Abstract
Background
Permanent pacemaker (PPM) has been touted as an inconsequential complication following Transcatheter Aortic Valve Replacement (TAVR). As TAVR moves to lower risk patients, the long-term implications remain poorly understood; therefore we evaluated the long-term outcomes of pacemaker in Surgical Aortic Valve Replacement (SAVR) patients.
Methods
A total of 2,600 consecutive patients undergoing SAVR over the past 15 years were reviewed using an institutional Society of Thoracic Surgeons (STS) database and social security death records. Patients were stratified by placement of a PPM within 30-days of surgery. The impact of PPM placement on long-term survival was assessed by Kaplan-Meier analysis and risk-adjusted survival by Cox Proportional Hazards modeling.
Results
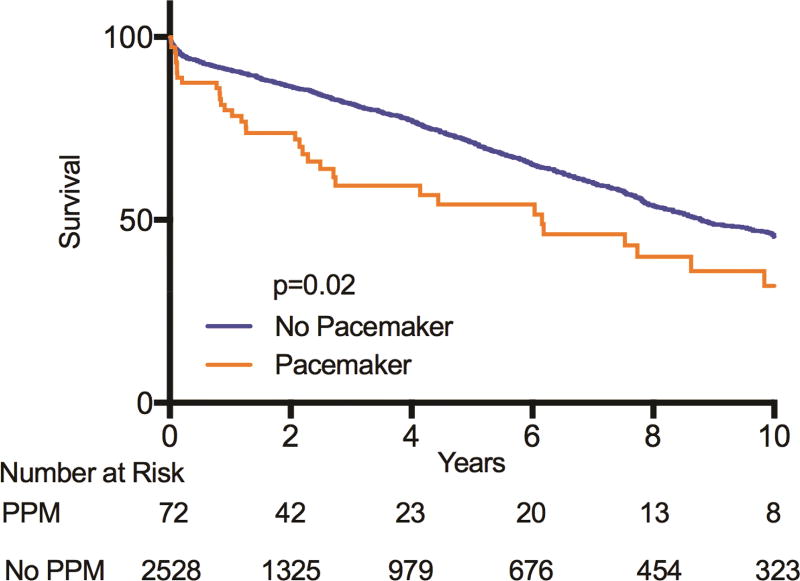
A total of 72 (2.7%) patients required PPM placement postoperatively. Patients requiring PPM had more postoperative complications including atrial fibrillation (43.1% vs 27.0%, p=0.003), prolonged ventilation (16.7 vs 5.7%, p<0.0001) and renal failure (12.5 vs 4.6%, p=0.002). These led to greater resource utilization including longer ICU (89 vs 44 hours, p<0.0001) and hospital (9 vs 6 days, p<0.0001) lengths of stay and higher inflation-adjusted hospital cost ($81,000 vs $47,000, p<0.0001). Median follow-up was 7.5 years and patients requiring PPM had significantly worse long-term survival (p=0.02), even after risk adjustment with STS predicted risk of mortality (HR=1.48, p=0.02).
Conclusions
The need for PPM following aortic valve replacement independently reduces long-term survival. The rate of PPM after SAVR remains very low but dramatically increases resource utilization. As TAVR expands into low-risk patients, impact of PPM placement on long-term survival warrants close monitoring.
Classifications: Aortic Valve Replacement, Permanent Pacemaker, TAVR, SAVR
Patients with symptomatic aortic stenosis, a disease associated with high mortality, have historically been offered surgical aortic valve repair (SAVR).(1–3) A high-risk sub group with this disease is known to have poor outcomes indicating the need for a less invasive approach.(1–4) The first transcatheter aortic valve replacement (TAVR) was performed in 2002 and has since grown in popularity.(1, 5, 6) Its use became widespread following the Placement of AoRTic TraNscathetER Valve (PARTNER) trial, which revealed its efficacy in high-risk patients with aortic stenosis.(1, 2, 4, 7, 8) Both SAVR and TAVR are associated with postoperative cardiac conduction abnormalities involving the AV node.(6) Many of these patients require permanent pacemaker placement (PPM) postoperatively. Following SAVR, 2–7% of patients require pacing.(6, 9–11) A considerably larger percentage (6–34%) develops a conduction abnormality requiring pacing following TAVR.(6, 8, 10, 12–15) The reported rates of PPM following TAVR are higher than those reported after SAVR and most estimates are between 10–30%.(6, 8, 10, 12, 15)
The long-term implications of PPM following cardiac surgery are poorly understood.(8, 16) Few studies have demonstrated an association between post-TAVR PPM placement and mortality/clinical events.(8, 16) These studies have been limited in follow-up (3 years) and have demonstrated conflicting results.(8, 16, 17) As TAVR becomes more prevalent and is shifted to lower risk patients, the long-term implications of PPM placement require close monitoring. While the relatively recent widespread use of TAVR makes the long-term impact of PPM difficult to elucidate, the long-term outcomes of PPM placement following SAVR can be examined and may provide insight in the TAVR population. Few data exist regarding the long-term outcome of patients with PPM following SAVR. Much of the existing data groups all cardiac surgery together, has limited sample size, or limited duration of follow up.(11, 18–23) Increased understanding of the long-term implications of PPM following SAVR will help to guide future investigation in the growing population requiring PPM following TAVR.
The purpose of this study was to evaluate the long-term survival of patients undergoing PPM placement following SAVR. We hypothesized a significant decrease in long-term survival in patients requiring PPM placement following SAVR compared to patients not requiring PPM placement.
Patients and Methods
Patient Data
All records for patients undergoing SAVR with or without coronary artery bypass grafting 2002–2017 were extracted from an institutional Society of Thoracic Surgeons database. Patients were excluded for endocarditis, emergent or emergent salvage procedures or if they had prior pacemaker placement. Our institutional clinical data repository (CDR) was queried for all patients requiring PPM placement within 30 days postoperatively. Additionally, social security death records were available in the CDR through the state health department to assess long-term survival. Finally, cost data was available as hospital charge codes are converted to true costs based on conversions derived from direct and indirect costs calculated by the hospital. All cost data are presented as 2016 equivalent dollars with conversion using the market basket for the Center for Medicare and Medicaid Services (CMS) Inpatient Prospective Payment System that captures medical related inflation.
Patients were stratified by need for PPM within 30 days postoperatively. Clinical variables utilize standard STS definitions(24, 25). Operative mortality is defined as either 30-day or in-hospital mortality. Major morbidity includes permanent stroke, prolonged ventilation, reoperation for any reason, renal failure and deep sternal wound infection. The University of Virginia Institutional Review Board approved this study with a waiver of patient consent due to its retrospective nature (IRB Protocol # 19762).
Statistical Analysis
Categorical variables are presented as counts (%) and continuous variables as median [25th, 75th percentile] except for cost, which was reported as mean standard deviation to capture variability. Patients were stratified by need for PPM and compared by univariate analysis using the Chi-square test for categorical variables and Mann-Whitney U test for continuous variables. Kaplan Meier Survival analysis was used to compare long-term survival between groups. Finally, Cox Proportional Hazards model was fit to assess the effects of PPM and other postoperative complications on risk adjusted long-term survival using STS predicted risk of mortality.(26) All statistical analyses were carried out using SAS Version 9.4 (SAS Institutive, Cary, NC) with a p-value less than 0.05 determining significance.
Results
Preoperative characteristics and intraoperative factors
Of 2,600 patients undergoing SAVR over the last 15 years, 72 (2.7%) required PPM placement post-operatively. Of these, 1128 (43.4%) of patients met low risk TAVR criteria with predicted risk of major morbidity or mortality <4.0% with only 28 (2.4%) requiring postoperative PPM placement. The median time to PPM placement was 12 days with all devices placed during index hospitalization. Preoperative characteristics and intraoperative factors in the PPM and no PPM groups were compared (Table 1). Although there were no significant differences in the demographics between groups, the PPM group had significantly higher preoperative rates of cerebral vascular disease (16.7% vs 6.8%, p=0.001), immunosuppression (11.1% vs 4.0%, p=0.003), prior cardiac surgery (23.6% vs 13.2%, p=0.011), and higher STS predicted mortality risk (4.4% vs 3.3%, p=0.009) compared to the no PPM group. Similarly, the PPM group had higher rates of concomitant atrial fibrillation surgery (11.7% vs 9.0%, p=0.006) and longer cardiopulmonary bypass times (116 vs 107 min, p=0.026) compared to the no PPM group (Table 1).
Table 1.
Preoperative Characteristics and Intraoperative Factors By Pacemaker Placement Status After Aortic Valve Replacement
| Preoperative Characteristics | Pacemaker (n=72) |
No Pacemaker (n=2528) |
p-value |
|---|---|---|---|
| Gender (Male) | 39 (54.2%) | 1580 (62.6%) | 0.148 |
| Age (Years) | 74.5 [13.5] | 73 [15] | 0.177 |
| Race (Black) | 8 (10.2%) | 313 (12.4%) | 0.323 |
| Tobacco Use | 27 (37.5%) | 963 (38.1%) | 0.918 |
| Heart Failure within 2 weeks | 40 (55.6%) | 1226 (48.5%) | 0.237 |
| Atrial Fibrillation | 14 (19.4%) | 360 (14.2%) | 0.215 |
| Hypertension | 55 (76.4%) | 1892 (74.8%) | 0.765 |
| Peripheral Arterial Disease | 12 (16.7%) | 373 (14.8%) | 0.652 |
| Cerebral Vascular Disease | 12 (16.7%) | 171 (6.8%) | 0.001 |
| Prior Myocardial Infarction | 18 (25.0%) | 522 (20.7%) | 0.370 |
| Dialysis Dependent | 0 (0.0%) | 56 (2.2%) | 0.202 |
| Diabetes | 26 (36.1%) | 753 (29.8%) | 0.248 |
| Severe Chronic Lung Disease | 2 (2.8%) | 82 (3.2%) | 0.940 |
| Immunosuppression | 8 (11.1%) | 101 (4.0%) | 0.003 |
| Prior Cardiac Surgery | 17 (23.6%) | 333 (13.2%) | 0.011 |
| Intraaortic Balloon Pump | 3 (4.2%) | 69 (2.7%) | 0.464 |
| Aortic Stenosis | 61 (84.7%) | 2282 (90.3%) | 0.117 |
| Severe Aortic Insufficiency | 4 (5.6%) | 230 (9.1%) | 0.303 |
| Predicted Risk of Mortality (%) | 4.4 [5.9] | 3.3 [4.1] | 0.009 |
|
| |||
| Operative Characteristics | |||
|
| |||
| Concomitant Atrial Fibrillation Surgery | 9 (12.5%) | 104 (9.0%) | 0.006 |
| Concomitant Coronary Artery Bypass | 31 (43.0%) | 970 (38.4%) | 0.421 |
| Cardiopulmonary Bypass Time (min) | 116 [54] | 107 [47.5] | 0.026 |
| Cross Clamp Time (min) | 84.5 [49] | 75 [39] | 0.176 |
Postoperative complications
Postoperative complications following SAVR in the PPM and no PPM groups are demonstrated in Table 2. Despite preoperative differences noted above, there were no significant differences in rates of re-operation, stroke, deep sternal wound infection, or operative mortality between groups. However, the group did have higher rates of postoperative atrial fibrillation (43.1% vs 27%, p=0.003), prolonged ventilation (16.7% vs 5.7%, p<0.0001), renal failure (12.5% vs 4.6%, p=0.002), and composite STS major morbidity (26.4% vs 14%, p=0.003) (Table 2).
Table 2.
Complications By Pacemaker Placement Status After Aortic Valve Replacement
| Variable | Pacemaker (n=72) |
No Pacemaker (n=2528) |
p-value |
|---|---|---|---|
| Operative Mortality | 5 (6.9%) | 95 (3.8%) | 0.166 |
| STS Major Morbidity | 19 (26.4%) | 355 (14.0%) | 0.003 |
| Postoperative Atrial Fibrillation | 31 (43.1%) | 682 (27.0%) | 0.003 |
| Prolonged Ventilation | 12 (16.7%) | 143 (5.7%) | <0.0001 |
| Reoperation | 8 (11.1%) | 147 (5.8%) | 0.061 |
| Renal Failure | 9 (12.5%) | 116 (4.6%) | 0.002 |
| Stroke | 3 (4.2%) | 71 (2.8%) | 0.494 |
| Deep Sternal Wound Infection | 1 (1.4%) | 12 (0.5%) | 0.278 |
Resource utilization
While there was no significant difference in rate of discharge to a specialized facility between groups, the PPM group had longer ICU stay (89 vs 44 hours, p<0.0001) and overall postoperative length of stay (9 days vs 6 days, p<0.0001, Table 3). In addition, the PPM group had higher medical-inflation-adjusted hospital cost (81,007 ± 52,680 vs 47,025 ± 35,705, p<0.0001) compared to the no PPM group. Finally, 30-day hospital readmission was significantly higher in the PPM group (20.8% vs 8.4%, p=0.023).
Table 3.
Resource Utilization By Pacemaker Placement Status After Aortic Valve Replacement
| Variable | Pacemaker (n=72) |
No Pacemaker (n=2528) |
p-value |
|---|---|---|---|
| Intensive Care Unit (hours) | 89 [104] | 44 [52] | <0.0001 |
| Postoperative Length of Stay (days) | 9 [6] | 6 [3] | <0.0001 |
| Discharge to Facility | 22 (30.6%) | 537 (21.2%) | 0.058 |
| Hospital Cost (2016 $) | 81,007 ± 52,680 | 47,025 ± 35,705 | <0.0001 |
| Readmission | 15 (20.8%) | 213 (8.4%) | 0.023 |
Survival analysis
Kaplan-Meier curves were generated in order to compare long-term survival between those that required PPM post SAVR and those that did not (Figure). Median follow-up was not significantly different between groups at 7.2 vs 7.6 years (p=0.567). Patients that required PPM had significantly worse long-term survival (p=0.02) compared to those that did not require PPM following SAVR (Figure 1). Most importantly, risk-adjustment for STS predicted risk of mortality using Cox Proportional Hazards modeling demonstrated reduced survival with PPM placement (HR=1.48, p=0.02, Table 4). The effect of PPM on long-term survival was greater than that seen with several other major complications including postoperative atrial fibrillation (HR=1.19, p=0.019) or deep sternal wound infection (HR=1.33, p=0.497). The hazards ratio of PPM placement was similar to other STS major morbidities (Table 4).
Figure 1.
Long-term survival for pacer vs no pacer after aortic valve replacement
Table 4.
Risk-adjusted Effect of Complications on Long-term Survival
| Variable | Hazards Ratio |
95% Confidence Interval | p-value | |
|---|---|---|---|---|
| Pacemaker Placement | 1.48 | 1.02 | 1.94 | 0.023 |
| Postoperative Atrial Fibrillation | 1.19 | 1.01 | 1.31 | 0.019 |
| Stroke | 1.97 | 1.43 | 2.51 | <0.0001 |
| Renal Failure | 2.48 | 1.94 | 3.01 | <0.0001 |
| Reoperation | 2.08 | 1.50 | 2.65 | <0.0001 |
| Deep Sternal Wound Infection | 1.33 | 0.92 | 1.73 | 0.497 |
| Prolonged Ventilation | 2.02 | 1.38 | 2.71 | <0.0001 |
| STS Major Morbidity | 2.15 | 1.55 | 2.74 | <0.0001 |
Comment
The present study demonstrates a relatively low rate of PPM following SAVR, however, this group experiences worse long-term survival compared to those that do not require PPM. Preoperative risks including prior stroke, prior cardiac surgery, and STS predicted risk of mortality were higher in the PPM group compared to the no PPM group. However, PPM placement shortens long-term survival in risk-adjusted models. This study also revealed PPM placement after aortic valve replacement had similar risk-adjusted effects on long-term survival as other STS major morbidities and should be considered a major complication. Finally, PPM placement was associated with greater resource utilization such as longer ICU stay, total hospital length of stay, and overall cost, which has serious implications on healthcare related value.
The rate of PPM placement following SAVR found in this study (2.7%) is within previously reported ranges (2% to 7%).(9, 10, 18, 19) This includes a recent paper by Greason et al demonstrating a 2.5% rate of PPM placement after SAVR over a 25-year study period. Similarly, several previous works have demonstrated increased preoperative risk/comorbidities and rate of postoperative complications in patients requiring PPM following SAVR.(11, 20, 21, 27) We found prior cardiac surgery, cerebral vascular disease, and immunosuppression to be associated with higher rate of PPM placement. Studies have shown similar association with prior cardiac surgery as well as “redo surgery” and rate of PPM placement.(20, 21, 28) Preoperative cerebral vascular disease and immunosuppression have not previously shown this pattern. Interestingly, age was not found to be predictive of postoperative PPM requirement in our analysis while several previous reports have shown an association.(9, 19–21, 29) Congruent with our intra-operative predictors, previous studies have shown positive association between postoperative PPM placement and cardiopulmonary bypass time as well as atrial fibrillation surgery.(20, 30) While an association with intraoperative aortic cross clamp time has also been reported, our analysis did not find this association to be significant.(20, 30)
Postoperative complications positively associated with PPM placement were atrial fibrillation, prolonged ventilation time, and renal failure. A similar association has previously been reported for postoperative atrial fibrillation and ventilation time.(21) While postoperative renal failure has not previously been identified as a postoperative predictor of PPM placement, several studies have identified “electrolyte imbalance/disturbance” as a predictive factor.(30, 31) Congruent with greater postoperative complications, patients receiving postoperative PPM also had longer ICU and overall hospital length of stay. Also not surprisingly as postoperative complications are more predictive of hospitals costs, PPM placement was associated with higher adjusted costs.(32) These resource utilization findings are consistent with previous studies.(9, 18, 20, 21)
This study demonstrated that the need for PPM following aortic valve replacement independently reduces long-term survival. A recent study by Greason and colleagues demonstrated nearly the exact hazards ratio (1.49) for the effect of PPM placement on long-term survival in their study of over five thousand SAVRs.(23) However, that study did not compare the risk-adjusted impact of PPM on survival with the effect of other major complications as seen in table 4. The present study highlighted the importance of PPM placement after SAVR as it had a comparative effect on long-term survival as other STS major morbidities. Raza et al. demonstrated no survival difference between patients receiving PPM following cardiac surgery and those that did not.(33) However, this study had a mean follow up of 5.6 years and was limited by the heterogenous nature of the patients that included all types of cardiac surgery including many patients without aortic valve disease (33). In addition, reports had suggested no significant decrease in survival in aortic stenosis patients requiring PPM following isolated SAVR.(18) In this study by Bagur et al. the number of patients requiring PPM was 25% and the maximum follow up was 5 years.(18) Perhaps the survival difference found in our study is due to the longer follow-up available. In addition, we feel that limiting the analysis to patients requiring PPM following isolated SAVR likely results in a healthier cohort with fewer comorbidities. Patients undergoing SAVR and concomitant CABG were included in our study because we feel this group better approximates the group of patients in whom combined catheter directed therapies including PCI and TAVR is increasingly being offered.
As TAVR becomes more prevalent, the long-term implications of PPM placement require close investigation. In the last several years, few studies have emerged examining the association between post-TAVR PPM placement and long-term mortality.(8, 16, 17) These studies have led to conflicting results. For example, Nazif et al. demonstrated increased one-year mortality in a cohort of 173 patients who required PPM post TAVR.(8) Other studies have contradicted this finding. After a mean follow-up of approximately 2 years, Urena et al. found no increase in mortality for a small cohort of patients requiring PPM post TAVR.(16) Our findings in the PPM post SAVR population suggest that as we move further into the TAVR era, with larger sample sizes it is possible we may see similar impact of PPM in the TAVR population. Thus, long-term follow up following TAVR is essential to determine the implication of postoperative PPM placement, particularly as it is increasingly offered to lower risk patients..
This study has limitations including its retrospective nature. While we were able to control for statistically significant pre-operative risks during our survival analysis, we did not control for intraoperative factors or postoperative complications. This indicates the potential for confounding bias in our survival analysis. Finally, the indication for PPM placement was not available for all patients, however a majority were for an indication of heart block.
In conclusion, we found that the need for PPM following aortic valve replacement is associated with postoperative complications as well as increased resource utilization and independently reduces long-term survival. The rate of PPM after SAVR remains very low but dramatically increases resource utilization. As TAVR expands into low-risk patients, impact of PPM placement on long-term survival warrants close monitoring.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Leon MB, Smith CR, Mack M, et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. The New England journal of medicine. 2010;363(17):1597–1607. doi: 10.1056/NEJMoa1008232. [DOI] [PubMed] [Google Scholar]
- 2.Smith CR, Leon MB, Mack MJ, et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. New England Journal of Medicine. 2011;364(23):2187–2198. doi: 10.1056/NEJMoa1103510. [DOI] [PubMed] [Google Scholar]
- 3.Iung B, Cachier A, Baron G, et al. Decision-making in elderly patients with severe aortic stenosis: Why are so many denied surgery? Eur Heart J. 2005;26(24):2714–2720. doi: 10.1093/eurheartj/ehi471. [DOI] [PubMed] [Google Scholar]
- 4.Daubert MA, Weissman NJ, Hahn RT, et al. Long-term valve performance of tavr and savr: A report from the partner i trial. JACC Cardiovascular imaging 2016. doi: 10.1016/j.jcmg.2016.11.004. [DOI] [PubMed] [Google Scholar]
- 5.Cribier A, Eltchaninoff H, Bash A, et al. Percutaneous transcatheter implantation of an aortic valve prosthesis for calcific aortic stenosis: First human case description. Circulation. 2002;106(24):3006–3008. doi: 10.1161/01.cir.0000047200.36165.b8. [DOI] [PubMed] [Google Scholar]
- 6.Young Lee M, Chilakamarri Yeshwant S, Chava S, Lawrence Lustgarten D. Mechanisms of heart block after transcatheter aortic valve replacement - cardiac anatomy, clinical predictors and mechanical factors that contribute to permanent pacemaker implantation. Arrhythmia & electrophysiology review. 2015;4(2):81–85. doi: 10.15420/aer.2015.04.02.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kapadia SR, Leon MB, Makkar RR, et al. 5-year outcomes of transcatheter aortic valve replacement compared with standard treatment for patients with inoperable aortic stenosis (partner 1): A randomised controlled trial. Lancet. 2015;385(9986):2485–2491. doi: 10.1016/S0140-6736(15)60290-2. [DOI] [PubMed] [Google Scholar]
- 8.Nazif TM, Dizon JM, Hahn RT, et al. Predictors and clinical outcomes of permanent pacemaker implantation after transcatheter aortic valve replacement: The partner (placement of aortic transcatheter valves) trial and registry. JACC Cardiovascular interventions. 2015;8(1 Pt A):60–69. doi: 10.1016/j.jcin.2014.07.022. [DOI] [PubMed] [Google Scholar]
- 9.Robich MP, Schiltz NK, Johnston DR, et al. Risk factors and outcomes of patients requiring a permanent pacemaker after aortic valve replacement in the united states. Journal of cardiac surgery. 2016;31(8):476–485. doi: 10.1111/jocs.12769. [DOI] [PubMed] [Google Scholar]
- 10.Simms AD, Hogarth AJ, Hudson EA, et al. Ongoing requirement for pacing post-transcatheter aortic valve implantation and surgical aortic valve replacement. Interactive cardiovascular and thoracic surgery. 2013;17(2):328–333. doi: 10.1093/icvts/ivt175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huynh H, Dalloul G, Ghanbari H, et al. Permanent pacemaker implantation following aortic valve replacement: Current prevalence and clinical predictors. Pacing and clinical electrophysiology : PACE. 2009;32(12):1520–1525. doi: 10.1111/j.1540-8159.2009.02552.x. [DOI] [PubMed] [Google Scholar]
- 12.Bagur R, Rodes-Cabau J, Gurvitch R, et al. Need for permanent pacemaker as a complication of transcatheter aortic valve implantation and surgical aortic valve replacement in elderly patients with severe aortic stenosis and similar baseline electrocardiographic findings. JACC Cardiovascular interventions. 2012;5(5):540–551. doi: 10.1016/j.jcin.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 13.Bates MG, Matthews IG, Fazal IA, Turley AJ. Postoperative permanent pacemaker implantation in patients undergoing trans-catheter aortic valve implantation: What is the incidence and are there any predicting factors? Interactive cardiovascular and thoracic surgery. 2011;12(2):243–253. doi: 10.1510/icvts.2010.256578. [DOI] [PubMed] [Google Scholar]
- 14.Piazza N, Onuma Y, Jesserun E, et al. Early and persistent intraventricular conduction abnormalities and requirements for pacemaking after percutaneous replacement of the aortic valve. JACC Cardiovascular interventions. 2008;1(3):310–316. doi: 10.1016/j.jcin.2008.04.007. [DOI] [PubMed] [Google Scholar]
- 15.Siontis GC, Juni P, Pilgrim T, et al. Predictors of permanent pacemaker implantation in patients with severe aortic stenosis undergoing tavr: A meta-analysis. Journal of the American College of Cardiology. 2014;64(2):129–140. doi: 10.1016/j.jacc.2014.04.033. [DOI] [PubMed] [Google Scholar]
- 16.Urena M, Webb JG, Tamburino C, et al. Permanent pacemaker implantation after transcatheter aortic valve implantation: Impact on late clinical outcomes and left ventricular function. Circulation. 2014;129(11):1233–1243. doi: 10.1161/CIRCULATIONAHA.113.005479. [DOI] [PubMed] [Google Scholar]
- 17.Mohananey D, Jobanputra Y, Kumar A, et al. Clinical and echocardiographic outcomes following permanent pacemaker implantation after transcatheter aortic valve replacement: Meta-analysis and meta-regression. Circulation Cardiovascular interventions. 2017;10(7) doi: 10.1161/CIRCINTERVENTIONS.117.005046. [DOI] [PubMed] [Google Scholar]
- 18.Bagur R, Manazzoni JM, Dumont E, et al. Permanent pacemaker implantation following isolated aortic valve replacement in a large cohort of elderly patients with severe aortic stenosis. Heart (British Cardiac Society) 2011;97(20):1687–1694. doi: 10.1136/heartjnl-2011-300308. [DOI] [PubMed] [Google Scholar]
- 19.Goldman BS, Hill TJ, Weisel RD, et al. Permanent cardiac pacing after open-heart surgery: Acquired heart disease. Pacing and clinical electrophysiology : PACE. 1984;7(3 Pt 1):367–371. doi: 10.1111/j.1540-8159.1984.tb04919.x. [DOI] [PubMed] [Google Scholar]
- 20.Gordon RS, Ivanov J, Cohen G, Ralph-Edwards AL. Permanent cardiac pacing after a cardiac operation: Predicting the use of permanent pacemakers. The Annals of thoracic surgery. 1998;66(5):1698–1704. doi: 10.1016/s0003-4975(98)00889-3. [DOI] [PubMed] [Google Scholar]
- 21.Del Rizzo DF, Nishimura S, Lau C, Sever J, Goldman BS. Cardiac pacing following surgery for acquired heart disease. Journal of cardiac surgery. 1996;11(5):332–340. doi: 10.1111/j.1540-8191.1996.tb00059.x. [DOI] [PubMed] [Google Scholar]
- 22.Baraki H, Al Ahmad A, Jeng-Singh S, et al. Pacemaker dependency after isolated aortic valve replacement: Do conductance disorders recover over time? Interactive cardiovascular and thoracic surgery. 2013;16(4):476–481. doi: 10.1093/icvts/ivs555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Greason KL, Lahr BD, Stulak JM, et al. Long-term mortality effect of early pacemaker implantation after surgical aortic valve replacement. Ann Thorac Surg. 2017;104(4):1259–1264. doi: 10.1016/j.athoracsur.2017.01.083. [DOI] [PubMed] [Google Scholar]
- 24.O'Brien SM, Shahian DM, Filardo G, et al. The society of thoracic surgeons 2008 cardiac surgery risk models: Part 2--isolated valve surgery. Ann Thorac Surg. 2009;88(1 Suppl):S23–42. doi: 10.1016/j.athoracsur.2009.05.056. [DOI] [PubMed] [Google Scholar]
- 25.Shih T, Paone G, Theurer PF, McDonald D, Shahian DM, Prager RL. The society of thoracic surgeons adult cardiac surgery database version 2.73: More is better. Ann Thorac Surg. 2015;100(2):516–521. doi: 10.1016/j.athoracsur.2015.02.085. [DOI] [PubMed] [Google Scholar]
- 26.Puskas JD, Kilgo PD, Thourani VH, et al. The society of thoracic surgeons 30-day predicted risk of mortality score also predicts long-term survival. Ann Thorac Surg. 2012;93(1):26–33. doi: 10.1016/j.athoracsur.2011.07.086. discussion 33-25. [DOI] [PubMed] [Google Scholar]
- 27.Erdogan HB, Kayalar N, Ardal H, et al. Risk factors for requirement of permanent pacemaker implantation after aortic valve replacement. Journal of cardiac surgery. 2006;21(3):211–215. doi: 10.1111/j.1540-8191.2006.00216.x. discussion 216–217. [DOI] [PubMed] [Google Scholar]
- 28.Van Mieghem NM, Head SJ, de Jong W, et al. Persistent annual permanent pacemaker implantation rate after surgical aortic valve replacement in patients with severe aortic stenosis. The Annals of thoracic surgery. 2012;94(4):1143–1149. doi: 10.1016/j.athoracsur.2012.04.038. [DOI] [PubMed] [Google Scholar]
- 29.Kogan A, Sternik L, Beinart R, et al. Permanent pacemaker insertion following isolated aortic valve replacement before and after the introduction of tavi. Pacing and clinical electrophysiology : PACE. 2015;38(4):424–430. doi: 10.1111/pace.12569. [DOI] [PubMed] [Google Scholar]
- 30.Klapkowski A, Pawlaczyk R, Kempa M, Jagielak D, Brzezinski M, Rogowski J. Complete atrioventricular block after isolated aortic valve replacement. Kardiologia polska. 2016;74(9):985–993. doi: 10.5603/KP.a2016.0038. [DOI] [PubMed] [Google Scholar]
- 31.Limongelli G, Ducceschi V, D'Andrea A, et al. Risk factors for pacemaker implantation following aortic valve replacement: A single centre experience. Heart (British Cardiac Society) 2003;89(8):901–904. doi: 10.1136/heart.89.8.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hawkins RB, Mehaffey JH, Yount KW, et al. Coronary artery bypass grafting bundled payment proposal will have significant financial impact on hospitals. J Thorac Cardiovasc Surg 2017. doi: 10.1016/j.jtcvs.2017.07.035. [DOI] [PubMed] [Google Scholar]
- 33.Raza SS, Li JM, John R, et al. Long-term mortality and pacing outcomes of patients with permanent pacemaker implantation after cardiac surgery. Pacing and clinical electrophysiology : PACE. 2011;34(3):331–338. doi: 10.1111/j.1540-8159.2010.02972.x. [DOI] [PubMed] [Google Scholar]