Abstract
Background
Cenani-Lenz Syndactyly (CLS) syndrome is a rare autosomal recessive disorder characterized by syndactyly and oligodactyly of fingers and toes, disorganization and fusion of metacarpals, metatarsals and phalanges, radioulnar synostosis and mesomelic shortness of the limbs, with lower limbs usually being much less affected than upper limbs.
Case presentation
we report here two patients, born to consanguineous Sri Lankan parents, present with bilateral postaxial oligodactyly limited to upper limbs. While the proband has no noticeable facial dysmorphism, renal impairments or cognitive impairments, his affected sister displays a few mild facial dysmorphic features. Whole exome sequencing of the proband showed a novel deleterious homozygous mutation (c.1348A > G) in the LRP4 gene, resulting in an Ile450-to-Val (I450V) substitution.
Conclusion
This recessive mutation in LRP4 confirmed the diagnosis of CLS syndrome in two patients present with isolated hand syndactyly. This is the first reported case of CLS syndrome in a family of Sri Lankan origin.
Electronic supplementary material
The online version of this article (10.1186/s12881-018-0646-1) contains supplementary material, which is available to authorized users.
Keywords: Cenani-Lenz syndactyly syndrome, Whole exome sequencing, LRP4 gene
Background
Cenani-Lenz Syndactyly syndrome (CLS, OMIM 212780) is a rare autosomal recessive disorder characterized by syndactyly and oligodactyly of fingers and toes, disorganization and fusion of metacarpals, metatarsals and phalanges, radioulnar synostosis and mesomelic shortness of the upper limbs, with lower limbs usually being much less severely affected than upper limbs [1–3]. It was first described in 1967 in two bothers with total syndactyly of the hands (‘spoon hands’), bilateral radioulnar synostosis and metacarpal fusion [1]. Facial involvement includes a prominent forehead, hypertelorism, downslanting palpebral fissures and micrognathia [4]. There have also been reports of renal hypoplasia or agenesis in over 50% of CLS families [5, 6]. The genetic etiology of CLS has been mapped to CLS1 locus on chromosome region 11p11.2–q13.1 and is thought to result from homozygous or compound heterozygous mutations in the LRP4 gene [6, 7]. The encoded protein LRP4 (OMIM 604270) belongs to the family of low-density lipoprotein (LDL) receptors and acts as an antagonist to LRP5 and LRP6 in the Wnt signaling cascade, a function that is lost when the gene is mutated. Wnt signaling is known to be essential for embryonic limb patterning and kidney development [8, 9]. Here we report the first confirmed CLS family of Sri Lankan origin.
Case presentation
The proband (II.1), a 22-year-old male, was the eldest son of three children born to 1st degree consanguineous parents of Sri Lankan origin (Fig. 1). Pregnancy and delivery were uneventful. He was diagnosed to have bilateral postaxial oligodactyly limited to upper limbs at birth. Radiological studies showed bilateral fusion of the 4th and 5th metacarpal bones (Figs 2 and 3). He has no noticeable facial dysmorphism, renal impairments or cognitive impairments. The second child (II.2), a 16-year-old boy, was normal. The youngest child (II.3), a 13-year-old girl, also has postaxial oligodactyly (Fig. 4) and a few mild facial dysmorphic features. Both patients do not show visible lower limb deformities or oligodactyly. By whole exome sequencing of the proband, we identified a deleterious homozygous mutation in LRP4 c.1348A > G, p.Ile450Val. Mutations in this gene were reported to cause CLS syndrome.
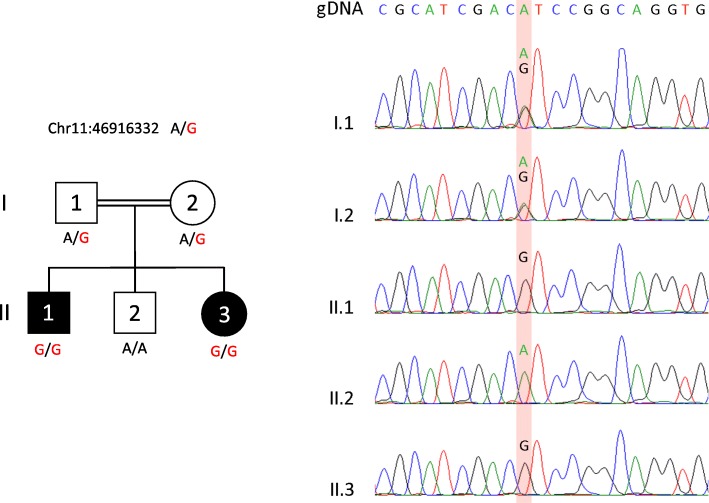
Fig. 1.
Pedigree of a consanguineous Sri Lankan family with two affected siblings with germline homozygous mutation in LRP4 with sanger sequencing results
Fig. 2.
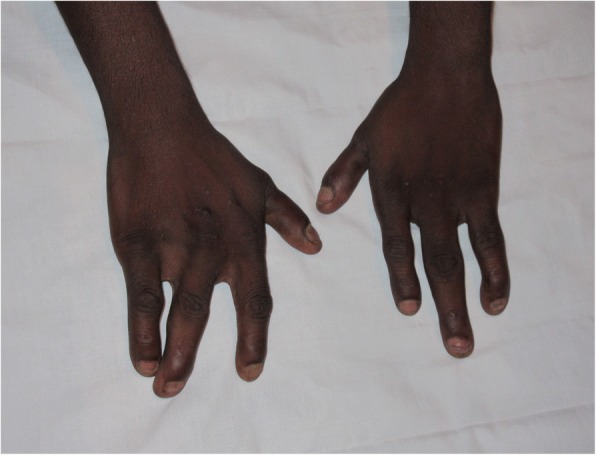
Hand photo of proband II.1 showing bilateral Syndactyly
Fig. 3.

X- ray findings of the proband II.1 with fused 4th and 5th metatarsal bones
Fig. 4.
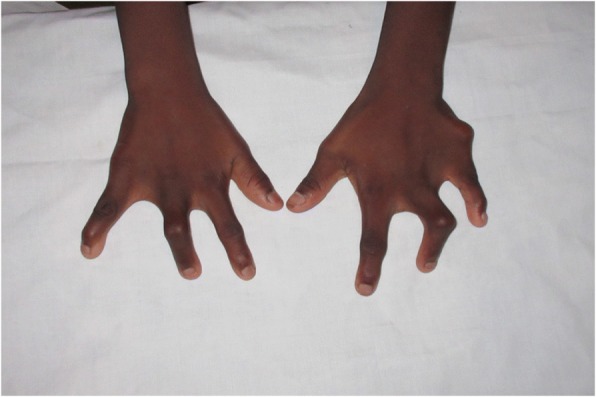
Hand photo of patient II.3 showing similar deformity as proband II.1
Whole exome sequencing (WES) method and results
Following written informed consent from the proband and the family, genomic DNA was obtained from venous blood from each member. One microgram of genomic DNA per sample was used for exome capture with Agilent Technologies SureSelectXT All Human ExonV6 Kit. DNA was sheared to target an average fragment size of 200 bp and amplified as per SureSelect protocol. The exome library was prepared on an Ion OneTouch System and sequenced on an Ion Proton instrument (Life Technologies, Carlsbad, CA, USA) using one Ion PI chip.
Sequence reads were aligned to the human reference genome (Human GRCh37 (hg19) build) using Torrent Mapping Alignment Program (TMAP) from the Torrent Suite (v5.0.2). The variants were called using the Torrent Variant Caller (TVC) plugin (v5.0.2), and were annotated with the associated gene, location, quality-score, coverage, predicted functional consequences, protein position and amino acid changes, SIFT [10], PolyPhen2 [11], Grantham [12] and M-CAP [13] prediction scores, phyloP conservation scores [14] and 5000 genomes Minor Allele Frequencies. Variants were filtered for common SNPs using the NCBI’s “common and no known medical impacts” database (ftp://ftp.ncbi.nlm.nih.gov/pub/clinvar/vcf_GRCh37/) and the Exome Aggregation Consortium (ftp://ftp.broadinstitute.org/pub/ExAC_release/release0.2/). We next removed variants that were present in greater than 1% of the previously 534 sequenced samples.
For the proband analysis, 16.7 Gb were sequenced with an average read length of 177 bp. An average coverage of 196× was achieved over the exome with 97% of the bases covered at least 20 × .
A total of 949 heterozygous, compound heterozygous and homozygous variants were identified across protein-coding exons, UTRs, splice sites and flanking introns (Additional file 1: Table S1). Based on the fact that the two affected siblings, male and female, were born to consanguineous parents, we favored an autosomal recessive mode of inheritance. Only 44 homozygous variants remained, including 12 that were exonic. Based on the Genome Aggregation Database (gnomAD, http://gnomad.broadinstitute.org/), 4 out of the 12 exonic variants have not been identified in population, including a novel missense mutation in LRP4 (c.1348A > G, p.Ile450Val). This variant was also not detected in our “in-house” database containing WES results of 534 patients who mainly originated from Middle-East. We predicted this variant to be pathogenic since its M-CAP score was 0.103, which is superior to the recommended pathogenicity threshold of 0.025 [13] (Additional file 1: Table S1). Moreover, the change of Isoleucine into Valine (p.Ile450Val) is expected to be deleterious since this amino-acid is highly conserved throughout evolution. Finally, mutations in LRP4 were previously reported to cause Cenani-Lenz Syndactyly syndrome, supporting our finding. Using Sanger sequencing, this germline mutation was confirmed to segregate with the disease in all 5 family members (Fig. 1).
Discussion and conclusion
Cenani-Lenz syndrome is a rare autosomal recessive disorder characterized by syndactyly and oligodactyly of fingers and toes. One gene underlying syndactyly is low-density lipoprotein receptor-related protein 4 (LRP4; OMIM 604270; RefSeq: NR_038909.1). Specifically, variants in the LRP4 gene are responsible for Cenani-Lenz syndrome (CLS; OMIM 212780) and Sclerosteosis 2 (OMIM 614305). CLS is characterized by bilateral complex syndactyly of the hands (carpal, metacarpal and digital synostoses, disorganization of the carpal bones, digital reduction) and feet (toe syndactyly, metatarsal fusion, absent metatarsals), renal abnormalities, and dysmorphic facial features [1, 4, 15].
In this family two of the three siblings had shown isolated hand syndactyly with no lower limb or renal involvement. Thus far, variants in the LRP4 gene have been reported only in one child with isolated hand syndactyly in literature. It has been recently suggested that variants in the fourth β-propeller of the extracellular protein domain may cause a phenotype distinct from previously characterized LRP4 variants, which has a more diverse phenotypic variation [16]. The genetic basis of several types of isolated Syndactyly has been identified but the genes underlying isolated syndactyly in many families remain to be discovered [17].
In conclusion we report a deleterious homozygous variant in LRP4 c.1348A > G, p.Ile450Val. This variant may alter the ability of LRP4 to inhibit Wnt signaling, resulting in CLS type syndactyly. Hence our findings suggest that isolated syndactyly is a rare presentation of CLS.
Additional file
Table S1. Variant data – Data related to Whole Exome Sequencing (WES). (XLSX 274 kb)
Acknowledgements
We wish to acknowledge the referring doctor and the laboratory staff for their contribution. This work was partly funded by a Strategic Positioning Fund for the Genetic Orphan Diseases program and an Industry Alignment Fund for the Singapore Childhood Undiagnosed Disease program from the A*STAR (Agency for Science, Technology and Research) Biomedical Research Council in Singapore.
Funding
No direct funding for this project.
Availability of data and materials
Data is not available in a public domain it will be shared on request from interested parties upon writing to the corresponding author.
Authors’ contributions
DH, SMAJ and VHWD were the clinicians looking after the patient. ST, AYJN and BV carried out WES and variant prediction. CB performed WES analysis and identified LRP4. BR and RS designed the study. DH wrote the first draft of the manuscript with contributions from all. All authors reviewed, modified and approved the final version of the manuscript.
Ethics approval and consent to participate
Ethics approval for the study was obtained by the Faculty of Medicine, University of Colombo Ethics Review Committee (EC-16-179). Duly filled consent forms are available with the corresponding author.
Consent for publication
Written informed consent to publish this material was obtained from the proband and his family.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Footnotes
Electronic supplementary material
The online version of this article (10.1186/s12881-018-0646-1) contains supplementary material, which is available to authorized users.
Contributor Information
Dineshani Hettiaracchchi, Phone: +94777222228, Email: dineshani.sirisena@gmail.com.
Carine Bonnard, Email: carine.bonnard@imb.a-star.edu.sg.
S. M. A. Jayawardana, Email: smajayawardana@gmail.com
Sumanty Tohari, Email: toharis@imcb.a-star.edu.sg.
Byrappa Venkatesh, Email: mcbbv@imcb.a-star.edu.sg.
Bruno Reversade, Email: bruno@reversade.com.
Roshni Singaraja, Email: rsingaraja@tlgm.a-star.edu.sg.
V. H. W. Dissanayake, Email: vajirahwd@hotmail.com
References
- 1.Cenani A, Lenz W. Totale Syndaktylie und totale radioulnare Synostose bie zwei Bruedern. Ein Beitrag zur Genetik der Syndaktylien. Ztschr Kinderheilk. 1967;101:181–190. doi: 10.1007/BF00438491. [DOI] [PubMed] [Google Scholar]
- 2.Elçioglu N, Atasu M, Cenani A. Dermatoglyphics in patients with Cenani–Lenz type syndactyly: studies in a new case. Am J Med Genet. 1997;70:341–345. doi: 10.1002/(SICI)1096-8628(19970627)70:4<341::AID-AJMG1>3.0.CO;2-W. [DOI] [PubMed] [Google Scholar]
- 3.Kariminejad A, et al. Severe Cenani–Lenz syndrome caused by loss of LRP4 function. Am J Med Genet A. 2013;161(6):1475–1479. doi: 10.1002/ajmg.a.35920. [DOI] [PubMed] [Google Scholar]
- 4.Temtamy SA, Ismail S, Nemat A. Mild facial dysmorphism and quasido- minant inheritance in Cenani–Lenz syndrome. Clin Dysmorphol. 2003;12:77–83. doi: 10.1097/00019605-200304000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Jarbhou H, Hamamy H, Al-Hadidy A, Ajilouni K. Cenani–Lenz syndactyly with facial dysmorphism, hypothyroidism, and renal hypo- plasia: a case report. Clin Dysmorphol. 2008;17:269–270. doi: 10.1097/MCD.0b013e328306a6ed. [DOI] [PubMed] [Google Scholar]
- 6.Li Y, Pawlik B, Elcioglu N, Aglan M, Kayserili H, Yigit G, Percin F, Goodman F, Nürnberg G, Cenani A, Urquhart J, Chung B-D, Ismail S, Amr K, Aslanger AD, Becker C, Netzer C, Scambler P, Eyaid W, Hamamy H, Clayton-Smith J, Hennekam R, Nürnberg P, Herz J, Temtamy SA, Wollnik B. LRP4 mutations alter Wnt/beta-catenin signaling and cause limb and kidney malformations in Cenani–Lenz syndrome. Am J Hum Genet. 2010;86:696–706. doi: 10.1016/j.ajhg.2010.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li Y, et al. LRP4 mutations alter Wnt/β-catenin signaling and cause limb and kidney malformations in Cenani-Lenz syndrome. Am J Hum Genet. 2010;86(5):696–706. doi: 10.1016/j.ajhg.2010.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Petersen CP, Reddien PW. Wnt signaling and the polarity of the primary body axis. Cell. 2009;139:1056–1068. doi: 10.1016/j.cell.2009.11.035. [DOI] [PubMed] [Google Scholar]
- 9.Gallegos TF, Kouznetsova V, Kudlicka K, Sweeney DE, Bush KT, Willert K, Farquhar MG, Nigam SK. A protein kinase a and Wnt-dependent network regulating an intermediate stage in epithelial tubulogenesis during kidney development. Dev Biol. 2012;364:11–21. doi: 10.1016/j.ydbio.2012.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kumar P, Henikoff S, Ng PC. Predicting the effects of coding non-synonymous variants on protein function using the SIFT algorithm. Nat Protoc. 2009;4:1073. doi: 10.1038/nprot.2009.86. [DOI] [PubMed] [Google Scholar]
- 11.Adzhubei IA, et al. A method and server for predicting damaging missense mutations. Nat Methods. 2010;7:248. doi: 10.1038/nmeth0410-248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grantham R. Amino acid difference formula to help explain protein evolution. Science. 1974;185:862. doi: 10.1126/science.185.4154.862. [DOI] [PubMed] [Google Scholar]
- 13.Jagadeesh KA, et al. M-CAP eliminates a majority of variants of uncertain significance in clinical exomes at high sensitivity. Nat Genet. 2016;48(12):1581–1586. doi: 10.1038/ng.3703. [DOI] [PubMed] [Google Scholar]
- 14.Pollard KS, Hubisz MJ, Rosenbloom KR, Siepel A. Detection of nonneutral substitution rates on mammalian phylogenies. Genome Res. 2010;20:110–121. doi: 10.1101/gr.097857.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harpf C, Pavelka M, Hussl H. A variant of Cenani-Lenz syndactyly (CLS): review of the literature and attempt of classification. Br J Plast Surg. 2005;58(2):251–257. doi: 10.1016/j.bjps.2004.10.024. [DOI] [PubMed] [Google Scholar]
- 16.Sukenik Halevy R, et al. Mutations in the fourth β-propeller domain of LRP4 are associated with isolated syndactyly with fusion of the third and fourth fingers. Hum Mutat. 2018;39(6):811–815. doi: 10.1002/humu.23417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Malik S. Syndactyly: phenotypes, genetics and current classification. Eur J Hum Genet. 2012;20(8):817–824. doi: 10.1038/ejhg.2012.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Variant data – Data related to Whole Exome Sequencing (WES). (XLSX 274 kb)
Data Availability Statement
Data is not available in a public domain it will be shared on request from interested parties upon writing to the corresponding author.