Abstract
Background:
Reperfusion injury of the spinal cord or “white cord syndrome” refers to the sudden onset of neurological deterioration after spinal decompressive surgery. Associated magnetic resonance (MR) findings only include focal hyperintensity on T2-weighted images without any other pathological changes.
Case Description:
A patient with cervical stenosis secondary to metastatic tumor in the intradural and extradural compartments presented with lower limb paraparesis. She underwent an uneventful tumor excision accompanied by posterior cervical decompression and fusion. Postoperatively, she was quadriplegic and required ventilator support. The emergent postoperative MR scan revealed focal hyperintensity on the T2-weighted image consistent with spinal cord edema extending into the lower brain stem.
Conclusion:
Very few cases of reperfusion injury of the cervical spinal cord or “white cord syndrome” are described in the literature. Here we present a patient who, following cervical laminectomy and fusion for excision of metastatic tumor, developed quadriplegia. Notably, postoperative MR showed only findings of upper cervical cord and lower brain stem edema consistent with a “white cord syndrome” without other compressive pathology.
Keywords: Blood spine barrier, spinal decompression surgery, white cord syndrome, quadriplegia
INTRODUCTION
Sudden neurological deterioration following spinal decompression may be attributed to a reperfusion injury of the spinal cord. On the postoperative magnetic resonance (MR) scan, cord ischemia and edema are characterized by a hyperintense intrinsic cord signal, which is typically labeled as the “white cord syndrome.”[1]
CASE REPORT
A 51-year-old female presented with a one-month history of progressive paraparesis and acute urinary retention. Her deficits were attributed to a cervical extramedullary metastatic ductal carcinoma.
MR imaging of the cervical spine showed a lesion involving the C3 vertebral body, with both extradural and intradural extension into both C3 neural foramina and the tumor enhanced with contrast [Figures 1 and 2].
Figure 1.
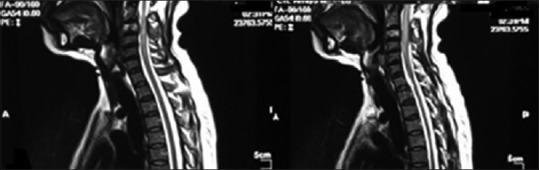
(Pre-operative T2 weighted sagittal MRI image showing the hyper intensity within the cord and canal narrowing at C3 and C4 levels)
Figure 2.
(Pre-operative T2 weighted axial MRI image showing the hyper intensity and canal narrowing at C3 and C4 levels)
A palliative cervical decompression and fusion was performed as her life expectancy was estimated at over 6 months. Intraoperatively, the right para spinous muscles were involved with tumor as were the C3 (total) and C4 (partial) vertebral bodies. A C2 to C5 laminectomy was performed and rods with pedicle screws were utilized to fuse C1, C2, C5, and C6 levels. The tumor was well-circumscribed, was not adherent to the dura, and was easily removed.
Patient had difficulty in extubation and was found to be quadriplegic with loss of sensation to pain, temperature, touch, and proprioception from C3 level and downwards.
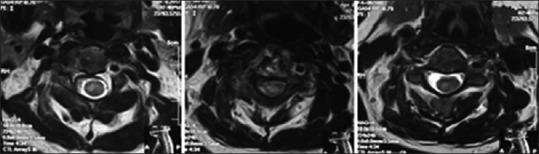
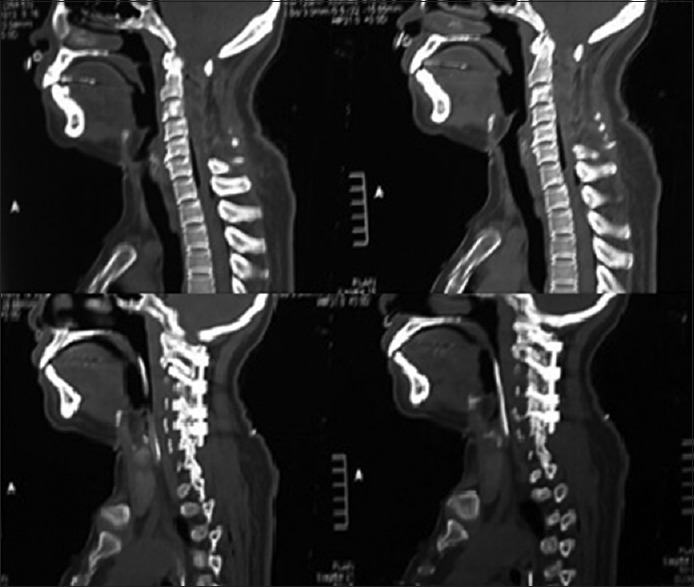
An urgent postoperative computed tomography showed good placement of the screws and rods with preserved alignment [Figure 3]. The postoperative MR images demonstrated worsening of cord edema extending to the lower brain stem [Figure 4]. She was started on high doses of dexamethasone to reduce the edema, and she was gradually weaned off the ventilator after 3 weeks. Nevertheless, her neurological status never improved.
Figure 3.
(Post-operative sagittal CT image showing laminectomy and good placement of screws and rods)
Figure 4.
(Post-operative T2 weighted MRI image showing resolved canal stenosis and high intensity patchy signal changes within the cord with cord swelling extending into the medulla oblongata: The appearance of “white cord syndrome”)
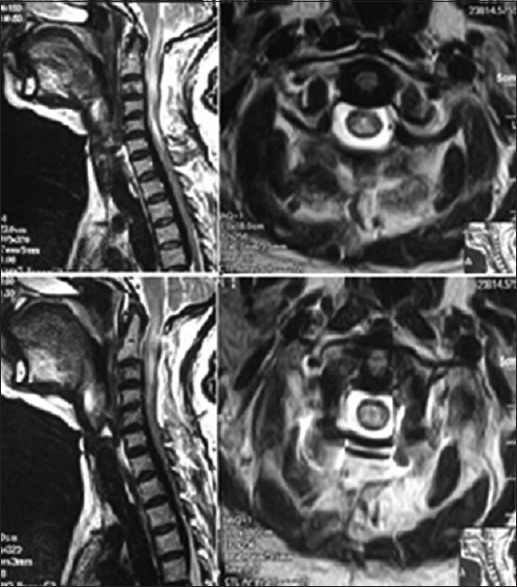
The T2 weighted MR scan was repeated 6 weeks later as seen in Figure 5, which documented the persistent “white cord syndrome” from C3 brain stem similar to the original immediate postoperative imaging. The patient was referred for palliative care.
Figure 5.
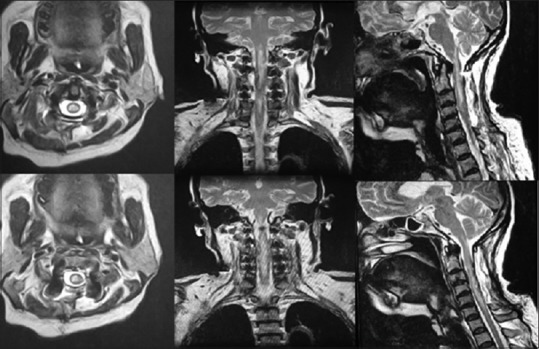
(Six weeks post-operative T2 weighted MRI image showing high intensity patchy signal changes within the cord with cord swelling extending into the medulla oblongata and is unchanged from the immediate post-operative MRI)
DISCUSSION
In this case, sudden decompression of the spinal cord following tumor removal was likely the source of acute cord injury. The etiology, therefore, is attributed to rapid cord expansion with acutely increased blood supply to the affected area. These sudden changes likely resulted in disruption in the blood–brain barrier and the blood–spinal cord barrier, resulting in a reperfusion injury (e.g., worsened edema with acute ischemia to the cord).[2]
A rat model study, published in 2015, investigated the pathogenesis of reperfusion spinal cord injury. Their theory was that grey matter could be dislodged when acute cord compression was “released.” They concluded that the group with severe spinal cord compression could exhibit significant deterioration.[3] However, only few clinical studies support the theory of reperfusion injury causing the “white cord syndrome” and resultant direct spinal cord injury after surgical decompression.[4]
CONCLUSION
The white cord syndrome is likely due to reperfusion injury following operative decompression of a chronically compressed spinal cord segment. Clinicians should be vary of this devastating complication and include it during the informed consent taking process preoperatively.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Contributor Information
Vayara P. Vinodh, Email: vinodhvayara@gmail.com.
Senthil K. Rajapathy, Email: vinodh_uk@hotmail.com.
Pulivendhan Sellamuthu, Email: spulivendhan@gmail.com.
Regunath Kandasamy, Email: kandasamy.regunath@gmail.com.
REFERENCES
- 1.Giammalva GR, Maugeri R, Graziano F, Gulì C, Giugno A, Basile L, et al. White cord syndrome after non-contiguous double-level anterior cervical decompression and fusion (ACDF): A “no reflow phenomenon”? Interdiscip Neurosurg. 2017;7:47–9. [Google Scholar]
- 2.Chin KR, Seale J, Cumming V. “White cord syndrome” of acute tetraplegia after anterior cervical decompression and fusion for chronic spinal cord compression: A case report. Case Rep Orthop. 2013;2013:697918. doi: 10.1155/2013/697918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wu L, Yang T, Yang C, Yao N, Wang H, Fang J, et al. Delayed neurological deterioration after surgery for intraspinal meningiomas: Ischemia-reperfusion injury in a rat model. Oncol Lett. 2015;10:2087–94. doi: 10.3892/ol.2015.3626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Seichi A, Takeshita K, Kawaguchi H, Nakajima S, Akune T, Nakamura K. Postoperative expansion of intramedullary high intensity areas on T2-weighted magnetic resonance imaging after cervical laminoplasty. Spine. 2004;29:1478–82. doi: 10.1097/01.brs.0000128757.32816.19. [DOI] [PubMed] [Google Scholar]


