Extrauterine lipoleiomyomas are rare tumors with only three cases reported in the medical literature. These benign soft tissue tumors are characterized by fat between muscle cells. Although these tumors are most often observed in the uterus, as well as associated with hormone replacement therapy (HRT), lipoleiomyomas can develop outside the uterus.1 Herein, we describe a case of a preperitoneal extrauterine lipoleiomyoma.
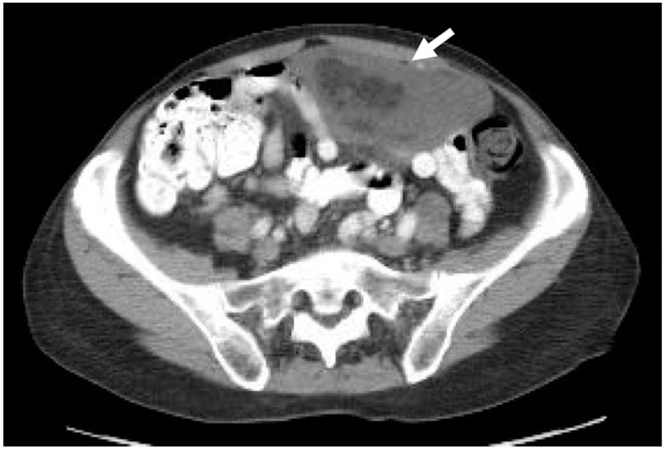
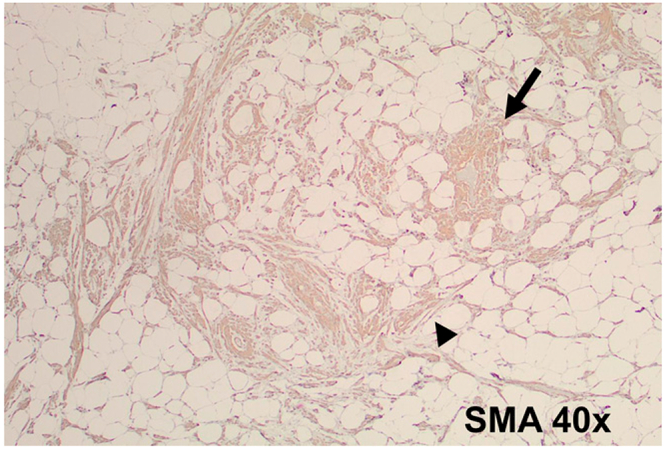
A 67-year-old postmenopausal female without significant past medical history or prior HRT presented for a follow-up of an incidentally discovered mass in the lower abdomen. On a CT scan with contrast, a 12 × 11 × 5-cm mass was noted in the abdomen (Fig. 1) and appeared to extend from the level of the umbilicus inferiorly to the dome of the bladder and uterine fundus. The imaging characteristics were notable for a heterogeneously appearing mass with Hounsfield units compatible with areas of fat and soft tissue. She subsequently underwent a CT-guided percutaneous biopsy of the mass, which revealed proliferation of bland spindle cells based on hemotoxylin and eosin staining. Given the tumor size and uncertain diagnosis, it was therefore recommended that she undergo radical surgical resection of the mass. Therefore, she underwent an exploratory laparotomy with resection of a preperitoneal abdominal wall mass measuring 10 × 8.5 × 4.5-cm with easily defined planes. There was no intraperitoneal involvement of adjacent organs or bowel. She tolerated the procedure well and was discharged to home without complications. Pathologic review demonstrated the presence of benign spindle cells with mature adipose tissue and smooth muscle elements. Immunohistochemical analyses revealed that bundles of spindle cells were positive for desmin and smooth muscle actin (SMA) (Fig. 2). These bundles of spindle cells were negative for CD34, S-100, and human melanoma black 45. Trichrome staining demonstrated abundant fibrosis.
Fig. 1.
CT of the abdomen demonstrates a 10.6 × 5.4 × 9.5 cm heterogeneous mass with areas of fat and soft tissue/fluid density (arrow) extending from the umbilicus to the bladder.
Fig. 2.
Photomicrograph (40×) demonstrates positive immunostaining for SMA in the eosinophilic bundles consistent with smooth muscle differentiation (arrow and arrowhead).
As previously noted, cross-sectional imaging suggested a fat-containing lower abdominal mass. At the time of resection, she had a 10-cm extraperitoneal tumor in the lower abdominal wall with easily defined fat planes. Final pathological diagnosis confirmed the presence of benign spindle cell neoplasm with mature adipose tissue and smooth muscle elements consistent with extrauterine lipoleiomyoma. Whereas uterine lipoleiomyomas are frequently associated with HRT, extrauterine lipoleiomyomas are a rare subtype of lipoma, the most common benign soft tissue tumor.
Given the MRI appearance of an encapsulated tumor and what appeared to be an intraabdominal location, there was concern for tumors ranging from gastrointestinal stromal tumor (GIST) to angiomyolipoma and liposarcoma (well-differentiated and dedifferentiated). Although there is some overlap between the three, the distinction is based on histological, immunohistochemical, and occasionally molecular analyses. Although the presence of abundant fat and smooth muscle can be seen with angiomyolipoma, the patient did not present with a clinical picture of tuberous sclerosis, the context in which angiomyolipomas are most often present.2 Angiomyolipoma was ruled out in this case by the absence of human melanoma black 45 immunostaining, which is normally present in this entity.2 The distinction between liposarcoma and lipoleiomyoma was made on the basis of benign histologic features. Unlike lipoleiomyomas, well-differentiated liposarcomas or atypical lipomatous tumors have cytologic atypia, may contain multivacuolated lipoblasts, have increased mitoses, and can harbor MDM2 translocations leading to protein overexpression. Although spindle cells are seen in GIST, the diffuse positivity for SMA and desmin within the spindle cells, and an absence of CD34-positive cells (normally patchy positive in GIST) confirm smooth muscle differentiation.3 Schwannoma was also included in the differential diagnosis, because it is another spindle cell neoplasm that can originate in this location. However, this diagnosis was ruled out based on the lack of staining for the S100 protein.4
Combining the clinical, radiographic, intraoperative, and final pathologic findings to rule out liposarcoma, angiomyolipoma, and GIST, a diagnosis of abdominal lipoleiomyoma was made based on the postresection histopathological and immunohistochemical analyses. Our patient tolerated the surgery well, and there was no need for long-term follow-up, given the benign nature of this tumor.
In summary, although the presence of an extrauterine lipoleiomyoma in postmenopausal women is rare, it should be included on the differential diagnosis of heterogeneously enhancing fat-containing intraperitoneal and extraperitoneal masses with soft tissue components, as well as bland appearing tumor cells with both spindeloid and adipocytic features.
Contributor Information
Krishna Bommakanti, University of California San Diego School of Medicine La Jolla, California
Mark A. Valasek, University of California San Diego School of Medicine, La Jolla, California; and the, Department of Pathology, University of California San Diego, La Jolla, California
Jason K. Sicklick, University of California San Diego School of Medicine, La Jolla, California; and the, Division of Surgical Oncology, Department of Surgery, Moores UCSD Cancer Center, University of California San Diego, La Jolla, California
REFERENCES
- 1.Lalor PF, Uribe A, Daum GS. De novo growth of a large preperitoneal lipoleiomyoma of the abdominal wall. Gynecol Oncol 2005;97:719–21. [DOI] [PubMed] [Google Scholar]
- 2.Gaskin CM, Helms CA. Lipomas, lipoma variants, and welldifferentiated liposarcomas (atypical lipomas): results of MRI evaluations of 126 consecutive fatty masses. AJR Am J Roentgenol 2004;182:733–9. [DOI] [PubMed] [Google Scholar]
- 3.van Roggen JFG, van Velthuysen MLF, Hogendoorn PCW. The histopathological differential diagnosis of gastrointestinal stromal tumours. J Clin Pathol 2001;54:96–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fletcher CDM, Berman JJ, Corless C, et al. Diagnosis of gastrointestinal stromal tumors: a consensus approach. Int J Surg Pathol 2002;10:81–9. [DOI] [PubMed] [Google Scholar]