPV infection (a change from HPV DNA negativity at baseline to HPV DNA positivity at the follow-up test). The HPV testing was performed using the Hybrid Capture 2 system (HC2; Digene, Gaithersburg, MA), and HPV genotyping was performed on HC2-positive samples using a Linear Array assay (LA; Roche Molecular Systems, Branchburg, NJ) [20].
3. Statistical analysis
The proportions of HPV type-specific persistence and clearance were calculated among the 105 women who were HPV-positive, based on their baseline LA results. The incidences of new HPV type-specific infections were calculated among the 1,119 women who were HPV-negative, based on their baseline LA results. Pearson’s chi-square test and Fischer exact test was used to assess the frequency distributions of potential risk factors for changing HPV infection status. Logistic regression analyses were also used to evaluate the role of potential risk factors in the changes in HPV infection status. Associations were reported as odds ratios (ORs) and 95% confidence intervals (CIs). All tests were two-sided, and a p-value of < 0.05 was considered statistically significant. All analyses were performed using STATA software ver. 13 (StataCorp LP, College Station, TX).
4. Ethical statement
The study protocol was approved by the Institutional Review Board of the National Cancer Center, and all participants provided written informed consent at the baseline test.
Results
Among the 4,588 women who participated in the baseline survey, only 1,224 women were followed-up and included in the present analysis. When we compared the participants from the baseline and follow-up testing, we did not observe any noticeably differences in their socio-demographic, behavioral, and reproductive characteristics, or in their HPV infection rates (S1 Table). The mean patient age at baseline was 47 years (range, 21 to 66 years), most participants were married or cohabitating, 17% of the participants had ≥ 2 sexual partners during their lifetime, and the prevalence of HPV infections was 8.6%. At the 2-year follow-up, the prevalence of HPV infection decreased to 6.0%. All participants and the high-risk group for HPV infection were most likely to live in Busan, have ≥ 2 sexual partners during their lifetime, have a family history of cancer, and have a history of HPV infection at baseline (Table 1).
Table 1.
General characteristics of 1,224 study participants at the follow up by HPV infection status
| Characteristic | Total (n=1,224) |
Overall HPV infectiona) (n=73) |
HR HPV infectiona) (n=52) |
||
|---|---|---|---|---|---|
| No. (%) | No. (%) | p-value | No. (%) | p-value | |
| Region | |||||
| Busan | 579 (47.3) | 57 (9.8) | 0.0001 | 41 (7.1) | 0.001 |
| Suwon | 645 (52.7) | 16 (2.5) | 11 (1.7) | ||
| Age group (yr) | |||||
| < 39 | 223 (18.2) | 15 (6.7) | 0.897 | 11 (5.0) | 0.913 |
| 40-49 | 529 (43.2) | 29 (5.5) | 23 (4.3) | ||
| 50-59 | 401 (32.8) | 25 (6.2) | 16 (4.0) | ||
| ≥ 60 | 71 (5.8) | 4 (5.6) | 2 (2.8) | ||
| Marital status | |||||
| Unmarried (single, divorced, and widower) | 204 (16.7) | 16 (7.8) | 0.214 | 10 (4.9) | 0.612 |
| Married (married and cohabitant) | 1,020 (83.3) | 57 (5.6) | 42 (4.1) | ||
| Education level | |||||
| None/Elementary/Middle school | 496 (40.5) | 34 (6.8) | 0.277 | 24 (4.8) | 0.398 |
| High school/University/≥ Master | 728 (59.5) | 39 (5.4) | 28 (3.8) | ||
| First marriage age (yr) | |||||
| < 25 | 402 (41.7) | 26 (6.5) | 0.169 | 19 (4.7) | 0.125 |
| ≥ 25 | 561 (58.3) | 25 (4.5) | 16 (2.8) | ||
| Smoking status | |||||
| Non smoker | 1,150 (94.0) | 70 (6.0) | 1.000 | 49 (4.2) | 0.474 |
| Current smoker | 73 (6.0) | 3 (5.8) | 3 (5.8) | ||
| Alcohol drinking | |||||
| No | 856 (69.9) | 45 (5.3) | 0.111 | 31 (3.6) | 0.097 |
| Yes | 368 (30.1) | 28 (7.6) | 21 (5.7) | ||
| Lifetime sexual partners | |||||
| 1 | 1,003 (82.2) | 49 (4.9) | 0.001 | 34 (3.4) | 0.003 |
| ≥ 2 | 217 (17.8) | 23 (10.6) | 17 (7.8) | ||
| Extramarital affair | |||||
| No | 1,065 (87.2) | 59 (5.5) | 0.283 | 42 (3.9) | 0.486 |
| Yes | 156 (12.8) | 12 (7.7) | 8 (5.1) | ||
| Parity | |||||
| 1 | 150 (12.8) | 10 (6.7) | 0.331 | 7 (4.7) | 0.873 |
| 2 | 719 (61.5) | 38 (5.3) | 29 (4.0) | ||
| ≥ 3 | 300 (25.7) | 23 (7.7) | 14 (4.7) | ||
| Menopause | |||||
| No | 506 (41.4) | 35 (6.9) | 0.24 | 22 (4.3) | 0.889 |
| Yes | 717 (58.6) | 38 (5.3) | 30 (4.2) | ||
| History of STDa) | |||||
| No | 1,155 (95.7) | 67 (5.8) | 0.231 | 47 (4.1) | 0.274 |
| Yes | 52 (4.3) | 5 (9.6) | 4 (7.7) | ||
| Family history of cancer | |||||
| No | 809 (66.1) | 38 (4.7) | 0.009 | 24 (3.0) | 0.002 |
| Yes | 414 (33.9) | 35 (8.4) | 28 (6.8) | ||
| Cervical screening history | |||||
| No | 158 (13.0) | 5 (3.2) | 0.147 | 4 (7.8) | 0.392 |
| Yes | 1,058 (87.0) | 67 (6.3) | 47 (4.4) | ||
| Chlamydia trachomatis at baseline | |||||
| Negative | 1,151 (96.2) | 67 (5.8) | 0.336 | 48 (4.2) | 0.712 |
| Positive | 45 (3.8) | 4 (8.9) | 2 (4.4) | ||
| HPV status at baseline by LA | |||||
| Negative | 1,119 (91.4) | 54 (4.8) | < 0.001 | 36 (3.2) | < 0.001 |
| Positive | 105 (8.6) | 19 (18.1) | 16 (15.2) | ||
HPV, human papillomavirus; STD, sexual transmitted disease; LA, linear array.
Sample sizes for individual characteristics may not equal total due to missing values.
Among the 105 HPV infections from the baseline, only 13 infections (12.4%) were remained, and the 10 cases of them are HR-HPV types including genotype 33, 45, 16, 35, and 52. Among the 1,119 women who tested negative at the baseline, 54 women (5%) exhibited new HPV infections at the followup. The most frequent HPV genotypes found in new infection cases were genotypes 39, 52, 16, 51, and 58 (Table 2).
Table 2.
HPV genotype distribution of 1,224 participants at the baseline and their changes at follow-up
| HPV type | Total | HPV positive at baseline (n=105) |
HPV negative at baseline (n=1,119) |
||
|---|---|---|---|---|---|
| Persistence at follow-upa) | Clearance at follow-upa) | Reinfection at follow-upa) | Incidence at follow-upa) | ||
| Alla) | 105 | 13 (12.4) | 92 (87.6) | 12 (11.4) | 54 (4.8) |
| High risk | 90 | 10 (11.1) | 80 (88.9) | 9 (8.6) | 47 (4.2) |
| HPV 16 | 10 | 2 (20.0) | 8 (80.0) | 0 | 6 (0.5) |
| HPV 18 | 5 | 0 | 5 (100) | 0 | 3 (0.3) |
| HPV 31 | 1 | 0 | 1 (100) | 0 | 3 (0.3) |
| HPV 33 | 3 | 1 (33.3) | 2 (66.7) | 0 | 0 |
| HPV 35 | 5 | 1 (20.0) | 4 (80.0) | 0 | 0 |
| HPV 39 | 10 | 1 (10.0) | 9 (90.0) | 1 (1.0) | 7 (0.6) |
| HPV 45 | 4 | 1 (25.0) | 3 (75.0) | 1 (1.0) | 1 (0.1) |
| HPV 51 | 11 | 0 | 11 (100) | 1 (1.0) | 6 (0.5) |
| HPV 52 | 15 | 3 (20.0) | 12 (80.0) | 4 (3.8) | 7 (0.6) |
| HPV 56 | 12 | 1 (8.3) | 11 (91.7) | 1 (1.0) | 4 (0.4) |
| HPV 58 | 6 | 0 | 6 (100) | 0 | 6 (0.5) |
| HPV 59 | 1 | 0 | 1 (100) | 0 | 2 (0.2) |
| HPV 68 | 7 | 0 | 7 (100) | 1 (1.0) | 2 (0.2) |
| Low risk | 90 | 7 (7.8) | 83 (92.2) | 8 (7.6) | 48 (4.3) |
| HPV 6 | 3 | 0 | 3 (100) | 0 | 0 |
| HPV 40 | 2 | 0 | 2 (100) | 0 | 0 |
| HPV 42 | 1 | 1 (100) | 0 | 1 (1.0) | 2 (0.2) |
| HPV 54 | 5 | 1 (20.0) | 4 (80.0) | 1 (1.0) | 3 (0.3) |
| HPV 53 | 15 | 1 (6.7) | 14 (94.3) | 0 | 8 (0.7) |
| HPV 55 | 6 | 1 (16.7) | 5 (83.3) | 2 (1.9) | 2 (0.2) |
| HPV 61 | 3 | 1 (33.3) | 2 (66.7) | 1 (1.0) | 4 (0.4) |
| HPV 62 | 11 | 1 (9.1) | 10 (98.9) | 1 (1.0) | 4 (0.4) |
| HPV 66 | 15 | 0 | 15 (100) | 0 | 1 (0.1) |
| HPV 70 | 10 | 0 | 10 (100) | 1 (1.0) | 2 (0.2) |
| HPV 71 | 4 | 0 | 4 (100) | 1 (1.0) | 2 (0.2) |
| HPV 72 | 2 | 0 | 2 (100) | 0 | 1 (0.1) |
| HPV 81 | 4 | 0 | 4 (100) | 0 | 6 (0.5) |
| HPV 83 | 1 | 0 | 1 (100) | 0 | 3 (0.3) |
| HPV 84 | 6 | 1 (16.7) | 5 (83.3) | 0 | 6 (0.5) |
| CP6108 | 2 | 0 | 2 (100) | 0 | 2 (0.2) |
Values are presented as number (%).
Same women can be counted more than once because of multiple infections.
Persistent HPV infections were relatively common among unmarried women, women with ≥ 2 more sexual partners during their lifetime, and women with a family history of cancer. Cleared and new infections were relatively common among women with a history of a sexually transmitted disease or Chlamydia infection. Persistent and new infections were more common in Busan, compared to Suwon (Table 3). After adjusting for all potential factors, having ≥ 2 sexual partners exhibited a marginally significant association with new HPV infections (OR, 2.0; 95% CI, 1.0 to 3.9). No factors were significantly associated with HPV persistence and clearance (Table 4).
Table 3.
Factors associated with type specific HPV persistence, clearance, and incidencea)
| Characteristic | Persistent HPV (n=13) |
Overall HPV (n=92) |
Incident HPV (n=54) |
|
|---|---|---|---|---|
| No. (%) | No. (%) | No. (%) | p-value | |
| Region | ||||
| Busan | 10 (76.9) | 46 (50.0) | 42 (77.8) | < 0.001 |
| Suwon | 3 (23.1) | 46 (50.0) | 12 (22.2) | |
| Age group (yr) | ||||
| < 39 | 2 (15.4) | 24 (26.1) | 10 (18.5) | 0.31 |
| 40-49 | 2 (15.4) | 35 (38.0) | 25 (46.3) | |
| 50-59 | 8 (61.5) | 27 (29.4) | 16 (29.6) | |
| ≥ 60 | 1 (7.7) | 6 (6.5) | 3 (5.6) | |
| Marital status | ||||
| Unmarried | 6 (46.2) | 19 (20.6) | 8 (14.8) | 0.036 |
| Married | 7 (53.9) | 73 (79.4) | 46 (85.2) | |
| Educational level | ||||
| None/Elementary/Middle school | 9 (69.2) | 39 (42.4) | 23 (42.6) | 0.19 |
| High school/University/≥ Master | 4 (30.7) | 53 (57.6) | 31 (57.4) | |
| Smoking status | ||||
| Nonsmoker | 12 (92.3) | 86 (95.9) | 53 (98.2) | 0.352 |
| Smoker | 1 (7.7) | 6 (4.1) | 1 (1.8) | |
| Alcohol drinking | ||||
| No | 8 (61.5) | 58 (63.1) | 34 (62.9) | 0.201 |
| Yes | 5 (38.5) | 34 (36.9) | 20 (37.1) | |
| Lifetime sexual partners | ||||
| 1 | 8 (61.5) | 64 (70.3) | 38 (71.7) | < 0.001 |
| ≥ 2 | 5 (38.5) | 27 (29.7) | 15 (28.3) | |
| Parity | ||||
| 1 | 2 (16.6) | 9 (11.1) | 6 (11.3) | 0.393 |
| 2 | 5 (41.7) | 47 (58.0) | 29 (54.7) | |
| ≥ 3 | 5 (41.7) | 25 (30.9) | 18 (34.0) | |
| Hormone therapy use | ||||
| Never user | 9 (100) | 31 (81.6) | 20 (83.3) | 0.478 |
| Ever user | 0 | 7 (18.4) | 4 (16.7) | |
| History of STD | ||||
| No | 12 (100) | 85 (92.4) | 49 (90.7) | 0.078 |
| Yes | 0 | 7 (7.6) | 5 (9.3) | |
| Family history of cancer | ||||
| No | 5 (38.5) | 57 (62.0) | 29 (53.7) | 0.021 |
| Yes | 8 (61.5) | 35 (38.0) | 25 (46.3) | |
| Chlamydia trachomatis at baseline | ||||
| Negative | 13 (100) | 82 (90.1) | 49 (94.2) | 0.019 |
| Positive | 0 | 9 (9.9) | 3 (5.8) | |
HPV, human papillomavirus; STD, sexual transmitted disease.
Sample sizes for individual characteristics may not equal total due to missing values.
Table 4.
ORs and 95% CI of potential factors associated with HPV persistence, and incidence
| Characteristic | HPV positive at baseline |
HPV negative at baseline |
||||
|---|---|---|---|---|---|---|
| Total HPVa) (n=105) | Persistent HPV (n=13) |
Adjusted OR |
Total HPVa) (n=1,119) | Incident HPVa) (n= 54) |
Adjusted OR |
|
| No. (%) | OR (95% CI) | No. (%) | OR (95% CI) | |||
| Age group (yr) | ||||||
| < 39 | 26 | 2 (7.7) | Ref | 197 | 10 (5.1) | Ref |
| 40-49 | 37 | 2 (5.4) | 1.0 (0.1-8.8) | 492 | 25 (5.1) | 1.2 (0.5-3.9) |
| 50-59 | 35 | 8 (22.7) | 4.6 (0.7-29.0) | 366 | 16 (4.4) | 1.0 (0.4-2.4) |
| ≥ 60 | 7 | 1 (14.3) | 3.4 (0.3-60.1) | 64 | 3 (4.7) | 1.1 (0.3-4.2) |
| Smoking status | ||||||
| Non-smoker | 98 | 12 (12.2) | Ref | 1,074 | 53 (4.9) | Ref |
| Current smoker | 7 | 1 (14.3) | 1.7 (0.1-21.7) | 44 | 1 (2.3) | 0.3 (0.1-2.4) |
| Lifetime sexual partners | ||||||
| 1 | 72 | 8 (11.6) | Ref | 931 | 38 (4.1) | Ref |
| ≥ 2 | 32 | 5 (15.6) | 1.6 (0.4-7.0) | 185 | 15 (8.1) | 2.0 (1.0-3.9) |
| Family history of cancer | ||||||
| No | 62 | 5 (8.1) | Ref | 747 | 29 (3.9) | Ref |
| Yes | 43 | 8 (18.6) | 4.0 (0.9-17.2) | 371 | 25 (6.7) | 1.7 (0.9-3.1) |
| History of STD | ||||||
| No | 97 | 12 (13.4) | Ref | 1,058 | 49 (4.6) | Ref |
| Yes | 7 | 0 | - | 45 | 5 (11.1) | 2.3 (0.8-6.2) |
| Chlamydia trachomatis at baseline | ||||||
| Negative | 95 | 13 (13.7) | Ref | 1,056 | 49 (4.6) | Ref |
| Positive | 9 | 0 | - | 36 | 3 (8.3) | 1.3 (0.3-5.5) |
Adjustment was done using all variable presented in this table except region. OR, odds ratio; CI, confidence interval; HPV, human papillomavirus; STD, sexually transmitted diseases.
Sample sizes for individual characteristics may not equal to total due to missing values.
Discussion
The present study provided information regarding HPV genotype-specific infections and their change patterns among Korean women. These data are important, because relevant data are sparse in this population, despite the prevalence of HPV infection and incidence of cervical cancer. Furthermore, ours is the first report regarding the natural history of HPV infection among Korean women who visited clinics or hospitals for routine health examinations (e.g., cervical cancer screening), rather than for the diagnosis or treatment of gynecological symptoms. Moreover, we performed both HPV LA and HPV genotyping to confirm the HPV type-specific changes that occurred during the course of the patients’ infections.
Most infections (87.6%) were cleared within 2 years, although 5% of women developed new HPV infections during this time. These results are consistent with findings from previous reports, which suggested that up to 90% of incident infections are cleared within 2 years [5], and that the estimated half-life of HR-HPV infections is 8-10 months [6]. However, HPV persistency varies according to country, and our results revealed a lower persistency (12.4%), compared to results from previous studies in Brazil (19.2%) [9], Italy (49.1%) [16], Denmark (31.4% [21] and 26.9% [12]), the United States (39%) [10], and the Netherlands (44.1%) [22]. These differences may be related to differences in the target populations, who may have different potential risks for persistent infection, and/or differences in the baseline and follow-up testing interval. Nevertheless, the result from a meta-analysis on the patterns of HPV persistence worldwide, the persistence rate tends to decrease with time passed after infection [23]. The association between age and HPV persistence remains controversial. A review of the natural history of HPV infection suggests that age indirectly affects HPV persistence [24], while others studies have reported that younger age is associated with an increased risk of persistence [9,21]. Our results were similar to the persistence rate among young Korean women (17-26 years), despite the differences in the study populations’ ages and the higher rate of new HPV infections among young Korean women [8]. The present study also revealed that the most persistent HPV type was HPV 33, which was followed by genotypes 45, 16, 35, and 52. These results are different with the findings from previous studies, which revealed that HPV 16 and 18 were the most prevalent incident and persistent HPV types [9,16,21,23].
After adjusting for potential risk factors, we did not observe any significant associations with HPV persistence. Some studies have revealed similar findings, although other studies have revealed significant positive [11,12,16,25] or inverse [9,21] associations between age and HPV persistence, including a large retrospective study of Korean women. Another study found that smokers were likely to have persistent HPV infections [22]. In the present study, the number of sexual partners was the only factor to exhibit a marginal association with new HPV infections, and this result is similar to the findings from previous studies [26-28]. The current findings including distributions of HPV genotype-specific infections and their change patterns among Korean women may help improve our understanding of the natural history of HPV infection in the same populations, and facilitate the development of prophylactic vaccines for specific populations.
The present study has several limitations that warrant consideration. First, there is the possibility of selection bias, based on the low follow-up participation rate. However, the participants exhibited similar characteristics at the baseline and follow-up testing, although HPV positivity was slightly more common at the follow-up (10.1%), compared to the baseline (7.7%) (S1 Table). These differences are unlikely to have significantly influenced our findings. Second, the small samples of women who were followed-up and women with HPV (n=105) might have influenced the absence of significant associations between HPV persistence and the potential risk factors in the multivariate analyses. Furthermore, the number of sexual partners not during the last two years when participants followed up but during their life time was included as one of important factors involving HPV infection status and their change. It could be linked to insignificant results on the association between sexual behaviors and change of HPV infection status. Nevertheless, our results regarding HPV change patterns evaluated a large number of Korean women at the baseline (n=4,558), and lifetime sexual behavior could represent overall tendency of sexual behaviors even if it is not the specific sexual behaviors change during the time followed up. Third, detailed data regarding the natural history of HPV infection should be obtained using long-term studies with repeated measurements over shorter intervals (e.g., every 6 months or every year), and we only evaluated HPV infection status after a 2-year interval. Also, information on further diagnosis and treatment such as Pap smear, colposcopic biopsy, and laser therapy during the follow up periods, which might be important factors associated with change of HPV infection status, were not available in this study. Fourth, HPV genotyping was only performed for HPV LA-positive cases at the baseline, although there was disagreement between the test results from HPV LA (6.0%) and HPV HC2 (7.0%) (data not shown). However, the correlation of HPV LA with HR HPV positivity is higher than that with HPV HC2, and this level of disagreement is likely acceptable, based on previously reported results [29,30].
In conclusion, the present study provided information regarding changes in HPV status over a 2-year interval among Korean women. Most infections resolved spontaneously, and only small fractions of the women experienced persistent infections or new HPV infections. The predominant persistent HPV genotypes were different in our study, compared to those from previous studies. We also found a marginally significant association between sexual behavior and HPV infection, but not with HPV persistence or clearance. Further large-scale studies are needed to better understand the natural history of HPV infections and the factors that are associated with HPV type-specific change patterns.
Acknowledgments
This study was supported by research grants from the National Cancer Center (No. 0410130, 0710140, 1610200), Republic of Korea.
Footnotes
Conflict of interest relevant to this article was not reported.
Electronic Supplementary Material
Supplementary materials are available at Cancer Research and Treatment website (http://www.e-crt.org).
References
- 1.Clifford G, Franceschi S, Diaz M, Munoz N, Villa LL. Chapter 3: HPV type-distribution in women with and without cervical neoplastic diseases. Vaccine. 2006;24 Suppl 3:S3/26-34. doi: 10.1016/j.vaccine.2006.05.026. [DOI] [PubMed] [Google Scholar]
- 2.Peto J, Gilham C, Deacon J, Taylor C, Evans C, Binns W, et al. Cervical HPV infection and neoplasia in a large populationbased prospective study: the Manchester cohort. Br J Cancer. 2004;91:942–53. doi: 10.1038/sj.bjc.6602049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Munoz N, Castellsague X, de Gonzalez AB, Gissmann L. Chapter 1: HPV in the etiology of human cancer. Vaccine. 2006;24 Suppl 3:S3/1-10. doi: 10.1016/j.vaccine.2006.05.115. [DOI] [PubMed] [Google Scholar]
- 4.Kim J, Kim BK, Lee CH, Seo SS, Park SY, Roh JW. Human papillomavirus genotypes and cofactors causing cervical intraepithelial neoplasia and cervical cancer in Korean women. Int J Gynecol Cancer. 2012;22:1570–6. doi: 10.1097/IGC.0b013e31826aa5f9. [DOI] [PubMed] [Google Scholar]
- 5.Bosch FX, Burchell AN, Schiffman M, Giuliano AR, de Sanjose S, Bruni L, et al. Epidemiology and natural history of human papillomavirus infections and type-specific implications in cervical neoplasia. Vaccine. 2008;26 Suppl 10:K1–16. doi: 10.1016/j.vaccine.2008.05.064. [DOI] [PubMed] [Google Scholar]
- 6.Castellsague X. Natural history and epidemiology of HPV infection and cervical cancer. Gynecol Oncol. 2008;110(3 Suppl 2):S4–7. doi: 10.1016/j.ygyno.2008.07.045. [DOI] [PubMed] [Google Scholar]
- 7.Syrjanen S, Shabalova I, Petrovichev N, Podistov J, Ivanchenko O, Zakharenko S, et al. Age-specific incidence and clearance of high-risk human papillomavirus infections in women in the former Soviet Union. Int J STD AIDS. 2005;16:217–23. doi: 10.1258/0956462053420211. [DOI] [PubMed] [Google Scholar]
- 8.Oh JK, Ju YH, Franceschi S, Quint W, Shin HR. Acquisition of new infection and clearance of type-specific human papillomavirus infections in female students in Busan, South Korea: a follow-up study. BMC Infect Dis. 2008;8:13. doi: 10.1186/1471-2334-8-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosa MI, Fachel JM, Rosa DD, Medeiros LR, Igansi CN, Bozzetti MC. Persistence and clearance of human papillomavirus infection: a prospective cohort study. Am J Obstet Gynecol. 2008;199:617. doi: 10.1016/j.ajog.2008.06.033. [DOI] [PubMed] [Google Scholar]
- 10.Ralston Howe E, Li Z, McGlennen RC, Hellerstedt WL, Downs LS Jr. Type-specific prevalence and persistence of human papillomavirus in women in the United States who are referred for typing as a component of cervical cancer screening. Am J Obstet Gynecol. 2009;200:245. doi: 10.1016/j.ajog.2008.10.050. e1-7. [DOI] [PubMed] [Google Scholar]
- 11.Louvanto K, Rintala MA, Syrjanen KJ, Grenman SE, Syrjanen SM. Genotype-specific persistence of genital human papillomavirus (HPV) infections in women followed for 6 years in the Finnish Family HPV Study. J Infect Dis. 2010;202:436–44. doi: 10.1086/653826. [DOI] [PubMed] [Google Scholar]
- 12.Nielsen A, Kjaer SK, Munk C, Osler M, Iftner T. Persistence of high-risk human papillomavirus infection in a populationbased cohort of Danish women. J Med Virol. 2010;82:616–23. doi: 10.1002/jmv.21750. [DOI] [PubMed] [Google Scholar]
- 13.Ye J, Cheng X, Chen X, Ye F, Lu W, Xie X. Short-term typespecific HPV persistence and its predictors in an asymptomatic general female population in Zhejiang, China. Int J Gynaecol Obstet. 2010;110:217–22. doi: 10.1016/j.ijgo.2010.03.040. [DOI] [PubMed] [Google Scholar]
- 14.Marks M, Gravitt PE, Gupta SB, Liaw KL, Tadesse A, Kim E, et al. Combined oral contraceptive use increases HPV persistence but not new HPV detection in a cohort of women from Thailand. J Infect Dis. 2011;204:1505–13. doi: 10.1093/infdis/jir560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miranda PM, Silva NN, Pitol BC, Silva ID, Lima-Filho JL, Carvalho RF, et al. Persistence or clearance of human papillomavirus infections in women in Ouro Preto, Brazil. Biomed Res Int. 2013;2013:578276. doi: 10.1155/2013/578276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sammarco ML, Del Riccio I, Tamburro M, Grasso GM, Ripabelli G. Type-specific persistence and associated risk factors of human papillomavirus infections in women living in central Italy. Eur J Obstet Gynecol Reprod Biol. 2013;168:222–6. doi: 10.1016/j.ejogrb.2013.01.012. [DOI] [PubMed] [Google Scholar]
- 17.Schmeink CE, Massuger LF, Lenselink CH, Quint WG, Witte BI, Berkhof J, et al. Prospective follow-up of 2,065 young unscreened women to study human papillomavirus incidence and clearance. Int J Cancer. 2013;133:172–81. doi: 10.1002/ijc.27986. [DOI] [PubMed] [Google Scholar]
- 18.Bae JH, Lee SJ, Kim CJ, Hur SY, Park YG, Lee WC, et al. Human papillomavirus (HPV) type distribution in Korean women: a meta-analysis. J Microbiol Biotechnol. 2008;18:788–94. [PubMed] [Google Scholar]
- 19.Jung KW, Won YJ, Kong HJ, Oh CM, Cho H, Lee DH, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2012. Cancer Res Treat. 2015;47:127–41. doi: 10.4143/crt.2015.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oh JK, Franceschi S, Kim BK, Kim JY, Ju YH, Hong EK, et al. Prevalence of human papillomavirus and Chlamydia trachomatis infection among women attending cervical cancer screening in the Republic of Korea. Eur J Cancer Prev. 2009;18:56–61. doi: 10.1097/CEJ.0b013e328305a0a6. [DOI] [PubMed] [Google Scholar]
- 21.Stensen S, Kjaer SK, Jensen SM, Frederiksen K, Junge J, Iftner T, et al. Factors associated with type-specific persistence of high-risk human papillomavirus infection: a population-based study. Int J Cancer. 2016;138:361–8. doi: 10.1002/ijc.29719. [DOI] [PubMed] [Google Scholar]
- 22.Schmeink CE, Melchers WJ, Siebers AG, Quint WG, Massuger LF, Bekkers RL. Human papillomavirus persistence in young unscreened women, a prospective cohort study. PLoS One. 2011;6:e27937. doi: 10.1371/journal.pone.0027937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mollers M, Boot Hein J, Vriend Henrike J, King Audrey J, van den Broek Ingrid VF, van Bergen Jan EA, et al. Prevalence, incidence and persistence of genital HPV infections in a large cohort of sexually active young women in the Netherlands. Vaccine. 2013;31:394–401. doi: 10.1016/j.vaccine.2012.10.087. [DOI] [PubMed] [Google Scholar]
- 24.Moscicki AB, Schiffman M, Burchell A, Albero G, Giuliano AR, Goodman MT, et al. Updating the natural history of human papillomavirus and anogenital cancers. Vaccine. 2012;30 Suppl 5:F24–33. doi: 10.1016/j.vaccine.2012.05.089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Syrjanen S, Shabalova I, Petrovichev N, Kozachenko V, Zakharova T, Pajanidi J, et al. Factors predicting persistence of high-risk human papillomavirus (HPV) infections in women prospectively followed-up in three New Independent States (NIS) of the former Soviet Union. Eur J Gynaecol Oncol. 2005;26:491–8. [PubMed] [Google Scholar]
- 26.Castellsague X, Bosch FX, Munoz N, Meijer CJ, Shah KV, de Sanjose S, et al. Male circumcision, penile human papillomavirus infection, and cervical cancer in female partners. N Engl J Med. 2002;346:1105–12. doi: 10.1056/NEJMoa011688. [DOI] [PubMed] [Google Scholar]
- 27.International Collaboration of Epidemiological Studies of Cervical Cancer Cervical carcinoma and sexual behavior: collaborative reanalysis of individual data on 15,461 women with cervical carcinoma and 29,164 women without cervical carcinoma from 21 epidemiological studies. Cancer Epidemiol Biomarkers Prev. 2009;18:1060–9. doi: 10.1158/1055-9965.EPI-08-1186. [DOI] [PubMed] [Google Scholar]
- 28.Moscicki AB, Schiffman M, Kjaer S, Villa LL. Chapter 5: Updating the natural history of HPV and anogenital cancer. Vaccine. 2006;24 Suppl 3:S3/42-51. doi: 10.1016/j.vaccine.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 29.Gravitt PE, Schiffman M, Solomon D, Wheeler CM, Castle PE. A comparison of linear array and hybrid capture 2 for detection of carcinogenic human papillomavirus and cervical precancer in ASCUS-LSIL triage study. Cancer Epidemiol Biomarkers Prev. 2008;17:1248–54. doi: 10.1158/1055-9965.EPI-07-2904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cook DA, Mei W, Smith LW, van Niekerk DJ, Ceballos K, Franco EL, et al. Comparison of the Roche cobas(R) 4800 and Digene Hybrid Capture(R) 2 HPV tests for primary cervical cancer screening in the HPV FOCAL trial. BMC Cancer. 2015;15:968. doi: 10.1186/s12885-015-1959-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


