Abstract
Background and Aims
Impulsivity impacts adolescent alcohol use. We aimed to prospectively evaluate the cognitive mechanisms outlined in two-factor models and the protective role of coping skills.
Methods
Two cohorts of adolescents followed for three years were included in the study (younger cohort: N = 908, aged 10–12 years at Time 1; older cohort: N = 943, aged 12–15 years at Time 1). Constructs measured included impulsivity (reward drive, rash impulsiveness), positive social alcohol expectancies (PSAE), drinking-refusal self-efficacy (DRSE), problem-based coping skills, family and community risk factors, and alcohol use including the Alcohol Use Disorders Identification Test (AUDIT).
Results
Data were analysed using structural equation modelling controlling for family and community risk factors, testing mediation and moderation. Impulsivity traits predicted cognitive mechanisms and these in turn predicted alcohol use in both cohorts (χ2 = 1,139.79, df = 249, p < .001, CFI = .92, SRMR = .06, RMSEA = .04). DRSE and PSAE mediated the effects of rash impulsiveness and reward drive, respectively, on alcohol use. Problem-based coping skills moderated several pathways to drinking within each cohort, being protective even when adolescents have low DRSE, and buffering the impact of PSAE on alcohol use.
Conclusions
The current study details the prospective interactive influences of impulsivity and cognitive risk factors on adolescent alcohol use. The findings have direct implications for prevention and treatment programs, providing information about possible high-impact targets for intervention.
Introduction
Early alcohol use is a pervasive problem in a number of Western societies. Adolescents in North America, Australia, and Europe have a high prevalence of alcohol use, alcohol-related problems, and mortality [1–3]. Due to the trajectory of alcohol use from adolescence to adulthood [4,5], prevention of alcohol misuse through identification and targeting of key risk factors is a commonly proposed solution to reducing alcohol-related harm. Consequently, there has been a push to identify modifiable psychological risk factors that predict alcohol use in adolescents.
One important psychological risk factor for adolescent alcohol use is impulsivity [6–8]. Impulsivity is a strong predictor of adolescent alcohol use and problematic adolescent alcohol consumption [9]. The adolescent developmental period is associated with increased impulsivity and sensitivity to reward due to rapid neurological changes which occur while the cognitive and emotional regulatory neurological systems are still developing [7,10]. Predominant models of impulsivity propose that it is composed of at least two factors or dual systems: one characterised by reward sensitivity and appetitive motivation, related to lower order mesolimbic dopamine systems (reward drive; RD); and another characterised by difficulty inhibiting approach behaviour in light of negative future consequences, related to higher order prefrontal serotoninergic systems (“rash” impulsiveness; RI; [8,10,11])
Recent studies have tested the hypothesis that the two impulsivity traits have unique effects on alcohol-related cognition; specifically, alcohol expectancies (AE) and drinking-refusal self-efficacy (DRSE) [7,12,13]. AE and DRSE derive from Social Cognitive Theory [14]. AEs reflect an individual’s positive or negative beliefs about the outcomes of drinking. There is evidence that adolescents, in particular, are driven by the expectations of social reward relating to alcohol use [15,16]. DRSE pertains to an individual’s belief in their ability to refrain from drinking alcohol in varying contexts [17]. Both of these cognitive factors are robust predictors of hazardous alcohol use [18–20].
According to the 2-Component Approach to Reinforcing Substances model (2-CARS; [7,13]), RD and RI create separate pathways of alcohol risk mediated through the cognitive factors of AEs and DRSE. RD produces a learning bias for the rewarding/positive outcomes of drinking, which then increases alcohol use and decreases DRSE. In contrast, RI’s impact on alcohol misuse is mediated by reduced DRSE, which then increases alcohol misuse. That is, individuals who know they tend to act without considering the consequences of their actions will be less likely to believe they can refuse alcohol in a tempting situation. This creates a self-fulfilling prophecy that is reinforced when realised. Several studies now empirically support these relationships in a range of populations [21–24].
While these studies have furthered the understanding of the mechanisms of impulsivity on alcohol use, no study has examined prospective mediation of impulsivity-related risk by cognition. Similarly, no study has examined factors that could moderate these relationships and serve as additional targets for prevention. Increased stress and negative affect have been identified as risk factors for increased alcohol consumption in adolescents [7,25]. Coping abilities, defined as how one responds to life stress, have been shown to alter the negative impact of stress on adolescent alcohol use [25,26]. Coping ability has been associated with alcohol-related cognitions, risk taking, reward seeking, and alcohol misuse [27–29]. It is possible that effective coping skills decrease alcohol use through increased behavioural and emotional regulation [25,26]. Thus, we believe that coping skills are a conceptually congruent moderator for the 2-CARS model.
This study prospectively examines the relationships between impulsivity, alcohol-related cognition, and growth in alcohol consumption and hazardous alcohol use in adolescents, controlling for family and community risk factors. We also prospectively examine the moderating effects of coping skills on the relationship between impulsivity, alcohol-related cognition, and growth in alcohol use and hazardous alcohol use in adolescents, controlling for family and community risk factors.
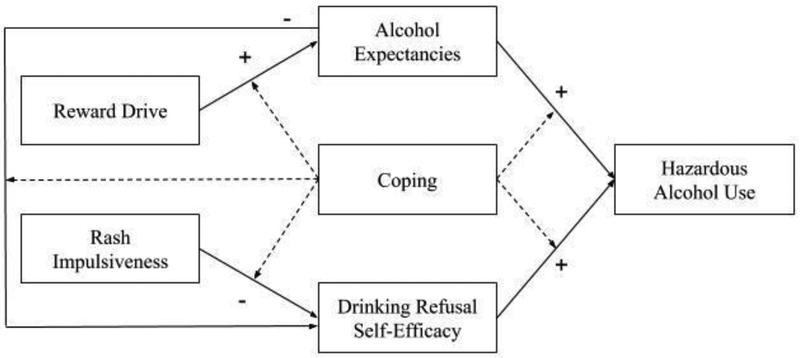
The hypothesized model is depicted in Figure 1. It is hypothesised that (a) DRSE will mediate the relationship between RI and alcohol misuse, (b) AEs will mediate the relationship between RD and alcohol misuse, and (c) DRSE will mediate the relationship between AE and alcohol misuse. It is hypothesised that adolescents with higher problem-solving coping skills will show weaker relationships between the impulsivity factors, cognitive factors, and alcohol use. By gaining a more comprehensive understanding of how alcohol use patterns in adolescents are developed, inferences can be made as to which mechanisms may be most effective to target at different ages.
Figure 1.
A simplified diagrammatic illustration of the hypothesised moderating and mediating relationships between variables in the current study (Note. Dashed lines represent hypothesised moderation effects.)
Methods
Participants
The sample comprised two cohorts of Australian children (N = 1,911) who participated in the International Youth Development Study (IYDS) across three annual time points. The IYDS is an ongoing longitudinal panel survey that began in 2002. A detailed description of the recruitment and data collection processes was given by McMorris, Hemphill, Toumbourou, and Patton [30]. The current study utilised the first three time points for Cohort 1 (younger cohort) and Cohort 2 (older cohort) (see Table 1 for participant information).
Table 1.
Demographic information.
| T1 (2002) | T2 (2003) | T3 (2004) | ||
|---|---|---|---|---|
| Younger Cohort (N =908) |
Age range | 10 – 12 years | 11 – 13 years | 12 – 14 years |
| Age M(SD) years | 10.98(.40) | 11.94(.40) | 12.96(.40) | |
| Grade | 5 | 6 | 7 | |
| Gender - #female (%) | 476 (52.4%) | |||
| Older Cohort (N = 943) |
Age range | 12 – 15 years | 13 – 15 years | 14 – 16 years |
| Age M(SD) years | 12.92(.41) | 13.96(.40) | 14.98(.40) | |
| Grade | 7 | 8 | 9 | |
| Gender - #female (%) | 491 (52.1%) | |||
Measures
Impulsivity.
Rash impulsiveness (RI) was assessed using three impulsivity items from the Australian Temperament Project adaptation of the Revised Behaviour Problem Checklist [31] and the Child Behaviour Checklist for school-aged children [32], e.g., “I answer without thinking about it first” (1 ‘NO!’ to 4 ‘YES!’). Internal consistency for the younger cohort and the older cohort was α = .53 and α = .58, respectively. Reward drive (RD) was measured using the item “How many times have you done what feels good no matter what?” (1 ‘Never’ to 6 ‘Once a week or more’). This item was modified from the Seattle Social Development Project sensation-seeking/disinhibition scale [33].
Alcohol use.
At Time 1, adolescents were assessed on drinking status (‘Never’ drank; drank ‘Once or more’). At Times 2 and 3, both cohorts were asked about their current drinking (30 days), drinking in the past year (1 ‘Never’ to 8 ‘40+ times’) and their binge drinking (occasions of five or more drinks in last two weeks; 1’None’ to 6 ‘10 or more times’). For analysis, these items at Time 2 and 3 were combined into latent factors.
Alcohol-related cognitions.
To measure positive (social) alcohol expectancies students were asked at all three time points “What are the chances you would be seen as cool if you: began drinking regularly, that is, at least once or twice a month?” (1 ‘No or Very Little Chance’ to 5 ‘Very Good Chance’). Drinking refusal self-efficacy was measured at all three time points using the item (DRSE1) “You are at a party at someone’s house, and one of your friends offers you a drink containing alcohol. What would you say or do?” (‘Drink it’ (0) vs. ‘Don’t drink it’ (+1)). The second item (DRSE2) was “Do you think you would handle this situation well: Peer offers you a drink at a party?” (1 ‘NO!’ to 4 ‘YES!’). A product term of DRSE1 and DRSE2 was computed to weight the response to DRSE2 and reflect strength of confidence.
Behavioural coping skills.
At Time 2, students were asked to rate their personal use of adaptive and maladaptive problem-based coping strategies, e.g., “When I have a problem I think about the best ways to handle it.” The four items were scored on a 4-point scale from ‘YES!’ to ‘NO!’ Internal consistency for the younger cohort and the older cohort was α = .59 and α = .62, respectively. Median splits were used to categorise students with “lower” and “higher” coping skills.
Other risk factors.
Family risk factors consisted of family history of antisocial behaviour, family conflict, and poor family management, which are known correlates of adolescent alcohol use [34,35]. Community risk factors were based on community disorganization, laws and norms favourable to drug use, and perceived availability of drugs [36]. These factors are composed from subscales from the Communities That Care family self-report youth survey [37,38]. Composite variables for both overall risk factors were calculated to reduce model complexity [39].
Analytical procedure
The prospective relationships between variables were analysed in Amos (version 22) using structural equation modelling (SEM). A multigroup SEM was used to examine the relationships between impulsivity variables (RI and RD), cognitive variables (positive alcohol expectancies (PSAE) and DRSE), and Time 2 and Time 3 alcohol use in the younger cohort (group 1) and the older cohort (group 2). Time 1 alcohol use, community risk, and family risk were included as covariates. Mediation hypotheses were tested using the bootstrapped indirect effects method [40] and the distribution of the products of coefficients method [41]. The moderation analyses used multigroup (lower vs higher coping skills) SEM for the older and younger cohorts separately. Significance was tested using chi-square difference tests comparing nested models in which paths of interest were constrained to be invariant across coping skill (no moderation) or free to vary (moderation). A reduction in model fit indicates moderation.
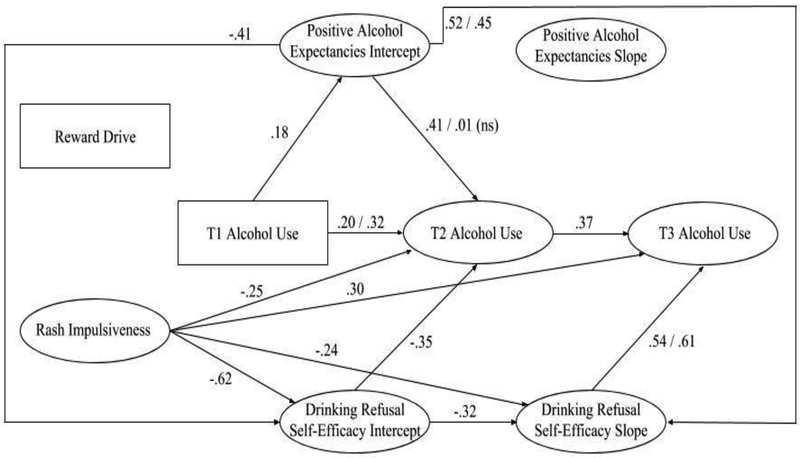
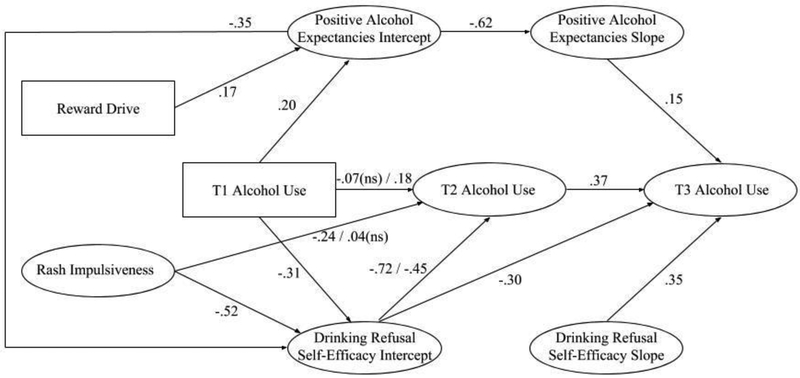
The hypothesised structural model (see Figures 2 and 3) included RD and the latent factor of RI predicting 3-time-point growth curve models of PSAE (positive growth) and DRSE (negative growth) as well as the latent factors of Time 2 and Time 3 alcohol use. PSAE was hypothesised to predict DRSE, and both were hypothesised to predict Time 2 and 3 alcohol use. Time 2 and Time 3 alcohol use residuals were allowed to covary, as were the residuals of PSAE slope, DRSE slope, and Time 2 alcohol use. Family risk and community risk composite variables were calculated and introduced into the model as covariates, with direct paths to Time 2 and Time 3 alcohol use and covariances with RI, RD, Time 1 alcohol use, and each other. These covariances and covariates are not shown in Figures 2 and 3 for clarity of exposition.
Figure 2.
Structural equation modelling analysis for the younger cohort controlling for Time 1 (T1) alcohol use, family risk, and community risk. Only significant paths are shown, p < .05. Paths with two coefficients are moderated by Time 2 (T2) coping (lower coping/higher coping). Note. DRSE slope is negative.
Figure 3.
Structural equation modelling analysis for the older cohort controlling for Time 1 (T1) alcohol use, family risk, and community risk. Only significant paths are shown, p < .05. Paths with two coefficients are moderated by Time 2 (T2) coping (lower coping/higher coping). Note. DRSE slope is negative.
The χ2 test statistic, comparative fit index (CFI), the standardized root mean-square residual (SRMR), and the root mean-square error of approximation (RMSEA) were used to examine model fit. As current recommendations are to view conventional “cut-offs” as guidelines [42], the model was considered as having good fit if the values approached CFI ≥ .95, RMSEA ≤ .06, and SRMR ≤ .08 [43].
Results
Sixty (3.14%) students were removed from the dataset based on negative responses to at least one of the honesty measures for each time point. After deletion, 1,851 students remained. Missing data were imputed using the Expectation Maximisation method in SPSS (version 22).
Alcohol use
Approximately half of the adolescents in both cohorts reported having consumed a full alcoholic beverage at Time 1. In Waves 2 and 3, the older cohort showed higher rates of binge drinking, current drinking, and past-year drinking (see Table 2).
Table 2.
Alcohol use.
| Alcohol use | Younger cohort (N = 908) |
Older cohort (N = 943) |
|
|---|---|---|---|
| T1 | N(%) ever consumed full alcoholic drink | 465 (51.2%) | 553 (58.6%) |
| N(%) ever binge drank | 46 (5.1%) | 170 (17.9%) | |
| T2 | N(%) currently drinking | 231 (25.4%) | 415 (44.0%) |
| N(%) drank in past year | 287 (31.7%) | 531 (56.3%) | |
| N(%) ever binge drank | 69 (7.6%) | 295 (31.4%) | |
| T3 | N(%) currently drinking | 263 (29.0%) | 569 (60.4%) |
| N(%) drank in past year | 334 (36.8%) | 678 (72.0%) |
Prospective structural model fit
The model was analysed as a multigroup (the younger cohort and the older cohort) analysis and showed acceptable to good fit to the data across both cohorts, χ2 = 1,139.79, df = 249, p < .001, CFI = .92, SRMR = .06, RMSEA = .04.
Prospective relationships between predictors and alcohol use
Overall, the results support the hypothesized model across the younger cohort (see Figure 2) and the older cohort (see Figure 3). Higher RI was related to decreased DRSE for both cohorts as well as decreased growth in DRSE for the younger cohort. This, in turn, predicted increased alcohol use, as higher DRSE was related to decreased future alcohol use.
Higher RD was related to increased PSAE for the older cohort but not the younger cohort. Higher PSAE was positively related to alcohol use in both cohorts. For the younger cohort, PSAE at Time 1 predicted increased alcohol use at Time 2. For the older cohort, adolescents with high PSAE at Time 1 had less growth of PSAE over time. This suggests a possible ceiling effect. For this cohort, PSAE growth was associated with increased alcohol use at Time 3. Time 1 (T1) alcohol use predicted Time 2 (T2) alcohol use in the younger cohort but not the older cohort. Time 1 drinking was associated with lower Time 1 DRSE for the older cohort. Time 2 alcohol use positively predicted Time 3 alcohol use in both cohorts.
Mediation analyses
For the younger cohort, DRSE slope mediated the relationship between RI and Time 3 alcohol use, 95% CI [−.146, −.009]; DRSE intercept mediated the relationship between RI and Time 2 alcohol use, 95% CI [.011, .111]; and DRSE intercept mediated the relationship between PSAE intercept and Time 2 alcohol use, 95% CI [.006, .07]. For the older cohort, DRSE intercept mediated the relationship between RI and Time 2 and Time 3 alcohol use, 95% CIs [.196, .518] and [.064, .366], respectively, and DRSE intercept mediated the relationship between PSAE intercept and Time 2 and Time 3 alcohol use, 95% CIs [.07, .185] and [.023, .131], respectively. There was also evidence that RD impacted Time 2 and 3 alcohol use through PSAE and DRSE. RD significantly indirectly affected T2 alcohol use, β = .008, 95% CIs [.003, .016], p = .002. While the direct and indirect effects of RD on Time 3 (T3) alcohol use were not significant, the total effect was, β = .036, 95% CIs [.009, .066]. RI had a larger effect on prospective drinking in the older cohort; RI to T2 alcohol use for the younger cohort, β = −.003, 95% CIs [−.025, .020] and the older cohort, β = .126, 95% CIs [.042, .266]; RI to T3 alcohol use for the younger cohort, β = .039, 95% CIs [.002, .089] and the older cohort, β = .173, 95% CIs [.060, .346].
Moderation analyses
Moderation analyses were conducted for the younger and older cohorts separately. The dichotomised (lower; higher) Time 2 problem-based coping variable was used to run the multigroup SEM analyses (see Table 3 for alcohol use data). Only significant paths were included in the unconstrained models. Each comparison was significantly variant at the model level (see Table 4).
Table 3.
Alcohol use for adolescents with lower and higher coping skills.
| Alcohol use | Younger cohort |
Older cohort |
|||
|---|---|---|---|---|---|
| Lower coping (N = 561) |
Higher coping (N = 347) |
Lower coping (N = 521) |
Higher coping (N = 422) |
||
| T1 | N(%) ever consumed full alcoholic drink |
307 (54.7%) |
158 (45.5%) |
308 (59.1%) |
245 (58.1%) |
| T2 | N(%) ever binge drank | 39 (7%) |
7 (2%) |
110 (21.1%) |
60 (14.2%) |
| N(%) currently drinking | 171 (30.5%) |
60 (17.3%) |
239 (45.9%) |
176 (41.7%) |
|
| N(%) drank in past year | 208 (37.1%) |
79 (22.8%) |
307 (58.9%) |
224 (53.1%) |
|
| T3 | N(%) ever binge drank | 52 (9.3%) |
17 (4.9%) |
183 (35.1%) |
112 (26.5%) |
| N(%) currently drinking | 199 (35.5%) |
64 (18.4%) |
331 (63.5%) |
238 (56.4%) |
|
| N(%) drank in past year | 243 (43.3%) |
91 (26.2%) |
390 (74.9%) |
288 (68.2%) |
|
Table 4.
Overall model level Time 2 coping moderation analyses.
| Unconstrained χ2
(df) |
Constrained χ2
(df) |
Difference (df) |
||
|---|---|---|---|---|
| Younger cohort |
T2 Coping | 697.86 (272) | 830.43 (292) | 132.58 (20)* |
| T3 Coping | 683.75 (270) | 767.88 (292) | 84.13 (22)* | |
| Older cohort |
T2 Coping | 779.76 (270) | 870.25 (290) | 90.49 (20)* |
| T3 Coping | 795.69 (270) | 847.73 (290) | 52.04 (20)* |
Note. Figures are χ2 values.
p < .001
Chi-square difference tests on theoretically relevant paths revealed significant invariances for Time 2 coping skills for the older and younger cohorts (see Table 5; moderated relationships are also represented in Figures 2 and 3). Within the younger cohort, lower coping skills strengthened the effect of higher PSAE on DRSE decline and of PSAE on Time 2 alcohol use, which was nonsignificant for adolescents with higher coping skills. The relationship between RI and Time 2 alcohol use was nonsignificant for adolescents in the older cohort with higher coping skills, and negative for those with lower coping skills. However, it is likely that this unexpected negative association is a statistical artefact caused by the mediation through DRSE, which is supported by the positive total effect of RI on T2 alcohol use for adolescents with lower coping skills, β = .151, 95% CIs [−.033, .495] and higher coping skills, β = .139, 95% CIs [.062, .256]. The path between T1 and T2 alcohol use was stronger for adolescents with higher coping skills for both cohorts. However, the total effects of T1 on T2 alcohol use indicated stronger overall effects for adolescents with lower coping skills in the younger cohort, β = .100, 95% CIs [.068, .142] and the older cohort, β = .309, 95% CIs [.210, .420] compared to those with higher coping skills in the younger cohort, β = .019, 95% CIs [.007, .048] and the older cohort, β = .274, 95% CIs [.196, .362]. Finally, the effect of DRSE decline on Time 3 alcohol use (increased decline predicting increased alcohol use) was weakened for the students with lower coping skills in the younger cohort, and the negative effect of DRSE intercept on Time 2 alcohol use was strengthened for the students with lower coping skills in the older cohort. In other words, drinking refusal self-efficacy seemed to be particularly protective for adolescents with lower coping skills. Several paths to the covariates were significant (see Table 5).
Table 5.
Path level moderation analyses of Time 2 Coping.
| Path | Lower coping standardised coefficient |
Higher coping standardised coefficient |
|
|---|---|---|---|
| Younger cohort | PSAE intercept → DRSE slope | .52** | .45** |
| PSAE intercept → T2 Alcohol use | .41** | .01 | |
| T1 Alcohol use → T2 Alcohol use | .20** | .32* | |
| DRSE slope → T3 Alcohol use | .54** | .61** | |
| Community risk → T2 Alcohol use | .12* | −.03 | |
| Older cohort |
Family risk → T2 Alcohol use | .20** | .06 |
| DRSE intercept → T2 Alcohol use | −.72** | −.45** | |
| T1 Alcohol use → T2 Alcohol use | −.07 | .18* | |
| RI → T2 Alcohol use | −.24* | .04 |
Note. All differences are significant,
p < .05
p < .001
p < .05
Discussion
This large-scale study tested prospective mediation and moderation relationships between impulsivity and cognitive risk factors for adolescent alcohol use. The hypothesised model was based on the 2-Component Approach to Reinforcing Substances theory (2-CARS; [7,13]). Results demonstrated the selective influence for reward drive and rash impulsiveness on the development of alcohol-related beliefs and adolescent drinking over two subsequent years. The present study, to our knowledge, is the first to prospectively investigate a model of the specific cognitive mechanisms uniquely associated with different facets of impulsivity. It is also the first study, to our knowledge, to evaluate the moderating effects of coping skills on these pathways.
The results suggest that pathways to alcohol use change during early to mid-adolescence, providing unique targets for intervention. Positive alcohol expectancies convey greater risk for future alcohol use in younger adolescents, especially those with lower coping skills, both directly and through their deleterious impact on drinking-refusal self-efficacy. Increased decline in drinking-refusal self-efficacy from age 11–13 years was the largest predictor of later alcohol use. It is possible that positive expectancies undermine drinking-refusal self-efficacy as adolescents may find it more difficult to resist a substance they believe will lead to rewarding social consequences, i.e., social approval and facilitation [13]. Lower coping skills may reduce drinking-refusal self-efficacy through a reduced ability to problem solve effective strategies to handle peer pressure or avoid situations where alcohol is offered.
This suggests that alcohol expectancies, coping, and drinking-refusal self-efficacy provide high-impact targets for adolescents aged 11–13 years, as the current study found that higher coping ameliorated the direct prospective impact of alcohol expectancies on prospective alcohol use, and a shallower decline in drinking-refusal self-efficacy was particularly protective for adolescents with low coping skills. A recent systematic review and meta-analyses of universal drug prevention programs found that directly strengthening drinking-refusal skills can have adverse effects in early and middle adolescence, increasing alcohol use [44]. Our findings suggest prevention approaches that aim to challenge alcohol-related cognitions and increase problem-based coping skills at this age may be able to target these mechanisms to better effect.
For older adolescents aged 13–15 years, interventions could incorporate efforts to directly reduce impulsivity, e.g., mindfulness meditation [45]. Reward drive emerged as risk factor for greater alcohol use in the older cohort, possibly due to increased alcohol use. Reward drive at age 13 was associated with drinking at age 15 through its effect on the other factors within the model (i.e., positive alcohol expectancies and their effect on drinking-refusal self-efficacy), indicating its increasing influence on alcohol use as adolescents age. This suggests that impulsivity may garner risk for increased alcohol use through experiential rather than vicarious alcohol learning. Rash impulsiveness also had larger impacts on later drinking for the older cohort, supporting the increased impact of impulsivity during this period. Much of this risk was conveyed through reduced drinking-refusal self-efficacy skills. Adolescents with higher rash impulsiveness may have a reduced capacity to end a drinking session, withdraw from drinking patterns once they are established, or to inhibit the impulse to engage in risk-taking behaviour [46]. The mediating role of drinking-refusal self-efficacy suggests this could encourage a self-fulfilling prophecy of poor drinking control, further exacerbating risk. Having high drinking-refusal self-efficacy showed greater protection for adolescents with low coping. Thus, approaches targeting impulsivity and drinking-refusal self-efficacy may be particularly effective at this age. As discussed earlier, the latter may best be achieved by targeting other components of the hypothesized causal chain.
A strength of the present study is that we were able to prospectively fit the proposed model across two parallel cohorts. The sophisticated analysis technique allowed us to evaluate prospective interactions as well as the effects of growth in cognitive risk factors over time. This allows for a more nuanced understanding of the development of cognitive constructs during adolescence and the effect of this growth on alcohol use. However, the results showed that the influences of various factors differed over the cohorts and different time points, so further investigation is needed into whether the current model is applicable to older adolescents and those with more drinking experience. Even so, the support of the model in adolescents as young as 11 and 13 years old is promising. Thus the model may demonstrate applicability for early interventions.
Another limitation of the present study is the measurement of constructs. While brief measures are not uncommon in large-scale studies, the use of validated measures of impulsivity and alcohol-related cognition is obviously preferable but often impractical in large-scale studies. Despite this, Connor et al. [18] found similar effect sizes between the cognitive mediators and alcohol use in a comparable population, and Harnett et al. [22] found similar effects for RI on alcohol use in a young adult population, indicating that the effects found in the present study may not have been severely impacted by measurement.
In summary, the present study provides evidence for the importance of impulsivity, drinking-refusal self-efficacy, and positive alcohol expectancies on the development of future adolescent alcohol use. We found that the model was predictive across two large cohorts of young adolescents across three years. We also found that coping ability impacted the relationship between the cognitive mediators and alcohol use. While this model should be replicated with specific construct measures and in older cohorts, it may be useful in understanding the interactive effects of personality and cognitive influences on adolescent alcohol use and inform targets for prevention programs.
Acknowledgements:
MJG was supported by a National Health and Medical Research Council (NHMRC) Early Career Fellowship (1036365). JPC is supported by a NHMRC Career Development Fellowship (1031909). The funder had no input into the design, analysis or interpretation of results.
Footnotes
Declaration of interests: Data collection for the International Youth Development Study has been supported by the National Institute on Drug Abuse (R01-DA012140–05), the Australian Research Council (ARC) Discovery Projects (DPO663371, DPO877359, DP1095744), and the Australian National Health and Medical Research Council (NHMRC) (Project 594793). The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
References
- 1.Australian Institute of Health and Welfare. National Drug Strategy Household Survey detailed report: 2013. Canberra: AIHW: 2014. [Google Scholar]
- 2.Geels LM, Bartels M, van Beijsterveldt TCEM, Willemsen G, van der Aa N, Boomsma DI, et al. Trends in adolescent alcohol use: effects of age, sex and cohort on prevalence and heritability. Addiction 2012;107:518–27. [DOI] [PubMed] [Google Scholar]
- 3.Keyes KM, Li G, Hasin DS Birth cohort effects and gender differences in alcohol epidemiology: A review and synthesis. Alcohol Clin Exp Res 2012;35:2101–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Duncan SC, Duncan TE, Strycker LA Alcohol use from ages 9–16: A cohort-sequential latent growth model. Drug Alcohol Depend 2006;81:71–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stoolmiller M, Wills T. a., McClure AC, Tanski SE, Worth K. a., Gerrard M, et al. Comparing media and family predictors of alcohol use: a cohort study of US adolescents. BMJ Open 2012;2:e000543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moffitt TE, Arseneault L, Belsky D, Dickson N, Hancox RJ, Harrington H, et al. A gradient of childhood self-control predicts health, wealth, and public safety. Proc Natl Acad Sci U S A 2011;108:2693–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gullo MJ, Dawe S Impulsivity and adolescent substance use: Rashly dismissed as “all-bad”? Neurosci Biobehav Rev 2008;32:1507–18. [DOI] [PubMed] [Google Scholar]
- 8.Steinberg L, Chein JM Multiple accounts of adolescent impulsivity. Proc Natl Acad Sci 2015;112:8807–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stautz K, Cooper A Impulsivity-related personality traits and adolescent alcohol use: A meta-analytic review. Clin Psychol Rev 2013;33:574–92. [DOI] [PubMed] [Google Scholar]
- 10.Steinberg L A social neuroscience perspective on adolescent risk-taking. Dev Rev 2008;28:78–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gullo MJ, Loxton NJ, Dawe S Impulsivity: Four ways five factors are not basic to addiction. Addict Behav 2014;39:1547–56. [DOI] [PubMed] [Google Scholar]
- 12.Connor JP, Gullo MJ, Feeney GFX, Young RM Validation of the Cannabis Expectancy Questionnaire (CEQ) in adult cannabis users in treatment. Drug Alcohol Depend 2011;115:167–74. [DOI] [PubMed] [Google Scholar]
- 13.Gullo MJ, Dawe S, Kambouropoulos N, Staiger PK, Jackson CJ Alcohol expectancies and drinking refusal self-efficacy mediate the association of impulsivity with alcohol misuse. Alcohol Clin Exp Res 2010;34:1386–99. [DOI] [PubMed] [Google Scholar]
- 14.Bandura A Social foundations of thought and action. Englewood Cliffs NJ: Prentice-Hall; 1986. [Google Scholar]
- 15.Tomlinson KL, Brown SA Self-medication or social learning? A comparison of models to predict early adolescent drinking. Addict Behav 2012;37:179–86. [DOI] [PubMed] [Google Scholar]
- 16.Jester JM, Wong MM, Cranford JA, Buu A, Fitzgerald HE, Zucker R a. Alcohol expectancies in childhood: Change with the onset of drinking and ability to predict adolescent drunkenness and binge drinking. Addiction 2015;110:71–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Oei TPS, Baldwin AR Expectancy theory: A two-process model of alcohol use and abuse. J Stud Alcohol Drugs 1993;55:525–34. [DOI] [PubMed] [Google Scholar]
- 18.Connor JP, George SM, Gullo MJ, Kelly AB, Young RM A prospective study of alcohol expectancies and self-efficacy as predictors of young adolescent alcohol misuse. Alcohol Alcohol 2011;46:161–9. [DOI] [PubMed] [Google Scholar]
- 19.Ehret PJ, Ghaidarov TM, LaBrie JW Can you say no? Examining the relationship between drinking refusal self-efficacy and protective behavioral strategy use on alcohol outcomes. Addict Behav 2014;38:1898–904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morawska A, Oei TPS Binge drinking in university students: A test of the cognitive model. Addict Behav 2005;30:203–18. [DOI] [PubMed] [Google Scholar]
- 21.Gullo MJ, St. John N., Young RM, Saunders JB, Noble EP, Connor JP Impulsivity-related cognition in alcohol dependence: Is it moderated by DRD2/ANKK1 gene status and executive dysfunction? Addict Behav 2014;39:1663–9. [DOI] [PubMed] [Google Scholar]
- 22.Harnett PH, Lynch SJ, Gullo MJ, Dawe S, Loxton N Personality, cognition and hazardous drinking: Support for the 2-Component Approach to Reinforcing Substances Model. Addict Behav 2013;38:2945–8. [DOI] [PubMed] [Google Scholar]
- 23.Kabbani R, Kambouropoulos N Positive expectancies and perceived impaired control mediate the influence of reward drive and rash impulsiveness on alcohol use. Pers Individ Dif 2013;54:294–7. [Google Scholar]
- 24.Leamy TE, Connor JP, Voisey J, Young RM, Gullo MJ Alcohol misuse in emerging adulthood: Association of dopamine and serotonin receptor genes with impulsivity-related cognition. Addict Behav 2016. [DOI] [PubMed] [Google Scholar]
- 25.Wills TA, Sandy JM, Yaeger AM, Cleary SD, Shinar O Coping dimensions, life stress, and adolescent substance use: A latent growth analysis. J Abnorm Psychol 2001;110:309–23. [DOI] [PubMed] [Google Scholar]
- 26.Corbin WR, Farmer NM, Nolen-Hoekesma S Relations among stress, coping strategies, coping motives, alcohol consumption and related problems: A mediated moderation model. Addict Behav 2013;38:1912–9. [DOI] [PubMed] [Google Scholar]
- 27.Allen KJD, Gabbay FH The amphetamine response moderates the relationship between negative emotionality and alcohol use. Alcohol Clin Exp Res 2012;37:348–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hasking PA, Oei TPS Alcohol expectancies, self-efficacy and coping in an alcohol-dependent sample. Addict Behav 2007;32:99–113. [DOI] [PubMed] [Google Scholar]
- 29.Richards JM, Patel N, Daniele-Zegarelli T, MacPherson L, Lejuez CW, Ernst M Social anxiety, acute social stress, and reward parameters interact to predict risky decision-making among adolescents. J Anxiety Disord 2015;29:25–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McMorris BJ, Hemphill SA, Toumbourou JW, Catalano RF, Patton GC Prevalence of substance use and delinquent behavior in adolescents from Victoria, Australia and Washington State, United States. Heal Educ Behav 2007;34:634–50. [DOI] [PubMed] [Google Scholar]
- 31.Quay HC, Peterson DR Manual for the Behaviour Problem Checklist. Miani, FL: 1987. [Google Scholar]
- 32.Achenbach TM, Rescorla LA Manual for the ASEBA school-age forms & profiles: an integrated system of mult-informant assessment. Burlington: University of Vermont, Research Center for Children, Youth & Families; 2001. [Google Scholar]
- 33.Hawkins JD, Smith BL, Hill KG, Kosterman R, Catalano RF, Abbott RD Understanding and preventing crime and violence: Findings from the Seattle Social Development Project In: Thornberry TP, Krohn MD, editors. Taking stock of delinquency: An overview of findings from contemporary longitudinal studies, New York, NY: Kluwer Academic/Plenum Publishers; 2003, p. 255–312. [Google Scholar]
- 34.Habib C, Santoro J, Kremer P, Toumbourou J, Leslie E, Williams J The importance of family management, closeness with father and family structure in early adolescent alcohol use. Addiction 2010;105:1750–8. [DOI] [PubMed] [Google Scholar]
- 35.Kelly AB, O’Flaherty M, Toumbourou JW, Connor JP, Hemphill SA, Catalano RF Gender differences in the impact of families on alcohol use: A lagged longitudinal study of early adolescents. Addiction 2011;106:1427–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Smith DT, Kelly AB, Chan GCK, Toumbourou JW, Patton GC, Williams JW Beyond the primary influences of parents and peers on very young adolescent alcohol use: Evidence of independent community associations. J Early Adolesc 2013;34:569–84. [Google Scholar]
- 37.Arthur MW, Hawkins JD, Pollard JA, Catalano RF, Baglioni AJ Jr. Measuring risk and protective factors for substance use, delinquency, and other adolescent problem behaviors: The Communities that Care Youth Survey. Eval Rev 2002;26:575–601. [DOI] [PubMed] [Google Scholar]
- 38.Glaser RR, Horn ML Van., Arthur MW, Hawkins JD, Catalano R.F. Measurement properties of the Communities That Care® Youth survey across demographic groups. J Quant Criminol 2005;21:73–102. [Google Scholar]
- 39.Jöreskog KG, Sörbom D LISREL 7 User’s Reference Guide. Chicago: Scientific Software, Inc; 1989. [Google Scholar]
- 40.Hayes AF Beyond Baron and Kenny: Statistical Mediation Analysis in the New Millennium. Commun Monogr 2009;76:408–20. [Google Scholar]
- 41.Tofighi D, MacKinnon DPR Mediation: An R package for mediation analysis confidence intervals. Behav Res Methods 2011;43:692–700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Marsh HW, Hau K-T, Wen Z In search of golden rules: Comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing Hu and Bentler’s (1999) findings. Struct Equ Model 2004;11:320–41. [Google Scholar]
- 43.Hu L, Bentler PM Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct Equ Model A Multidiscip J 1999;6:1–55. [Google Scholar]
- 44.Onrust SA, Otten R, Lammers J, Smit F School-based programmes to reduce and prevent substance use in different age groups: What works for whom? Systematic review and meta-regression analysis. Clin Psychol Rev 2016;44:45–59. [DOI] [PubMed] [Google Scholar]
- 45.Robinson JM, Ladd BO, Anderson KG When you see it, let it be: Urgency, mindfulness and adolescent substance use. Addict Behav 2014;39:1038–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dawe S, Gullo MJ, Loxton NJ Reward drive and rash impulsiveness as dimensions of impulsivity: Implications for substance misuse. Addict Behav 2004;29:1389–405. [DOI] [PubMed] [Google Scholar]