Abstract
A 7-day-old baby boy born by lower segment caesarean section as term appropriate for gestational age was admitted with the complaint of fever, lethargy, and refusal to feed. The baby was put on antibiotic treatment for sepsis and meningitis. On the 15th day of the treatment, he developed lower motor neuron paralysis of both lower limbs along with sensory deficit. He also had bladder and fecal incontinence. Magnetic resonance imaging of spine showed spinal epidural lipomatosis extending from T8 to L5 with maximum compression of theca at L3-L4 level.
KEYWORDS: Epidural, lipomatosis, neonatal
INTRODUCTION
Epidural lipomatosis, a condition characterized by abnormal unencapsulated accumulations of fat on or outside the dura, is rare.[1] It was first described in 1975 by Lee et al.[2] The youngest reported case is of a 2-year-old child.[3] To our knowledge, no reported case in neonates is present. We are reporting a newborn with epidural lipomatosis in this article.
CASE REPORT
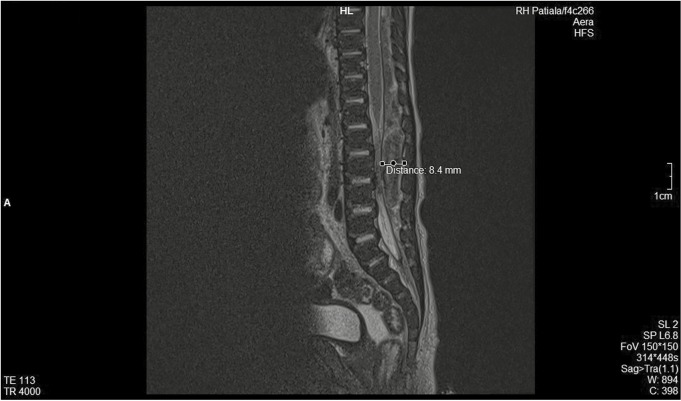
A 7-day-old baby boy was admitted with a complaint of fever, lethargy for 4 days, and refusal to feed for 2 days. The baby was delivered at term 39 weeks, 3400 g appropriate for gestational age by lower segment caesarean section (LSCS) to a primigravida mother. He cried immediately after birth. LSCS was performed because of chorioamnionitis, fetal bradycardia, and oligohydramnios. No history of (H/O) maternal drug intake, hypothyroidism, and decreased fetal movements were seen. The baby was on breastfeed before the onset of sickness. On examination, he was found to be lethargic. His respiratory rate was 60/min, heart rate was 120/min, capillary refill time was 3 s, and he was afebrile. His weight was 2470 g, head circumference was 35 cm, and length was 50 cm. Anterior fontanel was 3.3 cm and at level with sutural diastasis. Posterior fontanel tip was palpable. General physical examination was normal with no evidence of facial dysmorphism. On central nervous system examination, the baby was found to be lethargic. The Moro reflex was normal, but rooting and sucking were absent. Cranial nerves were normal. Posture, tone, and reflexes were normal. The hemoglobin level was 15.8 g/dL. Immature/total neutrophil cell ratio was 0.12. C reactive protein was positive. Platelet count was 2.12 × 105/cumm. Random blood sugar (RBS), serum calcium, and prothrombin time index were normal. Blood and urine cultures were sterile. Cerebrospinal fluid examination showed protein 50 mg/dL, sugar 55% of RBS. Cytology 2 lymphocytes/cumm. Blood urea/serum creatinine was 80/1.12 at admission, and it came to normal on the 3rd day of admission. Serum electrolytes were normal. The baby was treated on the lines of sepsis and meningitis with third generation cephalosporins and aminoglycosides. On the 15th day of treatment, the baby had edema in both feet, and was not moving both lower limbs. Note was made of the hyperpigmentation seen around the mouth of the baby. Pulses in both the lower limbs were normal. Lower limbs were flexed and abducted. There was an axial hypotonia in both the shoulders and the pelvic girdle. Tone was normal in upper limbs. However, it was decreased in the lower limbs, more in the right than in the left lower limb. Power was 5/5 in both the upper limbs. It was 2/5 in the left and 3/5 in the right lower limb. Abdominal reflexes were present. Cremasteric reflex was absent on the right and present on the left side. Plantar reflex was not elicitable on both the feet. Deep tendon reflexes were present in the upper limbs. Knee reflex was decreased on the left and absent on the right side. Ankle reflex was not elicitable on both the sides. There was no response to painful stimuli on both the feet and right lower limb. There was a response to deep pressure and painful stimuli on the left lower limb. There was continuous dribbling of urine. Bladder was not palpable. Fecal incontinence was present. Anal reflex was absent. Magnetic resonance imaging (MRI) of head revealed increased signal intensity in basal ganglia and thalamus in T1-weighted images, which was suggestive of hypoxic ischemic changes. MRI scan of spine revealed an epidural collection extending from T8 to L5 levels with a maximum extent at L3 and L4 levels. Maximum anterior posterior thickness of collection was at L3 level, and when measured it was found to be 8.4 mm. It was indenting and compressing the thecal sac with compression and effacement of thecal sac at L3-L4 levels. The collection demonstrated T1/T2 hyperintense signal with interspersed T2 low signal areas, suggestive of spinal epidural lipomatosis (SEL) [Figure 1].
Figure 1.
MRI of spine showing epidural lipomatosis
DISCUSSION
SEL was first described by Lee et al.[2] in an adolescent, who was receiving exogenous steroid therapy after a kidney transplant. Most cases of SEL are associated with a long-term use of exogenous steroids, but a number of cases have been reported, which are associated with Cushing’s disease, hypothyroidism, and pituitary prolactinoma. Idiopathic SEL, a rare entity, is usually observed in patients who are obese.[4] In a study by Moller et al.[5] in 2011, SEL was observed in a 10-year-old girl with relapsing polychondritis, who was on a long-term steroid treatment. SEL has been diagnosed after a mean (standard deviation) of 1.3 ( ± 1.5) years (median, 0.8 years; range, 3 weeks–6.5 years) of corticosteroid treatment given for different conditions in the children.
In their study by Toelle et al.[3] in 2012, an 11-year-old child with Bannayan–Riley–Ruvalcaba syndrome, which is characterized by macrocephaly, lipomatosis, penile freckles, hamartomatous intestinal polyps, and hemangiomas, was reported to have extensive SEL diagnosed at 2 years of age.[3]
In our case, H/O of any drug intake, hypothyroidism, obesity, or any other endocrinal disorder was not seen in the mother. The hyperpigmentation around the mouth observed in the baby could be due to increased adrenocorticotrophin hormone and melanocyte stimulating hormone levels. It could be related to stress. No macrocephaly was seen in our case.
Laminectomy results in the relief of symptoms in most cases of spinal cord compression in SEL. If the patient does not improve after surgery, then SEL must have caused irreversible neurological deficit. Regression of fat deposits after steroid reduction has been documented.[1]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Arroyo IL, Barron KS, Brewer EJ., Jr Spinal cord compression by epidural lipomatosis in juvenile rheumatoid arthritis. Arthritis Rheum. 1988;31:447–51. doi: 10.1002/art.1780310320. [DOI] [PubMed] [Google Scholar]
- 2.Lee M, Lekias J, Gubbay SS, Hurst PE. Spinal cord compression by extradural fat after renal transplantation. Med J Aust. 1975;1:201–3. doi: 10.5694/j.1326-5377.1975.tb111328.x. [DOI] [PubMed] [Google Scholar]
- 3.Toelle S, Poretti A, Scheer I, Huismann T, Boltshauser E. Bannayan-Riley-Ruvalcaba Syndrome with progressive spinal epidural lipomatosis. Neuropediatrics. 2012;43:221–4. doi: 10.1055/s-0032-1324402. [DOI] [PubMed] [Google Scholar]
- 4.Karageorgos A, Petsanas A, Gelalis I, Gkantaifis N, Aretha D. Idiopathic thoracic spinal epidural lipomatosis with relapsing and remitting symptoms. Internet J Orthop Surg. 2009;18:1–6. [Google Scholar]
- 5.Moller JC, Cron RQ, Young DW, Girschich HJ, Levy DM, Sherry DD, et al. Corticosteroid-induced spinal epidural lipomatosis in the pediatric age group: report of a new case and updated analysis of the literature. Pediatr Rheumatol. 2011;9:5. doi: 10.1186/1546-0096-9-5. [DOI] [PMC free article] [PubMed] [Google Scholar]