Abstract
Objectives
We aimed to study laryngeal stenosis among hospitalized children in the United States from 2003–2012. We hypothesized that the prevalence of laryngeal stenosis differs by race even when controlling for age, gender, and commonly associated disease conditions.
Methods
We report the results of a cross‐sectional survey of hospitalized patients with laryngeal stenosis. We utilized the Kids Inpatient Database (KID) to estimate the odds of laryngeal stenosis as a function of race using regression analysis. The effects of age, gender, and commonly associated conditions were controlled.
Results
There were 13,910 estimated discharges of patients with laryngeal stenosis (95% CI 13,715–14,105) within the study period. This accounts for 55 cases of laryngeal stenosis per 100,000 discharges (overall prevalence = 0.22%). After controlling for age and gender, Black children had the highest likelihood of laryngeal stenosis with OR of 1.9 (95% CI 1.8–2.0, P < .001) along with children classified as Other (OR = 1.2, 95% CI 1.0–1.3, P = .03). White (OR = 0.89, 95% CI 0.83–0.89, P < .001), Hispanic (OR = 0.86, 95% CI 0.80– 0.92, P < .001), and Asian (OR = 0.53, 95% CI 0.43–0.64, P < .001) children were less likely to be diagnosed with laryngeal stenosis while Native Americans (OR = 0.96, 95% CI 0.63–1.45, P = .51) were equally likely.
Conclusions
Laryngeal stenosis is more common among hospitalized Black children, while other racial groups appear to have lower risk. This elevated risk remained when controlling for age, gender, and commonly associated conditions with laryngeal stenosis.
Level of Evidence
4
Keywords: Laryngeal stenosis, subglottic stenosis, race, cross‐sectional survey, Kids Inpatient Database
INTRODUCTION
Laryngeal or subglottic stenosis (Ninth Revision, International Classification of Diseases, ICD‐9 code 478.74) refers to congenital or acquired narrowing of the larynx.1 The data concerning the incidence of laryngeal stenosis in children is limited. Few studies, of which most report the incidence in neonates, show the prevalence to be 1% to 8%.2, 3 In addition, association between endotracheal intubation and development of laryngeal stenosis has been previously described with more severe injuries resulting from multiple reintubations increasing the likelihood of laryngeal stenosis.4
Conditions that are associated with prolonged or repeated intubations in children include diseases or conditions that result in respiratory failure such as bronchopulmonary dysplasia, sepsis, and acute respiratory distress syndrome. Each of these conditions appears to be influenced by demographic factors such as race, age, and gender. For example, Black children are more likely to be born prematurely,5 and are therefore at higher risk of endotracheal intubation. The intrinsic risk associated with race when controlling for other factors such as prematurity and endotracheal intubation is currently unknown.
We report the results of a cross‐sectional survey of hospitalized children with laryngeal stenosis. Our primary aim was to study the prevalence of laryngeal stenosis in hospitalized children in the United States from 2003–2012. We hypothesized that there is a systematic influence of race on the prevalence of laryngeal stenosis among hospitalized patients even when controlling for age, gender, and commonly associated conditions.
MATERIALS AND METHODS
The University of Texas Southwestern Institutional Review Board approved the current study in the exempt status. We examined the 2003, 2006, 2009, and 2012 Kids Inpatient Database (KID) for patients with the ICD‐9 code for laryngeal stenosis (478.74). We queried a random sample of nonlaryngeal stenosis patients from these databases in a 2:1 fashion with two discharge records of children without laryngeal stenosis were designated as control for every discharge record associated with a diagnosis of laryngeal stenosis. The KID uses a complex survey design to produce national estimates of discharges. A complex survey uses statistical weighting of observations to produce estimated counts. Statistical calculations including means, proportions, regression analysis were performed on the estimated counts.
Continuous data is presented as means, standard errors, and 95% confidence intervals. Categorical data is presented as percentages, standard errors, and 95% confidence intervals. The odds of laryngeal stenosis as a function of race were estimated using regression analysis. The multiple regression models controlled for age, gender, and commonly associated conditions. Since the effects of age can change over time, we tested our model for two different functions—quadratic and cubic. The regression models used the observation‐weighted grand mean as the baseline estimation (regression coefficients). Pairwise comparisons of each racial group against each other (eg, Black vs. White, White vs. Asian, Hispanic vs. Black, etc.) were also performed. The pairwise comparisons were adjusted using the Bonferroni's method for multiple comparisons and observations were analyzed as unbalanced for racial groups.
We added the following diagnoses (utilizing ICD9 codes and HCUP's Clinical Classification Software, see Appendix for codes) to our logistic models to test for confounding factors impacting a principal diagnosis of laryngeal stenosis: (i) newborn status, (ii) intubation and mechanical ventilation, (iii) short gestation or low birth weight, (iv) birth trauma, (v) croup, and (vi) tracheostomy. We subsequently used logistic regression analysis to determine the effect of race on interventions performed for laryngeal stenosis. The interventions we examined were tracheostomy, laryngeal repair, tracheal repair, and bone graft harvest.
Since ICD‐9 coding contains overlapping of diagnoses and procedures as well as the large number of observations present in the KID, statistical significance was set at P ≤ .01. All statistics were performed with Stata statistical software (Release 14, StataCorp LP, College Station, Texas, U.S.A.).
RESULTS
A total of 13,910 estimated discharges of patients with laryngeal stenosis (95% CI 13,715–14,105) were identified within the study period. These included 2,099 in 2003, 3,535 in 2006, 3,992 in 2009, and 4,282 discharges in 2012. The incidence was therefore estimated to be 55 cases of laryngeal stenosis per 100,000 discharges, or 0.22% of all pediatric discharges. The average age was 3.0 (95% CI 2.9–3.1) years and 75% were less than or equal to 3 years of age. A strong male predominance (59%) that was observed and was consistent throughout childhood and adolescence. The racial breakdown was as follows: White (44%), Black (29%), Hispanic (19%), Asian (2.2%), Native American (0.62%), and Other (6.4%).
The average length of stay was 14 days (95% CI 13.5–14.8). The primary payer percentages were the following: Medicaid (56%), private insurance (35%), and self‐pay (6.3%). The mean total charges were $106 393 (95% CI $101,436–111,349). The majority of patients (77%) were discharged and 0.71% died during their hospitalization (See Table 1).
Table 1.
Basic Demographics of Laryngeal Stenosis Patients and Controls in the KIDS Database (Years 2003–2012).
| Characteristics |
Laryngeal Stenosis N = 9751 Est. = 13910 |
Control Group N = 18098 Est. =39179 |
P valuea |
|---|---|---|---|
| Age, yrs, mean (SE) | 3.0 (0.05) | 4.4 (0.06) | < .001 |
| Female, % (SE) | 41.1 (0.51) | 52.2 (0.60) | < .001 |
| Birth weight, gms | 1944 (136) | 3266 (27) | < .001 |
| Race, % (SE) | |||
| White | 43.2 (0.58) | 51.0 (0.64) | < .001 |
| Black | 28.7 (0.52) | 16.0 (0.45) | < .001 |
| Hispanic | 19.0 (0.45) | 22.4 (0.53) | < .001 |
| Asian | 2.2 (0.18) | 4.2 (0.31) | < .001 |
| Native Am | 0.62 (0.08) | 0.72 (0.09) | .43 |
| Other | 6.4 (0.29) | 5.6 (0.31) | .09 |
| Neonate, % (SE) | 15.2 (1.1) | 92.1 (0.40) | < .001 |
| Died, % (SE) | 0.71 (0.09) | 0.33 (0.03) | < .001 |
| Length of Stay, days, mean (SE) | 14.2 (0.29) | 3.6 (0.04) | < .001 |
| Payer, % (SE) | |||
| Medicaid | 47.4 (0.60) | 56.3 (0.51) | < .001 |
| Private | 44.5 (0.60) | 35.5 (0.49) | < .001 |
| Total Charges, dollars, mean (SE) | $106,393 (2528) | $15,146 (348) | < .001 |
| Median Income, % (SE) | |||
| < 25th | 30.9 (0.54) | 31.5 (0.48) | .43 |
| 26th to 50th | 25.5 (0.52) | 25.4 (0.45) | .80 |
| 51st to 75th | 23.8 (0.52) | 23.9 (0.44) | .79 |
| > 75th | 19.8 (0.47) | 19.2 (0.41) | .35 |
| Urban Hospital, % (SE) | 87.6 (0.44) | 98.3 (0.17) | < .001 |
P value based upon simple linear regression for continuous variables and Pearson X2 for categorical variables.
Several other results from analysis of the survey are worth mentioning: 36% of the patients had a tracheostomy or a tracheostomy placed during their stay; 21% had a laryngeal or tracheal repair surgery performed; and 23% of patients who underwent repair had a medical or surgical complication diagnosis during their admission. Patients who underwent laryngeal or tracheal repair were about 1.7 times more likely to have a complication than those who did not (15% vs. 23%, P < .001).
The primary analysis of race showed significant differences in the likelihood of laryngeal stenosis. After controlling for age and gender, Black children had the highest likelihood of laryngeal stenosis with OR of 1.9 (95% CI 1.8–2.0). Children classified as Other were more likely to have stenosis at the P ≤ .05 level but not the .01 level (OR = 1.2, 95% CI 1.0–1.3, P = .03). White (OR = 0.89, 95% CI 0.83–0.89, P < .001), Hispanic (OR = 0.86, 95% CI 0.80–0.92, P < .001), and Asians (OR = 0.53, 95% CI 0.43–0.64, P < .001) were all less likely to be diagnosed with laryngeal stenosis while Native Americans (OR = 0.96, 95% CI 0.63–1.45, P = .51) were equally likely (See Tables 2 and 3).
Table 2.
Multiple Logistic Regression Model of the Relationship Between Race and Laryngeal Stenosis Controlling for Age and Gender.
| Variable | Coeff. | SE | Wald X2 | P value | OR | 95% CI |
|---|---|---|---|---|---|---|
| Agea | 0.004 | 0.0001 | 962 | < .001 | 1.00 | 1.00–1.00 |
| Maleb | 0.30 | 0.03 | 66.3 | < .001 | 1.35 | 1.26–1.45 |
| Blackc | 0.76 | 0.04 | 261 | < .001 | 2.15 | 1.96–2.36 |
| Hispanic | −0.03 | 0.04 | 0.42 | .51 | 0.97 | 0.88–1.07 |
| Asian | −0.47 | 0.10 | 19.21 | < .001 | 0.62 | 0.50–0.78 |
| Native Am | 0.002 | 0.21 | 0.00 | .99 | 1.00 | 0.66–1.51 |
| Other | 0.29 | 0.07 | 14.4 | < .001 | 1.34 | 1.15–1.56 |
| Intercept | −1.71 | 0.03 | ‐ | ‐ | ‐ | ‐ |
Age is modeled as a cubic, age3 (see Figure 1 for illustration of main effects).
Female is the reference value for gender.
White is the reference value for racial categories.
Table 3.
Odds of Laryngeal Stenosis by Race Compared to the Grand Weighted Mean—KID Database (Years 2003–2012)a
| OR | SE | t test | 95% CI | P value | |
|---|---|---|---|---|---|
| White | 0.86 | 0.02 | −7.6 | 0.83–0.90 | < .001 |
| Black | 1.9 | 0.06 | 17.4 | 1.7–2.0 | < .001 |
| Hispanic | 0.84 | 0.03 | −4.9 | 0.78–0.90 | < .001 |
| Asian | 0.54 | 0.05 | −5.9 | 0.44–0.66 | < .001 |
| Native American | 0.87 | 0.18 | −0.66 | 0.58–1.31 | .51 |
| Other | 1.2 | 0.08 | 2.2 | 1.0–1.3 | .03 |
Adjusted by age and gender and then compared to the grand weighted mean of all racial groups. OR calculated using the logistic regression model presented in Table 2.
Pairwise comparisons shown in Figure 1 demonstrate that if the error bars cross the number zero, there is equal risk of stenosis when comparing each racial group. Specifically, Black children are more likely to be diagnosed with laryngeal stenosis than every other ethnic group. Hispanic and White children appear to have equal likelihood while Asian children have the lowest risk of laryngeal stenosis.
Figure 1.
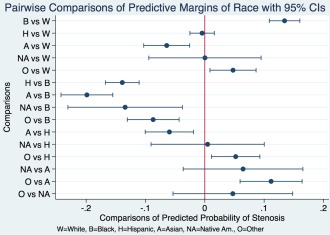
Pairwise comparisons of predictive probability of stenosis by race. W = White; B = Black; H = Hispanic; A = Asian; NA = Native American; O = Other.
When adding conditions commonly associated with laryngeal stenosis to the logistic regression model, Black children still have elevated risk when the following are present: (i) tracheostomy (OR = 1.9, 95% CI (1.7–2.0)), (ii) short gestation (OR = 1.9, 95% CI (1.8–2.0)), (iii) endotracheal intubation and mechanical ventilation (OR = 1.8, 95% CI (1.7–1.9)), (iv) croup (OR = 1.9, (1.8–2.0)), (v) birth trauma (OR = 1.9, 95% CI (1.8–2.0)), and (vi) newborn status (OR = 1.6, 95% CI (1.5–1.7)). White, Hispanic, and Asian children continue to have lower risk of laryngeal stenosis when compared to Black children when these conditions were present.
The different racial groups appeared to have no differences in the length of stay, total charges, or complications. Additionally, the likelihood of interventions that include tracheostomy, laryngeal repair, tracheal repair, or rib graft harvest were also similar (See Table 4).
Table 4.
Procedures for Laryngeal Stenosis by Race, KID 2003–2012.
| Racial Group | Number of Procedures (95% CI) | Percentage (SE) | Odds Ratio (95% CI)a | P value | |
|---|---|---|---|---|---|
| Tracheostomy | |||||
| Total |
1038 (962–1112) |
9.2 (0.3) | ‐ | ‐ | |
| White |
427 (378–476) |
9.2 (0.5) |
0.95 (0.87–1.04) |
.32 | |
| Black |
329 (286–372) |
10.7 (0.7) |
1.12 (1.00–1.27) |
.05 | |
| Hispanic |
164 (133–194) |
8.0 (0.7) |
0.82 (0.69–97) |
.02 | |
| Asian |
28 (16–40) |
11.7 (2.5) |
1.25 (0.78–2.00) |
.35 | |
| Native Am | ‐ | 13.2 (4.7) |
1.44 (0.64–3.22) |
.37 | |
| Other |
81 (60–112) |
7.8 (1.0) |
1.27 (0.96–1.66) |
.08 | |
| Laryngeal and/or Tracheal Repair | |||||
| Total |
2103 (1999–2227) |
19.5 (0.5) | ‐ | ‐ | |
| White |
898 (828–968) |
19.3 (0.7) |
0.98 (0.92–1.05) |
.74 | |
| Black |
632 (573–691) |
20.5 (0.9) |
1.06 (0.97–1.16) |
.19 | |
| Hispanic |
382 (336–428) |
18.7 (1.0) |
0.94 (0.84–1.07) |
.40 | |
| Asian |
41 (26–56) |
17.3 (2.9) |
0.86 (0.57–1.28) |
.48 | |
| Am Indian |
22 (11–33) |
32.5 (6.8) |
1.99 (1.08–3.6) |
.03 | |
| Other |
127 (100–155) |
18.6 (1.8) |
0.94 (0.74–1.18) |
.61 | |
Reference is the grand weighted mean for race.
DISCUSSION
The current study identifies significant racial disparities among hospitalized children diagnosed with laryngeal stenosis. Black children are approximately twice as likely to present with laryngeal stenosis compared to the average rate of laryngeal stenosis and therefore are more likely to be diagnosed with stenosis when compared to White, Hispanic, or Asian children. White and Hispanic children have roughly equal rates of laryngeal stenosis while Asian children have lowest rates overall. These differences persist even when controlling for conditions that are commonly associated with laryngeal stenosis, including age, gender, intubation and mechanical ventilation, croup, and the presence of a tracheostomy. While the KID cannot account for previous hospitalization, our results suggest that regardless of associated conditions, Black children are more likely to have laryngeal stenosis.
Laryngeal stenosis is most commonly caused by injury to the larynx and subglottic trachea secondary to intubation although congenital stenosis is well known to occur.6 Premature children who require prolonged intubation for mechanical ventilation are at particular risk for the development of stenosis.7
Considering the known risk factors for laryngeal stenosis, prematurity and endotracheal intubation, the finding of Black children having elevated risk of hospitalization with stenosis is not surprising since they have increased risk for both.5 That said, the increase in risk persists even when controlling for these conditions. This data therefore suggests that congenital stenosis and/or development of acquired stenosis is more common among Black children in addition to the risk of prematurity as well as prolonged intubation.
Since most instances of stenosis are due to injuries to laryngeal mucosa from intubation,4 the elevated risk of intubations combined with propensity towards hypertrophic scarring among Black children could explain this apparent disparity. Thus, a Black child is more likely to be premature or be intubated and have a hypertrophic response to laryngeal injury and therefore have increased incidence of laryngeal stenosis.
In addition to the most probable cause of these elevated rates, other potential relationships also need to be considered. For instance, Black children may also have higher rates of congenital stenosis or even that the notion of congenital stenosis is a misnomer in this population. Additionally, standard endotracheal size formulas for the pediatric airway are primarily adjusted by age and not with other characteristics such as gender or weight. Therefore, the “normal” airway size for a Black child could be different when compared to White, Hispanic, or Asian children of the same age and gender? The literature in this domain appears to be scant.
This study has some limitations. The KID only examines hospitalized patients. Potential cohorts of children with laryngeal stenosis may not be adequately captured by the KID and that group of patients may not show racial disparities. The KID also uses discharge abstracts from hospitals used for reimbursement purposes and not research. Therefore, the coding used to justify services may contain inaccuracies or overlap. The KID also does not account for repeat hospitalizations. Black children may be readmitted more often and therefore duplicate observations of hospitalized children may result in a skew. While these observations should affect all patients equally regardless of race, this factor must be considered in any interpretation.
Our findings demonstrate that Black children are disproportionately hospitalized with laryngeal stenosis. The increased incidence does not appear to affect outcome like length of stay, complication, or reconstructive surgeries but only the presence of the condition. Future studies should focus on confirming these findings as well as exploring the potential efforts to mitigate this risk if proven true.
CONCLUSIONS
Laryngeal stenosis is more common among hospitalized Black children, while other racial groups appear to have lower risk. This elevated risk remained when controlling for age, gender, and commonly associated conditions with laryngeal stenosis.
Supporting information
Additional supporting information may be found online in the Supporting Information section at the end of the article.
Supporting Information
Conflicts of interest: The authors declare no conflicts of interest. Dr. Isaiah has patent related royalties from the University of Maryland unrelated to this article.
Disclosure statement: The authors have no conflicts of interest. Dr. Isaiah receives royalties from the University of Maryland unrelated to this study.
BIBLIOGRAPHY
- 1.Centers for Disease Control and Prevention. International classification of diseases, ninth revision, clinical modification. Available at: http://www.cdc.gov/nchs/icd/icd9cm.htm Accessed December 1, 2016.
- 2. Walner DL, Loewen MS, Kimura RE. Neonatal subglottic stenosis—incidence and trends. Laryngoscope 2001;111(1):48–51. [DOI] [PubMed] [Google Scholar]
- 3. Choi SS, Zalzal GH. Changing trends in neonatal subglottic stenosis. Otolaryngol Head Neck Surg 2000;122(1):61–63. [DOI] [PubMed] [Google Scholar]
- 4. Gomes Cordeiro AM, Fernandes JC, Troster EJ. Possible risk factors associated with moderate or severe airway injuries in children who underwent endotracheal intubation. Pediatr Crit Care Med 2004;5(4):364–368. [DOI] [PubMed] [Google Scholar]
- 5. Balchin I, Steer PJ, Race, prematurity and immaturity. Early Hum Dev 2007;83 (12):749–754. [DOI] [PubMed] [Google Scholar]
- 6. Contencin P, Narcy P. Size of endotracheal tube and neonatal acquired subglottic stenosis. Study Group for Neonatology and Pediatric Emergencies in the Parisian Area. Arch Otolaryngol Head Neck Surg 1993;119(8):815–819. [DOI] [PubMed] [Google Scholar]
- 7. Dankle SK, Schuller DE, McClead RE. Risk factors for neonatal acquired subglottic stenosis. Ann Otol Rhinol Laryngol 1986;95(6‐Pt 1):626–630. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional supporting information may be found online in the Supporting Information section at the end of the article.
Supporting Information


