In contrast to previously published reports, we have detected sustained infectivity of aerosolized influenza viruses in respiratory mucus over a wide-range of relative humidity conditions, indicating a risk of airborne transmission in a broad range of environments.
Keywords: Influenza virus, relative humidity, rotating drum, aerosol, mucus, respiratory airway cells, transmission
Abstract
Pandemic and seasonal influenza viruses can be transmitted through aerosols and droplets, in which viruses must remain stable and infectious across a wide range of environmental conditions. Using humidity-controlled chambers, we studied the impact of relative humidity on the stability of 2009 pandemic influenza A(H1N1) virus in suspended aerosols and stationary droplets. Contrary to the prevailing paradigm that humidity modulates the stability of respiratory viruses in aerosols, we found that viruses supplemented with material from the apical surface of differentiated primary human airway epithelial cells remained equally infectious for 1 hour at all relative humidities tested. This sustained infectivity was observed in both fine aerosols and stationary droplets. Our data suggest, for the first time, that influenza viruses remain highly stable and infectious in aerosols across a wide range of relative humidities. These results have significant implications for understanding the mechanisms of transmission of influenza and its seasonality.
Influenza viruses are highly successful pathogens that emerge every winter in temperate regions. Epidemiologically successful influenza viruses must replicate efficiently in humans and transmit via the airborne route [1]. Coughing, talking, and exhaling can release aerosols and droplets of varying sizes containing respiratory fluid and viral particles [2–7]. The spread of influenza virus by either aerosol transmission (inhalation of infectious particles) or fomite transmission (self-inoculation from a contaminated surface) requires that influenza virus remain infectious in a variety of environmental conditions [8].
The risk of airborne disease transmission to a naive host is linked to a combination of environmental and biological factors, including ventilation in buildings, gravitational settling of respiratory droplets out of the air and onto surfaces, and biological inactivation of virus [5, 9, 10]. The link between the environment and influenza virus transmission is evident in the seasonal cycles of influenza virus infections, particularly in temperate regions [11, 12], that coincide with seasonal variations in temperature and absolute humidity [13–16]. Relative humidity (RH) can affect airborne transmission of influenza virus, as shown in the guinea pig model with deficient transmission at mid-range and very high RHs [9]. A partial explanation for this observation may be biological inactivation of influenza virus in aerosols at mid-range RHs, as suggested by the results of studies performed primarily in the 1960s [17–22]. We and others have previously shown that the presence of exogenous proteins in the virus solution can alter the pattern of viral decay in large stationary droplets in response to RH [23] and can prolong the viability of viruses on surfaces [24, 25]. However, these studies do not accurately represent the composition of droplets produced by the human respiratory system and fail to examine the impact of RH on the viability of circulating seasonal influenza virus in aerosols.
Human respiratory droplets contain a variety of proteins, including but not limited to mucins [26, 27], yet droplet composition is difficult to recapitulate in an experimental setting since the precise components and their concentrations are unknown. In some previous studies of influenza virus viability [17–23], proteins were present in the aerosolization medium, but they were not mucins. A source of mucus that may help recapitulate a biologically relevant system to explore virus viability in a controlled experimental setting is extracellular material (ECM) collected from the apical surface of human bronchial epithelial (HBE) cell cultures at an air-liquid interface.
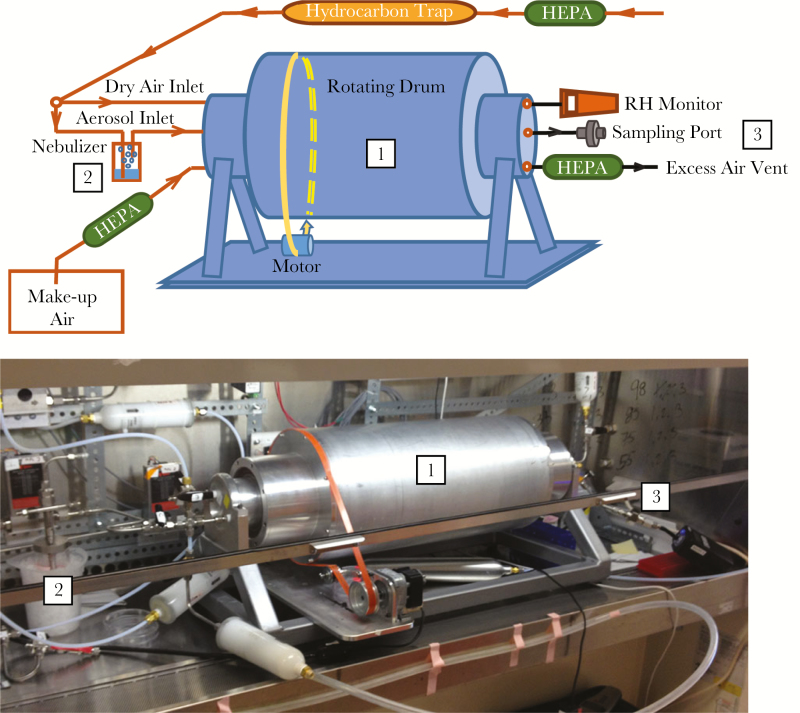
In this work, we have studied the viability of 2009 pandemic influenza A(H1N1) virus (A[H1N1]pdm09) in suspended aerosols and stationary droplets over a wide range of RHs. To mimic a physiologically relevant composition of the aerosols and droplets, we supplemented the suspension medium with HBE ECM. Aerosol experiments took place within a custom rotating drum, which is designed to minimize loss of aerosols due to gravitational settling (Figure 1), as first described by Goldberg et al [28]. Rotating drums have been widely used to study the viability of airborne bacteria and viruses under controlled environmental conditions [17, 19], although not since 1968 for influenza virus [29]. We hypothesized detection of RH-dependent decay of influenza virus in aerosols and were surprised to find sustained infectivity of influenza virus at all RHs. To determine whether this observation might extend to other viruses, we also investigated the survival of aerosolized φ6, a bacteriophage commonly used for studying pathogenic enveloped viruses in the environment [30, 31], with and without the HBE ECM. Our studies suggest that HBE ECM protects influenza virus and φ6 from RH-dependent decay.
Figure 1.
Design of a controlled relative humidity (RH) rotating drum for the aerosolization of influenza viruses. Schematic (top) and photograph (bottom) of the tunable RH rotating drum. The rotating drum (1) is preconditioned to the desired RH prior to aerosolization of the virus. Bulk virus solution is kept on ice and aerosolized via a nebulizer (2) into the drum. The drum is sealed during incubation of the viral aerosols at each specified RH. Viral aerosols are extracted through the sampling port (3) onto a gelatin filter, using a pump, at 2 L/minute for 15 minutes. The gelatin filter is dissolved in warm medium to allow for titration of infectious virus. HEPA, high-efficiency particulate air filter.
METHODS
Cells and Viruses
Primary HBE cells were differentiated from human lung tissue by following an institutional review board–approved protocol and were maintained at an air-liquid interface [32]. HBE ECM was generated by pooling washes (150 µL of phosphate-buffered saline for 10 minutes at 37°C) of the apical surface of uninfected HBE cells from multiple patients. The protein concentration in undiluted HBE ECM was found to be 100–500 μg/mL (BCA assay; Thermo Fisher). Madin-Darby canine kidney (MDCK) cells (ATCC CCL-34) were maintained in Eagle’s minimal essential medium (Sigma) supplemented with 10% fetal bovine serum and L-glutamine.
Influenza A virus, A/California/07/2009 (H1N1)pdm09 Antiviral Resistance (AVR) Reference Virus M2: S31N NA: wild type (wt) (item number FR-458) was obtained through the Influenza Reagent Resource, Influenza Division, World Health Organization Collaborating Center for Surveillance, Epidemiology, and Control of Influenza, Centers for Disease Control and Prevention (Atlanta, GA). Virus stocks were prepared in MDCK cells until the onset of cytopathic effect, clarified by low-speed centrifugation, and concentrated by ultracentrifugation through a 30% sucrose cushion. Virus pellets were resuspended in a 1:10 ratio of HBE ECM to L-15 medium. Virus collected from HBE cells was prepared by infecting each Transwell with 103 50% tissue culture infective doses (TCID50) of A(H1N1)pdm09 per milliliter as described elsewhere [33] and was collected in phosphate-buffered saline 48–72 hours after infection. Influenza virus samples were titered on MDCK cells as previously described [34].
Bacteriophage φ6 was propagated with its host Pseudomonas syringae according to established methods [30]. Virus was harvested in tryptic soy broth (TSB) and stored at 4°C. φ6 stocks were concentrated, and the pellets were resuspended in a 1:10 ratio of HBE ECM to L-15 medium in the same manner as influenza virus. Samples collected from experiments were titered using plaque assays. Briefly, 50 µL of virus was mixed with 200 µL of P. syringae and 4.75 mL of TSB (Sigma) soft agar (0.75% w/v). The mixture was poured over a TSB plate and incubated at 25°C for 24 hours prior to determination of viral titer.
Rotating Drum Experiment for Aerosols
A 27-L aluminum drum, modified from previous studies to fit inside a biosafety cabinet [28], was built to investigate the stability of aerosolized viruses at various RHs. Three inlet ports introduced dry air, aerosols, and saturated air generated by a Collison nebulizer (MRE-3; BGI) and, during sampling, make-up air (Figure 1). House air passed through a high-efficiency particulate air filter (catalog number 12144; Pall) and hydrocarbon trap (BHT-4; Agilent) to provide purified air to the nebulizer and dry air line. Three other ports were dedicated to an RH probe (catalog number HC2-C04; Rotronic), collection of samples, and exhaust flow passing through a high-efficiency particulate air filter to prevent the release of viruses. The drum rotated at a speed of 2.5 rpm, optimized to minimize aerosol losses. All influenza virus aerosolization experiments were done inside a biosafety cabinet.
Seven RHs—23%, 33%, 43%, 55%, 75%, 85%, and 98%—were investigated; they were selected to span environmentally relevant conditions and correspond to levels readily achievable in the droplet experiments described below. The 3 lowest conditions (23%, 33%, and 43% RHs) are representative of dry climates or heated indoor environments during winter. Two moderate conditions (55% and 75% RHs) are typical of indoor environments during warmer seasons. The 2 highest RHs (85% and 98%) occur during rainy periods everywhere and in tropical regions. The RH in the drum was controlled by adjusting the flow rate of dry air (which varied from 0 to 10 L/minute, depending on the targeted RH), and the targeted RH was maintained within ±3%. Temperature and RH were recorded prior to aerosolization and after collection of the aged sample. Temperature was maintained at 25°C ± 1°C throughout all experiments. Representative RH data are provided in Supplementary Table 1.
Aerosolization experiments were conducted with influenza virus in a 1:10 ratio of HBE ECM to L-15 medium, with φ6 in a 1:10 ratio of HBE ECM to L-15 medium, and with φ6 in TSB. For each experiment, the corresponding virus-free medium was nebulized to condition the drum to the desired RH. The aerosol flow rate was maintained at 3.9 L/minute at all RHs except 23% because nearly all inflow was distributed to dry air to achieve the desired RH. During conditioning, air at the targeted RH was collected into a separate polyethylene bag (AtmosBag; Sigma) to use as make-up air during sample collection, to maintain a constant RH. After conditioning, virus was aerosolized at the same flow rate for 20 minutes to fill the drum. While aerosolization proceeded, samples were collected onto 25-mm gelatin filters (catalog number 225−9551; SKC) installed in stainless steel holders (catalog number 304500; Advantec), at a flow rate of 2 L/minute for 15 minutes. These represented “unaged” samples. The drum was then sealed, and viral aerosols were aged for 1 hour, which was chosen to represent typical air-exchange rates in residences and some office buildings [35–39]. One hour is longer than prescribed by ASHRAE (formerly known as the American Society of Heating, Refrigerating, and Air-Conditioning Engineers). Aged aerosol samples were collected in the same way as unaged samples, and the gelatin filters were dissolved in 3 mL of warm medium and stored at −80°C prior to virus titration.
Correction for Physical Loss of Aerosols
A mass balance equation was used to correct for loss of aerosols via gravitational settling and dilution during aging, assuming first-order decay for both processes. Instantaneous measurement of infectious virus titer was not possible, so this correction assumed that the measured virus titers represent time averages over the 15-minute sampling period. The particle physical loss coefficient (kp; units are minutes−1) and dilution coefficient (kd; units are minutes−1) were determined as described previously [40]. The equations for this correction are shown in the Supplementary Materials.
RH Chamber Experiment for Stationary Droplets
Stationary droplets were incubated in chambers with RH controlled using saturated salt solutions (Supplementary Figure 3A and 3B) [23]. Chambers were maintained within a biosafety cabinet at approximately 22°C. RH and temperature data were collected for each experiment, using a HOBO UX100-011 data logger (Onset; representative data are in Supplementary Figure 3C). After incubation for 1 hour to achieve the desired RH, 10 stationary 1-µL virus droplets were incubated for 1 or 2 hours at each RH and then collected in 500 µL of L-15 medium. A total of 10 µL of enclosed virus samples were incubated outside the chamber during the experiment. Data are presented as log decay [23]. All data are available on request.
RESULTS
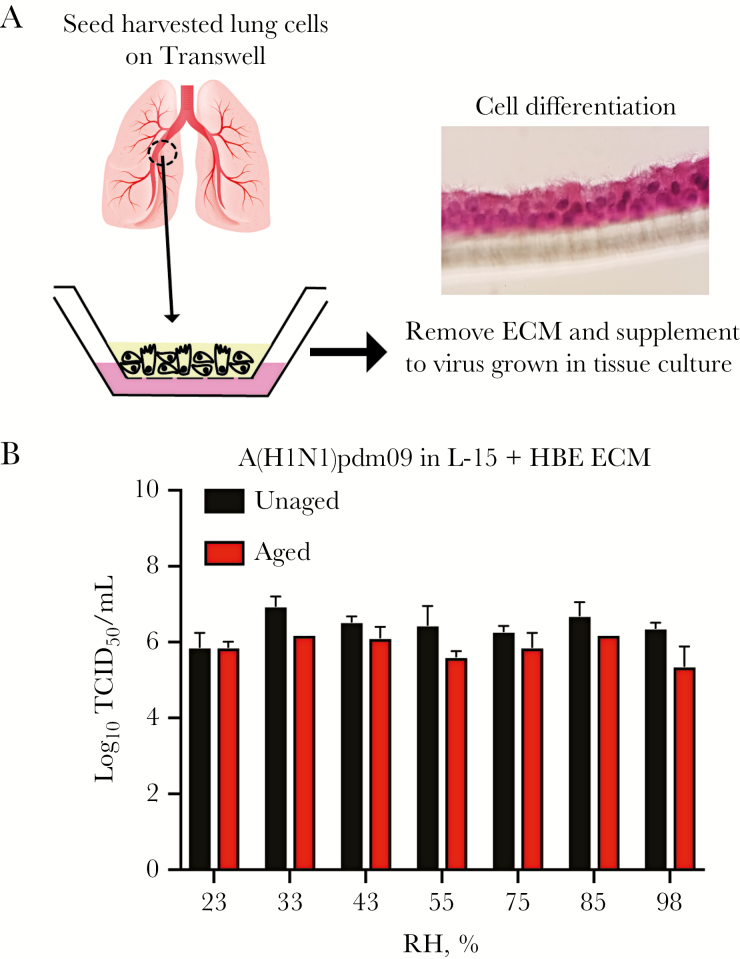
Aerosolized Influenza Virus Remains Infectious at All RHs
To study the impact of RH on the viability of airborne influenza virus, we aerosolized A(H1N1)pdm09 into a custom rotating drum (Figure 1), aged the aerosols for 1 hour, and then collected aerosols for analysis of infectivity by a TCID50 assay on MDCK cells. The bulk virus solution was prepared in traditional tissue culture cells and supplemented with HBE ECM (Figure 2A) to simulate respiratory secretions that would be expelled from an infected person. We observed a <0.5-log reduction in the amount of infectious A(H1N1)pdm09 in the aged aerosols in the presence of HBE ECM at each RH tested, which is within the error of our assay (Figure 2B). There was no loss in virus viability in the bulk virus solution during the aerosolization process, which includes recirculation of larger aerosols that were trapped by the nebulizer, because the virus titer before and after each experiment was unchanged (Supplementary Figure 1).
Figure 2.
Influenza virus maintains infectivity in fine aerosols at all relative humidities (RHs). A, Schematic representing preparation of the virus in physiological aerosolization medium including extracellular material (ECM) produced by primary human bronchial epithelial (HBE) cells. Inset is a hematoxylin and eosin–stained image of HBE cells, demonstrating the 3-dimensional culture. B, Infectivity of aerosolized 2009 pandemic influenza A(H1N1) virus (A[H1N1]pdm09) supplemented with HBE ECM from uninfected cells in L-15 tissue culture medium. The amount of virus before and after 1 hour of aging in aerosols was determined by a 50% tissue culture infective dose (TCID50) assay on Madin-Darby canine kidney cells. Data represent mean values ± standard deviations of 3 independent biological replicates, exclusive of 85% RH, which was done twice.
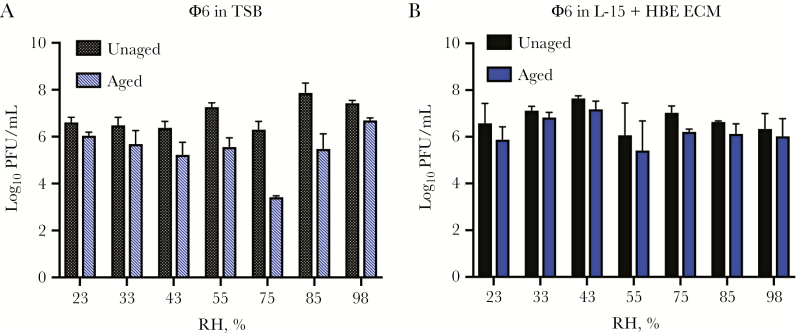
Addition of Respiratory Extracellular Material Protects φ6 Viruses From Decay at All RHs
We found A(H1N1)pdm09 to be remarkably resistant to RH-induced decay at all RHs in our rotating drum. To further explore this finding, we conducted additional studies with an enveloped virus, bacteriophage φ6, in the presence and absence of HBE ECM. We aerosolized φ6 in traditional laboratory growth medium into the rotating drum and found that φ6 decayed in aerosols in an RH-dependent manner after 1 hour (Figure 3A). In contrast, φ6 in medium supplemented with HBE ECM showed little to no decay at all RHs tested, as with A(H1N1)pdm09 (Figure 3B). Taken together with the A(H1N1)pdm09 data, we provide strong evidence that HBE ECM can protect enveloped viruses from RH-dependent decay in aerosols for at least 1 hour.
Figure 3.
Presence of primary human bronchial epithelial (HBE) cell extracellular material (ECM) protects φ6 bacteriophage from decay at mid-range relative humidities (RHs). A, Infectivity of aerosolized φ6 in tryptic soy broth (TSB) was tested at a range of RHs within the rotating drum. B, As with 2009 pandemic influenza A(H1N1) virus (A[H1N1]pdm09), φ6 was aerosolized in medium containing HBE ECM for comparison of virus titer in unaged aerosols and aerosols aged for 1 hour. The amount of virus before and after aging was determined by plaque assay. Data represent mean values ± standard deviations of 3 independent biological replicates. PFU, plaque-forming units.
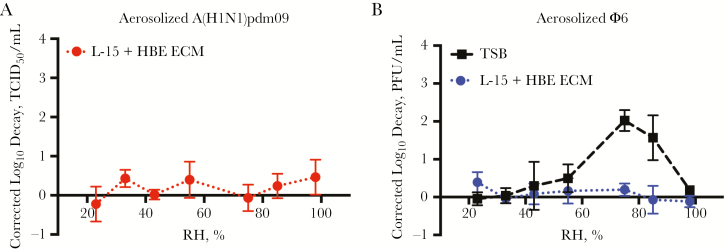
Adjustment for Physical Loss of Aerosols in a Rotating Drum
The rotating drum reduced but did not eliminate physical losses of aerosols due to gravitational settling. Furthermore, the sample of aged aerosols collected at the end of the 1 hour aging period was subject to dilution by RH-conditioned make-up air. Therefore, a mass balance equation specific to each aerosolization medium was used to account for these processes, assuming first-order decay for both gravitational settling and dilution (Supplementary Figure 2). As expected, physical loss of aerosols due to settling was greater at higher RHs because they evaporated less and were larger. Application of this equation to the data allows measurement of the change in viral infectivity unbiased by physical loss of aerosols within the drum. Corrected log10 decay values confirmed the lack of decay of A(H1N1)pdm09 (Figure 4A) and φ6 (Figure 4B) in the presence of HBE ECM. φ6 experienced up to a 2 log10 decay at 75% and 85% RH without HBE ECM (TSB in Figure 4B), confirming our observation that it protects aerosolized viruses from RH-dependent decay.
Figure 4.
Viral decay corrected for physical loss of aerosols within the rotating drum. A, Log10 decay of 2009 pandemic influenza A(H1N1) virus (A[H1N1]pdm09) aerosolized with primary human bronchial epithelial (HBE) cell extracellular material (ECM) was calculated as the difference in log10 titer between aged and unaged samples at each relative humidity (RH). A mass balance equation was used to correct for physical loss of aerosols due to gravitational settling and dilution. B, Log10 decay of φ6 in traditional laboratory medium (black) and HBE ECM (blue) demonstrates protection from decay at 75% and 85% RH. PFU, plaque-forming units; TCID50, 50% tissue culture infective dose; TSB, tryptic soy broth.
Influenza Virus in Stationary Droplets Remains Infectious at All RHs
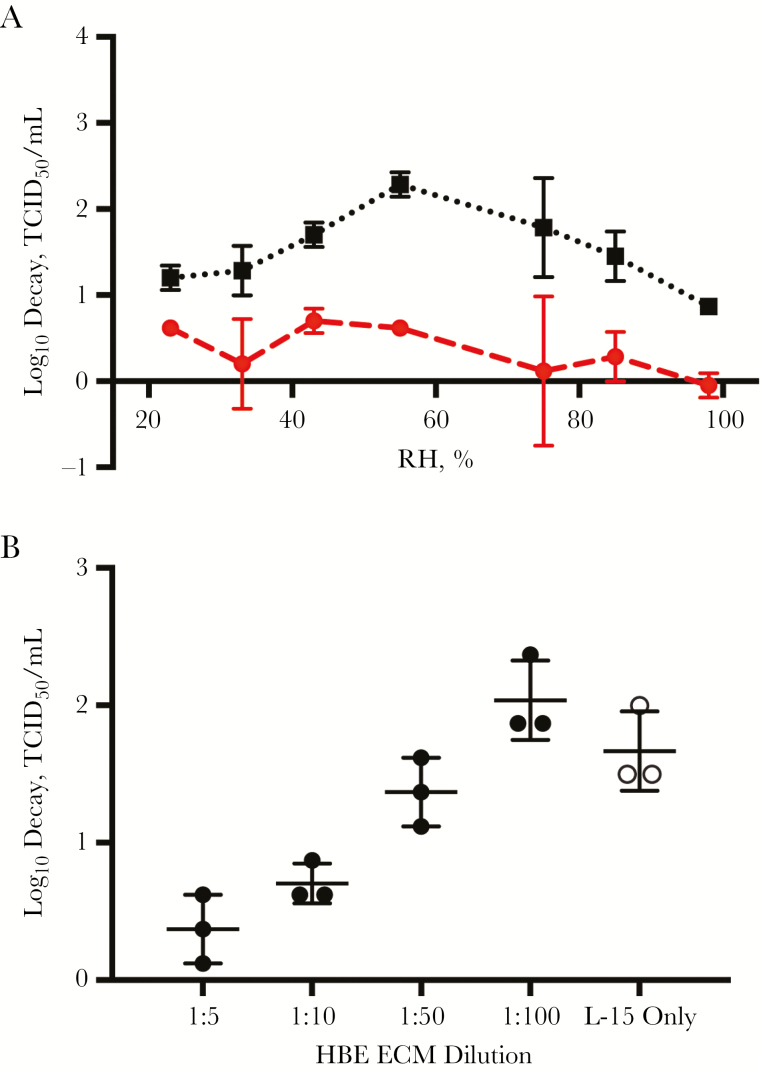
To test whether HBE ECM also protected influenza virus from decay in stationary droplets, we performed a series of studies with A(H1N1)pdm09 in stationary, 1-µL droplets exposed to the same RH conditions used in the rotating drum. RH was maintained using saturated aqueous salt solutions within an enclosed chamber (Supplementary Figure 3A) and, along with temperature, was continuously monitored during each experiment, to ensure stability of the specified RH (Supplementary Figure 3 B and 3C). Consistent with our analysis of φ6 and A(H1N1)pdm09 viability in aerosols, we observed that A(H1N1)pdm09 experienced very little decay in infectivity in stationary droplets containing HBE ECM at each RH tested (Figure 5A). In contrast, there was an RH-dependent decay of virus infectivity in droplets lacking exogenous HBE ECM, with peak loss at 55% RH. Decay in virus infectious titer exceeded 1 log10 across all RHs, and the concentration decayed over 2 log10 at 55% RH. Further, we found this protective effect at 55% RH to be dependent on the concentration of exogenous ECM. We supplemented A(H1N1)pdm09 with 1:5, 1:10, 1:50, and 1:100 dilutions of HBE ECM, finding that the 1:50 and 1:100 samples decayed similarly to control virus without exogenous HBE ECM after 1 hour at 55% RH (Figure 5B). Similar droplet experiments that compared the viability of virus collected from either infected transformed tissue culture or primary differentiated HBE cells also indicated a lack of RH-dependent decay in the HBE-propagated viruses (Supplementary Figure 4). This result indicates that the protection observed with HBE ECM collected from uninfected cells behaves similarly to ECM from infected cells that would be present in expelled aerosols in nature.
Figure 5.
Exogenous primary human bronchial epithelial (HBE) cell extracellular material (ECM) protects influenza virus from decay in stationary droplets. The viability of 2009 pandemic influenza A(H1N1) virus (A[H1N1]pdm09) was tested in stationary droplets at a range of different relative humidities (RHs) in a controlled RH chamber. Virus samples were compared with (circles) and without (squares) exogenous HBE ECM. A, RH-dependent decay of A(H1N1)pdm09 with (red) and without (black) exogenous HBE ECM after 1 hour. Data represent mean values ± standard deviations from 3 biological replicates. B, Protection from decay of A(H1N1)pdm09 in droplets is dependent on the concentration of HBE ECM. Virus was prepared with (shaded circles) or without (open circles) HBE ECM dilutions in L-15 tissue culture medium. Droplets were incubated at 55% RH for 1 hour. Individual data points are shown, with error bars indicating standard deviations, and are representative of at least 2 biological replicates. TCID50, 50% tissue culture infective dose.
Influenza Virus Viability in Stationary Droplets Is Not Dependent on Virus Concentration
The φ6 and A(H1N1)pdm09 bulk virus solutions used for our rotating drum experiments had titers ranging from 108 to 109 plaque-forming units/mL or TCID50/mL. Individuals infected with A(H1N1)pdm09 shed approximately 105 RNA copies/mL, as determined by quantitation of virus from nasopharyngeal specimens [41, 42]. To assess whether the sustained infectivity of influenza virus over a range of RHs was dependent on virus concentration, we determined the viability of 10-fold serial dilutions of A(H1N1)pdm09 (109–104 TCID50/mL) in stationary droplets (Supplementary Figure 5). We observed very little decay of infectivity for all virus concentrations and all RHs tested.
DISCUSSION
Here we provide new insights into the interplay of humidity and respiratory virus viability in expelled aerosols and droplets that has long been proposed to influence influenza virus transmission. We have previously demonstrated that release of submicron aerosols containing influenza virus correlated with efficient transmission of A(H1N1)pdm09 in the ferret model [43]. In both humans and animal models, aerosol transmission of human influenza virus has been suggested to be equally or more efficient than fomite transmission [44–46].
RH has previously been shown to impact the viability of influenza virus in aerosols and stationary droplets [5, 17–22]. Contrary to prevailing wisdom, we found that aerosolized influenza virus lost little infectivity over a wide range of RHs, indicating that virus decay is not a barrier to efficient aerosol transmission of influenza virus. The infectivity of A(H1N1)pdm09 was sustained in aerosols for up to 1 hour at all 7 RHs tested (Figures 2B and 4A). Based on these observations, we postulated that the lack of RH-dependent decay in aerosols results from protection conferred by supplementation of the viruses with HBE ECM. We confirmed this idea by evaluating bacteriophage φ6 in the absence and presence of HBE ECM (Figures 3 and 4B). Complementary studies of influenza virus in stationary droplets, both with exogenous HBE ECM and virus collected from infected HBE cells (Figure 5 and Supplementary Figure 4), similarly recapitulated the protective effect of HBE ECM against RH-dependent decay of viral infectivity.
The protective effect of HBE ECM was concentration dependent (Figure 5B), raising the question of how well the media composition represented that of actual aerosols and droplets expelled by an infected host. The total protein concentration in the diluted aerosolization media fell at the lower end of the range reported in different types of respiratory fluid [47]; the exact origin of virus-laden aerosols within the respiratory system and their chemical composition are not known. Although protein is an obvious candidate, it is possible that something other than protein in HBE ECM protects the virus from decay. Even though the concentration of virus in our experimental aerosols and droplets may have been higher than found in real ones, studies using a series of serially diluted A(H1N1)pdm09 samples did not indicate a concentration-dependent response to RH, suggesting that viability of respiratory viruses in expelled droplets with much lower viral load is also maintained.
Our observations have substantial implications for understanding transmission of epidemiologically successful seasonal and pandemic influenza virus and other respiratory pathogens, and they reaffirm the importance of aerosolized respiratory droplets as vehicles for transmission. Studies in the guinea pig model have shown that airborne influenza virus transmission is deficient at 50% RH, perhaps due to biological inactivation of viruses in aerosols [9]. However, transmission of influenza virus in ferrets is routinely studied at RHs close to 50%, resulting in 100% transmission efficiency of the A(H1N1)pdm09 [43, 48]. Our data indicate that exhaled viruses likely have not been inactivated at this RH, although whether guinea pig respiratory secretions offer protection to viruses similar that offered by HBE ECM is unknown. We have also shown that aerosol gravitational settling within our rotating drum increases as RH increases (Supplementary Figure 2), which is consistent with a reanalysis of the guinea pig study by Lowen et al that concluded that RH effects on aerosol size and transport can explain the results without invoking airborne virus viability [49]. At higher RHs, much less evaporation and shrinkage of aerosolized respiratory droplets occurs, resulting in more of them settling out of the air and contaminating fomites [5]. Therefore, RH-dependent biological inactivation of influenza virus in aerosols and droplets may not significantly affect the efficiency of airborne transmission, suggesting a more substantial role for physical factors that act directly on the droplet vehicle.
Our novel use of HBE ECM to recapitulate physiologically relevant expelled aerosols and droplets has revealed that the classical paradigm regarding the decay of influenza virus at mid-range RHs may not accurately represent the processes that occur in nature. These data support the notion that influenza virus may have evolved to exploit host protective barriers to support efficient airborne transmission via creation of a stable microenvironment for the viruses released into the air. While the ECM of the respiratory tract may change during influenza virus infection, our observation that viruses propagated in HBE cells were also protected from RH-mediated decay (Supplementary Figure 4) suggests that uninfected HBE ECM acts as a reasonable surrogate to study this effect.
Our findings raise a host of questions for future investigation. Studies are required to identify the contribution of other factors, including temperature and virus strain background, that may also affect viability of influenza virus in aerosols and contribute to the seasonal emergence of influenza virus. Characterization of the composition of respiratory droplets emitted by infected hosts will identify the factors that confer protection of influenza virus from environmental decay. Specifically, investigation into the structure and composition of respiratory secretions is needed. Rheological characterization of viscoelasticity and other physical properties of mucus has enhanced understanding of disease pathology at mucosal surfaces [50]. Similar studies of the HBE mucosal matrix will identify host factors affecting the stability of influenza virus released from the respiratory tract. Further investigation of the kinetics of virus decay in aerosols and droplets is also needed. Prior studies have shown that decay is most rapid within the first approximately 15 minutes after aerosolization [17, 20, 21]. The way we conducted our experiments in the rotating drum, our “unaged” aerosols spanned a range of ages, from near zero to several minutes, during which some decay, possibly RH dependent, might have occurred.
The results of our studies have important implications for the control of airborne influenza virus transmission. Based on our observations, we recommend a combination of increased air exchange rates coupled with filtration or UV irradiation of recirculated air, as well as regular disinfection of high-touch surfaces to minimize transmission. Use of personal protective equipment that reduces inhalation exposure to infectious aerosols, such as N95 respirators, may be recommended to healthcare professionals in high-risk situations. The results of this study have substantial implications for understanding transmission of epidemiologically successful seasonal and pandemic influenza virus and other respiratory pathogens, and they reaffirm the importance of aerosolized respiratory droplets as vehicles for transmission.
Supplementary Data
Supplementary materials are available at The Journal of Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Acknowledgments. We thank the members of the Marr and Lakdawala laboratories and Dr Peter Vikesland, for his helpful discussion and review of drafts of this manuscript.
Financial support. This work was supported by the National Institutes of Health (NIH) through the NIH Director’s New Innovator Award Program (1-DP2-A1112243); the Virginia Tech Institute for Critical Technology and Applied Science; the Fulbright Scholar Program; the National Institute of Allergy and Infectious Diseases, NIH (K22 grant AI108600-01 and T32 award AI049820); and the NIH and the Cystic Fibrosis Foundation Research Development Program (grant P30DK072506 to the University of Pittsburgh).
Potential conflicts of interest. All authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
Presented in part: American Society for Virology 36th Annual Meeting, Madison, Wisconsin, 24–28 June 2017; 36th American Association for Aerosol Research Annual Conference, Raleigh, North Carolina, 16–20 October 2017; Biology of Acute Respiratory Infection Gordon Research Seminar/Gordon Research Conference, Ventura, California, 17–23 March 2018.
References
- 1. Lakdawala SS, Subbarao K. The ongoing battle against influenza: The challenge of flu transmission. Nat Med 2012; 18:1468–70. [DOI] [PubMed] [Google Scholar]
- 2. Lindsley WG, Blachere FM, Beezhold DH, et al. . Viable influenza A virus in airborne particles expelled during coughs versus exhalations. Influenza Other Respir Viruses 2016; 10:404–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lindsley WG, Noti JD, Blachere FM, et al. . Viable influenza A virus in airborne particles from human coughs. J Occup Environ Hyg 2015; 12:107–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Milton DK, Fabian MP, Cowling BJ, Grantham ML, McDevitt JJ. Influenza virus aerosols in human exhaled breath: particle size, culturability, and effect of surgical masks. PLoS Pathog 2013; 9:e1003205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Yang W, Marr LC. Dynamics of airborne influenza A viruses indoors and dependence on humidity. PLoS One 2011; 6:e21481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fabian P, McDevitt JJ, DeHaan WH, et al. . Influenza virus in human exhaled breath: an observational study. PLoS One 2008; 3:e2691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Yan J, Grantham M, Pantelic J, et al. ; EMIT Consortium Infectious virus in exhaled breath of symptomatic seasonal influenza cases from a college community. Proc Natl Acad Sci U S A 2018; 115:1081–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Tang JW. The effect of environmental parameters on the survival of airborne infectious agents. J R Soc Interface 2009; 6(Suppl 6):S737–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lowen AC, Mubareka S, Steel J, Palese P. Influenza virus transmission is dependent on relative humidity and temperature. PLoS Pathog 2007; 3:1470–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Tang JW, Li Y, Eames I, Chan PK, Ridgway GL. Factors involved in the aerosol transmission of infection and control of ventilation in healthcare premises. J Hosp Infect 2006; 64:100–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Tamerius J, Nelson MI, Zhou SZ, Viboud C, Miller MA, Alonso WJ. Global influenza seasonality: reconciling patterns across temperate and tropical regions. Environ Health Perspect 2011; 119:439–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Tang JW, Loh TP. Influenza seasonality. Curr Treat Options Infect Dis 2016; 8:343–67. [Google Scholar]
- 13. Deyle ER, Maher MC, Hernandez RD, Basu S, Sugihara G. Global environmental drivers of influenza. Proc Natl Acad Sci U S A 2016; 113:13081–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Shaman J, Goldstein E, Lipsitch M. Absolute humidity and pandemic versus epidemic influenza. Am J Epidemiol 2011; 173:127–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Shaman J, Kohn M. Absolute humidity modulates influenza survival, transmission, and seasonality. Proc Natl Acad Sci U S A 2009; 106:3243–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Shaman J, Pitzer VE, Viboud C, Grenfell BT, Lipsitch M. Absolute humidity and the seasonal onset of influenza in the continental United States. PLoS Biol 2010; 8:e1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Harper GJ. Airborne micro-organisms: survival tests with four viruses. J Hyg (Lond) 1961; 59:479–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hemmes JH, Winkler KC, Kool SM. Virus survival as a seasonal factor in influenza and poliomylitis. Antonie Van Leeuwenhoek 1962; 28:221–33. [DOI] [PubMed] [Google Scholar]
- 19. Hood AM. Infectivity of influenza virus aerosols. J Hyg (Lond) 1963; 61:331–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Noti JD, Blachere FM, McMillen CM, et al. . High humidity leads to loss of infectious influenza virus from simulated coughs. PLoS One 2013; 8:e57485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Schaffer FL, Soergel ME, Straube DC. Survival of airborne influenza virus: effects of propagating host, relative humidity, and composition of spray fluids. Arch Virol 1976; 51:263–73. [DOI] [PubMed] [Google Scholar]
- 22. Shechmeister IL. Studies on the experimental epidemiology of respiratory infections. III. Certain aspects of the behavior of type A influenza virus as an air-borne cloud. J Infect Dis 1950; 87:128–32. [DOI] [PubMed] [Google Scholar]
- 23. Yang W, Elankumaran S, Marr LC. Relationship between humidity and influenza a viability in droplets and implications for influenza’s seasonality. PLoS One 2012; 7:e46789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Parker ER, Wolcott AB, Dunham MD, Mac Neal WJ. Resistance of the Melbourne strain of influenza virus to desiccation. J Lab Clin Med 1943:37–42. [Google Scholar]
- 25. Thomas Y, Vogel G, Wunderli W, et al. . Survival of influenza virus on banknotes. Appl Environ Microbiol 2008; 74:3002–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Casado B, Pannell LK, Iadarola P, Baraniuk JN. Identification of human nasal mucous proteins using proteomics. Proteomics 2005; 5:2949–59. [DOI] [PubMed] [Google Scholar]
- 27. Joo NS, Evans IA, Cho HJ, Park IH, Engelhardt JF, Wine JJ. Proteomic analysis of pure human airway gland mucus reveals a large component of protective proteins. PLoS One 2015; 10:e0116756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Goldberg LJ, Watkins HM, Boerke EE, Chatigny MA. The use of a rotating drum for the study of aerosols over extended periods of time. Am J Hyg 1958; 68:85–93. [DOI] [PubMed] [Google Scholar]
- 29. Mitchell CA, Guerin LF, Robillard J. Decay of influenza A viruses of human and avian origin. Can J Comp Med 1968; 32:544–6. [PMC free article] [PubMed] [Google Scholar]
- 30. Lin K, Marr LC. Aerosolization of Ebola virus surrogates in wastewater systems. Environ Sci Technol 2017; 51:2669–75. [DOI] [PubMed] [Google Scholar]
- 31. Turgeon N, Toulouse MJ, Martel B, Moineau S, Duchaine C. Comparison of five bacteriophages as models for viral aerosol studies. Appl Environ Microbiol 2014; 80:4242–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Myerburg MM, Harvey PR, Heidrich EM, Pilewski JM, Butterworth MB. Acute regulation of the epithelial sodium channel in airway epithelia by proteases and trafficking. Am J Respir Cell Mol Biol 2010; 43:712–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Nturibi E, Bhagwat AR, Coburn S, Myerburg MM, Lakdawala SS. Intracellular colocalization of influenza viral RNA and Rab11A is dependent upon microtubule filaments. J Virol 2017; 91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Reed LJ, Muench H. A simple method of estimating fifty per cent endpoints. Am J Hyg 1938; 27:493–7. [Google Scholar]
- 35. Breen MS, Breen M, Williams RW, Schultz BD. Predicting residential air exchange rates from questionnaires and meteorology: model evaluation in central North Carolina. Environ Sci Technol 2010; 44:9349–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Daisey JM, Angell WJ, Apte MG. Indoor air quality, ventilation and health symptoms in schools: an analysis of existing information. Indoor Air 2003; 13:53–64. [DOI] [PubMed] [Google Scholar]
- 37. Murray DM, Burmaster DE. Residential air exchange-rates in the United-States - empirical and estimated parametric distributions by season and climatic region. Risk Anal 1995; 15:459–65. [Google Scholar]
- 38. Nazaroff WW. Indoor particle dynamics. Indoor Air 2004; 14(Suppl 7):175–83. [DOI] [PubMed] [Google Scholar]
- 39. Yamamoto N, Shendell DG, Winer AM, Zhang J. Residential air exchange rates in three major US metropolitan areas: results from the Relationship Among Indoor, Outdoor, and Personal Air Study 1999–2001. Indoor Air 2010; 20:85–90. [DOI] [PubMed] [Google Scholar]
- 40. Quadros ME, Marr LC. Silver nanoparticles and total aerosols emitted by nanotechnology-related consumer spray products. Environ Sci Technol 2011; 45:10713–9. [DOI] [PubMed] [Google Scholar]
- 41. Lee N, Chan PK, Hui DS, et al. . Viral loads and duration of viral shedding in adult patients hospitalized with influenza. J Infect Dis 2009; 200:492–500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Suess T, Buchholz U, Dupke S, et al. . Shedding and transmission of novel influenza virus A/H1N1 infection in households--Germany, 2009. Am J Epidemiol 2010; 171:1157–64. [DOI] [PubMed] [Google Scholar]
- 43. Lakdawala SS, Lamirande EW, Suguitan AL Jr, et al. . Eurasian-origin gene segments contribute to the transmissibility, aerosol release, and morphology of the 2009 pandemic H1N1 influenza virus. PLoS Pathog 2011; 7:e1002443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Mubareka S, Lowen AC, Steel J, Coates AL, García-Sastre A, Palese P. Transmission of influenza virus via aerosols and fomites in the guinea pig model. J Infect Dis 2009; 199:858–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Tellier R. Review of aerosol transmission of influenza A virus. Emerg Infect Dis 2006; 12:1657–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Cowling BJ, Ip DK, Fang VJ, et al. . Aerosol transmission is an important mode of influenza A virus spread. Nat Commun 2013; 4:1935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Vejerano EP, Marr LC. Physico-chemical characteristics of evaporating respiratory fluid droplets. J R Soc Interface 2018; 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Lakdawala SS, Jayaraman A, Halpin RA, et al. . The soft palate is an important site of adaptation for transmissible influenza viruses. Nature 2015; 526:122–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Halloran SK, Wexler AS, Ristenpart WD. A comprehensive breath plume model for disease transmission via expiratory aerosols. PLoS One 2012; 7:e37088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Lai SK, Wang YY, Wirtz D, Hanes J. Micro- and macrorheology of mucus. Adv Drug Deliv Rev 2009; 61:86–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.