Abstract
BACKGROUND
Pedicle subtraction osteotomy (PSO) can be used to treat rigid sagittal plane deformities. Nonunions and rod breakages are known complications of PSO.
OBJECTIVE
To assess outcomes of 2 methods of posterior instrumentation for PSO, traditional 2 rods vs a novel 4-rod technique in which 2 additional rods span only the osteotomy level.
METHODS
This study was a retrospective, radiographic review of consecutive PSOs performed at 2 centers. The primary difference in technique between the centers was the use of 4 rods including 2 independent rods attached only to the vertebral levels immediately adjacent to the PSO (group 1, n = 29 patients) vs the traditional 2-rod technique (group 2, n = 20 patients).
RESULTS
Demographics and preoperative to postoperative radiographic measurements were similar between the study groups, including the PSO wedge resection angle (P = .56). The rod breakage rate was 25% with 2 rods and 0% with 4 rods (P = .008), and the pseudarthrosis rate with 2 rods was 25% and with 4 rods was 3.4% (P = .035). The patient with pseudarthrosis from group 1 had an infection and developed pseudarthrosis only after instrumentation removal. Rates of other complications did not differ significantly between the study groups.
CONCLUSION
This study provides a comparison between 2 techniques for rod placement across a PSO and suggests that the described novel 4-rod technique may help to reduce the rates of pseudarthrosis and rod failure. It will be important to confirm these findings in a prospectively designed study with multiple institutions in order to better control for potentially confounding factors.
Keywords: Complications, Deformity, 4-rod technique, Fusion, Pedicle subtraction osteotomy, Pseudarthrosis
ABBREVIATIONS
- ASD
adult spinal deformity
- GCA
global coronal alignment
- LL
lumbar lordosis
- PI
pelvic incidence
- PSO
pedicle subtraction osteotomy
- PT
pelvic tilt
- rh-BMP-2
recombinant human bone morphogenetic protein-2
- RF
rod fracture
- SVA
sagittal vertical axis
- TK
thoracic kyphosis
In the setting of severe rigid spinal deformities, pedicle subtraction osteotomy (PSO) can be useful in correcting the sagittal angular alignment up to 30° to 40° without the morbidity of a combined anterior and posterior approach.1 Additional advantages of PSO include avoiding excessive lengthening of the anterior vessels and viscera, and providing a greater, more stable correction.1-4 As a result, PSO has become increasingly popular and can be used in a wide variety of patients with flatback or other rigid sagittal plane deformities in order to increase lordosis.5-7
While the traditional 2-rod technique has been widely used in conjunction with PSO surgeries, it has been associated with high rates of rod failure, nonunions, and other complications.8-10 A novel 4-rod technique, in which the 2 additional rods are introduced to span only the osteotomy level, offers several advantages, since the 2 additional rods help to control the closing of the osteotomy and may reduce the risk of vertebral body translation. In addition, with this 4-rod technique, the additional rods aid in holding the osteotomy closed, while the longer rods are placed to connect the remaining proximal and distal extent of the fusion levels independently. Perhaps most importantly, having 4 rods across the osteotomy site may provide greater stability at the level where the instrumentation has the greatest mechanical stress and reduce the risks of pseudarthrosis and instrumentation failure. With this technique, the 2 additional rods are placed to span only 1 level above and below the osteotomy site. The longer rods that span the entire length of the instrumented fusion are not connected to the screws at the osteotomy site, avoiding the need for severe angular bending, which may weaken the rod making it more vulnerable for early rod fracture (RF) and place the patient at greater risk of pseudarthrosis.11-14
Smith et al8-10 reported RF rates of 6.8% in 442 patients with adult spinal deformity (ASD), but noted RF rates as high as 15.8% in 114 ASD patients treated with PSO. Eighty-nine per cent of the patients who had RF had the failure at or adjacent to the PSO level and early RF occurred in 63% at a mean of 6.4 mo.9 Tang et al,13 in a biomechanical study, showed that the magnitude of angular contouring of the rods is associated with lower fatigue life which can weaken the entire construct and suggests the need for other rod strategies to increase stability at the osteotomy site.13 Adding an additional midline rod that spans osteotomies has been suggested to decrease rod failure.15 Previous studies have not shown the clinical outcomes of the described 4-rod technique compared to the traditional 2-rod construct.
Despite the associated high rates of complications, the potential utility of a PSO in the surgical treatment of a rigid, sagittally malaligned spine is undeniable. The purpose of this study was to assess 2 methods of posterior instrumentation when performing PSO based on patients from 2 centers. One of the centers first used this novel 4-rod technique in 2002, and to our knowledge this is the first report of this technique in the literature. The other center contributed cases in which the traditional 2-rod technique was used. This study is the first to quantitatively assess and compare the complications, including early rod failures, nonunions, infection, and the degree of correction, between the traditional 2-rod technique and the novel 4-rod technique.
METHODS
A retrospective review of consecutive patients who underwent a PSO from 2 centers between the years of 2008 and 2011 was conducted with 3-yr minimum follow-up and an average follow-up of 5 yr for group 1 (4-rod technique) and 4 yr for group 2 (2-rod technique). Group 1 had a total of 29 patients and group 2 had a total of 20 patients. Patients at each center were treated with the same type of osteotomy, a PSO. The primary difference was that the patients in group 1 were treated with a 4-rod system (Figure 1) and those in group 2 were treated with the traditional 2-rod technique (Figure 2). Institutional review board approval was obtained prior to collection and analysis of data.
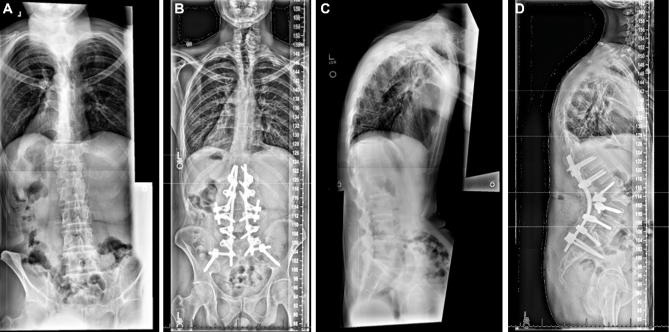
Figure 1.
Preoperative (A and C) and postoperative (B and D) radiographic films of the sagittal and coronal planes showing the 4-rod technique used in group 1, with 2 small rods spanning only the osteotomy site and 2 longer rods extending proximally and distally across all fusion levels but not attaching to the vertebral levels connected by the shorter rods.
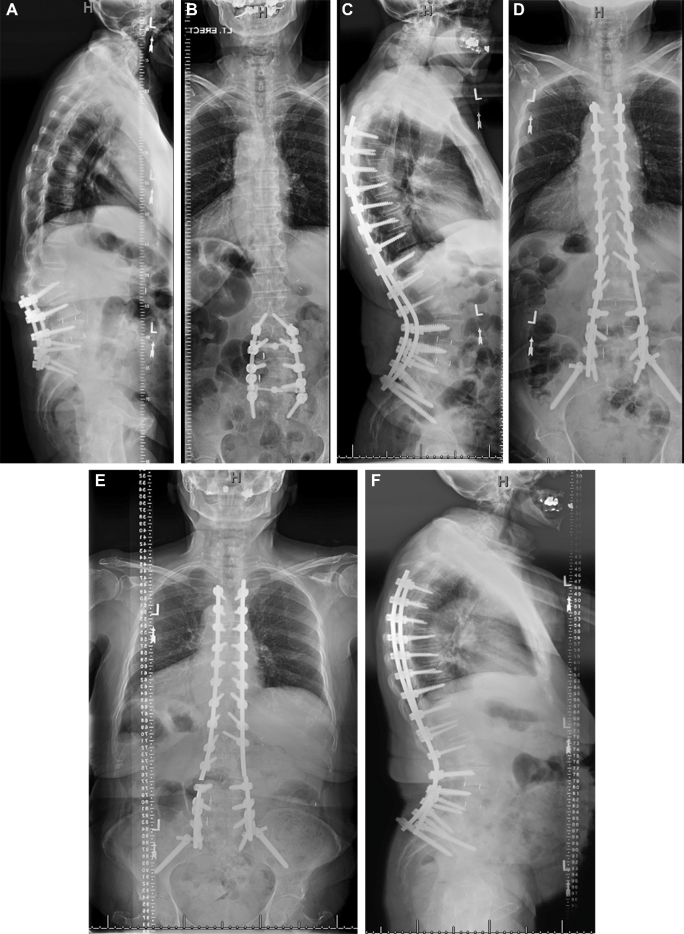
Figure 2.
Preoperative (A and C) and postoperative (B and D) radiographic films of the sagittal and coronal planes showing the traditional 2-rod technique used in group 2, with only 2 long rods across the osteotomy site extending proximally and distally. Rod fracture across the pedicle subtraction osteotomy level occurred in this patient and is shown on posteroanterior (E) and lateral (F) radiographs.
Spine fellows, who were not the attending surgeons at the time of surgery, performed radiographic measurements. These measurements were collected both preoperatively and postoperatively and included lumbar lordosis (LL), thoracic kyphosis (TK), pelvic tilt (PT), pelvic incidence (PI), sagittal vertical axis (SVA), global coronal alignment (GCA) based on the offset of the C7 plumbline relative to the central sacral vertical line, Cobb for the coronal curve, vertebral level at which the PSO was performed, and the resulting PSO bony wedge angle. Major and minor complications, classified according to Carreon et al,16 were also collected.
Patients were assessed for fusion primarily based on plain radiographs at follow-up unless they developed significant back pain, in which case CT imaging was performed to further assess for pseudarthrosis. RF was assessed primarily based on plain radiographs and, if present, prompted imaging with CT for further evaluation.
Summary data were tabulated for a total of 29 patients in group 1 and 20 patients in group 2. Statistical comparisons of the data were then performed. Preoperative and postoperative radiographic measurements and changes in these measurements were compared between institutions using 2-sample t-tests. Rod diameters were compared between institutions using the Wilcoxon rank-sum test. Complication rates and rates of usage of different rod types were compared between institutions using Fisher's exact test. A P-value of < .05 was considered statistically significant.
RESULTS
Demographics
The average age for group 1 was 62 yr and for group 2 was 64 yr. There were 13 men and 16 women in group 1, and there were 9 men and 11 women in group 2 (P = .61). In group 1, 28 of 29 patients had a history of at least 1 prior spine surgery. The 1 primary PSO patient had a rigid post-traumatic kyphotic deformity. All patients in group 2 had a history of at least 1 prior spine surgery. The most common PSO level was L3 for both groups, followed by L2 and L4. The mean number of vertebral levels fused for group 1 and group 2 was 10.
Radiographic Data
Regional Sagittal Alignment
Radiographic measures of preoperative and postoperative regional sagittal alignment for groups 1 and 2 are summarized in Table 1. The preoperative regional sagittal alignment measures (TK, LL, and PT) did not differ significantly between groups 1 and 2 (P > .17). Postoperatively, these regional sagittal alignment measures were statistically similar between the 2 groups, except for the TK, which was modestly but significantly greater in the group 1 patients (P = .001). The mean change in TK showed an increase of 19.3° in group 1 and 11.0° in group 2 (P = .08).
TABLE 1.
Preoperative and Postoperative Radiographic Measurements for 49 Patients With Adult Spinal Deformity Treated With Pedicle Subtraction Osteotomy Stratified by Whether 2 or 4 Rods Were Used Across the Osteotomy
| Preoperative | Postoperative | |||||
|---|---|---|---|---|---|---|
| Parameter (SD) | Group 1 (4 rods) | Group 2 (2 rods) | P-value | Group 1 (4 rods) | Group 2 (2 rods) | P-valuea |
| SVA (cm) | 14.4 (6.4) | 10.1 (5.2) | .014 | 6.1 (5.5) | 3.6 (3.1) | .049 |
| GCA (cm) | 3.8 (3.8) | 1.4 (1.5) | .004 | 1.9 (1.4) | 1.0 (1.5) | .042 |
| Cobb Angle (°) | 19.5 (16.3) | 16.8 (21.5) | .63 | 11.9 (13.8) | 12.4 (17.5) | .90 |
| TK (°) | 36.2 (24) | 28.4 (14.2) | .17 | 55.5 (15.9) | 39.4 (16.3) | .001 |
| LL (°) | 19.0 (18.0) | 23.1 (22.7) | .52 | 52.5 (13.1) | 51.3 (10.9) | .73 |
| PT (°) | 32.3 (14.0) | 27.4 (11.7) | .20 | 24.8 (10.5) | 21.3 (8.4) | .21 |
| PI+TK+LL (°) | 78.6 (20.1) | 65.0 (21.7) | .033 | 64.0 (17.7) | 46.4 (17.8) | < .001 |
| PSO angle (°) | NA | NA | NA | 39.4 (6.3) | 37.2 (15.9) | .56 |
SVA = sagittal vertical axis; GCA = global coronal alignment (offset of the central sacral vertical line from the C7 plumbline); TK = thoracic kyphosis; LL = lumbar lordosis; PT = pelvic tilt; PI + TK + LL = pelvic incidence + thoracic kyphosis + lumbar lordosis; PSO angle = pedicle subtraction osteotomy angle.
aSignificant P values are shown in bold print.
Coronal Cobb Angle and GCA
Table 1 summarizes the preoperative and postoperative coronal radiographic measures. The coronal Cobb angles did not differ significantly between groups 1 and 2 based on either preoperative or postoperative assessment. The GCA was modestly but significantly greater for group 1 compared with group 2 both preoperatively and postoperatively.
Global Sagittal Alignment
Table 1 summarizes the preoperative and postoperative global sagittal alignment. The mean preoperative SVA for group 1 was 14.4 cm and the mean preoperative SVA was 10.1 cm for group 2 (P = .014). The postoperative mean SVA was 6.1 cm in group 1 and 3.6 cm in group 2 (P = .049), demonstrating an average decrease of 8.3 cm in group 1 and 6.5 cm in group 2, compared with the respective preoperative measurement.
The preoperative PI+TK+LL was measured according to Rose et al17 to help predict long-term success of PSO. The mean preoperative PI+TK+LL was 78.6° for group 1 and 65.0° for group 2 (P = .033). The postoperative PI+TK+LL was significantly different with a mean of 64.0° in group 1 and 46.4° in group 2 (P < .001). However, when comparing the change between preoperative and postoperative PI+TK+LL between groups, the difference did not reach statistical significance (P = .62).
Instrumentation Type
The types of rods used and rod diameters were significantly different between the study groups (P < .001 for both comparisons; Table 2). For group 1 patients, the vast majority of rods were either titanium (58.6%) or stainless steel (37.9%), while the majority of the rods used in group 2 were cobalt chromium (80%). With regard to rod diameters, nearly all of the rods used in group 1 were 6.35 mm, while the majority of the rods used in group 2 were either 6.0 mm (55%) or 5.5 mm (35%).
TABLE 2.
Rod Composition and Diameter for 49 Patients With Adult Spinal Deformity Treated With Pedicle Subtraction Osteotomy Stratified by Whether 2 or 4 Rods Were Used Across the Osteotomy
| Group 1 (4 rods) | Group 2 (2 rods) | P-value | |
|---|---|---|---|
| Rod type | <.001 | ||
| Cobalt chromium | 1 (3.4%) | 16 (80%) | |
| Stainless steel | 11 (37.9%) | 2 (10%) | |
| Titanium | 17 (58.6%) | 2 (10%) | |
| Rod diameter (mm) | <.001 | ||
| 6.35 | 28 (97%) | 2 (10%) | |
| 6.0 | 0 (0%) | 11 (55%) | |
| 5.5 | 1 (3.4%) | 7 (35%) |
Complications
In terms of complications, both major and minor complications were comparable between both study groups, with the exception of pseudarthrosis and rod breakage (Table 3). Nine patients (31%) in group 1 and 8 patients in group 2 (40%) had major complications (P = .56; Table 3). Minor complications occurred in 9 patients (31%) from group 1 and 11 patients (55%) from group 2 (P = .14). In group 1 (4-rod technique), 1 of 29 patients (3.4%) developed pseudarthrosis, while in group 2 (2 rods), 5 of 20 patients (25%) were found to have pseudarthroses (P = .035). All patients with rod breakages had surgical exploration and confirmation of the pseudarthrosis. Eight out of 20 patients in group 2 had off-label use of recombinant human bone morphogenetic protein-2 (rh-BMP-2) used as an adjunct for fusion, while all patients in group 1 had rh-BMP-2 placed. Nevertheless, 3 of 5 patients from group 2 (60%) with a pseudarthrosis had rhBMP-2 used. Notably, the patient in group 1 who developed pseudarthrosis had rh-BMP-2 used but had a recalcitrant postoperative infection that required removal of instrumentation, which led to the pseudarthrosis. Thus, there were zero rod failures in group 1, but 5 rod failures in group 2, corresponding to the cases of pseudarthrosis (P = .008). The broken rods in this series were stainless steel (5.5 or 6.35 mm diameter) or cobalt chromium (5.5, 6.0, or 6.35 mm diameter). None of the group 1 patients underwent a circumferential fusion adjacent to the PSO. In group 2, 15 of 20 (75%) of patients had circumferential fusion adjacent to the PSO (either transforaminal or lateral interbody placement). Notably, in group 2, 4 out of the 5 patients (80%) with rod failure and pseudarthrosis had undergone circumferential fusions.
TABLE 3.
Complications for 49 Patients With Adult Spinal Deformity Treated With Pedicle Subtraction Osteotomy Stratified by Whether 2 or 4 Rods Were Used Across the Osteotomy
| Number of patients with specified complication (%) | |||
|---|---|---|---|
| Complication | Group 1 (4 rods, n = 29) | Group 2 (2 rods, n = 20) | P-valuea |
| Any complication | 14 (48.3) | 14 (70.0) | .15 |
| Major complications | 9 (31) | 8 (40) | .56 |
| Pseudarthrosis | 1 (3.4) | 5 (25) | .035 |
| Rod breakage | 0 (0.0) | 5 (25) | .008 |
| Junctional breakdown | 1 (3.4) | 1 (5.0) | .99 |
| Wound infection | 5 (17.2) | 0 (0.0) | .07 |
| Pneumonia | 2 (6.9) | 0 (0.0) | .51 |
| Renal failure | 0 (0.0) | 1 (5.0) | .41 |
| Myocardial infarction | 0 (0.0) | 1 (5.0) | .41 |
| Respiratory distress | 2 (6.9) | 0 (0.0) | .51 |
| Neurological deficit | 2 (6.9) | 0 (0.0) | .51 |
| Vein injury | 0 (0.0) | 1 (5.0) | .41 |
| Minor complications | 9 (31) | 11 (55) | .14 |
| Confusion | 1 (3.4) | 1 (5.0) | .99 |
| Ileus | 1 (3.4) | 1 (5.0) | .99 |
| Diarrhea | 1 (3.4) | 0 (0.0) | .99 |
| Dural tear | 5 (17.2) | 8 (40.0) | .10 |
| Prominent instrumentation | 0 (0.0) | 1 (5.0) | .41 |
| Wound dehiscence | 0 (0.0) | 1 (5.0) | .41 |
| Deep venous thrombosis | 1 (3.4) | 0 (0.0) | .99 |
aSignificant P values are shown in bold print.
Other major complications included 1 junctional breakdown in each group (P = .99). In group 1, there were 5 wound infections, but none were found in group 2 (P = .07). Group 1 had 2 patients who developed pneumonia, 2 patients with respiratory distress, and 2 with neurological deficits, while group 2 had no patients in those categories. In contrast, while group 1 lacked patients with renal failure and myocardial infarction, group 2 had 1 patient each in of these categories.
In terms of minor complications, 1 patient in each group experienced confusion and ileus (P = .99). Five patients in group 1 (17.2%) and 8 patients in group 2 (40%) experienced a dural tear (P = .10). In the categories of prominent instrumentation and wound dehiscence, 1 patient from group 2 had each of these complications. Overall, only 1 patient (from group 1) was diagnosed with a deep venous thrombosis.
DISCUSSION
PSO is an effective tool in correcting rigid sagittal plane deformities. One of the early descriptions of a lumbar PSO was in 1985 by Thomasen.3 He described the osteotomy to manage fixed sagittal plane deformities in the setting of ankylosing spondylitis. Subsequently, PSO and its applications have been discussed by multiple authors.1,2,4,7,14,18-21
PSOs are most commonly used in treating patients with a history of previous lumbar spine fusion. Loss of LL and positive sagittal malalignment are common presentations of patients in which a PSO may be useful.7,17 The patients in this study presented with loss of LL or a frankly kyphotic lumbar spine, and the majority of the patients had a history of previous spine surgery.
The 2 groups that are compared in this study were similar in age and sex distribution. The technique of the PSO between the groups was similar in terms of the wide decompression, bony resection, and correction. The mean PSO angular correction achieved was also similar (group 1 = 39° and group 2 = 37°). Although the patients in group 1 had a greater mean preoperative SVA (14.4 cm) compared with patients in group 2 (10.1 cm), the amount of SVA correction achieved with surgery was similar (8.3 and 6.5 cm, respectively). The residual SVA in group 1 was on average 6.1 cm which is greater than for group 2 (average 3.6 cm), reflecting the greater average SVA at baseline for group 1. The regional sagittal parameters preoperatively were similar between the 2 groups. The sagittal correction obtained with surgery was also similar between the groups.
The primary difference between the 2 study groups was the instrumentation technique across the PSO site. Group 1 used 2 short rods that spanned only the osteotomy site and 2 additional rods that spanned all levels of instrumented fusion but did not connect to the screws at the vertebral levels immediately adjacent to the PSO level. Patients in group 2 underwent the traditional 2-rod technique with the left and right rods connecting to all of the screws spanning the instrumented levels. Radiographically, both groups had excellent results in correcting the sagittal plane deformity. The major difference between the 2 groups following surgery was in rate of rod failures.
There were 5 nonunions in group 2 and 1 nonunion in group 1. The difference in the nonunion rate was statistically significant (P = .035). The rod failure rate in group 2 was 5 out of 20 or 25% and was 0 out of 29 or 0% in group 1 (P = .008). Notably, 4 out of the 5 patients with rod failures and pseudarthrosis in group 2 had circumferential fusions, demonstrating that circumferential fusion does not eliminate rod failures. The use of rhBMP-2 did not appear to have a significant impact, since 3 of 5 patients from group 2 with a pseudarthrosis had rhBMP-2 used in surgery. Rod failures occurred in proximity to the osteotomy site in group 2. The nonunion occurred at the osteotomy site in group 1 only after the instrumentation was removed for recalcitrant deep infection. The stress on the rod at the apex of the deformity, which is the site of the osteotomy, is mechanically the most unstable part of the long fusion. These factors may collectively contribute to the vulnerability for instrumentation failure and nonunion in the setting of PSO. The 4-rod technique reduces the need for extreme in situ contouring at the apex which may further compromise the integrity of the rod.13
There was a trend toward a higher rate of infection in group 1 (17.2%) compared with group 2 (0%; P = .07); the reason for this is unclear but it is unlikely related to the instrumentation technique. The incidence of dural tears was 5 in group 1 (17.2%) and 8 in group 2 (40%). These rates of dural tears are not unusual given that the majority of these cases are revisions. The wide decompression and dural dissection needed for PSO also contribute to a higher rate of expected durotomies.
The novel 4-rod technique described in this study has several potential advantages. Compared with the traditional 2-rod technique, the 4-rod construct can make it easier to close the osteotomy in a controlled manner. The rods that span the entire length of the fusion can be placed without the need to replace the shorter rods, a step which may compromise the degree of correction. More importantly, the rods spanning the entire length of the fusion do not have to be bent as sharply at the site of the PSO. The maximum stress on the rod is at the apex of the rods where the vertebral column is destabilized from the osteotomy. The rods usually fail around the osteotomy site. This technique also helps to significantly reduce early failure of the rods that likely relates to biomechanical compromise of the rods.9,10,13
Use of multiple rods to span thoracic and lumbar 3-column osteotomies has been previously reported by Hyun et al.15 In contrast to the novel technique described in the present report, in their study additional rods were attached using dominos and cross-links. They noted a significant reduction in rates of pseudarthrosis, RF, and need for revision surgery in the multirod group compared with the traditional 2-rod group and strongly recommended use of multiple rods to better stabilize 3-column osteotomies. How the added mechanical support of the novel 4-rod technique described in this study compares with the technique of adding multiple rods described by Hyun et al15 remains to be determined. Notably, Tang et al13 demonstrated that greater magnitude of angular contouring of a rod is associated with lower fatigue life. While the technique described by Hyun et al15 may strengthen the spinal construct, it may not reduce the required angular contouring of the primary rods bridging the 3-column osteotomy, which may remain vulnerable with longer follow-up.
This study compares 2 techniques for rod placement across PSO sites and shows statistically significant decreases in the rates of pseudarthrosis and rod failure when using the described novel 4-rod technique. Reduction of rod failure rates can save patients from the need for additional surgery and offers the potential for substantial cost savings by decreasing the need for revision procedures. Also, this research serves as a basis for future studies to further investigate the observed differences in larger patient populations. Several studies have reported increase in fusion rates and decrease in pseudarthrosis when using circumferential fusion.22-24 Therefore, future research may focus on investigating whether the use of circumferential fusion in comparison to a posterior-only fusion plays an important role when using 2 rods vs 4 rods. In addition, future research may focus on optimization of techniques and instrumentation to facilitate passage of the primary rods across the region of the short segment. Current strategies include use of lateral offset connectors for the short-segment rod and use of more deeply seating screws at the vertebral bodies immediately adjacent to the PSO level without the need for offset connectors. Whether one of these strategies provides more durable mechanical support remains to be assessed.
Limitations
Limitations of this study include the relatively small numbers of patients in each group and the retrospective design. However, the primary limitation of this study is that patients in each group were drawn from 2 different institutions. Although the 2 study groups had many similarities, including age, sex, history of previous surgery, PSO vertebral levels, number of levels fused, and PSO wedge resection angle, it is possible that specific differences in implants or operative techniques could have contributed to the differences in RF and pseudarthrosis rates observed in this study. These potentially confounding factors include rod composition and diameter, use of rh-BMP-2, and use of circumferential fusion adjacent to the level of the PSO. There are several observations that argue against these factors being solely responsible for the differences in pseudarthrosis and RF rates between the study groups. For example, although rh-BMP-2 was used in all patients in group 2 but in only 40% of those in group 1, the majority (60%) of the RFs that occurred in group 2 were in patients in whom rh-BMP-2 had been used. In addition, circumferential fusion adjacent to the PSO level, which has been reported to be protective against pseudarthrosis,25 was used in 75% of the patients in group 2 but in none of the patients in group 1. However, the majority (80%) of RFs in group 2 were in patients in whom circumferential fusion adjacent to the PSO level was performed. Rod composition differed between the study groups, but titanium, which has been suggested to be more vulnerable to RF in the setting of PSO,9 was preferentially used in group 1 patients. Although 6.35 mm diameter rods were preferentially used in group 1 patients and 6.0 and 5.5 mm diameter rods were preferentially used in group 2 patients, all rod diameters were represented among the 5 RFs in group 2, including 1 of the 2 patients in which 6.35 mm diameter rods were used. Nevertheless, given the limitations of this study, it will be important to confirm these findings in a prospectively designed study with multiple institutions.
CONCLUSION
This study provides a comparison between 2 techniques for rod placement across a PSO and suggests that the described novel 4-rod technique may help to reduce the rates of pseudarthrosis and rod failure. It will be important to confirm these findings in a prospectively designed study with multiple institutions in order to better control for potentially confounding factors.
Disclosures
Dr Ames is a consultant for DePuy Synthes, Medtronic, and Stryker, holds patnets with Fish & Richardson, PC, receives royalties from Zimmer Biomet and Aesculap, and has stock/stock options in Baxano Surgical, Doctors Research Group, and Visualase. Dr Deviren is a consultant for Nuvasive and Guidepoint and receives grants from Nuvasive, OREF, AOSpine, and Globus. Dr Smith is a consultant for and receives honoraria for teaching and royalties from Zimmer Biomet, is a consultant for and receives honoraria for teaching from Nuvasive and K2M, consults for Cerapdeics, receives fellowship funding and research support from AOSpine, and has fellowship funding from NREF. Dr Gupta is a consultant for and receives honoraria for lectures from DePuy Synthes and Orthofix, and receives royalties from DePuy Synthes. The other authors have no personal, financial, or institutional interest in any of the drugs, materials, or devices described in this article. Dr Durbin-Johnson receives research grant funding from the NIH.
REFERENCES
- 1. Bridwell KH, Lewis SJ, Rinella A, Lenke LG, Baldus C, Blanke K. Pedicle subtraction osteotomy for the treatment of fixed sagittal imbalance. Surgical technique. J Bone Joint Surg Am. 2004;86-A(suppl 1):44-50. [DOI] [PubMed] [Google Scholar]
- 2. Thiranont N, Netrawichien P. Transpedicular decancellation closed wedge vertebral osteotomy for treatment of fixed flexion deformity of spine in ankylosing spondylitis. Spine. 1993;18(16):2517-2522. [DOI] [PubMed] [Google Scholar]
- 3. Thomasen E. Vertebral osteotomy for correction of kyphosis in ankylosing spondylitis. Clin Orthop Relat Res. 1985;194:142-152. [PubMed] [Google Scholar]
- 4. van Royen BJ, Slot GH. Closing-wedge posterior osteotomy for ankylosing spondylitis. Partial corporectomy and transpedicular fixation in 22 cases. J Bone Joint Surg Brit. 1995;77(1):117-121. [PubMed] [Google Scholar]
- 5. Berven SH, Deviren V, Smith JA, Emami A, Hu SS, Bradford DS. Management of fixed sagittal plane deformity: results of the transpedicular wedge resection osteotomy. Spine. 2001;26(18):2036-2043. [DOI] [PubMed] [Google Scholar]
- 6. Booth KC, Bridwell KH, Lenke LG, Baldus CR, Blanke KM. Complications and predictive factors for the successful treatment of flatback deformity (fixed sagittal imbalance). Spine. 1999;24(16):1712-1720. [DOI] [PubMed] [Google Scholar]
- 7. Smith JS, Singh M, Klineberg Eet al. Surgical treatment of pathological loss of lumbar lordosis (flatback) in patients with normal sagittal vertical axis achieves similar clinical improvement as surgical treatment of elevated sagittal vertical axis: clinical article. J Neurosurg Spine. 2014;21(2):160-170. [DOI] [PubMed] [Google Scholar]
- 8. Smith JS, Klineberg E, Lafage Vet al. Prospective multicenter assessment of perioperative and minimum 2-year postoperative complication rates associated with adult spinal deformity surgery. J Neurosurg Spine. 2016;25(1):1-14. [DOI] [PubMed] [Google Scholar]
- 9. Smith JS, Shaffrey CI, Ames CPet al. Assessment of symptomatic rod fracture after posterior instrumented fusion for adult spinal deformity. Neurosurgery. 2012;71(4):862-867. [DOI] [PubMed] [Google Scholar]
- 10. Smith JS, Shaffrey E, Klineberg Eet al. Prospective multicenter assessment of risk factors for rod fracture following surgery for adult spinal deformity. J Neurosurg Spine. 2014;21(6):994-1003. [DOI] [PubMed] [Google Scholar]
- 11. Hyun SJ, Rhim SC. Clinical outcomes and complications after pedicle subtraction osteotomy for fixed sagittal imbalance patients: a long-term follow-up data. J Korean Neurosurg Soc. 2010;47(2):95-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ikenaga M, Shikata J, Takemoto M, Tanaka C. Clinical outcomes and complications after pedicle subtraction osteotomy for correction of thoracolumbar kyphosis. J Neurosurg Spine. 2007;6(4):330-336. [DOI] [PubMed] [Google Scholar]
- 13. Tang JA, Leasure JM, Smith JS, Buckley JM, Kondrashov D, Ames CP. Effect of severity of rod contour on posterior rod failure in the setting of lumbar pedicle subtraction osteotomy (PSO): a biomechanical study. Neurosurgery. 2013;72(2):276-282; discussion 283. [DOI] [PubMed] [Google Scholar]
- 14. Yang BP, Ondra SL, Chen LA, Jung HS, Koski TR, Salehi SA. Clinical and radiographic outcomes of thoracic and lumbar pedicle subtraction osteotomy for fixed sagittal imbalance. J Neurosurg Spine. 2006;5(1):9-17. [DOI] [PubMed] [Google Scholar]
- 15. Hyun SJ, Lenke LG, Kim YC, Koester LA, Blanke KM. Comparison of standard 2-rod constructs to multiple-rod constructs for fixation across 3-column spinal osteotomies. Spine. 2014;39(22):1899-1904. [DOI] [PubMed] [Google Scholar]
- 16. Carreon LY, Puno RM, Dimar JR 2nd, Glassman SD, Johnson JR. Perioperative complications of posterior lumbar decompression and arthrodesis in older adults. J Bone Joint Surg Am. 2003;85-A(11):2089-2092. [DOI] [PubMed] [Google Scholar]
- 17. Rose PS, Bridwell KH, Lenke LGet al. Role of pelvic incidence, thoracic kyphosis, and patient factors on sagittal plane correction following pedicle subtraction osteotomy. Spine. 2009;34(8):785-791. [DOI] [PubMed] [Google Scholar]
- 18. Bakaloudis G, Lolli F, Di Silvestre Met al. Thoracic pedicle subtraction osteotomy in the treatment of severe pediatric deformities. Eur Spine J. 2011;20(suppl 1):S95-S104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bridwell KH, Lewis SJ, Edwards Cet al. Complications and outcomes of pedicle subtraction osteotomies for fixed sagittal imbalance. Spine. 2003;28(18):2093-2101. [DOI] [PubMed] [Google Scholar]
- 20. Chen IH, Chien JT, Yu TC. Transpedicular wedge osteotomy for correction of thoracolumbar kyphosis in ankylosing spondylitis: experience with 78 patients. Spine. 2001;26(16):E354-E360. [DOI] [PubMed] [Google Scholar]
- 21. Jaffray D, Becker V, Eisenstein S. Closing wedge osteotomy with transpedicular fixation in ankylosing spondylitis. Clin Orthop Relat Res. 1992;279:122-126. [PubMed] [Google Scholar]
- 22. Gertzbein SD, Hollopeter MR, Hall S. Pseudarthrosis of the lumbar spine. Outcome after circumferential fusion. Spine. 1998;23(21):2352-2356; discussion 2356-2357. [DOI] [PubMed] [Google Scholar]
- 23. Grob D, Scheier HJ, Dvorak J, Siegrist H, Rubeli M, Joller R. Circumferential fusion of the lumbar and lumbosacral spine. Arch Orthop Trauma Surg. 1991;111(1):20-25. [DOI] [PubMed] [Google Scholar]
- 24. Slosar PJ, Reynolds JB, Schofferman J, Goldthwaite N, White AH, Keaney D.. Patient satisfaction after circumferential lumbar fusion. Spine. 2000;25(6):722-726. [DOI] [PubMed] [Google Scholar]
- 25. Strom RG, Bae J, Mizutani J, Valone F 3rd, Ames CP, Deviren V. Lateral interbody fusion combined with open posterior surgery for adult spinal deformity. J Neurosurg Spine. 2016;25(6):697-705. [DOI] [PubMed] [Google Scholar]