Abstract
Objective
To investigate whether lifetime trauma exposure predicts all-cause mortality and whether this association is mediated or moderated by perceived control.
Method
A sample of middle-aged and older adults (N = 4,961) who participated in the second wave of the Midlife in the United States Survey provided data. Lifetime trauma was operationalized using the reported number of potentially traumatic experiences spanning childhood through adulthood. Both constraints and mastery dimensions of perceived control were examined. Cox regression models tested main effects and interactions of lifetime trauma with mastery and constraints predicting 10-year mortality risk.
Results
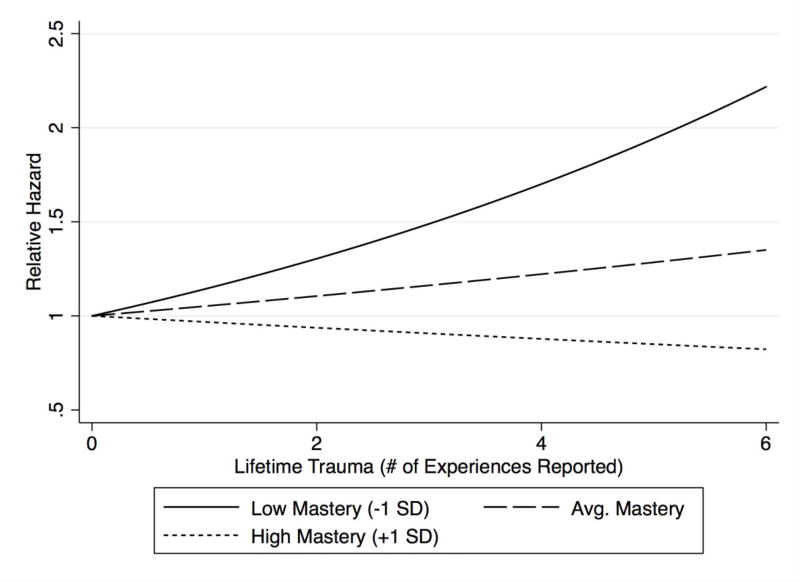
There was a significant main effect of lifetime trauma (b = .06, HR = 1.07, p = .032) and an interaction of trauma with mastery (b = −.08, p = .004). A greater number of traumatic experiences was associated with increased mortality risk at below-average levels of mastery (−1 SD: HR = 1.14, p < .001) but not at above-average levels (+1 SD: HR = 0.97, p = .48). This interaction persisted after further adjustment for health status, psychological, and behavioral covariates. An association of perceived constraints with elevated mortality risk (HR = 1.33, p = .008) was attenuated in a fully adjusted model (HR = 1.06, p = .26).
Conclusions
A strong sense of mastery may buffer elevated mortality risk associated with exposure to traumatic experiences. Findings extend evidence that mastery may foster resilience to the adverse health effects of traumatic stressors, whereas constraints may show stronger independent associations with health outcomes.
Keywords: trauma, stress, perceived control, control beliefs, mastery, self-efficacy, mortality
Exposure to potentially traumatic stressors is common and associated with higher morbidity and mortality (Felitti et al., 1998; Hendrickson et al., 2013; Krause, Shaw, & Cairney, 2004). Individuals exposed to traumatic stressors such as abuse or assault, military combat, and natural disasters are at greater risk for medical and psychiatric conditions including cardiovascular disease, cancer, diabetes, pain disorders, and depression (Felitti et al., 1998; Kendall-Tackett, 2009; Pietrzak, Goldstein, Southwick, & Grant, 2011), as well as earlier mortality (Brown et al., 2009; Chen, Turiano, Mroczek, & Miller, 2016; Hendrickson et al., 2013; Kelly-Irving et al., 2013). In addition to associations of medical comorbidity and mortality with child abuse and other adverse childhood experiences (ACEs) (Brown et al., 2009; Felitti et al., 1998), studies have reported associations with cumulative lifetime exposure to traumatic experiences, independent of post-traumatic stress disorder (PTSD) status (Hendrickson et al., 2013; Pietrzak et al., 2011). These studies support an accumulation of risk model, in which exposure to each additional potentially traumatic stressor increases risk for a given health outcome in an additive, cumulative fashion (Appleton, Holdsworth, Ryan, & Tracy, 2017).
There is growing interest in identifying factors associated with reduced susceptibility to the adverse health consequences of ACEs and other traumatic stressors. One factor conceptually and empirically linked with such resilience is high perceived control—beliefs in one’s ability to influence circumstances and attain goals (Benight & Bandura, 2004; Dunkel Schetter & Dolbier, 2011; Ong, Bergeman, & Boker, 2009). Conceptual models of stress, coping, and health (Folkman, 1984; Pearlin, Menaghan, Lieberman, & Mullan, 1981; Taylor & Stanton, 2007) propose that greater perceived control may reduce perceived threat in appraisals of stressful events as well as promote more adaptive coping responses (e.g., problem-solving, support seeking). This may, in turn, reduce the severity or chronicity of negative cognitive-emotional states, as well as stress-related physiological alterations, evoked by potentially traumatic events and experiences. Trauma exposure is linked with affective and physiological states such as depression, inflammation, and shortened telomeres, which predict health and mortality risk (Cuijpers et al., 2014; Felitti et al., 1998; O’Donovan, Neylan, Metzler, & Cohen, 2012; O'Donovan et al., 2011; Puterman et al., 2016). In prior studies perceived control mediated or moderated associations of traumatic and other stressors with negative affect and depressive symptoms (Jang, Chiriboga, & Small, 2008; King, Wardecker, & Edelstein, 2015; Turiano, Silva, McDonald, & Hill, 2017), and moderated associations of lifetime trauma with the inflammatory marker C-reactive protein (Elliot, Mooney, Infurna, & Chapman, 2017). In addition to these pathways, positive coping behaviors fostered by greater perceptions of control may reduce the likelihood of engagement in risky behaviors as means of coping with distress associated with trauma exposure. Such behaviors potentially linking trauma and mortality include smoking, alcohol and substance abuse (Bellis, Lowey, Leckenby, Hughes, & Harrison, 2014; Feldner, Babson, & Zvolensky, 2007; Felitti et al., 1998).
Potentially operating through these behavioral, psychological, or biological pathways, perceived control moderated associations of chronic stressors and low SES with self-report and objective health outcomes including mortality (Elliot & Chapman, 2016; Mausbach et al., 2007; Pudrovska, Schieman, Pearlin, & Nguyen, 2005; Turiano, Chapman, Agrigoroaei, Infurna, & Lachman, 2014). As for traumatic stressors, control buffered associations of childhood sexual abuse with self-rated health in pregnant women (King et al., 2015) and of physical abuse with self-reported physical health in middle-aged and older adults (Pitzer & Fingerman, 2010). Perceived control also directly predicts mortality and other health conditions (Infurna, Ram, & Gerstorf, 2013; Infurna & Mayer, 2015) and may play a mediating role in their relationships with trauma exposure. Beginning in childhood and continuing through the lifespan, traumatic stressors may sensitize individuals to external threats and undermine global perceptions of control (Bolger & Patterson, 2001; Shaw & Krause, 2002). In prior studies perceived control mediated associations of child maltreatment and various stressors in adulthood (e.g., chronic stressors, discrimination) with mental and physical health status (Bolger & Patterson, 2001; Jang et al., 2008; Mooney, Elliot, Douthit, Marquis, & Seplaki, 2016; Shaw & Krause, 2002). Although on average individuals with greater exposure to traumatic or other stressors report lower perceptions of internal or overall control, those able to maintain high perceived control may experience better health. Indeed, in several studies perceived control has both mediated and moderated associations between lifespan stress exposures and physical and mental health outcomes (Bolger & Patterson, 2001; Jang et al., 2008; Pitzer & Fingerman, 2010).
In the present study we investigated whether perceived control mediates or moderates an association between cumulative lifetime exposure to potentially traumatic experiences and mortality risk. We examined two conceptually and empirically distinct dimensions of control: mastery (perceived capacity to achieve goals) and constraints (beliefs that outcomes are determined by uncontrollable factors rather than individual actions) (Infurna & Mayer, 2015; Lachman & Weaver, 1998). We hypothesized that mastery and constraints would partly explain associations of greater lifetime trauma with higher mortality (mediation), and that high mastery and low constraints would also buffer mortality risk associated with trauma (moderation). Additionally, we expected that these interactions would be partly explained by physical health status, psychological factors, and health-related behaviors. We further investigated whether any mediation or moderation by mastery or constraints was specific to trauma experienced in childhood versus in adulthood.
Method
Participants
The present study utilized data from the Midlife Development in the United States Study (MIDUS), a national longitudinal study that commenced in 1995 with the first follow-up (MIDUS 2) conducted between 2004 and 2006. The initial sample consisted of approximately 7,000 adults ages 25 to 74, of whom 4,963 participated in MIDUS 2 (mortality-adjusted response rate of 75%). The present study is restricted to the MIDUS 2 sample due to availability of survey items comprising the measure of lifetime trauma. Whites, women, and individuals with higher levels of education, better self-rated health, and fewer functional limitations were more likely to participate in MIDUS 2 (Radler & Ryff, 2010). Two participants were excluded due to missing survival data. We also performed sensitivity analyses using a more restricted sample with complete data on all study variables (N = 3,809). Relative to those excluded, participants included in this sample had higher levels of perceived control, higher SES, were in better health, and were more likely to be male and of minority race/ethnicity. The present study was exempt from IRB approval as the selected MIDUS data are publically available through the Inter-University Consortium for Political and Social Research (ICPSR).
Measures
Lifetime trauma exposure
As in other studies testing accumulation of risk models, lifetime trauma exposure was operationalized using a count of reported potentially traumatic experiences, out of twelve total (prevalence shown in Table 1). These items were drawn from a larger subset of stressful experiences assessed in the MIDUS 2 survey, along with a measure of childhood abuse assessed in the MIDUS 1 survey. Selected items were based on those included in other surveys of lifetime trauma exposure in community samples (Krause et al., 2004; Turner & Lloyd, 1995). Six items referred to experiences that participants may have had during childhood and are commonly included in measures of ACEs (parental physical and emotional abuse, parental alcohol and substance abuse, parental divorce) (Bellis et al., 2014; Brown et al., 2009; Hostinar, Lachman, Mroczek, Seeman, & Miller, 2015). We also included parental death in childhood. Childhood abuse was measured using the validated Conflict Tactics Scale (Straus, 1979), which was administered only at MIDUS 1. Physical abuse was considered present if it was reported to have occurred “sometimes” or “often” (Chen et al., 2016), and emotional abuse, if it occurred “often.” In addition to moderate physical abuse (e.g., pushed, grabbed, slapped), severe physical abuse (e.g., hit with fist or object, choked, burned) was considered an additional traumatic exposure. A measure of physical or emotional abuse in adulthood was not available. The remaining six experiences were based on survey items asking about experiences that participants may have had at any point in the lifespan. To increase comparability with other studies (Elliot et al., 2017), including those using narrower criteria for traumatic events (Hendrickson et al., 2013; O’Donovan et al., 2012), we selected only those experiences commonly regarded as potentially traumatic in nature (e.g., abuse, assault, natural disaster, life-threatening illness or accident etc.).
Table 1.
Descriptive statistics for the analytic sample (N = 3,809)
| Variables | % / Mean (SD) | Range |
|---|---|---|
| Sociodemographic covariates | ||
| Age | 55.4 (12.45) | 28 – 84 |
| Female gender | 53.3% | |
| White race | 86.0% | |
| Minority race/ethnicity | 10.9% | |
| Parental / personal education: | 5.71 (2.88) / 7.20 (2.52) | 1 – 12 |
| Less than high school | 25.7% / 7.5% | |
| High school degree | 35.5 % / 25.5% | |
| Some college | 15.8% / 29.9% | |
| Graduated 4-year college | 23.0 % / 37.1% | |
| Participant SES | 0.0 (1.00) | −3.46 – 3.90 |
| Lifetime trauma | 1.15 (1.41) | 0 – 8 |
| Parental alcohol abusea | 22.9% | |
| Parental drug usea | 1.6% | |
| Parent dieda | 6.3% | |
| Parental divorcea | 16.6% | |
| Emotional abuse (often) a | 11.2% | |
| Moderate/severe physical abusea | 27.0% / 12.0% | |
| Child diedb | 14.2% | |
| Child life threatening illnessb | 12.2 % | |
| Physical assaultb | 14.2% | |
| Sexual assaultb | 14.2% | |
| Lost home to fire, flood, etc.b | 6.7% | |
| Experienced combatb | 8.2% | |
| Perceived Control | 7.6% | |
| Mastery | 5.74 (1.03) | 1 – 7 |
| Perceived constraints | 2.58 (1.18) | 1 – 7 |
| Other Covariates | ||
| Chronic disease | 2.43 (2.38) | 0 – 13 |
| ADL Limitations | 1.56 (0.73) | 1 – 4 |
| Self-rated health | 3.54 (1.02) | 1 – 5 |
| Depression | 10.0% | |
| Neuroticism | 2.07 (0.63) | 1 – 4 |
| Social support | 3.46 (0.46) | 1 – 4 |
| Pack-years smoked | 16.8 (28.24) | 0 – 244.80 |
| Alcoholic drinks per week | 11.4 (20.62) | 0 – 83 |
| Alcohol problems | 3.5% |
Notes. SEI = Socioeconomic index; ADL = Activities of daily living
Survey items asked whether these experiences occurred during childhood
Survey items asked whether these experiences occurred at any point in life
The MIDUS stressful life events questionnaire also asked participants to report the age at which a given event occurred. Based on reported ages we also created separate counts of potentially traumatic experiences in childhood (before age 18) and adulthood (age 18 and over). Participants also rated how the given experience affected them both “initially” and “In the long-run” on a five-point scale from “very negatively” to “very positively.”
Perceived Control
The measure of perceived control was developed by Lachman and Weaver (1998). Personal Mastery (α = .73) was measured using four items (e.g., “I can do just about anything I really set my mind to”), and perceived constraints (α = .85) using eight items (e.g., “What happens in my life is often beyond my control”), rated on a seven-point Likert scale.
Sociodemographic covariates
Sociodemographic covariates included gender and race (White vs. minority race/ethnicity). We controlled for parental education (highest level achieved by either parent, measured on a 12-point scale from “no school/some grade school” to “advanced graduate/professional degree”) given that lower family SES is associated with greater odds of various ACEs (Lee, Coe, & Ryff, 2017). Similarly, we adjusted for adult SES as a potential confounder. To derive a comprehensive measure of SES, we constructed a composite by averaging standardized scores (z-scores) for education (measured on the same 12-point scale), household income, household wealth, and occupational prestige (Hauser & Warren, 1996).
Health status covariates
Disease burden was measured using a count of the number of reported medical conditions (out of 29 total; e.g., diabetes, high blood pressure, stroke, ulcer). Functional health was assessed using a measure of limitations in basic and instrumental activities of daily living (ADLs). Participants rated the extent to which their health limited them in performing each of ten total activities (e.g., bathing or dressing, climbing stairs, lifting or carrying groceries), with scores on a 4-point scale (“not at all” to “a lot”) averaged to generate an overall limitations score. Self-rated physical health, measured on a five-point scale from “poor” to “excellent,” was also included as it predicts mortality over and above objective measures of health status (DeSalvo, Bloser, Reynolds, He, & Muntner, 2006).
Psychosocial covariates
Depressive symptoms were measured using the reported number of symptoms (up to seven in total, e.g., loss of interest, low energy, trouble concentrating) among participants who reported feeling “sad, blue, or depressed” most or all of the day for two weeks or more in the past 12 months. We also included the Big 5 personality trait neuroticism (α = .74) as well as social support as potential confounders, given observed associations with both perceived control (Judge, Erez, Bono, & Thoresen, 2002; Taylor, Lehman, Kiefe, & Seeman, 2006) and mortality (Chapman, Fiscella, Kawachi, & Duberstein, 2010; Holt-Lunstad, Smith, & Layton, 2010). For neuroticism, participants rated themselves on four trait adjectives (moody, worrying, nervous, calm), on a four-point scale (“not at all” to “a lot”). Support from family, friends, and spouse/partner were each measured with between four and six items (e.g., “How much do your family members really care about you?”), rated on the same four-point scale and averaged for a total network support score (α = .86).
Behavioral covariates
Behavioral covariates included pack-years of smoking (number of packs of cigarettes smoked per day times the number of years smoking) and multiple variables assessing alcohol use/abuse. Participants were asked questions about their alcohol consumption “during the period in your life, now or in the past, when you drank the most,” from which we constructed a continuous variable measuring the number of drinks per week. We also included an indicator variable for whether participants reported at least one alcohol related problem (e.g., psychological problems stemming from use, development of tolerance) in the past 12 months.
Mortality
Mortality follow-up was conducted through October, 2015. Mortality data on participants was obtained using several methods. First, a National Death Index (NDI) search conducted in 2009 confirmed 173 participant deaths. Second, 322 deaths were recorded during tracing and mortality closeout interviews conducted by the University of Wisconsin Survey Center (UWSC) as part of MIDUS 3 (2013–15) survey fielding. Lastly, 57 deaths were recorded during the course of normal longitudinal sample maintenance.
Statistical Analysis
We utilized Cox regression to evaluate an association of trauma with all-cause mortality and to examine potential mediation or moderation by mastery and perceived constraints. We used age at death (attained age) as the time scale as it provides a natural metric for longitudinal observational studies while still adjusting for age effects (Pencina, Larson, & D'Agostino, 2007). We also screened for non-proportionality (i.e., hazards that change with increasing survival time) by testing interactions of predictors with survival time (attained age in these models). We first tested main effects of lifetime trauma, mastery, and constraints in separate models adjusted for sociodemographic covariates. To test for mediation, we used the “difference method,” which measures the indirect or mediated effect as the difference in the coefficient for the exposure variable (lifetime trauma) in models with and without the mediator (mastery or constraints) (VanderWeele, 2011). To evaluate potential moderation, a second set of models tested interactions of lifetime trauma with each dimension of control in separate models, and if significant we examined the effect of trauma at varying levels of the given control variable. To facilitate these analyses, mastery and constraints variables were standardized (z-scored). Next, we examined the extent to which additional health status, psychosocial, and behavioral covariates statistically accounted for any observed interactions (Turiano et al., 2014). To do so, we tested a fully adjusted model that included all covariates and their interactions with trauma, if significant. Additional analyses repeated tests of mediation and moderation for separate measures of trauma in childhood and adulthood. We also performed various sensitivity analyses detailed in the results section. Missing values in the MIDUS 2 (longitudinal) sample were imputed using multiple imputation with chained equations (MICE). Following recommendations for imputation in Cox models (White & Royston, 2009), in addition to covariates we included the event indicator (deceased status) as well as the Nelson–Aalen estimator of the baseline hazard function in the imputation model. We performed ten imputations.
Results
Descriptive statistics are shown in Table 1. Participants ranged in age from 28 to 84, with an average age of 55.4 (SD = 12.5). The majority (86%) were White and around two-thirds had completed some college. More than half of the sample (60%) reported at least one potentially traumatic experience and nearly a third (30%) reported two or more. In the analytic sample there were 552 deaths (11.1%). The mean age at death was 74.9 years (SD = 10.8), with 99 deaths (18%) before age 65, 135 (24%) between 65 and 74, 200 (36%) between 75 and 85, and 118 (21%) at age 85 and over. Mastery was uncorrelated with lifetime trauma (r = −.02, p = .30) and with trauma in childhood (r = −.01, p = .52) and adulthood (r = −.03, p = .11) specifically. Constraints was significantly correlated with lifetime trauma (r = .08, p < .001), and showed similar correlations with trauma exposure in childhood (r = .06, p < .001) and adulthood (r = .08, p < .001). When examining specific experiences (analyses not shown), only physical assault was significantly associated with lower mastery. Perceived constraints were higher for those reporting emotional abuse, moderate and severe physical abuse, physical and sexual assault, and having lost a home. Mastery and constraints were moderately correlated (r = −.50, p < .001).
Table 2 shows coefficients and corresponding hazard ratios for the series of Cox regression models. In the baseline model (Model 1), greater lifetime trauma predicted higher all-cause mortality in a dose-response fashion (HR = 1.07 [95% CI: 1.01 – 1.13], p = .032). The hazard associated with lifetime trauma was proportional (i.e., it did not change with increasing survival time). Mastery and perceived constraints, however, showed non-proportional hazards: their associations with lower and higher mortality, respectively, diminished with increasing survival time. As shown in Table 2, non-proportional hazards for mastery and constraints, expressed as significant interactions with survival time (attained age), were retained in all models. When mastery and constraints were added to the model with lifetime trauma, the coefficient for trauma was largely unchanged (HR = 1.07, p = .038). As such, there was no evidence for mediation. When examined separately, mortality was not significantly associated with childhood trauma (HR = 1.06, p = .14) or adulthood trauma (HR = 1.09, p = .10).
Table 2.
Coefficients and 95% confidence intervals for Cox regression models predicting all-cause mortality
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | b | HR | p | b | HR | p | b | HR | p |
| Female gender | −.42 | .66 | <.001 | −.43 | .65 | < .001 | −.36 | .70 | < .001 |
| Minority race | .08 | 1.08 | .553 | .09 | 1.09 | .520 | .01 | 1.01 | .922 |
| Parental education | −.01 | .99 | .726 | −.01 | .99 | .704 | .01 | 1.01 | .728 |
| Participant SES | −.39 | .67 | <.001 | −.39 | .68 | <.001 | −.15 | .86 | .054 |
| Lifetime trauma | .06 | 1.07 | .032 | .05 | 1.05 | .100 | .06 | 1.06 | .124 |
| Masterya | −.11 | .89 | .010 | .01 | 1.01 | .089 | −.07 | 0.93 | .859 |
| Mastery × Attained age | .01 | -- | .011 | .01 | -- | .038 | .00 | -- | .410 |
| Constraints | .28 | 1.33 | .008 | .26 | 1.29 | .020 | .06 | 1.06 | .264 |
| Constraints × Att. age | −.01 | -- | .045 | −.01 | -- | .076 | −.00 | -- | .271 |
| Trauma × Mastery | −.08 | -- | .004 | −.08 | -- | .012 | |||
| Trauma × Constraintsb | .01 | -- | .568 | -- | -- | -- | |||
| Chronic disease | .03 | 1.03 | .113 | ||||||
| Self-rated health | −.32 | .73 | <.001 | ||||||
| ADL limitations | .34 | 1.41 | <.001 | ||||||
| Trauma × ADL | −.08 | .93 | .003 | ||||||
| Depression | −.01 | .99 | .768 | ||||||
| Neuroticism | −.07 | .93 | .435 | ||||||
| Social support | −.10 | .90 | .364 | ||||||
| Pack years smoked | .00 | 1.00 | <.001 | ||||||
| Alcohol problem | .18 | 1.20 | .540 | ||||||
| Alc. drinks per week | .00 | 1.00 | .988 | ||||||
Notes. HR = hazard ratio (exp(b)). ADL = activities of daily living
p values less than .05 are bolded
Represents coefficient for mastery at average attained age of 65
The interaction with constraints was tested in a separate model
With regard to moderation, we observed a significant interaction of trauma with mastery (b = −..08 [−.14 – −.03], p = .004), whereby the trauma-mortality association decreased in magnitude with increasing mastery. Simple slopes revealed a significant association at low mastery (−1 SD: HR=1.14 [95% CI: 1.06 – 1.23], p < .001) but not at average mastery (HR = 1.05 [0.99 – 1.12], p = .10) or high mastery (+1 SD: HR = .97 [.89 – 1.06], p = .48). The association was statistically significant at a level of mastery just below the mean (−.25 SD: HR = 1.07 [1.01 – 1.14], p = .018). Figure 1 shows the relative mortality hazard across the range of observed trauma scores at low, average, and high mastery. The interaction of trauma with constraints was not significant (p = .57) When examined separately, interactions of mastery with separate measures of trauma occurring in childhood and in adulthood were both significant (b = −.09, p = .031; b = −.14, p = .004, respectively), with each showing significant effects at a low level of mastery (−1 SD: HR = 1.14, p = .011; HR = 1.24, p = .011, respectively. When included in the same model the interaction of childhood trauma and mastery was attenuated to non-significance (b = −.07, p = .089) whereas the interaction for adulthood trauma persisted (b = −.12, p = .013). Lastly, we tested a fully adjusted model (Table 2, Model 3) including all additional covariates and any significant interactions with lifetime trauma, which applied only to functional limitations. The interaction with mastery was minimally attenuated (<5%) and the HR for trauma at low mastery (HR = 1.14), average mastery (HR=1.05) and high mastery (HR=.98) were essentially unchanged.
Figure 1.
Relative hazards associated with lifetime trauma at varying levels of mastery.
In a sensitivity analysis using mastery scores averaged across MIDUS 1 and MIDUS 2 assessments (possible reflecting average levels of mastery over a longer period of time), the interaction with lifetime trauma was significant and slightly larger (b = −.09, p < .001). This interaction also remained significant in a sensitivity analysis examining measures of lifetime trauma weighted by participants’ ratings of both the initial and the long-term impact (b = .09, p = .013; b = −.10, p = .006, respectively). Complete case analysis (N = 3,809) revealed a similar interaction of lifetime trauma and mastery (b = −.09, p = .003), although there appeared to be some selection effects involving a somewhat larger main effect of trauma (b = .09, HR = 1.09, p = .008) as well as effects at varying levels of mastery. We also imputed missing values and tested associations in the entire initial MIDUS cohort (N = 7,049). The interaction of lifetime trauma with mastery scores averaged across MIDUS 1 and MIDUS 2 was significant (b = −.042, p = .036), with lifetime trauma again predicting mortality at just below the mean level of mastery (−.25 SD; HR = 1.05, p = .028).
Discussion
Using a national sample of middle-aged and older adults, we found that a greater number of potentially traumatic experiences was associated with elevated risk for all-cause mortality. Neither mastery nor constraints mediated the trauma-mortality association. However, mastery moderated the association: the effect of trauma was weaker with increasing mastery and no longer evident at above-average levels of mastery. In prior studies perceived control mediated associations of childhood maltreatment, as well as various stressors in adulthood, with measures of mental and physical health (Bolger & Patterson, 2001; Jang et al., 2008; Mooney et al., 2016; Pudrovska et al., 2005; Shaw & Krause, 2002). Here, higher perceived constraints was associated with trauma exposure in childhood (including child maltreatment) and adulthood, but did not explain associations of lifetime trauma with mortality. With regard to moderation, the interaction of lifetime trauma and mastery observed here adds to a growing body of evidence implicating mastery or perceived control as a key psychological factor associated with resilience, broadly defined as positive or better-than-expected outcomes despite exposure to significant risk or adversity (Ong et al., 2009). Prior studies have found weaker associations of traumatic or other stressors with self-reported mental and physical health symptoms or conditions at high levels of perceived control (Jang et al., 2008; King et al., 2015; Pitzer & Fingerman, 2010; Pudrovska et al., 2005). We extend these findings by showing buffering effects of mastery/control involving a measure of cumulative stress exposure and predicting an objective endpoint in mortality. It is unclear whether and why the role of perceived control (mediation, moderation, or both) in the health effects of traumatic or other stressors might differ across specific mental or physical health outcomes. Further research examining pathways underlying stress-buffering and main effects of control variables may help to shed light on this question.
Notably, at lower levels of mastery lifetime trauma was related to mortality in a dose-dependent fashion. A prior study of cardiovascular patients (Hendrickson et al., 2013) found elevated mortality risk only at the upper end of the lifetime trauma distribution, a discrepancy that may attributable to the clinical population as well as a narrower diagnostic conceptualization of trauma. With regard to ACEs, Brown et al. (2009) found an association with mortality only at a high level of exposure, whereas Kelly-Irving et al. (2013) found a graded association in women but not men. In this study, potentially traumatic stressors experienced in childhood (similar to the ACE measures) showed a graded association with mortality at lower levels of mastery, although effects of trauma exposure in adulthood appeared to be stronger. Prior studies have also found associations of biomarkers and self-report health outcomes with cumulative trauma or adversity occurring in both childhood and adulthood (Hostinar et al., 2015; Krause et al., 2004; Lin, Neylan, Epel, & O’Donovan, 2016; Puterman et al., 2016).
In this study, lifetime trauma interacted with mastery but not constraints, which exhibited an independent association with mortality. These results parallel recent reports of differential effects for mastery and constraints—including a stronger main effect of constraints on mortality (Duan-Porter, Hastings, Neelon, & Van Houtven, 2017) and a moderating effect of mastery in relation to CRP (Elliot et al., 2017)—and further suggest examining these constructs separately. Constraints may be an independent risk factor whereas mastery may buffer excess risk associated with stress exposures (viewed alternately, it may be protective only at higher levels of stress exposure). Constraints may reflect circumstances leading to a perceived lack of contingency between actions and outcomes (i.e., the belief that desired outcomes are thwarted by limitations beyond one’s control), whereas mastery may reflect beliefs regarding personal competence (i.e., the perceived ability to perform the requisite actions) (Infurna & Mayer, 2015; Skinner, 1996).
Social-cognitive models (Bandura, 1997; Benight & Bandura, 2004) conceptualize perceived control as central to self-efficacy, which is thought to play an instrumental role in recovery from trauma and is related to better self-reported health in trauma survivors (Luszczynska, Benight, & Cieslak, 2009). Higher mastery may be accompanied by greater “coping self-efficacy”—the perceived ability to perform specific coping behaviors in response to stressors including problem-solving, managing negative thoughts and emotions, and obtaining support (Bandura, 1997). These coping behaviors may serve to blunt the adverse behavioral, psychological, or physiological impact of traumatic experiences. With regard to health behaviors, we found little evidence that the moderating effect of mastery was explained by less alcohol use/abuse or smoking, although we were unable to examine diet, exercise, or obesity. The interaction of lifetime trauma and mastery also persisted after adjustment for various health and psychological covariates, indicating that it was not merely an artifact of better health status, less depression (although the measure was limited in capturing duration and severity of symptoms), lower neuroticism, or greater social support among individuals with higher mastery. The lack of attenuation upon adjustment for health status and depression was surprising as these are also plausible mediators. Nevertheless, this result is in line with prior studies of ACEs and lifetime trauma exposure (Brown et al., 2009; Hendrickson et al., 2013; Kelly-Irving et al., 2013) showing minimal or modest attenuation of mortality effects in similar analyses.
Another possibility is that mastery modulates biological processes such as systemic inflammation or telomere length, through which trauma increases mortality risk. Preliminary support for this possibility emerged in a recent study (Elliot et al., 2017) in which mastery buffered an association of greater lifetime trauma with elevated CRP. Studies that directly test potential biological mediators as well as validated measures of behavioral and psychological factors are needed to identify mechanisms underlying the moderating effect of mastery. Future studies should also investigate the role of stress reactivity. Unexpectedly, a recent community study (Infurna, Rivers, Reich, & Zautra, 2015) found that childhood trauma-exposed adults with high perceived control were more rather than less emotionally reactive to negative daily events.
Findings of the present study suggest that individuals with substantial lifetime trauma exposure and low mastery are at the greatest risk for earlier death. It is possible that enhancing mastery/control, a modifiable characteristic (Lachman, Neupert, & Agrigoroaei, 2011; Zautra et al., 2012) could reduce excess mortality risk in individuals with histories of trauma exposure. For example, cognitive-behavioral interventions widely utilized in the treatment of PTSD and potentially feasible for implementation in primary care may impact perceptions of control and self-efficacy (Benight & Bandura, 2004), and have improved mental health and reduced risk behaviors among individuals exposed to ACEs (Korotana, Dobson, Pusch, & Josephson, 2016).
Findings of the present study should be interpreted in consideration of both the strengths and limitations of the design. The sample was predominantly White and relatively well-educated, and further research is needed to determine whether findings extend to more ethnically diverse, lower SES populations. Regarding mortality assessment, a greater number of decedents may have been missed through sample maintenance and fielding procedures than if a National Death Index search had been repeated in 2015. This may have resulted in some additional error in mortality classification. We were also unable to examine cause-specific mortality.
The measure of lifetime trauma utilized in this study also has various limitations, including its retrospective nature and the assessment of childhood abuse and other traumatic experiences occurring many years apart. However, evidence supports the validity and cross-time stability of retrospective reports of childhood abuse (Hardt & Rutter, 2004; Yancura & Aldwin, 2009), including in the MIDUS survey (Lee et al., 2017). As noted, the measure of cumulative trauma exposure is similar to measures in several health-related investigations (Krause et al., 2004; Puterman et al., 2016; Turner & Lloyd, 1995) but reflects a broader conceptualization and less precision than in others that have utilized structured clinical interviews (Hendrickson et al., 2013). There is ongoing debate as to how to conceptualize and measure trauma exposure (Saunders & Adams, 2014). The use of a count variable also has limitations: it does not capture differences associated with repeated or prolonged exposure to the same type of stressor (Appleton et al., 2017). In addition, it makes the assumption that each type of traumatic stressor impacts risk to a similar degree. To address this limitation we also examined a measure weighted by subjective impact ratings (Appleton et al., 2017), which showed similar results. In sum, here as in other studies (Lin et al., 2016) there were limitations in the measurement of trauma resulting from the use of an existing population-based dataset. New studies would ideally include more extensive and repeated measures of trauma, and prospective designs are needed to address important questions concerning the temporal nature of associations between trauma exposure (including specific types of experiences), perceived control, and health status over the lifespan. The MIDUS data used here also has advantages, including a national sample that is more representative than smaller single-site or convenience samples. As well, while retrospective, the data permits a lifespan view in connecting these childhood and adulthood experiences with a key health endpoint in midlife and older adulthood. Ultimately, multiple types of research designs and measures of trauma are needed to achieve a comprehensive understanding of relationships between trauma, perceived control, and health. Other strengths of the present study include the examination of separate dimensions of control and several potential explanatory variables.
In the present study, we found that a strong sense of mastery buffered excess mortality risk associated with lifetime exposure to potentially traumatic experiences in middle-aged and older adults. These findings extend evidence implicating mastery/perceived control in health-related resilience to stress, and call for further investigation of underlying mechanisms. Further research on trauma and perceived control has the potential to inform programs and interventions to reduce health-related risk in persons with histories of trauma exposure.
Acknowledgments
Source of Funding: This research was supported by a grant from the National Institute on Aging (R01AG044588) awarded to Benjamin P Chapman.
Footnotes
Conflicts of Interest: None declared.
When included in the same model, the interaction term for mastery was attenuated by less than 20% and approached significance (p = .058), whereas the interaction term for constraints was more than 50% attenuated and non-significant (p = .53), suggesting that the interaction effect is largely specific to mastery.
Contributor Information
Ari J. Elliot, Department of Psychiatry, University of Rochester Medical Center
Nicholas A. Turiano, Department of Psychology, West Virginia University
Frank J. Infurna, Department of Psychology, Arizona State University
Margie E. Lachman, Department of Psychology, Brandeis University
Benjamin P. Chapman, Departments of Psychiatry and Public Health Sciences, University of Rochester Medical Center
References
- Appleton AA, Holdsworth E, Ryan M, Tracy M. Measuring childhood adversity in life course cardiovascular research: A systematic review. Psychosomatic Medicine. 2017;79(4):434–440. doi: 10.1097/PSY.0000000000000430. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. New York, NY: W.H. Freeman; 1997. [Google Scholar]
- Bellis MA, Lowey H, Leckenby N, Hughes K, Harrison D. Adverse childhood experiences: Retrospective study to determine their impact on adult health behaviours and health outcomes in a UK population. Journal of Public Health (Oxford, England) 2014;36(1):81–91. doi: 10.1093/pubmed/fdt038. [DOI] [PubMed] [Google Scholar]
- Benight CC, Bandura A. Social cognitive theory of posttraumatic recovery: The role of perceived self-efficacy. Behaviour Research and Therapy. 2004;42(10):1129–1148. doi: 10.1016/j.brat.2003.08.008. [DOI] [PubMed] [Google Scholar]
- Bolger KE, Patterson CJ. Pathways from child maltreatment to internalizing problems: Perceptions of control as mediators and moderators. Development and Psychopathology. 2001;13(4):913–940. [PubMed] [Google Scholar]
- Brown DW, Anda RF, Tiemeier H, Felitti VJ, Edwards VJ, Croft JB, Giles WH. Adverse childhood experiences and the risk of premature mortality. American Journal of Preventive Medicine. 2009;37(5):389–396. doi: 10.1016/j.amepre.2009.06.021. [DOI] [PubMed] [Google Scholar]
- Chapman BP, Fiscella K, Kawachi I, Duberstein PR. Personality, socioeconomic status, and all-cause mortality in the united states. American Journal of Epidemiology. 2010;171(1):83–92. doi: 10.1093/aje/kwp323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen E, Turiano NA, Mroczek DK, Miller GE. Association of reports of childhood abuse and all-cause mortality rates in women. JAMA Psychiatry. 2016;73(9):920–927. doi: 10.1001/jamapsychiatry.2016.1786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, Vogelzangs N, Twisk J, Kleiboer A, Li J, Penninx BW. Comprehensive meta-analysis of excess mortality in depression in the general community versus patients with specific illnesses. American Journal of Psychiatry. 2014;171(4):453–462. doi: 10.1176/appi.ajp.2013.13030325. [DOI] [PubMed] [Google Scholar]
- DeSalvo KB, Bloser N, Reynolds K, He J, Muntner P. Mortality prediction with a single general Self-Rated health question. Journal of General Internal Medicine. 2006;21(3):267–275. doi: 10.1111/j.1525-1497.2005.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duan-Porter W, Hastings SN, Neelon B, Van Houtven CH. Control beliefs and risk for 4-year mortality in older adults: A prospective cohort study. BMC Geriatrics. 2017;17(1):13. doi: 10.1186/s12877-016-0390-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunkel Schetter C, Dolbier C. Resilience in the context of chronic stress and health in adults. Social and Personality Psychology Compass. 2011;5(9):634–652. doi: 10.1111/j.1751-9004.2011.00379.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliot AJ, Chapman BP. Socioeconomic status, psychological resources, and inflammatory markers: Results from the MIDUS study. Health Psychology. 2016;35(11):1205–1213. doi: 10.1037/hea0000392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliot AJ, Mooney CJ, Infurna FJ, Chapman BP. Associations of lifetime trauma and chronic stress with C-reactive protein in adults aged 50 and older: Examining the moderating role of perceived control. Psychosomatic Medicine. 2017;79(6):622–630. doi: 10.1097/PSY.0000000000000476. [DOI] [PubMed] [Google Scholar]
- Feldner MT, Babson KA, Zvolensky MJ. Smoking, traumatic event exposure, and post-traumatic stress: A critical review of the empirical literature. Clinical Psychology Review. 2007;27(1):14–45. doi: 10.1016/j.cpr.2006.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felitti M, Vincent J, Anda M, Robert F, Nordenberg M, Williamson M, Edwards B. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. American Journal of Preventive Medicine. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Folkman S. Personal control and stress and coping processes: A theoretical analysis. Journal of Personality and Social Psychology. 1984;46(4):839–852. doi: 10.1037//0022-3514.46.4.839. [DOI] [PubMed] [Google Scholar]
- Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: Review of the evidence. Journal of Child Psychology and Psychiatry. 2004;45(2):260–273. doi: 10.1111/j.1469-7610.2004.00218.x. [DOI] [PubMed] [Google Scholar]
- Hauser RM, Warren JR. Socioeconomic indexes for occupations: A review, update, and critique. University of Wisconsin-Madison Center for Demography & Ecology; 1996. Retrieved from http://www.ssc.wisc.edu/cde/cdewp/96-01.pdf: Working Paper No. 96-01. [Google Scholar]
- Hendrickson CM, Neylan TC, Na B, Regan M, Zhang Q, Cohen BE. Lifetime trauma exposure and prospective cardiovascular events and all-cause mortality: Findings from the heart and soul study. Psychosomatic Medicine. 2013;75(9):849–855. doi: 10.1097/PSY.0b013e3182a88846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: A meta-analytic review. PLoS Medicine. 2010;7(7):e1000316. doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hostinar CE, Lachman ME, Mroczek DK, Seeman TE, Miller GE. Additive contributions of childhood adversity and recent stressors to inflammation at midlife: Findings from the MIDUS study. Developmental Psychology. 2015;51(11):1630–1644. doi: 10.1037/dev0000049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Infurna FJ, Mayer A. The effects of constraints and mastery on mental and physical health: Conceptual and methodological considerations. Psychology and Aging. 2015;30(2):432–448. doi: 10.1037/a0039050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Infurna FJ, Ram N, Gerstorf D. Level and change in perceived control predict 19-year mortality: Findings from the Americans' Changing Lives study. Developmental Psychology. 2013;49(10):1833–1847. doi: 10.1037/a0031041. [DOI] [PubMed] [Google Scholar]
- Infurna FJ, Rivers CT, Reich J, Zautra AJ. Childhood trauma and personal mastery: Their influence on emotional reactivity to everyday events in a community sample of middle-aged adults. PloS One. 2015;10(4):e0121840. doi: 10.1371/journal.pone.0121840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jang Y, Chiriboga DA, Small BJ. Perceived discrimination and psychological well-being: The mediating and moderating role of sense of control. The International Journal of Aging and Human Development. 2008;66(3):213–227. doi: 10.2190/AG.66.3.c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Judge TA, Erez A, Bono JE, Thoresen CJ. Are measures of self-esteem, neuroticism, locus of control, and generalized self-efficacy indicators of a common core construct? Journal of Personality and Social Psychology. 2002;83(3):693–710. doi: 10.1037//0022-3514.83.3.693. [DOI] [PubMed] [Google Scholar]
- Kelly-Irving M, Lepage B, Dedieu D, Bartley M, Blane D, Grosclaude P, Delpierre C. Adverse childhood experiences and premature all-cause mortality. European Journal of Epidemiology. 2013;28(9):721–734. doi: 10.1007/s10654-013-9832-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendall-Tackett K. Psychological trauma and physical health: A psychoneuroimmunology approach to etiology of negative health effects and possible interventions. Psychological Trauma: Theory, Research, Practice, and Policy. 2009;1(1):35–48. [Google Scholar]
- King A, Wardecker BM, Edelstein RS. Personal mastery buffers the effects of childhood sexual abuse on women’s health and family functioning. Journal of Family Violence. 2015;30(7):887–897. [Google Scholar]
- Korotana LM, Dobson KS, Pusch D, Josephson T. A review of primary care interventions to improve health outcomes in adult survivors of adverse childhood experiences. Clinical Psychology Review. 2016;46:59–90. doi: 10.1016/j.cpr.2016.04.007. [DOI] [PubMed] [Google Scholar]
- Krause N, Shaw BA, Cairney J. A descriptive epidemiology of lifetime trauma and the physical health status of older adults. Psychology and Aging. 2004;19(4):637–648. doi: 10.1037/0882-7974.19.4.637. [DOI] [PubMed] [Google Scholar]
- Lachman ME, Weaver SL. The sense of control as a moderator of social class differences in health and well-being. Journal of Personality and Social Psychology. 1998;74(3):763–773. doi: 10.1037//0022-3514.74.3.763. [DOI] [PubMed] [Google Scholar]
- Lachman ME, Neupert SD, Agrigoroaei S. The relevance of control beliefs for health and aging. In: Schaie KW, Willis S, editors. Handbook of the psychology of aging. 7. Boston, MA: Academic Press; 2011. pp. 175–190. [Google Scholar]
- Lee C, Coe CL, Ryff CD. Social disadvantage, severe child abuse, and biological profiles in adulthood. Journal of Health and Social Behavior. 2017;58(3):371–386. doi: 10.1177/0022146516685370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin JE, Neylan TC, Epel E, O’Donovan A. Associations of childhood adversity and adulthood trauma with C-reactive protein: A cross-sectional population-based study. Brain, Behavior, and Immunity. 2016;53:102–112. doi: 10.1016/j.bbi.2015.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luszczynska A, Benight CC, Cieslak R. Self-efficacy and health-related outcomes of collective trauma: A systematic review. European Psychologist. 2009;14(1):51–62. [Google Scholar]
- Mausbach B, Patterson T, Känel RV, Mills P, Dimsdale J, Ancoli-Israel S, Grant I. The attenuating effect of personal mastery on the relations between stress and Alzheimer caregiver health: A five-year longitudinal analysis. Aging & Mental Health. 2007;11(6):637–644. doi: 10.1080/13607860701787043. [DOI] [PubMed] [Google Scholar]
- Mooney CJ, Elliot AJ, Douthit KZ, Marquis A, Seplaki CL. Perceived control mediates effects of socioeconomic status and chronic stress on physical frailty: Findings from the health and retirement study. Journals of Gerontology, Series B: Psychological and Social Sciences. 2016 doi: 10.1093/geronb/gbw096. Advance online publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Donovan A, Neylan TC, Metzler T, Cohen BE. Lifetime exposure to traumatic psychological stress is associated with elevated inflammation in the heart and soul study. Brain, Behavior, and Immunity. 2012;26(4):642–649. doi: 10.1016/j.bbi.2012.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Donovan A, Epel E, Lin J, Wolkowitz O, Cohen B, Maguen S, Neylan TC. Childhood trauma associated with short leukocyte telomere length in posttraumatic stress disorder. Biological Psychiatry. 2011;70(5):465–471. doi: 10.1016/j.biopsych.2011.01.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong AD, Bergeman CS, Boker SM. Resilience comes of age: Defining features in later adulthood. Journal of Personality. 2009;77(6):1777–1804. doi: 10.1111/j.1467-6494.2009.00600.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin LI, Menaghan EG, Lieberman MA, Mullan JT. The stress process. Journal of Health and Social Behavior. 1981;22(4):337–356. [PubMed] [Google Scholar]
- Pencina MJ, Larson MG, D'Agostino RB. Choice of time scale and its effect on significance of predictors in longitudinal studies. Statistics in Medicine. 2007;26(6):1343–1359. doi: 10.1002/sim.2699. [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Medical comorbidity of full and partial posttraumatic stress disorder in US adults: Results from wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Psychosomatic Medicine. 2011;73(8):697–707. doi: 10.1097/PSY.0b013e3182303775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitzer LM, Fingerman KL. Psychosocial resources and associations between childhood physical abuse and adult well-being. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 2010;65(4):425–433. doi: 10.1093/geronb/gbq031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pudrovska T, Schieman S, Pearlin LI, Nguyen K. The sense of mastery as a mediator and moderator in the association between economic hardship and health in late life. Journal of Aging and Health. 2005;17(5):634–660. doi: 10.1177/0898264305279874. [DOI] [PubMed] [Google Scholar]
- Puterman E, Gemmill A, Karasek D, Weir D, Adler NE, Prather AA, Epel ES. Lifespan adversity and later adulthood telomere length in the nationally representative US health and retirement study. Proceedings of the National Academy of Sciences of the United States of America. 2016;113(42):E6335–E6342. doi: 10.1073/pnas.1525602113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radler BT, Ryff CD. Who participates? Accounting for longitudinal retention in the MIDUS national study of health and well-being. Journal of Aging and Health. 2010;22(3):307–331. doi: 10.1177/0898264309358617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders BE, Adams ZW. Epidemiology of traumatic experiences in childhood. Child and Adolescent Psychiatric Clinics of North America. 2014;23(2):167–184. doi: 10.1016/j.chc.2013.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw BA, Krause N. Exposure to physical violence during childhood, aging, and health. Journal of Aging and Health. 2002;14(4):467–494. doi: 10.1177/089826402237179. [DOI] [PubMed] [Google Scholar]
- Skinner EA. A guide to constructs of control. Journal of Personality and Social Psychology. 1996;71(3):549–570. doi: 10.1037//0022-3514.71.3.549. [DOI] [PubMed] [Google Scholar]
- Taylor SE, Lehman BJ, Kiefe CI, Seeman TE. Relationship of early life stress and psychological functioning to adult C-reactive protein in the coronary artery risk development in young adults study. Biological Psychiatry. 2006;60(8):819–824. doi: 10.1016/j.biopsych.2006.03.016. [DOI] [PubMed] [Google Scholar]
- Taylor SE, Stanton AL. Coping resources, coping processes, and mental health. Annu. Rev. Clin. Psychol. 2007;3:377–401. doi: 10.1146/annurev.clinpsy.3.022806.091520. [DOI] [PubMed] [Google Scholar]
- Turiano NA, Chapman BP, Agrigoroaei S, Infurna FJ, Lachman M. Perceived control reduces mortality risk at low, not high, education levels. Health Psychology. 2014;33(8):883–890. doi: 10.1037/hea0000022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turiano NA, Silva NM, McDonald C, Hill PL. Retrospective reports of childhood misfortune are associated with positive and negative affect in adulthood: Exploring the moderating role of control beliefs. The International Journal of Aging and Human Development. 2017;84(3):276–293. doi: 10.1177/0091415016688480. [DOI] [PubMed] [Google Scholar]
- Turner RJ, Lloyd DA. Lifetime traumas and mental health: The significance of cumulative adversity. Journal of Health and Social Behavior. 1995;36(4):360–376. [PubMed] [Google Scholar]
- VanderWeele TJ. Causal mediation analysis with survival data. Epidemiology (Cambridge, Mass.) 2011;22(4):582–585. doi: 10.1097/EDE.0b013e31821db37e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White IR, Royston P. Imputing missing covariate values for the cox model. Statistics in Medicine. 2009;28(15):1982–1998. doi: 10.1002/sim.3618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yancura LA, Aldwin CM. Stability and change in retrospective reports of childhood experiences over a 5-year period: Findings from the Davis Longitudinal Study. Psychology and Aging. 2009;24(3):715. doi: 10.1037/a0016203. [DOI] [PubMed] [Google Scholar]
- Zautra AJ, Davis MC, Reich JW, Sturgeon JA, Arewasikporn A, Tennen H. Phone-based interventions with automated mindfulness and mastery messages improve the daily functioning for depressed middle-aged community residents. Journal of Psychotherapy Integration. 2012;22(3):206–228. [Google Scholar]